Summary
Background
Health authorities worldwide, especially in the Asia Pacific region, are seeking effective public-health interventions in the continuing epidemic of severe acute respiratory syndrome (SARS). We assessed the epidemiology of SARS in Hong Kong.
Methods
We included 1425 cases reported up to April 28, 2003. An integrated database was constructed from several sources containing information on epidemiological, demographic, and clinical variables. We estimated the key epidemiological distributions: infection to onset, onset to admission, admission to death, and admission to discharge. We measured associations between the estimated case fatality rate and patients’age and the time from onset to admission.
Findings
After the initial phase of exponential growth, the rate of confirmed cases fell to less than 20 per day by April 28. Public-health interventions included encouragement to report to hospital rapidly after the onset of clinical symptoms, contact tracing for confirmed and suspected cases, and quarantining, monitoring, and restricting the travel of contacts. The mean incubation period of the disease is estimated to be 6.4 days (95% Cl 5.2–7.7). The mean time from onset of clinical symptoms to admission to hospital varied between 3 and 5 days, with longer times earlier in the epidemic. The estimated case fatality rate was 13.2% (9.8–16.8) for patients younger than 60 years and 43.3% (35.2–52.4) for patients aged 60 years or older assuming a parametric γ distribution. A non-parametric method yielded estimates of 6.8% (4.0–9.6) and 55.0% (45.3–64.7), respectively. Case clusters have played an important part in the course of the epidemic.
Interpretation
Patients’age was strongly associated with outcome. The time between onset of symptoms and admission to hospital did not alter outcome, but shorter intervals will be important to the wider population by restricting the infectious period before patients are placed in quarantine.
Published online May 7, 2003 http://image.thelancet.com/extras/03art4453web.pdf
Introduction
The rapid worldwide spread of the coronavirus that causes severe acute respiratory syndrome (SARS)1, 2 has led to 28 countries reporting cases as of May 5, 2003. The evolution, spread, and persistence of infectious diseases are facilitated by the mobility of contemporary society, for example through air travel, the continued growth in the world population, and the steady rise in the number of densely populated urban areas, especially in Asia.
The Asia Pacific region, including mainland China, has been badly affected by SARS. The impact on the regional economy and health-care systems led to a meeting of health ministers from 14 Association of South East Asian Nations on April 24–26. Health authorities are urgently seeking guidance on the public-health measures most likely to be effective in controlling the epidemic.
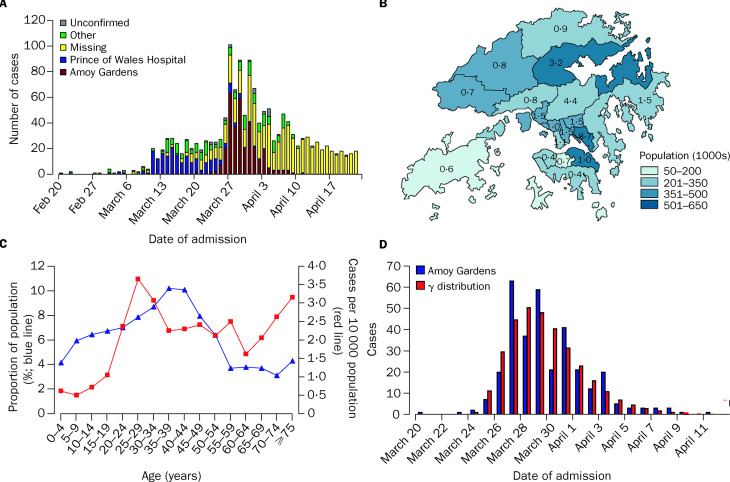
Key epidemiological determinants of the magnitude and timescale of the epidemic (figure 1 ) include the interval between infection and onset of symptoms and between onset and hospital admission, the degree and duration of the infectiousness of the agent, and the extent of contact and mixing between infectious and susceptible people enabling transmission of the virus. Public-health interventions can affect many of these factors.
Figure 1.
Epidemiological description of SARS epidemic in Hong Kong
A: Temporal pattern of SARS epidemic in Hong Kong by cluster of infection. B: Spatial distribution of population of Hong Kong and district-specific incidence (per 10 000 population) over course of epidemic to date. C: Age distribution of residents of Hong Kong and age-specific incidence (per 10 000 population) over course of epidemic to date. D: Detail of temporal pattern for Amoy Gardens cluster, according to day of admission, and fitted γ distribution.
