Abstract
Objectives
To describe the pathogenesis, clinical presentation, cerebrospinal fluid findings and outcome of Aspergillus meningitis, meningoencephalitis and arachnoiditis.
Methods
A case of Aspergillus meningitis is described. A comprehensive review of the English-language literature was conducted to identify all reported cases of Aspergillus meningitis described between January 1973 and December 2011.
Results
Ninety-three cases (including the one described herein) of Aspergillus meningitis were identified. Fifty-two (55.9%) were in individuals without any predisposing factor or known causes of immunosuppression. Acute and chronic meningitis was diagnosed in 65.6% of patients and meningoencephalitis in 24.7% of them with the remaining presenting with spinal arachnoiditis and ventriculitis. Cerebrospinal fluid cultures for Aspergillus spp. were positive in about 31% of cases and the galactomannan antigen test in 87%. Diagnosis during life was achieved in 52 patients (55.9%) with a case fatality rate of 50%. The overall case fatality rate was 72.1%.
Conclusions
Aspergillus meningitis may occur in both immunocompetent and immunocompromised patients and run an acute or chronic course. The findings of this systematic review extend the information on this life-threatening infection and could assist physicians in achieving an improved outcome.
Keywords: Aspergillus meningitis, Galactomannan antigen, Diagnosis, Therapy
Central nervous system (CNS) infections are well recognized manifestations of disseminated aspergillosis observed in about 10% of immunocompromised patients and with mortality rates greater than 90%.1, 2 By contrast, Aspergillus meningitis is a more seldomly encountered clinical entity and it is found more frequently in immunocompetent rather than in immunocompromised hosts.3, 4, 5, 6, 7, 8 Information about Aspergillus meningitis is limited and sparse and to our knowledge no review on this topic has been published so far. We present here a case of Aspergillus meningitis, along with a review of published cases since 1973.
Methods
Case reports of Aspergillus meningitis, meningoencephalitis, arachnoiditis and ventriculitis as well as series of CNS aspergillosis were identified through a search of PubMed and Scopus databases of the English literature, and the reference lists were reviewed for additional cases. Research was conducted from the year 1973 through 2011. Used research terms included “Aspergillus meningitis”, “cerebral aspergillosis”, “central nervous system aspergillosis”, “Aspergillus arachnoiditis”, “mycotic meningitis”. For the purpose of this review a case of meningitis or meningoencephalitis caused by Aspergillus spp. was defined during life as follows: 1) a cerebrospinal culture positive for Aspergillus spp. together with a meningeal or encephalic syndrome; 2) the presence of galactomannan antigen or Aspergillus DNA detected by polymerase chain reaction (PCR) test in the CSF, together with a meningeal syndrome. Post-mortem diagnoses of Aspergillus meningitis were included if the autopsy clearly indicated involvement of the meninges or a picture of meningitis with microscopic identification of Aspergillus hyphae or a positive Aspergillus culture. When inflammation involved the spinal leptomeninges the case was classified as spinal arachnoiditis. Patients were considered immunocompromised if the following conditions were met: 1) HIV/AIDS infection; 2) solid organ transplantation; 3) hematologic diseases with or without bone marrow transplantation; 4) autoimmune diseases treated with steroids or other immunosuppressive drugs; 5) diabetes mellitus; 6) any other condition treated with corticosteroids or immunosuppressive drugs.
