Summary
Background
We investigated the temporal progression of the clinical, radiological, and virological changes in a community outbreak of severe acute respiratory syndrome (SARS).
Methods
We followed up 75 patients for 3 weeks managed with a standard treatment protocol of ribavirin and corticosteroids, and assessed the pattern of clinical disease, viral load, risk factors for poor clinical outcome, and the usefulness of virological diagnostic methods.
Findings
Fever and pneumonia initially improved but 64 (85%) patients developed recurrent fever after a mean of 8.9 (SD 3.1) days, 55 (73%) had watery diarrhoea after 7.5 (2.3) days, 60 (80%) had radiological worsening after 7.4 (2.2) days, and respiratory symptoms worsened in 34 (45%) after 8.6 (3.0) days. In 34 (45%) patients, improvement of initial pulmonary lesions was associated with appearance of new radiological lesions at other sites. Nine (12%) patients developed spontaneous pneumomediastinum and 15 (20%) developed acute respiratory distress syndrome (ARDS) in week 3. Quantitative reverse-transcriptase (RT) PCR of nasopharyngeal aspirates in 14 patients (four with ARDS) showed peak viral load at day 10, and at day 15 a load lower than at admission. Age and chronic hepatitis B virus infection treated with lamivudine were independent significant risk factors for progression to ARDS (p=0.001). SARS-associated coronavirus in faeces was seen on RT-PCR in 65 (97%) of 67 patients at day 14. The mean time to seroconversion was 20 days.
Interpretation
The consistent clinical progression, shifting radiological infiltrates, and an inverted V viral-load profile suggest that worsening in week 2 is unrelated to uncontrolled viral replication but may be related to immunopathological damage.
Published online May 9, 2003 http://image.thelancet.com/extras/03art4432web.pdf
Introduction
Severe acute respiratory syndrome (SARS) is a new emerging disease that has affected many countries, with more than 3500 cases reported. A novel virus, the SARS-associated coronavirus, has been identified as the causal agent.1, 2, 3, 4 The clinical, radiological, and other investigative findings at initial presentation have been previously described,5, 6, 7 but the temporal progression is unclear. The routes and duration of viral shedding and the best clinical samples for diagnosis at different stages of the illness are also largely unknown. From March 24, 2003, a major outbreak of SARS involving 321 patients occurred in Amoy Gardens, a high-rise housing estate in Hong Kong. Epidemiological investigations suggested a point-source outbreak, which was linked to a faulty sewage system, initially contaminated by the excreta of the index case who visited the housing block on March 14 and 19.8 The first 75 adult patients, belonging to 57 households, were admitted with a clinical diagnosis of SARS to one hospital. We did a prospective study on the clinical, haematological, radiological, and microbiological findings of these 75 patients over a period of 24 days, and correlated these findings with treatment9, 10 and with viral load in the nasopharyngeal aspirate to elucidate the pathogenesis and the impact of treatment. We report the usefulness of different clinical samples for virological diagnosis and its importance in transmission.
Patients and methods
Patients
Between March 24 and 28, 2003, we included 75 patients admitted to the United Christian Hospital from the Amoy Gardens housing estate who fulfilled the modified WHO definition of SARS.3 Briefly, the case definition is: fever 38°C or higher, cough or shortness of breath, new pulmonary infiltrates on chest radiography or high-resolution CT in the absence of an alternative diagnosis to explain the clinical presentation. Patients were nursed in an isolation ward with other SARS patients.