The Hong Kong authorities have taken several measures to combat the spread of SARS. Since formal recognition of the outbreak in the Prince of Wales Hospital, Hong Kong, on March 10, these measures have included: public-service announcements about personal protection (March 17); addition of SARS to the list of notifiable diseases and requests for close contacts of cases to attend designated medical centres for screening (March 26) until the later introduction of mandatory home quarantine; a 2-week suspension of schools’(March 26) and universities’(March 29) sessions; introduction of health declarations for all incoming residents and visitors (March 29); isolation of residents of a building in the Amoy Gardens estate, at the centre of a cluster of about 300 cases (March 30) and their subsequent move to rural isolation camps for 10 days (March 31); home quarantining of close contacts and restrictions on their travel out of Hong Kong (April 10); new public announcements urging symptomatic people to seek medical attention (April 15); and body-temperature checks for all air passengers (April 17).
In the global response to SARS, there are three priority tasks: the identification of the causal agent and the development of tests to detect the virus and allow rapid confirmation of cases; the development and assessment of treatment protocols; and the determination of the key epidemiological processes and parameters that affect the spread and persistence of infection to support the formulation of appropriate public-health interventions. We describe the epidemiology in Hong Kong in the first 9 weeks of the epidemic, during which 1425 cases were confirmed, and 122 deaths from SARS occurred. We focus on the key distributions and parameters that define the observed pattern of the spread of SARS, and their change over time since the introduction of the virus into Hong Kong.
Methods
Data sources
We analysed an integrated database, coordinated by the Department of Community Medicine, University of Hong Kong on behalf of the Health, Welfare and Food Bureau, derived from the Hong Kong Hospital Authority eSARS system, and the Department of Health's Master List, which contains details of all patients with confirmed or suspected SARS admitted to hospitals in Hong Kong since Feb 20, 2003. Primary health care in Hong Kong is provided by private practitioners (80%) and general outpatient departments operated by the public sector. The Hospital Authority also currently provides 95% of total inpatient bed-days.3 The Department of Health provides the public-health function, including the monitoring and control of communicable diseases.4 The eSARS system is designed as a registry and monitoring system. All patients admitted for investigation and observation into the SARS cohort wards in all the hospitals under the Hospital Authority of Hong Kong are recruited on entry. The patients on the registry are progressively classified into: patient under observation, patient suspected of SARS, patient with confirmed SARS, and not SARS. The criteria for inclusion in the eSARS register as a patient confirmed with SARS are radio-graphic evidence of infiltrates consistent with pneumonia, and current fever higher than 38°C or history of such at any time in the past 2 days, and at least two of the following: history of chills in the past 2 days, cough (new or increased) or breathing difficulty, general malaise or myalgia, and known exposure. Patients are listed as suspected of having SARS if they do not fulfil this definition but are still thought to be likely cases of SARS on the basis of the collective evidence and clinical judgment. However, patients are excluded if an alternative diagnosis can fully explain their illness.
A questionnaire was administered to all patients 24 h after confirmation of SARS by the Department of Health, initially by regional community-medicine teams and later by a central interviewing team of nurses, to record symptoms at presentation to hospital and to identify contacts and events of probable relevance to transmission. When possible, patients are classified into infection clusters by location (eg, housing estates), occupation (eg, health-care workers), and workplace (eg, hospitals and other buildings). In addition, we used demographic data on Hong Kong, which has a population size of 6.7 million in 19 districts (figure 1).
Statistical analysis
Time-delay distributions (infection to onset, onset to admission, admission to death, and admission to discharge) were fitted to γ distributions by maximum likelihood estimation methods, with allowance for censoring for incomplete observation of the disease process in all cases. Likelihood ratio statistics were used for tests of significance when comparing distributional parameters and for calculating CI.
While the epidemic is continuing, the estimation of the admission-to-death and admission-to-discharge distributions must be undertaken jointly with the estimation of the case fatality rate, because among patients still recorded as being in hospital it is impossible to ascertain who will eventually die or be discharged. We assume that no confirmed SARS patients who has been discharged from hospital will go on to die of SARS-related causes. If F() and G() are the cumulative distribution functions of the admission-to-death and admission-to-discharge distributions, respectively, and πF is the case fatality rate—ie, the proportion of SARS patients who will die of the disease—the following likelihood structure is assumed: if a patient died t days after admission, the likelihood is πF′[F(t+1)–F(t)]; if a patient was discharged t days after admission, the likelihood is (1–πF)×[G(t+1)–G(t)]; and if a patient remained in hospital t days after admission, the likelihood is πF×[1-F(t)]+(1-πF)]×[1–G(t)]. The parameters of the F() and G() distributions are thus jointly estimated along with the case fatality rate.