Case report
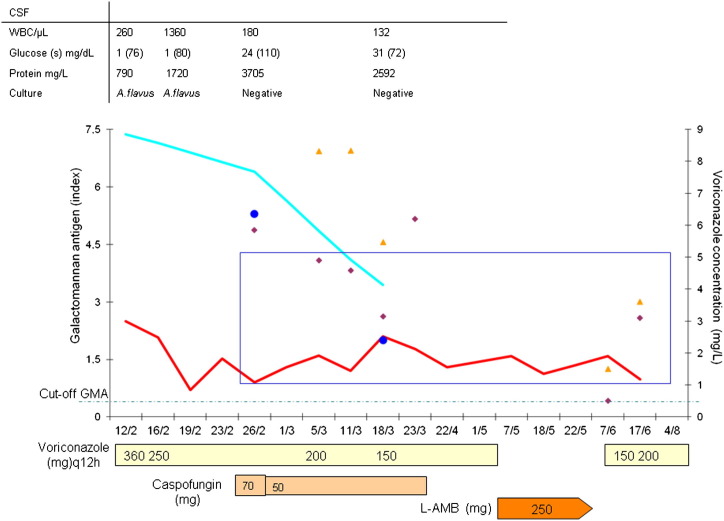
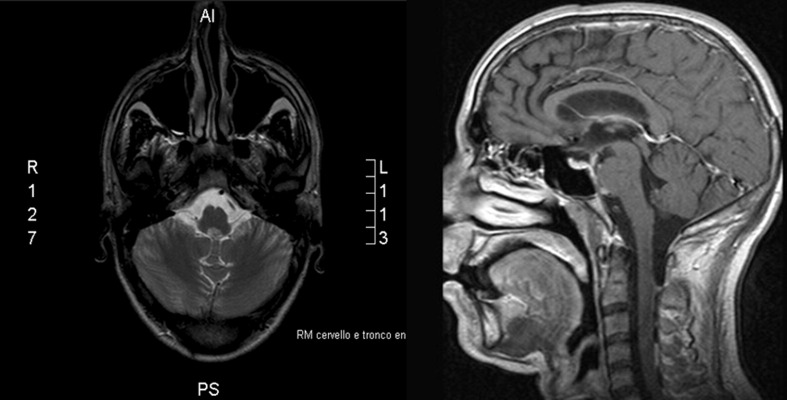
A 34-year-old man was referred to our Infectious Diseases ward on February 9, 2010 from a Neurosurgery Unit where a diagnosis of Aspergillus meningitis had been made (Fig. 1 ). The clinical history was notable for heroin intravenous drug abuse, high alcohol intake, untreated chronic hepatitis C and methadone maintenance therapy (50 mg/day). One month before he was admitted to the Internal Medicine ward of another Hospital to investigate the nature of low back pain, headache and low grade fever (37.5 °C) that had appeared 1 month earlier. Magnetic resonance imaging (MRI) of the brain was negative for parenchimal and meningeal lesions. On the contrary, MRI of the lumbar spine showed abnormal contrast enhancement into the spinal canal between L4 and S1 suggesting an intradural mass lesion conditioning a traction effect on the roots of the cauda equina. A color-doppler echocardiogram showed only a mild mitral regurgitation. Blood and urine cultures were negative as well as a serologic test for HIV. Cerebrospinal fluid (CSF) analysis performed on February 9 is shown in Fig. 1. Gram and Ziehl-Neelsen stains, as well as bacterial and mycobacterial cultures, were negative as was the search for bacterial and Cryptococcus neoformans antigens. Cerebrospinal culture grew Aspergillus flavus that was susceptible to amphotericin B, voriconazole, posaconazole, itraconazole and caspofungin. Aspergillus galactomannan antigen-GM (Platelia Aspergillus, Sanofi Diagnostics Pasteur, Marne-La Coquette, France) was detected both in the CSF and blood with a higher index value in the former (respectively, 7.4 and 2.5). Upon admission to our ward (February 12), the patient had fever (38.5 °C), was alert and complained of frontal headache and photophobia, without neck stiffness. Intravenous treatment with voriconazole was started (6 mg/kg every 12 h (q12h) as loading dose, followed by 4 mg/kg q12h) together with ceftriaxone (2 g q12). Two weeks later, a control brain and spinal MRI showed meningeal enhancement with cysternal distribution especially in the pre-pontine area around the basilar artery, together with endocanalar pathologic enhancement between L4 and S2 (Figure 2, Figure 3 a and b). A concomitant CSF analysis showed a reduction of WBCs (180/μL, 61% PMNs), improvement of glucose levels (24 mg/dL, serum 110 mg/dL) and a striking increase of protein level (3705 mg/dl), whereas, at this time point, CSF culture turned negative. The GM index was 6.36 in the CSF and 0.9 in the peripheral blood. Because of persistent fever, headache and worsening of the radiological picture, caspofungin (70 mg loading dose, 50 mg maintenance dose) was added to the antifungal regimen with discontinuation of the antibiotic therapy. Voriconazole blood and CSF trough concentrations obtained after 2 weeks of therapy were similar (5.85 and 5.86 mg/L, respectively). Therapeutic drug monitoring was arranged 6 and 10 days later and it showed toxic concentrations of the drug that prompted dosage adjustments despite the absence of any clinical or biochemical signs of voriconazole toxicity. Another CSF examination performed on March 18, disclosed an improvement of all parameters (Fig. 1). Repeated MRI of the brain and spine (March, 17) showed the reduction of the pial and cysternal contrast enhancement but a progression of the endocanalar inflammation now involving the segments L3 to S2. After a new evaluation by the neurosurgery consultant, who deemed any procedure unfeasible, the patient was discharged after having received 38 days of voriconazole therapy (total cumulative dosage: 21,200 mg) and one month of caspofungin (total cumulative dosage:1520 mg). The patient was left on maintenance therapy with oral voriconazole at a dosage of 150 mg q12 due to raised ALT levels (199 U/L), the appearance of visual disturbances and persistently elevated trough voriconazole concentrations (6.2 mg/L). At the end of April, the patient was readmitted to our hospital ward because of persistent abnormal liver function test results and visual disturbances that required discontinuation of voriconazole and its substitution with intravenous liposomal amphotericin B (L-AMB, 250 mg/day). He complained of persistent low back pain that was irradiated to both the lower extremities with preserved deep tendon and superficial reflexes. Repeated attempts to obtain CSF samples by lumbar puncture were unsuccessful. Nerve conduction and electromyography studies showed mild sensorimotor bilateral demyelinating polyneuropathy. A new MRI of the brain and spine (performed on May, 17) was substantially unchanged. During the 30-day therapy with L-AMB, GM was evaluated weekly and showed values ranging from 0.9 to 1.59. Because of the patient's drug addiction history, it was decided to resume oral voriconazole therapy since the positioning of a permanent intravenous device for L-AMB infusion on an outpatient basis was judged risky. A dosage of 150 mg every 12 h was started on June 9, showing after a week trough and peak concentrations of 3.4 and 3.6 mg/L, respectively. A new MRI of the brain and spine was performed on August 4, that demonstrated a reduction of pial enhancement along the cervical tract, the conus medullaris and cauda equina with a only a mild volumetric reduction of the endocanalar lumbar abscess. Clinically, the patient was well oriented with a positive bilateral Lasègue sign at the neurologic examination. He was discharged and subsequently lost to follow-up.