Methods
The study was approved by the ethics committee of the United Christian Hospital, Hong Kong. We entered on a predesigned database the daily clinical findings based on history and physical examination, oximetric measurement, and haematological, biochemical, radiological, and microbiological investigations. We collected nasopharyngeal aspirates and clotted blood for virological studies from all patients at presentation and on day 14 after the onset of illnesses. Anteroposterior chest radiography was done daily for each patient. All chest radiographs were jointly reported by specialist radiologists and respiratory physicians. We did high-resolution CT of the thorax for patients who had apparently normal, equivocal, or atypical chest radiographs. For patients who developed acute respiratory distress syndrome (ARDS) with partial arterial pressure of oxygen (PaO2) to fraction of inspired oxygen (FiO2) less than 26.6 kPa,11 and recorded acute physiology and chronic health evaluation II (APACHE II) scores.12
From 20 patients in whom SARS-associated coronavirus RNA was detected by reverse-transcriptase (RT) PCR in the initial nasopharyngeal aspirate samples, we collected further nasopharyngeal aspirates, urine, and faecal samples every 3 days. In 14 of these patients, quantitative PCR was done on the nasopharyngeal aspirates collected on days 5, 10, and 15 after onset of symptoms. The nasopharyngeal aspirates on admission were assessed by rapid immunofluorescent antigen detection for influenza A and B, parainfluenza types 1, 2, and 3, respiratory syncytial virus, and adenovirus, and were cultured for conventional respiratory pathogens on Mardin Darby Canine Kidney, LLC-Mk2, RDE, Hep-2, MRC-5, and fetal rhesus kidney (FRhK-4) cell lines. RT-PCR for SARS coronavirus was done directly on all clinical samples. Briefly, total RNA from clinical samples was reverse transcribed with random hexamers and cDNA was amplified with primers 5′TACACACCTCAGCGTTG-3′and 5′-CACGAACGTGACGAAT-3′.3 For real-time quantitative PCR assays, cDNA was amplified in an SYBR Green I fluorescence reactions (Roche, Mannheim, Germany) as described.13 Briefly, 20 μL reaction mixtures containing 2 μL cDNA, 3.5 mmol/L magnesium chloride, and 0.25 μmol/L of the same forward and reversed primers as the reaction mixtures were thermal-cycled by a Light cycler (Roche, Mannheim; 95°C, 10 min followed by 50 cycles of 95°C, 10 min; 57°C, 5 s; 72°C, 9 s). Plasmids with the target sequence were used to generate the standard curve. At the end of the assay, PCR products (182 bp) were subjected to a melting curve analysis (65–95°C, 0.1°C/s) to find out the specificity of the assay. The acute and convalescent sera were tested in parallel for SARS-associated coronavirus IgG, with SARS-associated-coronavirus-infected Vero cells fixed in acetone in an indirect immunofluorescent format.
We investigated blood, sputum or endotracheal aspirates, and urine bacteriologically, as clinically indicated. All patients had sepsis work up on admission and if fever recurred. Stools were sent for routine bacteriological culture, Clostridium difficile cytotoxin assay, and examined for parasites in selected patients.
All patients were treated with 1.2 g intravenous amoxicillin-clavulanate every 8 h, and 500 mg oral azithromycin daily. In patients with a known penicillin allergy, we administered 500 mg oral levofloxacin every 24 h. As soon as the diagnosis of SARS was established, 8 mg/kg intravenous ribavirin every 8 h for 14 days, and a tailing regimen of hydrocortisone (starting dose 200 mg intravenously every 8 h) over 10 days, followed by oral prednisolone for 11 days (1 mg/kg for 5 days, 0.5 mg/kg for 3 days, and 0.25 mg/kg for 3 days) were given. We used pulses of methylprednisolone 500 mg intravenously daily for two or three doses if patients worsened, with increasing shortness of breath, oxygen desaturation, and radiological worsening. All HBsAg-positive patients were given 100 mg oral lamivudine daily while taking corticosteroids.
Statistical analysis
We compared risk factors associated with the development of ARDS by Fisher's exact test for categorical variables and Student's t test for continuous variables. Significant risk factors identified on univariate analyses were further analysed by multiple logistic regressions to identify independent risk factors associated with the development of ARDS. We took p<0.05 to be significant. We used SPSS (version 11.0) for all analyses.
Role of the funding source
The sponsors of the study had no role in the study design, data collection, data analysis, data interpretation, or in the writing of the report.
Results
Of the 75 patients, 71 (95%) were ethnic Chinese, and the remainder were Filipino. The male-to-female ratio was one to 0.92, and mean age was 39.8 (SD 12.2) years. Five patients were smokers. Underlying diseases were identified in 13 patients, including nine patients positive for HBsAg with no stigmata of chronic liver disease and normal liver function tests. The clinical symptoms on admission included fever in 75 (100%) patients, chills in 49 (65%), rigors in 42 (56%), myalgia in 51 (68%), cough in 22 (29%), sore throat in eight (11%), shortness of breath in three (4%), headache in 11 (15%), dizziness in three (4%), and diarrhoea in one (1%).