To assess further the case fatality rate, we also used a version of the Kaplan-Meier survival curve, adapted to allow for two types of outcome (death and discharge). Censoring was used to obtain non-parametric estimates of the admission-to-death and admission-to-discharge distributions and the case fatality rate.
Role of the funding source
The sponsors of the study had no role in the study design, data collection, data analysis, data interpretation, or in the writing of the report.
Results
The development of the epidemic (figure 1) features a period of exponential growth, beginning on March 10, after the formal announcement of the outbreak, followed by a period of comparative stability throughout early to mid April, with evidence of a slight decay over the week April 21–28. The geographical and age distributions of the cases are presented in figure 1. 57% of patients were female and 43% male.
Clinical symptoms at presentation were fully recorded for about 90% of the cases confirmed by the Department of Health. The frequency of self-reported symptoms is similar to that noted in the early cases.5 The most common reported symptom was fever (94%), with 51–72% of patients reporting general influenza-like symptoms, chills, malaise, loss of appetite, and myalgia. Gastrointestinal symptoms were less common at presentation, including diarrhoea (27%), vomiting (14%), and abdominal pain (13%). 88% reported fever plus any one other symptom, and 79% fever plus one of the five most common symptoms (table ).
Table.
Prevalence of self-reported clinical symptoms in cases confirmed by Department of Health
| Overall proportion with specified symptom (%) | |
|---|---|
| Symptom | |
| Fever | 94.0 |
| Influenza-like | 72.3 |
| Chills | 65.4 |
| Malaise | 64.3 |
| Loss of appetite | 54.6 |
| Myalgia | 50.8 |
| Cough | 50.4 |
| Headache | 50.1 |
| Rigor | 43.7 |
| Dizziness | 30.7 |
| Shortness of breath | 30.6 |
| Sputum | 27.8 |
| Night sweat | 27.8 |
| Diarrhoea | 27.0 |
| Coryza | 24.6 |
| Sore throat | 23.1 |
| Nausea | 22.2 |
| Vomiting | 14.0 |
| Abdominal pain | 12.6 |
| Fever+at least 1 other | 87.6 |
| Fever+at least 2 other | 80.3 |
| Fever+at least 3 other | 70.7 |
| Fever+at least 1 of 5 most common* | 78.5 |
| Fever+at least 2 of 5 most common* | 61.7 |
| Fever+at least 3 of 5 most common* | 42.9 |
Five most common symptoms (except fever): influenza-like, chills, malaise, loss of appetite, and myalgia.
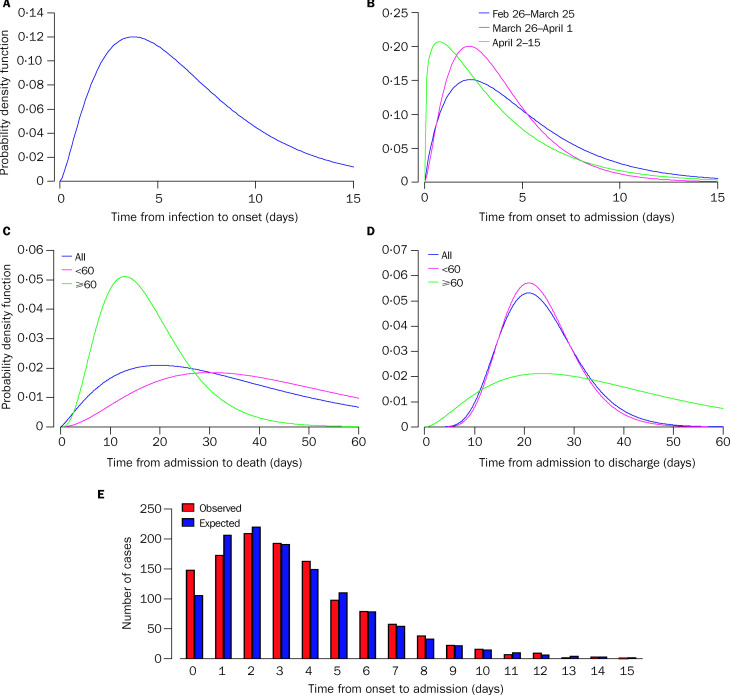
Infection events cannot be observed, but for patients with short and defined periods of exposure to known SARS cases, data on the timing and duration of exposure can be used to estimate the distribution of the incubation period, the time from infection to the onset of clinical symptoms of SARS. The database contained 57 patients with one exposure to SARS over a limited time scale with recorded start and end dates. The maximum likelihood estimate of the mean and variance of the time from infection to onset was 6.37 days (95 CI 5.29–7.75) and 16.69 days2, respectively; therefore 95% of patients would experience the onset of symptoms within 14.22 days of infection. The estimated distribution is presented in figure 2 . However, this distribution is based on a limited number of observations to date, and has high variance and may reflect biases in reporting, different routes of transmission, or varying infectious doses of the virus.