Figure 1.
Medication history, clinical course and kinetic of Aspergillus antigen in CSF of our case of Aspergillus flavus meningitis. The dotted line represents the cut-off value of GM. The light blue line is the index on CSF and the red line on plasma. The blue circle represents the CSF levels of voriconazole. The purple diamond and the yellow triangle are respectively the down and peak plasma levels of voriconazole. The blue rectangle denotes the range of expected therapeutic levels of voriconazole.
Figure 2.
Sagittal and coronal T1-weighted gadolinium-enhanced magnetic resonance scan of the brain of our patient with Aspergillus flavus meningitis showing contrast impregnation along the basilar artery in the prepontine cistern.
Figure 3.
Sagittal T2 (a) and gadolinium enhanced T1-weighted (T1W) (b) MRI demonstrate pathologic enhancement and endocanalar pathologic tissue of the L4-S2 tract.
Results
A detailed, chronologically ordered summary of 93 cases of Aspergillus meningitis, chronic meningitis/pachymeningitis, meningoencephalitis, arachnoiditis and ventriculitis including the one presented herein (case 46) is shown in Table 1 . There were 46 women (50%) and 46 men, with a median age of 37 years (range 3–75 years). Diagnosis was made during life in 52 patients (55.9%) and at autopsy in 41 patients. A diagnosis was obtained more frequently during life among immunocompetent patients (69%) in comparison with immunocompromised individuals (39%) (Table 2 ).
Table 1.
Characteristics of patients with Aspergillus meningitis.
| Author, year [Reference] | Age/sex | Risk factor/Underlying disease | Sign and symptoms (time duration)/Time from TX | Syndrome | Diagnosis/methods | CSF characteristics | Aspergillus species | CSF Ag GMN (method) | Antifungal treatment (time duration) | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Meningitis | ||||||||||
| Atkinson & Israel, 19739 | 27/M | None/Sarcoidosis | Headache, blurred vision | Meningitis | L/CSF | WBC 144/μL (PMNs 10%) | Aspergillus fumigatus (CSF) | NA | 5-FLU (3 months) | Alive 2 years after stopping antifungal therapy |
| Feely et al., 197710 | 57/F | Neurosurgery (Trans-sphenoidal Yttrium90 implant)/Acromegaly | Meningeal signs, left hemiparesis/11 months | Meningitis | Pm/Autopsy (purulent basal leptomeningitis + multiple infarcts) | WBC 138/μL (PMNs 96%); proteins 850 mg/L | Aspergillus spp. (autopsy culture) | NA | None | Death after 1 day |
| 37/M | Neurosurgery (Trans-sphenoidal Yttrium90 implant)/Diabetic retinopathy | Fever, stiff neck, headache, blurred vision/9 months | Meningitis | L/Biopsy (tissue adherent to the screws) | WBC 8800/μL (PMNs 90%); protein 330 mg/L | Aspergillus spp. (biopsy) | NA | AMFB (NR)+ removal of implant | Alive | |
| Mohandas et al., 197811 | 38/M | Neurosurgery/Maxillary sinusitis | Meningeal irritation, coma/6 days post-operatively | Meningitis | L/Surgery of fungal granuloma | WBC 100/μL (PMNs 0%); glucose 35 mg/dL; protein 1160 mg/L | Aspergillus spp. (biopsy) | NA | AMFB (7 days) ev + intratechal (1 day) | Death after 7 days |
| Aung et al., 197912 | 22/F | Pregnancy/None | Headache, retrobulbar pain, blurred vision, ophthalmoplegia (22 days after delivery) | Meningitis | L/Biopsy leptomeninges | ND | Aspergillus spp. (biopsy) | NA | Antifungal drugs (not mentioned) | Death after 1 month |
| Beal et al., 198213 | 47/F | None/Sphenoid sinusitis | Frontal headache (5 months); nuchal rigidity, fever, hydrocephalus | Meningitis | L/biopsy sinus | WBC 120/μL (PMNs 63%); glucose 25 mg/dL; protein 620 mg/L | Aspergillus spp. (sinus biopsy) | NA | AMFB (NR) | Alive 2 years later |