Initial chest radiograph was abnormal in 53 (71%) patients; involvement was confined to one lung zone in 37 (49%) and was multizonal in 16 (21%). Lower-zone infiltrates or consolidation occurred in 45 (60%) patients. Initial high-resolution CT was done in 33 (44%) patients in whom the initial chest radiographs were normal, equivocal, or atypical. Of these 33 patients, 18 (55%) had abnormalities confined to one lobe. Multilobar involvement was seen in 15 (46%) patients. Focal ground-glass opacification was the only type of abnormality in eight (24%) patients. 12 (36%) patients had consolidation only, and 13 (39%) had both types of infiltrates.
On haematological and biochemical investigation, anaemia was detected in six (8%), leucopenia in five (7%), severe lymphopenia of less than 1X109/L in 56 (75%), and thrombocytopenia in 28 (37%). Raised values were seen for alanine aminotransferase (42–343 U/L), aspartate aminotransferase (39–302 U/L), and creatinine kinase (176–1466 U/L) in 22 (29%), 24 (32%), and 27 (36%) patients, respectively. The median lymphocyte counts decreased from 0.8X109/L (IQR 0.6–1.1) on admission to 0.6X109/L (0.5–0.9), 0.4X109/L (0.3–0.5), and 0.4X109/L (0.3–0.6) at days 7, 14, and 21, respectively.
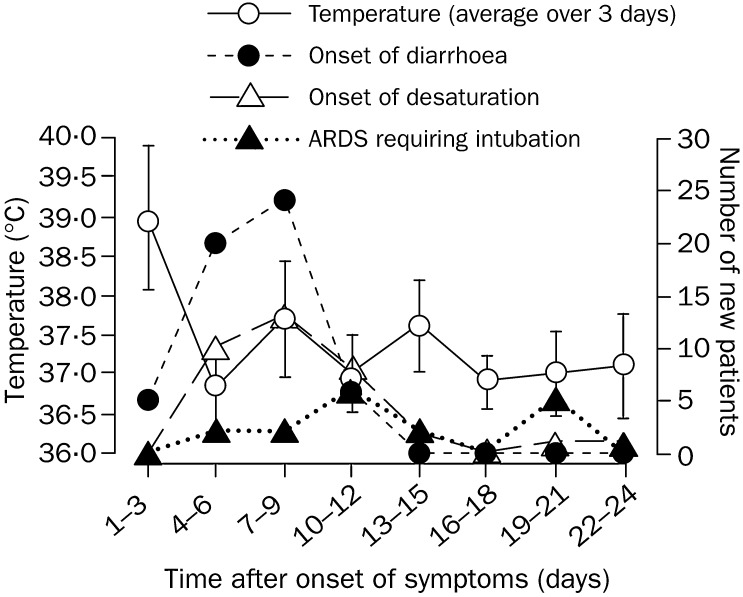
In terms of disease progression, all except one patient became afebrile within 48 h with the standard treatment protocol, but the fever recurred in 64 (85%) patients at a mean of 8.9 days (SD 3.1). Only ten of these patients had positive findings on sepsis work up: three had Stenotrophomonas maltophilia bacteraemia, four had clinical evidence of catheter-related sepsis, and three had nosocomial pneumonia due to Klebsiella pneumoniae (in two) and Escherichia coli (one). All these septic episodes responded to the appropriate antimicrobial treatment and removal of infected catheters. In the remaining 54 patients, fever recurred after a mean of 8.0 (2.1) days, which was unlikely to be caused by hospital-acquired infection. Between days 13 and 15, 17 (23%) patients developed another episode of fever (figure 1 ).
Figure 1.
Temporal clinical profiles in 75 patients with SARS
Mean (SD) are presented.
Watery diarrhoea developed in 55 (73%) patients, with onset at a mean of 7.5 (2.3) days. The rate of diarrhoea peaked at a mean of 8.7 (2.3) days, with a maximum frequency of 6.3 (3.5) times daily (figure 1). Work up for diarrhoeal pathogens, including C difficile cytotoxin, was negative in all these patients. The mean duration of diarrhoea was 3.9 (2.3) days. Simultaneous occurrence of fever and diarrhoea occurred in 24 (32%) patients. Concomitant fever, diarrhoea, and radiological worsening occurred in 16 (21%) patients. Improvement of diarrhoea occurred in all patients by day 13.