Figure 2.
Maximum likelihood estimates
A: Infection-to-onset distribution. B: Time-dependent onset-to-admission distribution as a function of time of onset of clinical symptoms. C: Admission-to-death distribution by patients’age. D: Admission-to-discharge distribution by patients’age. E: Observed and maximum likelihood estimated onset-to-admission intervals in presence of censoring.
Onset and admission times are both observable events. However, allowance must be made in the analysis for censoring due to incomplete observation. If censoring is not taken into account, the distribution will be biased towards short onset-to-admission times, because patients are only eligible to be included in the hospital-based database on admission to hospital. Patients with recent onsets and long onset-to-admission times are less likely to have been admitted to hospital and thus be included.
In the analysis, patients were grouped by their week of clinical onset, and seven weekly time periods were analysed (Feb 26 to March 4, March 5–11, March 12–18, March 19–25, March 26 to April 1, April 2–8, and April 9–15). There were too few patients with clinical onset before Feb 26 for robust analysis and too little time has elapsed after onset to allow analysis of those with clinical onset after April 15. We assume that the recorded data are complete up to April 15. Estimated mean onset-to-admission times were obtained for each week, assuming that the times were γ distributed: Feb 26 to March 4, 5.36; March 5–11, 3.21; March 12–18, 5.06; March 19–25, 4.95; March 26 to April 1, 3.83; April 2–8, 3.67; and April 9–15, 3.46. The distributions differed significantly over the 7-week period (p<0.001) but not for the first 4 weeks (p=0.053) or the last 2 weeks (p=0.459). The maximum likelihood means and variances for the resulting three time periods are: Feb 26 to March 25, 48.5 days (95% CI 4.49–5.24) and 12.19 days2; March 26 to April 1, 3.83 (3.61–4.06) and 5.99 days2; and April 2–15, 3.67 days (3.31–4.11) and 10.7122 days. The corresponding distributions are presented in figure 2, as well as the qualitatively good fit between the observed and expected values in the presence of censoring.
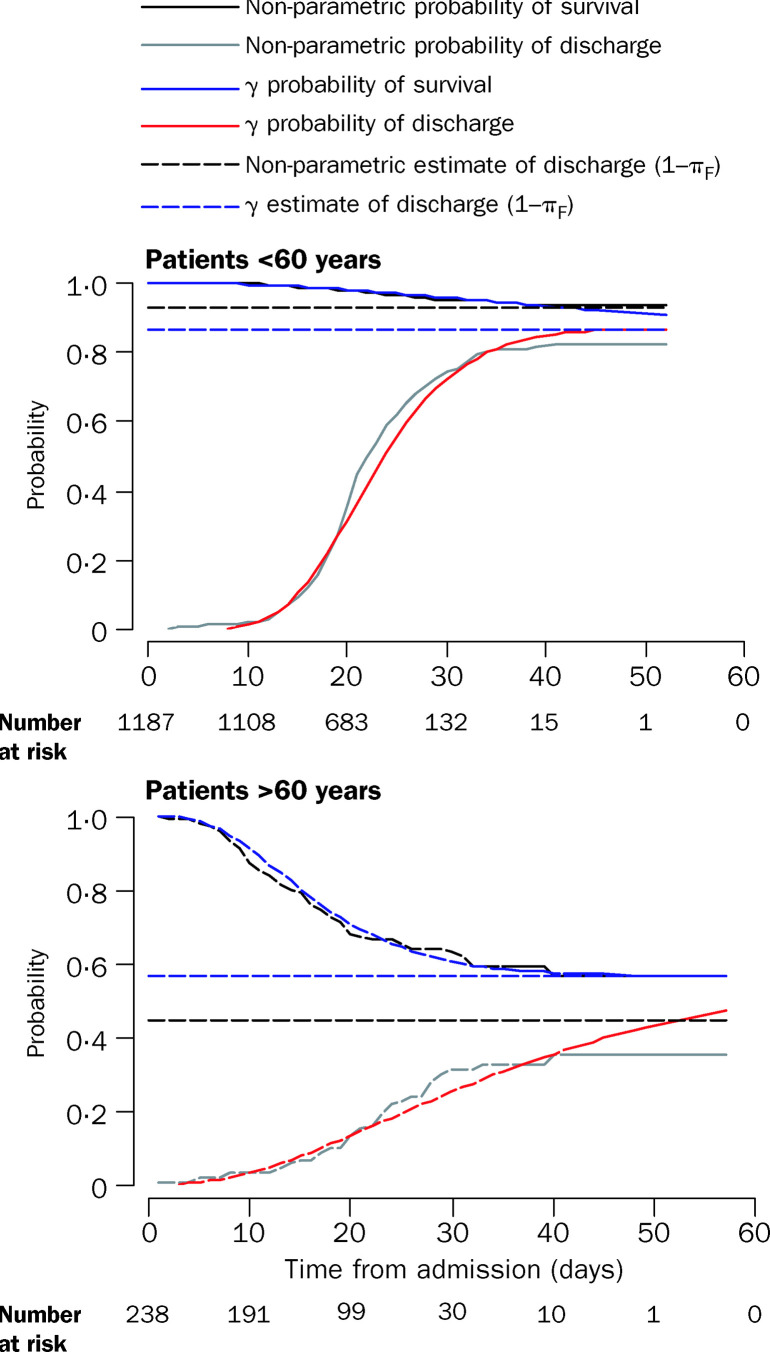
The estimated mean and variance of the admission-to-death time was 35.9 days and 572.92 days, respectively, and the estimated mean and variance of the time from admission to discharge was 23.5 days and 62.12 days, respectively (figure 2). If γ distribution is assumed, the estimated distributions and case fatality rate varied as a function of patients’age, but not the time from onset to admission (figure 2). The estimated case fatality rate for patients younger than 60 years was 13.2% (9.8–16.8) and 43.3% (35.2–52.4) for patients aged 60 years and older. The adapted Kaplan-Meier-like non-parametric method gave estimates of 6.8% (4.0–9.6) and 55.0% (45.3–64.7), respectively (figure 3 ). The estimated fatality rates are higher than the estimate obtained from the current cumulative number of deaths divided by the current cumulative number of hospital admissions, because of the incomplete follow-up on patients still in hospital.