| 22/F | Neurosurgery/Medullo-blastoma | Fever (38.8 °C), severe headache, meningismus 12 days after neurosurgey | Meningitis | L/CSF; Autopsy (basilar Aspergillus meningitis with exudate in the subarachnoid space of spinal cord) | WBC 2650/μL (PMNs 10%); glucose 26 mg/dL; protein 1750 mg/L | Aspergillus spp. (CSF culture after multiple attempts) | NA | AMFB (3 days) | Death after 20 days | |
| Diendogh et al., 198314 | 60/M | Neurosurgery (Trans-sphenoidal Yttrium90 implant)/Diabetic retinopathy | Drowsy, disoriented in time and space, neck stiffness, positive Kernig sign | Meningitis | PM/Autopsy (meningitis; necrotizing vasculitis (pons); fungal invasion of basilar and middle cerebral arteries) | WBC 323/μL (PMNs 60%) | Aspergillus spp. (autopsy histology) | NA | None | Death after 2 weeks |
| Walsh et al., 19858 | 64/F | Steroid treatment/Cushing syndrome | Meningismus,headache, hemiparesis | Meningitis | Pm/Autopsy : mycotic Aspergillus aneurism & subarachnoid hemorrhage | WBC 15/μL (PMNs 0%); glucose 90 mg/dL; protein 1450 mg/L | Aspergillus spp. (autopsy histology) | NA | None | Death after 9 days |
| Hajjar et al., 198715 | 28/M | Neurosurgery/Acoustic neurinoma | NR/9 days | Meningitis | L/Wound culture | NR | Aspergillus fumigatus (wound culture) | NA | AMFB + 5-FLU (2 months) | Death after 2 months |
| Asnis et al., 198816 | 44/M | None/AIDS | Confusion, generalized seizures | Meningitis | Pm/Autopsy (Aspergillus leptomeningites) | NR | Aspergillus spp. (autopsy histology) | NA | AMFB (20 days) | Death |
| Carrazana et al., 199117 | 44/M | None/AIDS; sphenoid sinusitis | Headache, fever, nausea, ataxia, hemiparesis, seizures | Meningitis | Pm/Autopsy (Aspergillus meningeal infiltration; thrombosis of basilar artery) | NR | Aspergillus spp. (autopsy histology) | NA | None | Death |
| Komatsu et al., 199118 | 61/F | Neurosurgery/Rathke’cleft cyst | High fever and meningeal signs/12 days after surgery | Meningitis | Pm/Autopsy (Aspergillus meningitis & mycotic aneurism, subarachnoid hemorrhage) | WBC 881/μL (PMNs 70%); glucose 46 mg/dL; protein 540 mg/L | Aspergillus spp. (autopsy histology) | NA | ND | Death after 23 days |
| Lammens et al., 199219 | 39/F | Immunosuppressive therapy/SLE | Headache (1 month), fever (39.5 °C), neck stiffness, Horner syndrome | Meningitis | Pm/Autopsy (Aspergillus basal meningitis & subarachnoid hemorrhage) | WBC 3750/μL (PMNs 84%); glucose 32 mg/dL; protein 1000 mg/L | Aspergillus spp. (autopsy histology) | NA | None | Death after 15 days |
| Torre-Cisneros et al., 199320 | 31/F | Liver transplant/End stage liver disease | Seizurea | Meningitis | Pm/Autopsy (ischemic infarct; leptomeningeal aspergillosis) | NR | Aspergillus spp. (autopsy histology) | NA | NR | Death |
| 21/F | Liver transplant/End stage liver disease | NRa | Meningitis | Pm/Autopsy (ischemic infart; leptomeningeal aspergillosis) | NR | Aspergillus spp. (autopsy histology) | NA | NR | Death | |
| 24/F | Liver transplant/End stage liver disease | Seizurea | Meningitis | Pm/Autopsy (acute leptomeningitis) | NR | Aspergillus spp. (autopsy histology) | NA | NR | Death | |
| 38/M | Kidney transplant/End stage kidney disease | Seizurea | Meningitis | Pm/Autopsy (acute leptomeningitis; haemorrhagic infarcts) | NR | Aspergillus spp. (autopsy histology) | NA | NR | Death | |
| Miaux et al., 199521 | 41/M | Bone marrow transplant; steroid therapy/CML | Fever (38 °C), hemiplegia/2 months | Meningitis | Pm/Autopsy (thickening and meningeal inflammation with haemorrhagic necrosis; lung & heart involvement) | WBC 2000/μL (PMNs 95%); protein 900 mg/L | Aspergillus spp. (autopsy histology) | NA | NR | Death after 5 days |