Radiological worsening was noted in 60 (80%) patients at a mean of 7.4 (2.2) days: 34 (45%) developed shifting of radiological lesions, evidenced by improvement of original lesions followed by the appearance of new lesions (figure 2 ); worsening of original lesions with or without development of new lesions was noted in the remaining 26 (35%) patients. Overall, 46 (61%) patients subsequently improved, 11 (15%) had remained static at the time of writing, and 18 (24%) further progressed into a diffuse ground-glass appearance at a mean of 12.0 (4.4) days. Of the 18 patients with diffuse ground-glass changes, 15 developed ARDS. Among all 75 patients, nine (12%) developed spontaneous pneumomediastinum during follow-up. The characteristic shifting of radiological changes is illustrated in figure 2.
Figure 2.
Chest radiographs and high-resolution CT scans from two SARS patients
A Man aged 34 years admitted for high fever and cough. A: Consolidation seen in left upper and middle zones, which progressed maximally at day 7. B: At day 20, resolution of consolidation in the left upper and middle zones but new widespread air-space opacities noted; those in left lung base were confluent. Man aged 32 years, presented with fever, chills, rigors and myalgia, with clear chest radiograph at admission. C: High-resolution CT of thorax shows peripheral subpleural consolidation in medial basal segment of left lower lobe. D: Resolution of original left lower-lobe consolidation at day 18. E: Disease complicated by spontaneous pneumomediastinum.
33 (44%) patients developed arterial oxygen desaturation of less than 90% at room air, at a mean of 9.1 (4.2) days after onset of symptoms (figure 1). 24 (32%) patients required intensive care at a mean of 11.0 (6.4) days, among whom 19 had to be intubated at a mean of 12.9 (6.4) days. 15 (20%) patients progressed to ARDS and required mechanical ventilation. On day 1 of mechanical ventilation for ARDS, the mean PaO2-to-FiO2 ratio was 14.7 kPa (10.8) and the mean APACHE II score was 22.3 (5.8). Time to occurrence of ARDS showed a bimodal pattern, with one peak at 11.0 days and another peak at 20.0 days (figure 1). Seven patients developed hospital-acquired infection during their stay in the intensive-care unit, including hospital-acquired pneumonia in three, meticillin-resistant Staphylococcus epidermidis bacteraemia in one, and clinical sepsis in three, without positive cultures.
On univariate analysis, the risk factors associated with ARDS requiring ventilatory support and intensive care were age, male sex, chronic hepatitis B virus carriage, raised creatinine, and recurrence of fever (table 1 ). Lymphocyte counts of ARDS patients on days 7, 14, and 21 did not differ significantly from those in non-ARDS patients. On multivariate analysis, only age and chronic hepatitis B virus infection were significant risk factors (table 2 ).
Table 1.
Risk factors associated with development of ARDS requiring ventilatory support and intensive care
| ARDS (n=15) | No ARDS (n=60) | p | |
|---|---|---|---|
| Mean (SD) age (years) | 48.5 (12.6) | 37.3 (11.3) | 0.002 |
| Male/female ratio | 11/4 | 25/35 | 0.042 |
| Underlying illnesses | 9 (60%)* | 4 (7%) | <0.001† |
| Chronic hepatitis B virus infection | 6 (40%) | 3 (5%) | 0.001 |
| Mean (SD) duration of symptoms to admission (days) | 2.6 (1.1) | 2.38 (1.2) | 0.51 |
| Mean (SD) initial haemoglobin concentration (g/L) | 135 (21) | 134 (12) | 0.79 |
| Mean (SD) initial total peripheral white blood cell count (.109/L) | 7.1 (2.1) | 6.1 (2.1) | 0.09 |
| Mean (SD) initial lymphocyte count (.109/L) | 1.1 (0.9) | 0.9 (0.4) | 0.19 |
| Mean (SD) initial platelet count (.109/L) | 163 (56) | 167 (41) | 0.77 |
| Mean (SD) initial creatinine (μmol/L) | 94.5 (11.1) | 86.1 (14.6) | 0.004 |
| Mean (SD) initial ALT (U/L) | 47.8 (27.5) | 35.9 (45.2) | 0.33 |
| Mean (SD) initial CPK | 327.1 (367.7) | 161.5 (125.9) | 0.11 |
| Mean (SD) initial LDH | 482.6 (242.9) | 384.8 (119.8) | 0.25 |
| NPA RT-PCR positive at diagnosis | 5 (33%) | 19 (31.7%) | 0.77 |
| Mean (SD) day of antibody seroconversion after onset of symptoms | 20.0 (5.5) | 19.9 (4.9) | 0.94 |
| Apparently normal chest radiograph on admission‡ | 4 (27%) | 18 (30%) | 1.0 |
| Multilobar involvement on chest radiograph on admission | 5 (33%) | 11 (18%) | 0.29 |
| Diarrhoea | 12 (80%) | 43 (72%) | 0.75 |
| Recurrent fever | 13 (87%) | 41 (68%) | 0.21 |
ALT=alanine aminotransferase. CPK=creatinine phosphokinase. LDH=lactic dehydrogenase. NPA=nasopharyngeal aspirate.