Figure 3.
Non-parametric and maximum-likelihood γ probabilities of survival and discharge
A key feature of this epidemic is the clustering of cases in place and time linked to a particular individual (in some cases in a particular setting such as a residence block or health-care setting), where one primary case has led to many secondary and tertiary cases. The Amoy Gardens outbreak is particularly striking, with the onset times of the cases identified as arising from this setting following a γ distribution (figure 1). Work on the clusters is still evolving and will be reported in detail separately.
Discussion
Our findings underline the importance of estimating the key epidemiological determinants of the epidemic, the infection-to-onset and onset-to-admission interval distributions. The analysis of the onset-to-admission interval shows that over time there has been a progressive shortening of the time from clinical onset of symptoms to presentation at hospital.
The estimation of case fatality rates in the situation of an emerging epidemic is not straightforward. First, our estimates are derived from data on clinical cases that have been admitted to hospital and, hence, estimate the mortality rate only in this population. Second, the temporal evolution of the epidemic complicates analysis. Finally, the estimates of the case fatality may vary dependent on the methods used and their underlying assumptions, although the estimates we present have statistical validity. All these issues require further investigation as the epidemic evolves, and explain partly the wide range of mortality estimates reported to date.
Shortening the time between onset of clinical symptoms and admission to hospital does not seem to affect clinical outcome. However, shortening the time from clinical onset to admission expedites isolation and reduces the effective infectious period and, thus, the risk of onward transmission. Such changes were already evident in late March and early April, but any additional shortening of the time that symptomatic individuals are in the community will lead to further benefits at the population level. The extent to which this time needs to be shortened to reduce the generation of secondary cases from each primary case to less than one (the effective reproductive number, R0) in Hong Kong is the subject of a continuing analysis.