| 39/F | Bone marrow transplant; steroid therapy/RAEB | Mental confusion/3.5 months | Meningitis | Pm/Autopsy (brain hemorrhagic necrosis; lung involvement) | WBC 2560/μL (PMNs 98%); | Aspergillus spp. (autopsy histology) | NA | NR | Death after 8 days | |
| Adunsky et al., 199622 | 74/M | None/None | Fever (38.3°), stuporous, left hemiplegia, dysarthria (1 day) | Meningitis | L/CSF | WBC 2400/μL (PMNs 94%); glucose 10 mg/dL; protein 1500 mg/L | Aspergillus flavus (CSF culture) | NA | AMFB (few days) | Death after few days |
| Darras-Joly et al., 199623 | 68/M | Neurosurgery/Metastatic cancer | Allucinations, disorientation, hemyanopsia/5 months after surgery | Meningitis; extradural empyema; abscesses | L/Surgery extradural abscess | NR | Aspergillus fumigatus (extradural abscess) | Negative (NR) | AMFB (2 months)+ itraconazole (2 months) | Death after 12 months |
| 29/M | Neurosurgery/Acoustic neurinoma | Fever (38 °C), severe headache/3 days after surgery | Meningitis; abscess; | L/CSF | WBC 830/μL (PMNs 53%); glucose 48 (s 155) mg/dL; protein 830 mg/L | Aspergillus fumigatus (CSF culture) | Positive (NR) | L-AMB (5 weeks)+ 5-FLU (7 weeks); itraconazole (6 months) | Alive after 12 months | |
| Monlun et al., 199724 | 75/F | Steroid therapy/Asthma | Fever (38 °C); acute respiratory failure (22 days) | Meningitis | Pm/Autopsy (right haemorragic infarct with subcortical vessel invasion and meningeal diffusion by Aspergillus; pulmonary involvement) | ND | Aspergillus spp. (autopsy histology) | ND | AMFB (3 weeks) | Death 22 days later |
| Verweij et al., 199925 | 73/F | Mastoidectomy/Otitis media | Fever (39 °C), headache, vomiting, drowsiness, meningismus/NR | Meningitis | L/CSF (sixth attempt) | WBC 2130/μL; glucose 27 mg/dL (47 mg/dL serum); protein 150 mg/L | Aspergillus fumigatus (CSF culture, 6th attempt + PCR) | 10.4 (Platelia) | Itraconazole 1 week; AMFB (4weeks + AMFB intraventricular; voriconazole (9 weeks) | Alive 12 months after voriconazole discontinuation |
| Mariushi et al., 199926 | 43/F | None/None | Headache, neck stiffness (11 days), fever (37.6 °C), nausea, chills | Meningitis | L/CSF | WBC 329/μL (PMNS 0%); glucose 46 mg/dl; protein 500 mg/L | Aspergillus spp. (CSF culture, 5th attempt) | ND | Fluconazole (2 years) | Alive after 2 years |
| Arabi, 200127 | 58/M | None/Maxillary sinusitis | Confusion, progressive unresponsiveness, 4th nerve palsy 8 days after pneumonia | Meningitis | L/Sinus aspirate/Autopsy (Aspergillus ventriculitis, meningitis; focal encephalitis; pneumonia) | WBC 3500/μL (PMNs 91%); glucose 77 mg/dL(s 102); protein 3370 mg/L | Aspergillus fumigatus (sinus culture) | ND | AMFB (3 weeks) | Death 20 days later |
| Nenoff et al., 200128 | 74/M | Ethmoidectomy and orbitotomia (for A.fumigatus orbital and sinus infection)/Diabetes mellitus | Vomiting, nausea, exophthalmus, somnolent and disoriented/7 months | Meningitis | L/Biopsy (orbital apex)/Autopsy (Aspergillus meningitis, vasculitis internal carotid, mycotic aneurism with subarachnoid hemorrhage) | NR | Aspergillus fumigatus (biopsy) | 1:2 (Pastorex) | AMFB+ 5-FLU (few days) | Death 3 weeks after surgical procedure |
| Moling et al., 200229 | 24/M | Kidney transplant (reject); Hemodialysis + steroid therapy/complement 4 deficiency | Fever (39 °C); confusion; disorientation; right motor hemi-syndrome (2 weeks) | Meningitis | L/CSF | WBC 3200/μL; glucose 4 mg/dL | Aspergillus fumigatus (CSF culture, 4th attempt + PCR) | ND | Fluconazole (2 weeks): L-AMB (3 weeks); itraconazole (4 months) | Alive after 7 months; Death after 6 yearsb |