Three patients had chronic active hepatitis B, one had uterine fibroid.
SARS established by clinical features plus high-resolution CT findings.
Six patients had chronic active hepatitis B infection, one had carcinoma of ovary, one had diabetes mellitus, and one had asthma.
Table 2.
Independent risk factors predicting development of ARDS by multivariate analysis
| Adjusted odds ratio (95% CI) | p | |
|---|---|---|
| Independent predictive factors | ||
| Age-groups (years) | ||
| 21–40 | 1.0 | .. |
| 41–60 | 4.3 (0.9–20.0) | 0.06 |
| 61–80 | 28.0 (3.1–253.3) | 0.003 |
| HBsAg-positive patients | 18.0 (3.2–101.3) | 0.001 |
The mean length of stay for 75 patients was 22.1 (3.1) days, whereas for the 15 patients who developed ARDS, the mean length of stay was 26.8 days at the time of writing. Five patients died during the study period, of whom two, aged 79 and 64 years, had succumbed to acute myocardial infarction on days 13 and 17, respectively. One patient died of clinical sepsis on day 23. Another two patients died of clinical sepsis and ARDS on days 24 and 25, respectively. 27 (36%) of patients were discharged home or transferred to a rehabilitation facility. One patient was transferred to a specialised obstetric unit for urgent delivery of a baby at 32 weeks’gestation. For the 42 patients who remained in the hospital, 13 were treated in intensive care for ARDS (table 3 ).
Table 3.
Outcomes in SARS patients at the time of writing
| n=75 | |
|---|---|
| Outcome | |
| Death* | 5 (7%) |
| Convalescence at home or at rehabilitation facility | 27 (36%) |
| Transfer to special obstetric unit | 1 (1%) |
| Hospital admission | |
| In general ward | 29 (39%) |
| In intensive-care unit for ARDS | 13 (17%) |
Two patients died of acute myocardial infarction, one of clinical sepsis, and two of clinical sepsis and ARDS
IgG seroconversion was documented in 70 (93%) patients at mean of 20 (5.1) days (figure 3 ). SARS-associated coronavirus RNA was detected in nasopharyngeal aspirates by RT-PCR in 24 (32%) of 75 patients at initial presentation (mean 3.2 [1.3] days after onset) and in 51 (68%) at day 14. In stool samples collected later in the illness (a mean of 14.2 [2.2] days after onset), viral RNA was detected in 65 (97%) of 67. Similarly, viral RNA was detected in 31 (42%) of 74 urine samples collected at a mean of 15.2 (1.7) days after onset of symptoms.
Figure 3.
Kinetics of IgG seroconversion to SARS-associated coronavirus
Cumulative data on earliest time to seroconversion is presented.
The 20 patients initially documented to have SARS-associated coronavirus RNA in the nasopharyngeal aspirates on RT-PCR were serially followed up with sequential samples; the virological profile is shown in table 4 . Quantitative RT-PCR of the nasopharyngeal aspirates showed an inverted V pattern, with mean geometric viral loads of 2.3X105 copies per mL, and 1.9X107 copies per mL, and 9.8X104 copies per mL on days 5, 10, and 15, respectively, after onset of symptoms (figure 4 ).
Table 4.
