Summary
The causative agent of severe acute respiratory syndrome (SARS) has been identified as a new type of coronavirus. Here, we have investigated the ability of adenoviral delivery of codon-optimised SARS-CoV strain Urbani structural antigens spike protein S1 fragment, membrane protein, and nucleocapsid protein to induce virus-specific broad immunity in rhesus macaques. We immunised rhesus macaques intramuscularly with a combination of the three Ad5-SARS-CoV vectors or a control vector and gave a booster vaccination on day 28. The vaccinated animals all had antibody responses against spike protein S1 fragment and T-cell responses against the nucleocapsid protein. All vaccinated animals showed strong neutralising antibody responses to SARS-CoV infection in vitro. These results show that an adenoviral-based vaccine can induce strong SARS-CoV-specific immune responses in the monkey, and hold promise for development of a protective vaccine against the SARS causal agent.
Events of the past year have shown that a new and deadly disease has become epidemic. The syndrome, called severe acute respiratory syndrome (SARS), has spread to many countries on several continents and has taken its toll in illness and death. Through the efforts of an international consortium of laboratories, the causative agent of SARS was identified as a new type of coronavirus. In less than 2 months after the SARS-associated coronavirus (SARS-CoV) was identified, the genomic sequences of two independently isolated viruses were completed.1 Here, we report our initial efforts to develop a SARS-CoV vaccine. We generated three adenoviral-based vectors that express codon-optimised SARS-CoV strain Urbani structural antigens, including the spike protein S1 fragment, membrane protein, and nucleocapsid protein. We constructed adenoviral vectors in which early regions 1 and 3 had been deleted by use of Cre-lox recombination. Codon optimisation and gene synthesis were done with the UpGene codon optimisation algorithm software (http://www.vectorcore.pitt.eduupgene.html). Combinations of spike, membrane, and nucleocapsid proteins have been tested previously as vaccines against different strains of coronavirus. In particular, induction of high concentrations of virus-specific antibodies against transmissible gastroenteritis requires stimulation by at least two viral proteins, and the best responses are induced by a combination of spike and nucleocapsid proteins.2
Here, we immunised six rhesus macaques intramuscularly on day 0 with a combination of the three Ad5-SARS-CoV vectors (1×1011 viral particles each); two control animals were immunised with the same amount of empty adenoviral vector. On day 28, animals received a second vaccination with the same regimen. We monitored all animals for T-cell and antibody responses. The rhesus macaque was chosen for these studies because it is a highly relevant translational model for people. Immunological assays including the ELISPOT assay have been well characterised and validated in this model.