| Kleinschmidt-De Masters, 200230 | 40/F | Steroid therapy/Wegener's granulomatosis | NR | Meningitis | Pm/Autopsy (Aspergillus acute and chronic basilar granulomatous meningitis; mycotic aneurism; lung, skin, heart involvement) | NR | Aspergillus spp. (autopsy histology) | ND | NR | Death after 68 days |
| 51/M | Chemotherapy/Lymphoma | NR | Meningitis | Pm/Autopsy (Aspergillus basilar meningitis; thrombotic occlusion of arteries | NR | Aspergillus spp. (autopsy histology) | ND | NR | Death after 4 days | |
| Pandian et al., 200431 | 34/F | Spinal anaesthesia/None | Fever, headache, vomitingc | Meningitis | Pm/Autopsy (Aspergillus meningitis; mycotic aneurism with subarachnoid hemorrhage) | WBC 640/μL (PMNs 76%); glucose 32 mg/dL; protein 3600 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Death |
| 21/F | Spinal anaesthesia/None | Fever, headache, vomitingc | Meningitis | Pm/Autopsy (Aspergillus meningitis; mycotic aneurism with subarachnoid hemorrhage) | WBC 678/μL (PMNs 65%); glucose 23 mg/dL; protein 3600 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Death | |
| 42/F | Spinal anaesthesia/None | Fever, headache, vomitingc | Meningitis | Pm/Autopsy (Aspergillus meningitis; mycotic aneurism with subarachnoid hemorrhage) | WBC 240/μL (PMNs 68%); glucose 23 mg/dL; protein 2400 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Death | |
| 32/F | Spinal anaesthesia/None | Fever, headache, vomitingc | Meningitis | Pm/Autopsy (Aspergillus meningitis; mycotic aneurism with subarachnoid hemorrhage) | WBC 345/μL (PMNs 76%); glucose 23 mg/dL; protein 1230 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Unknown | |
| 24/F | Spinal anaesthesia/None | Fever, headache, vomitingc | Meningitis | Pm/Autopsy (Aspergillus meningitis; mycotic aneurism with subarachnoid hemorrhage) | WBC 435/μL (PMNs 96%); glucose 32 mg/dL; protein 4200 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Death after 18 months | |
| Larson Kolbe et al., 200732 | 51/F | Epidural steroid injections/COPD | Mental status changes; 3rd nerve palsy/2 months | Meningitis | L/Disc aspiration | NR | Aspergillus fumigatus (disc aspiration + vpsoas abscess culture) | ND | Caspofungin + oriconazole (4 months) | Death after 5 months |
| Gunaratne et al., 200733, 78 | 26/F | Spinal anesthesia (Pregnancy)/None | Low grade fever; headache; nausea; vomiting 12 days after sa | Meningitis | Pm/Autopsy | WBC 302/μL (PMNs 99%); glucose 56 mg/dl (s 115 mg/dL)d; protein 680 mg/L | Aspergillus fumigatus (autopsy culture) | ND | Fluconazole | Death after 4 weeks |
| 21/Fe | Spinal anesthesia (Pregnancy)/None | Fever, chills, neck stiffness 10 days after sa | Meningitis | Pm/Autopsy | WBC 575/μL (PMNs 70%); glucose 25 mg/dl (s 90 mg/dL)d; protein 490 mg/L | Aspergillus fumigatus (autopsy culture) | ND | AMFB (4 days) | Death after 4 weeks | |
| 27/F | Spinal anesthesia (Pregnancy)/None | Fever, headache, neck stiffness; diplopia, photophobia 15 days after sa | Meningitis | L/CSF (microscopy) | WBC 720/μL (PMNs 3%); glucose 21 mg/dl (s 133 mg/dL)d; protein 680 mg/L | Aspergillus spp. (CSF) | ND | AMFB iv + it (4 weeks) voriconazole (4 weeks) | Alive after 12 months (residual 6th cranial nerve palsy and impaired hearing) | |
| 29/F | Spinal anesthesia (Pregnancy)/None | Fever, headache, vomiting, neck stiffness, photophobia 11 days after sa | Meningitis | L/CSF | WBC 1430/μL (PMNs 40%); glucose 45 mg/dl; protein 330 mg/L | Aspergillus fumigatus (CSF culture) | ND | AMFB iv + it (2 weeks); voriconazole (16 weeks) | Alive after 12 months (no disability) | |