Subsequent analysis of clinical samples of 20 patients with initial RT-PCR-positive nasopharyngeal aspirates and antibody seroconversion to SARS-associated coronavirus
| Time after onset of symptoms (days; n=20) |
|||||
|---|---|---|---|---|---|
| 10 | 13 | 16 | 19 | 21 | |
| Sample (positivity rate) | |||||
| Nasopharyngeal aspirate | 19 (95%) | 18 (90%) | 18 (90%) | 15 (75%) | 9 (47%)* |
| Stool | 20 (100%) | 20 (100%) | 19 (95%) | 12 (80%)† | 10 (67%)† |
| Urine | 10 (50%) | 9 (45%) | 7 (35%) | 6 (30%) | 4 (21%)* |
in 19 patients.
In 15 patients
Figure 4.
Sequential quantitative RT-PCR for SARS-associated coronavirus in nasopharyngeal aspirates of 14 SARS patients
Discussion
Studies on SARS have generally been retrospective or limited to the description of the initial clinical, haematological, radiological and microbiological findings. The patients we studied, however, were residents of a housing estate placed under closed surveillance by the Department of Health soon after identification of the outbreak. All residents underwent frequent health checks, and symptomatic patients were admitted to hospital soon after the onset of symptoms and, thus, were admitted early in the course of the illness. Therefore, we were able to do a prospective study in a large cohort of patients infected in one community outbreak of SARS who were epidemiologically linked, and of whom most had virologically confirmed SARS-associated coronavirus.
The clinical progression of SARS was mostly uniform in our cohort, with a tri-phasic pattern. Week 1 was characterised by fever, myalgia, and other systemic symptoms that generally improve after a few days. The increasing viral load during this phase suggests that the symptoms are largely related to the effect of viral replication and cytolysis. As the disease progressed into week 2, the patients frequently had recurrence of fever, onset of diarrhoea, and oxygen desaturation. Strikingly, nearly half the patients had shifting radiographic shadows. If viral-induced damage was the primary pathological mechanism, such a flitting pattern of radiological change is difficult to explain. The timing of the IgG seroconversion, which starts on day 10, seems to correlate with falls in viral load, which occurs from between day 10 and 15, despite the use of pulse methylprednisolone. Severe clinical worsening also occurs at this time, which cannot be explained by uncontrolled viral replication. This finding is supported by the progressive decrease in rates of viral shedding from nasopharynx, stool, and urine from day 10 to 21 after onset of symptoms in the 20 patients who underwent prospective follow-up with RT-PCR. Taken together, these findings suggest that the lung damage at this phase is related to immunopathological damage as a result of an overexuberant host response, rather than uncontrolled viral replication. 20% of patients in this cohort progressed to the third phase, characterised by ARDS necessitating ventilatory support. Inevitably, several patients developed nosocomial sepsis during this phase of end-organ damage and severe lymphopenia.
In terms of pathogenesis, in pulmonary reovirus infection in athymic mice, a lower plaque-forming value of 106 is associated with pathological changes of bronchiolitis obliterans organising pneumonia, whereas a higher inoculum of 107 is associated with ARDS.14 To lessen the risk of progression to the chronic phase of ARDS, an effective antiviral to reduce the viral load may be important. At the time of writing, no antiviral is reported to be clinically effective for the treatment of this novel coronavirus. Ribavirin has broad-spectrum antiviral activities and is effective for the treatment of fulminant hepatitis in mice caused by the mouse hepatitis coronavirus.15 Although the inhibitory activity of ribavirin against mouse hepatitis coronavirus is weak, ribavirin can decrease the release of proinflammatory cytokines from the macrophages of mice. It also switched the immune response of the mice from a T-helper-2 to a T-helper-1 response. Thus, irrespective of its antiviral role, ribavirin may act as an immunomodulator. An effective antiviral agent is needed because decreasing the initial cytolytic damage and viral load in the first phase may in turn result in decreased immunopathological damage during the second phase. Since a notable proportion of our patients developed ARDS, the role of immunologically directed strategies, such as corticosteroids, intravenous immunoglobulin, IgM-enriched immunoglobulin, convalescent plasma, and the antitumour necrosis factor thymosin, deserve further investigation.