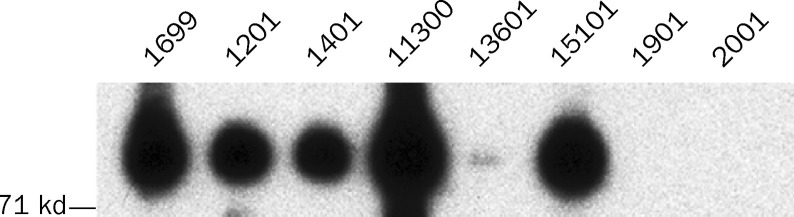
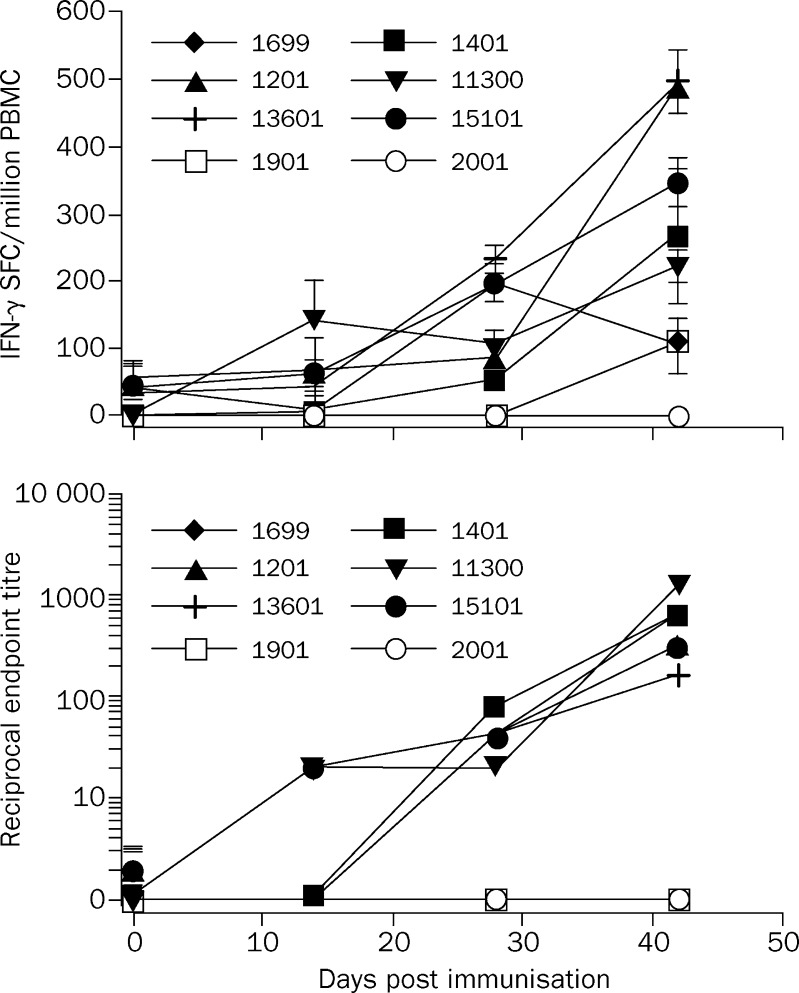
We did western blot analysis directed toward the spike protein SI fragment—the most likely to elicit neutralising responses—on serum samples from immunised animals. We transfected HEK293 cells with expression plasmids encoding the SI fragment or a control empty plasmid, and cells were harvested 48 h later. Lysates were separated by gel electrophoresis and transferred to a polyvinylidine difluoride (PVDF) membrane. Antibodies against the SI fragment were detected by immunoprobing with immunised animal serum (1 in 1000), followed by detection with horseradish peroxidase-conjugated goat antimonkey IgG (H+L). Western blot analysis detected antibodies against the SI fragment in all six immunised animals but not in either control animal at 6 weeks after vaccination (figure 1 ). To investigate T-cell responses in immunised monkeys, we did ELISPOT assays to measure production of interferon γ on peripheral blood mononuclear cells obtained at intervals after vaccination as described.3 We used 15-mer overlapping peptides as antigens, which represented the complete sequence of the SARS-CoV strain Urbani nucleocapsid protein. We chose the nucleocapsid protein because it is a representative antigen for the T-cell response in this vaccine setting. All animals receiving intramuscular injections of Ad5-SARS-CoV vaccine showed nucleocapsid-specific T-cell responses in response to immunisation (figure 2 ). The intensity of the response varied among animals, but was generally largest after the booster vaccination, with a peak frequency of about one nucleocapsid-specific T cell per 2000 freshly isolated peripheral blood mononuclear cells (monkeys 13601 and 1201; figure 2).
Figure 1.
Western blot analysis of immunised (1699, 1201, 1401, 11300, 13601 and 15101) and control (1901 and 2001) monkeys
Bands indicate presence of S1-specific antibodies in serum.
Figure 2.
Nucleocapsid-specific T-cell responses (upper) and neutralising capacity (lower) of serum samples after vaccination
Immunised animals represented by black symbols, controls by white symbols. (Upper) ELISPOT analysis 24 h after monkey peripheral blood mononuclear cells (PBMC) were incubated with pools of nucleocapsid-specific peptides and interferon-γ (IFN-γ) spot-forming cells (SFC) were counted. Data are mean (SE) of triplicate determinations after subtraction of background responses. (Lower) Detection of virus-specific neutralising antibodies in serum by inhibition of E6 Vero cell lysis by SARS-CoV strain Urbani in a microneutralisation assay. Data for 1699 and 1201 overlap at all time points.