| 38/F | Spinal anesthesia (Pregnancy)/None | Fever, neck stiffness 8 days after sa | Meningitis | Pm/Autopsy | WBC 225/μL (PMNs 0%); glucose 61 mg/dL (s 109 mg/dL)e; protein 280 mg/L | Aspergillus fumigatus (autopsy culture) | ND | AMB (9 days) | Death after 24 days | |
| Saitoh et al., 200734 | 33/M | Chemotherapy/AML | Fever, headache, neck stiffness/14 days post-chemotherapy | Meningitis | L/CSF | WBC 15/μL; glucose 30 mg/dL; protein 760 mg/L | Aspergillus spp. (PCR + Ag on CSF) | 2.2 (s 0.1) (Platelia) | AMFB (1 week); voriconazole (12 months) | Alive after 1 year |
| Sundaram et al., 200735 | 22/M | Spinal anesthesia (1 month prior)/None | Fever, headache, vomiting (2 months), neck stiffness | Meningitis | Pm/Autopsy (Aspergillus purulent meningitis & mycotic aneurism with subarachnoid hemorrages) | WBC 720/μL (PMNs 90%); glucose 37 mg/dL; protein 850 mg/L | Aspergillus fumigatus (CSF culture, 5th attempt)f | ND | ND | Death after 68 days |
| Van de Beek et al., 200836 | 56/M | Kidney-pancreas transplant/End stage disease; sphenoid sinusitis | Headache, fever (6 weeks); neck stiffness, dysarthria, hemiparesis | Meningitis | L/sphenoid biopsy/Autopsy (Aspergillus meningitis; midline herniation, subarachnoid hemorrhage) | WBC 1200/μL (PMNs 94%); glucose 64 mg/dL; protein 7300 mg/L | Aspergillus fumigatus (sphenoid biopsy + autopsy) | 6.47 (s 0.39) (Platelia) | Voriconazole (NR) | Death after 4 weeks |
| [PR], 2011 | 35/M | IVDA (heroin)/Chronic hepatitis C | Fever (37.5 °C), headache, back pain (1 month) | Meningitis & spinal arachnoiditis | L/CSF | WBC 260/μL (PMN 70%); glucose 1 mg/dL (s 76 mg/dL); protein 7900 mg/L | Aspergillus flavus (CSF culture) | 7.4 (s 2.5) (Platelia) | Voriconazole 5 months (+1 month caspofungin); L-AMB 3 months | Alive after 9 months |
| Chronic meningitis/pachimeningitis | ||||||||||
| Palo et al., 197537 | 69/M | None/Diabetes | Headache, fever, diplopia, vertigo hearing loss (6 months) | Chronic meningitis | Pm/CSF; autopsy: (granulomatous leptomeningitis and spinal cord involvement) | WBC 103/μL (PMNs 8%); glucose 45 mg/dL; protein 1400 mg/L | Aspergillus fumigatus (CSF culture, 6th attempt)f | NA | None | Death 1 month later |
| Gordon et al., 19763, 79 | 34/F | IVDA (heroin, cocaine)/None | Bifrontal headache, neck stiffness (weeks), low-grade fever | Chronic meningitis | L/CSF | WBC 2892/μL (PMNs 80%); glucose 16 (s 110) mg/dL; protein 990 mg/L; | Aspergillus oryzae (CSF culture, 7th attempt) | NA | AMFB+ 5-FLU (12 months) | Alive (6 year later; episode of bilateral necrotizing scleritis due to A.orizae)g |
| Mielke et al., 198138 | 58/F | Neurosurgery/Acromegaly | Severe headache (4 months), retro-orbital pain, blindness, ophalthalmoplegia/10 months | Chronic meningitis | Pm/Autopsy (chronic basilar meningitis by A.fumigatus & C.albicans; mycotic aneurism of the basilar artery with subarachnoid hemorrhage) | ND | Aspergillus fumigatus (autopsy culture) | NA | None | Death after 7 days |
| Weinstein et al., 198239 | 67/M | None/none | Retro-orbital and periorbital pain, vertigo (months); decrease eye vision; weakness; malaise | Chronic meningitis | L/biopsy sphenoid wing | WBC 88/μL (PMNs 6%); glucose 53 (s 97) mg/dL; protein 1130 mg/L | Aspergillus fumigatus (biopsy + culture sphenoid) | NA | AMFB + rifampicin (2 weeks) | Death after 18 days from surgery |
| Salaki et al., 198440 | 32/M | Steroid treatment/SLE | Fever (38 °C), frontal headache, lethargy (3 weeks), stiff neck, 6th nerve palsy | Chronic meningitis | L/CSF + spinal aspirate | WBC 1400/μL (92%); glucose 33 mg/dL; protein 1100 mg/L | Aspergillus fumigatus (CSF culture, 4th attempt) | NA | AMFB +5-FLU (NR) | Alive |