Unexpectedly, chronic hepatitis B infection was an important independent risk factor for progression to ARDS. This finding may also explain a higher rate of death among young Chinese patients because of the high rate of chronic hepatitis B infection in Southern China. The finding is important because in all our patients, lamivudine was given as prophylaxis while the patients were taking corticosteroids. We did not assess the viral load for hepatitis B virus DNA since the liver function tests were normal with no clinical stigmata of chronic liver diseases. Thus these patients’poor outcome cannot be explained by uncontrolled hepatitis activity. An unknown immune defect in chronic hepatitis B carriers may account for their poor ability to control the coronavirus infection or the associated immunopathological damage. Co-infection with SARS coronavirus in hepatitis B carriers may predict a worse prognosis. The option of prophylaxis with intranasal interferon alfa could be investigated in household contacts and health-care workers, especially in those with chronic hepatitis B virus carriage, because this approach is effective in other human coronavirus infections.16
The case definition of SARS is clinical and rather non-specific in the absence of epidemiological history of contact. We showed that IgG seroconversion has 93% sensitivity at day 28, even despite corticosteroid treatment. In this case, IgG isotype-specific antibody to the SARS coronavirus was tested for. If antibody to all immunoglobulin classes is assayed for, seroconversion will probably be detected earlier. Although viral RNA detection in the nasopharyngeal aspirate has a sensitivity of only 32% at presentation, testing of multiple nasopharyngeal and faecal samples increased the sensitivity of the RT-PCR assay.
The presence of virus in the stool is an important finding because it suggests the possibility of oral-faecal transmission. The epidemiological investigation of the Amoy Gardens SARS outbreak suggested that the outbreak was caused by a faulty sewage system.8 Diarrhoea seemed more prominent in our cohort of patients than previously reported,3, 7 and the severe watery diarrhoea in these patients presented a challenge to health-care workers for infection control. Whether this apparent change in the clinical presentation is related to the difference in the route of infection or a mutation in the virus is still conjectural. Importantly, the mortality rate of 6.7% we reported is higher than the previously reported figure of 3.5% at day 21.6
We noted the absence of a relation between the high rate of spontaneous pneumomediastinum unrelated to intubation and positive-pressure ventilation. This phenomenon is rarely reported in advanced cytomegalovirus pneumonia,17 and influenza bronchiolitis,18 whereas spontaneous pneumothorax is commonly reported in Pneumocystis carinii, and Staphylococcus aureus pneumonia. The initial radiographic lesions in SARS were pleural based.6 In patients in whom the initial consolidation is abutting on to the mediastinum, adhesions and cyst formation might occur at the interface between the mediastinal pleura and the pulmonary pleura. Any rupture of these cysts will result in spontaneous pneumomediastinum. Alternatively, a diffuse peripheral pneumonic changes followed by pleural adhesion may occur over the parietal pleura of the chest walls, which leaves the mediastinal sites as the area in which rupture of cyst can occur. This will also create the necessary setting for spontaneous pneumomediastinum to occur without spontaneous pneumothorax.
RT-PCR on respiratory and faecal samples, together with serology, can confirm the diagnosis of SARS-associated coronavirus infection in most SARS patients. The progression of the disease to respiratory failure might not be associated with uncontrolled viral replication, but may, in fact, be immunopathological in nature.
Acknowledgments
Acknowledgments
We thank E K Yeoh of the Hong Kong Government for facilitating this study; Klaus Stöhr and WHO for initiating and coordinating the information exchange between members of the WHO SARS Laboratories network; and the staff of the Department of Microbiology, Queen Mary Hospital, and of the Department of Medicine and Intensive Care Unit, United Christian Hospital, for technical assistance and management of patients. Research funding was received from from the National Institute of Allergy and Infectious Diseases, USA (public health research grant A195357), the Wellcome Trust (grant GR067072/D/02/Z), University of Hong Kong and the Hospital Authority of Hong Kong.
Contributors
J S M Peiris and K Y Yuen are co-principal investigators, jointly wrote the report, and supervised the virological and clinical component of the study. C M Chu, V C C Cheng, K S Chan, I F N Hung, K I Law, B Y F Tang, J S C Ng, and W L Ng were involved in collection and analysis of the clinical data. C S Chan and T Y W Hon were involved in radiological analysis. L L M Poon, K H Chan, and Y Guan did the quantitative PCR and other virology assays. R W M Lai coordinated the microbiological investigations in United Christian Hospital.