Given the likely benefits to the wider community from early presentation at hospital after the onset of symptoms, there should now be an intensive assessment of the different public-health interventions, including publicity campaigns in various media, to assess their impact on the early reporting of symptoms. The promotion of early reporting of all symptoms will challenge the health-care system in dealing with those caused by other pathogens and the so-called worried well. However, given the high need for intensive care of patients, the case fatality rate, and public alarm worldwide, use of stringent measures to limit the effective infectious period of probable SARS cases would seem prudent. This approach alone may contribute substantially to the eventual curtailing or even eradication of the epidemic.
The epidemic has shown the need for communication of risk that will inform and warn the public, in a way that will improve personal protection, without inducing raised anxiety and fear, as an essential part of epidemic control. A change in risk perception would potentially lead to an increase in early reporting of symptoms as well as improvements in hygiene and prevention of transmission.
Further data may reveal that the incubation period depends on the route of transmission and on the infectious dose received by an individual. The duration of the infectious period and its relation to the incubation period is uncertain at present (for example, the onset of infectiousness may precede the onset of clinical symptoms). Continuing clinical studies involving quantitative assays of viral load at known times after exposure and after the onset of clinical symptoms should, however, clarify this property of the SARS agent. Critical questions relating to how long patients should remain in isolation are whether and to what extent virus remains in faeces or in aspirate after overt clinical symptoms have stopped.
The occurrence of clusters of cases linked to particular individuals in a particular spatial setting has been an important determinant of the overall magnitude of the epidemic to date. A WHO team has now joined the Hong Kong Government in examining on-site factors that were apparently associated with a possible point-source outbreak in Amoy Gardens.6 The assessment of whether there is variation in the characteristics of the disease, including presenting symptoms by different clusters, requires further investigation as the definition of clusters improves. The occurrence of clusters is not necessarily a feature that can inform public-health interventions in advance, except within health-care settings in which stringent isolation procedures must be adopted in handling suspected and confirmed cases. Clusters do, however, provide a focus for contact-tracing studies to assess incubation periods and the nature of the contact that resulted in transmission.
The reported cases to date in Hong Kong and elsewhere may simply reflect people with the most severe clinical symptoms of infection with the new SARS virus. We estimated the case fatality rate based on cases in hospital only. If additional infections in the community do not lead to admission to hospital or death, the case fatality rate based on all infections would be lower. Community-based serological surveys to assess infection and recovery rates are a priority once a specific and sensitive serological test is available.
Finally the warm season has begun in Hong Kong, with daily temperatures now at 25–30°C. The seasonal risks of dengue and influenza will increase, and if serious outbreaks occur, they will complicate the triage of patients with possible symptoms of SARS. Thus, measures that can be taken now to limit further transmission, such as the shortening of the onset-to-admission interval, should be given high priority.
Acknowledgments
We thank David R Cox for developing a suitable non-parametric method for estimation of the case fatality rate. ACG and NMF receive fellowship support from The Royal Society. SR and NMF receive research funding from the Howard Hughes Medical Institute, CF, LJA-R, and NMF from the Medical Research Council, and RMA from the Wellcome Trust. We thank Tom Johnston for Geographic Information System assistance. We thank all our colleagues in the Department of Health and the Hospital Authority for their work in data collection and processing, and pay tribute to all the front-line health workers who are caring for patients with SARS.
References
- 1.Peiris JSM, Lai ST, Poon LLM. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Coronavirus never before seen in humans is the cause of SARS. www.who.int/mediacentre/releases/2003/pr31/en/ (accessed May 5, 2003).
- 3.Hong Kong Hospital Authority. www.ha.org.hk (accessed May 5, 2003).
- 4.Department of Health, Hong Kong Government of Special Administrative Region website. http://www.info.gov.hk/dh/ (accessed May 5, 2003).
- 5.Tsang KW, Ho PL, Ooi GC, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. http://content.nejm.org/cgi/reprint/NEJMoa030666v3.pdf (accessed May 5, 2003). [DOI] [PubMed]
- 6.WHO. Cumulative number of reported probable cases of severe acute respiratory syndrome (SARS). www.who.int/csr/sarscountry/en/ (accessed May 5, 2003).