Finally, we tested the neutralising capacity of serum samples from immunised monkeys in an in-vitro micro-neutralisation assay. All procedures were done at biosafety level 3. We diluted heat-inactivated serum samples serially and seeded them in triplicate into 96-well plates. We then added about 37 plaque forming units of SARS-CoV (Urbani strain). After incubation at 37°C for 1 h, we added 200 000 E6 Vero cells and incubated the plates for a further 3–4 days. Cells were then stained with crystal violet-formaldehyde for 1 h. The neutralisation titre was measured as the reciprocal of the highest serum dilution that completely inhibited E6 Vero cell lysis in at least two of the three triplicate wells. Serum samples from vaccinated animals but not from control animals showed strong neutralising capacity against SARS-CoV after immunisation, some of which appeared even at early time points (figure 2). Notably, three animals in the test group (1699, 1201, and 11300) had low concentrations of pre-existing neutralising antibody to Ad5 because of previous exposure to the Ad5 vector (data not shown), yet they responded in a similar manner as non-immune animals do to vaccination. These findings support use of such an adenoviral-based vaccine platform in people even if they have pre-existing adenoviral immunity.
Our results show that an adenoviral-based vaccine can induce SARS-CoV-specific T-cell and virus neutralising antibody responses. It is essential to determine whether patients convalescing from SARS have similar responses, since this could suggest that such vaccine-induced responses are protective. The capacity for our immunisation strategy to protect from infection will require challenge tests in a clinically relevant SARS disease animal model. Use of such a model will also be important to exclude any potential for vaccine-induced immunopathology, as seen in the feline infectious peritonitis virus model.4 A non-human primate challenge model of SARS has been described,5 although its suitability for vaccine testing remains to be determined.
Acknowledgments
Acknowledgments
This work was supported by National Heart Lung and Blood Institute, Program of Excellence in Gene Therapy supplement Grants U01 HL66949–01S1 to A Gambotto. The authors thank K Okada and H Sun for assistance with adenoviral preparation. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or in the writing of the report.
Contributors
W Gao and L D'Aiuto generated the codon-optimised SARS-CoV proteins and recombinant adenoviral vectors, and did the western blot analyses. W Bellini and A Tamin did the SARS-CoV microneutralisation assay. S Barratt-Boyes and A Soloff were responsible for immunisations and the interrferon-γ ELISPOT T-cell assay. P Robbins and E Nwanegbo were responsible for the adenoviral neutralising assay. A Gambotto was the principal investigator; he conceived and coordinated the study. A Gambotto had full access to the data and had final responsibility for the decision to submit for publication.
Conflict of interest statement
None declared.
References
- 1.Rota PA, Oberste MS, Monroe SS. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 2.Anton IM, Gonzalez S, Bullido MJ. Cooperation between transmissible gastroenteritis coronavirus (TGEV) structural proteins in the in vitro induction of virus-specific antibodies. Virus Res. 1996;46:111–124. doi: 10.1016/S0168-1702(96)01390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown K, Gao W, Alber S, etal. Adenovirus-transduced dendritic cells injected into skin or lymph node prime potent siv-specific t-cell immunity in monkeys. J Immunol (in press). [DOI] [PubMed]
- 4.Weiss RC, Scott W. Antibody-mediated enhancement of disease in feline infectious peritonitis: comparisons with dengue hemorrhagic fever. Comp Immunol Microbiol Infect Dis. 1981;4:175–189. doi: 10.1016/0147-9571(81)90003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fouchier RA, Kuiken T, Schutten M. Aetiology: Koch's postulates fulfilled for SARS virus. Nature. 2003;423:240. doi: 10.1038/423240a. [DOI] [PMC free article] [PubMed] [Google Scholar]