Members of the HKU/UCH SARS Study Group
S W Kwan, K F Lo, A M Y Fung, I M T Chu, W T Hui, H K Leung, W H Seto, Department of Microbiology, Queen Mary Hospital; S Y Lam, P C Y Woo, S K P Lau, W Luk, H Y Ng, L J Zhang, C Y Cheung, O K Wong, W Cheung, G Tse, Department of Microbiology, University of Hong Kong; P W Ng, T C Sim, L S Lau, V Chan, W S Leung, J T M Chan, K L Lee, Y S Poon, E Chow, C Y Leung, F L Lau, W L Tsoi, A C H Choi, C N C Chan, M F Leung, C Y Tse, United Christian Hospital.
Conflict of Interest statement
None declared.
References
- 1.Severe Acute Respiratory Syndrome (SARS) multi-country outbreak—update 34. http://www.who.int/csr/don/2003_04_19/en/ (accessed May 5, 2003).
- 2.Centers for Disease Control and Prevention SARS coronavirus sequencing. http://www.cdc.gov/ncidod/sars/sequence.htm (accessed May 5, 2003).
- 3.Peiris JSM, Lai ST, Poon LLM. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ksiazek TG, Erdman D, Goldsmith CS. A novel coronavirus associated with severe acute respiratory syndrome. http://content.nejm.org/cgi/reprint/NEJMoa030781v3.pdf (accessed at May 5, 2003). [DOI] [PubMed]
- 5.Poutanen SM, Low DE, Henry B. Identification of severe acute respiratory syndrome in Canada. http://content.nejm.org/cgi/reprint/NEJMoa030634v3.pdf (accessed May 5, 2003). [DOI] [PubMed]
- 6.Lee N, Hui D, Wu A. A major outbreak of severe acute respiratory syndrome in Hong Kong. http://content.nejm.org/cgi/reprint/NEJMoa030685v2.pdf (accessed May 5, 2003). [DOI] [PubMed]
- 7.Tsang KW, Ho PL, Ooi GC. A cluster of cases of severe acute respiratory syndrome in Hong Kong. http://content.nejm.org/cgi/reprint/NEJMoa030666v3.pdf (accessed May 5, 2003). [DOI] [PubMed]
- 8.Atypical pneumonia. http://www.info.gov.hk/dh/ap.htm (accessed May 5, 2003).
- 9.Ho W. Guideline on management of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1313–1315. doi: 10.1016/S0140-6736(03)13085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HA guidelines on severe acute respiratory syndrome. http://www.ha.org.hk/sars/guidelines/index.html (accessed May 5, 2003).
- 11.Bernard GR, Artigas A, Brigham KL. The American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 12.Knaus WA, Draper EA, Wagner DP. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 13.Poon LLM, Wong OK, Luk W. Rapid diagnosis of a coronavirus associated with severe acute respiratory syndrome (SARS) http://www.clinchem.org/cgi/content/full/49/4/DCI (accessed May 5, 2003). [DOI] [PMC free article] [PubMed]
- 14.Majeski EI, Harley RA, Bellum SC. Differential role for T cells in the development of fibrotic lesions associated with reovirus 1/L-induced bronchiolitis obliterans organizing pneumonia versus acute respiratory distress syndrome. Am J Respir Cell Mol Biol. 2003;28:208–217. doi: 10.1165/rcmb.4891. [DOI] [PubMed] [Google Scholar]
- 15.Ning Q, Brown D, Parodo J. Ribavirin inhibits viral-induced macrophage production of TNF, IL-1, the procoagulant fg12 prothrombinase and preserves Th1 cytokine production but inhibits Th2 cytokine response. J Immunol. 1998;160:3487–3493. [PubMed] [Google Scholar]
- 16.Turner RB, Felton A, Kosak K. Prevention of experimental coronavirus colds with intranasal alpha-2b interferon. J Infect Dis. 1986;154:443–447. doi: 10.1093/infdis/154.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ollif JF, Williams MP. Radiological appearances of cytomegalovirus infections. Clin Radiol. 1989;40:463–467. doi: 10.1016/s0009-9260(89)80245-4. [DOI] [PubMed] [Google Scholar]
- 18.Tutor JD, Montgomery VL, Eid NS. A case of influenza bronchiolitis complicated by pneumomediastinum and subcutaneous emphysema. Pediatr Pulmonol. 1995;19:393–395. doi: 10.1002/ppul.1950190614. [DOI] [PubMed] [Google Scholar]