| Woods et al., 199041 | 44/M | None/AIDS | Headache, fever, nausea, vomiting, lethargy, slurred speech, severe back pain (4 months) | Chronic meningitis | Pm/Autopsy (Aspergillus acute and chronic basilar meningitis; spinal arachnoiditis; pleural, brain, lumbar spinal cord involvement) | WBC 80/μL (PMNs 80%); glucose 19 mg/dL; protein 2000 mg/L | Aspergillus fumigatus (autopsy culture) | NA | None | Death after 18 days |
| Murai et al., 199242 | 59/F | None/Diabetes; Liver cirrhosis; Mondini's anomaly; otitis media | Headache; hearing loss; multiple nerve palsy (6th, 8th, 9th, 10th, 11th) | Chronic pachymeningitis | L/surgery maxillary sinus | WBC 7/μL; protein 660 mg/L | Aspergillus flavus (surgery culture) | NA | Miconazole (2 months); 5-FLU, fluconazole (1 month) | Alive after 4 months |
| Kurino et al., 199343 | 63/M | None/Diabetes; otitis media | Fever, headache, hyperesthesia of face, abducens palsy, deafness | Chronic meningitis | Pm/Biopsy granuloma + autopsy | WBC 138/μL (PMNs 50%); glucose 87 mg/dL; protein 1007 mg/L | Aspergillus spp. (biopsy + autopsy) | NA | None | Death 30 days post-surgery |
| Mochizuki et al., 200044 | 75/M | None/Otitis media | Multiple cranial nerve palsy (2nd, 3rd, 4th), impaired vision (4 months) | Chronic pachymeningitis | L/Biopsy | NR | Aspergillus flavus (biopsy culture) | ND | Fluconazole (4 weeks); AMFB (4 months)+5-FLU (4 months); itraconazole (5 months) | Alive after 36 months |
| Moling et al., 200229 | 48/M | Alcohol abuse/None | Headache, fever, gait instability, apathy (5 months) | Chronic meningitis + ventriculitis + arachnoiditis | L/CSF | WBC 1880/μL; glucose 20 mg/dL | Aspergillus candidus group (CSF culture) | 6.7 (s 1.7) (Platelia) | AMFB (1 week); rifampicin (several months); voriconazole (10 days); itraconazole (10 months) | Alive after 24 months |
| Kowacs et al., 200445 | 26/M | Near drowning/None | Fever (37.2 °C), mild meningismus (4 weeks) | Chronic meningitis | L/CSF | WBC 165/μL (PMNs 69%); glucose 64 mg/dL; protein 778 mg/L | Aspergillus fumigatus (CSF culture, 3rd attempt) | ND | Fluconazole (12 days); itraconazole + AMFB (44 days) | Death after 56 days |
| Ismail et al., 200746 | 73/M | None/Diabetes mellitus; pulmonary asbestosis | Headache, left-sided visual loss, scalp tenderness, fatigue (3 weeks) | Hypertrophic pachymeningitis | L/Meningeal biopsy | WBC 0/μL; protein 5670 mg/L | Aspergillus flavus (biopsy culture) | ND | Antifungal treatment (NR) | Death 3 months later |
| Kagawa et al., 200847 | 33/F | Spinal cord mass lesion | Headache, low grade fever (5 months), hydrocephalus | Chronic meningitis | L/Biopsy VA shunt | WBC 1340/μL; glucose 8 mg/dL; protein 1580 mg/L | Aspergillus spp. (VA shunt biopsy) | ND | AMFB (NR); fluconazole (NR) | Alive after 15 years (multiple recurrences) |
| Chan et al., 201148 | 59/M | Diabetes; impaired renal function | Headache, diplopia, hoarseness (2 months) | Pachymeningitis | L/Dural biopsy | Glucose 102 mg/dL; protein 1270 mg/L | Aspergillus flavus (culture from dural biopsy) | Positive (β-d-glucan + Platelia) | Voriconazole (2 weeks); caspofungin (4 weeks); voriconazole | Alive after 7 months |
| Kato et al., 201149 | 42/M | None/None | Headache, right nucal pain, cranial nerve palsies9, 10, 11, 12 (2 months) | Hypertrophic pachymeningitis | L/CSF | WBC 43/μL (PMNs 4%); glucose 56 mg/dL; protein 1000 mg/L | Aspergillus spp. (CSF PCR positive) | β-d-glucan (Fungitell) 164 pg/mL; serum < 5 pg/mL | Voriconazole (8 week)s; L-AMB+ 5-FLU( 2 week)s; fluconazole 8 weeks | Alive after 30 months |
| Meningoencephalitis | ||||||||||
| Goldhammer et al., 197450 | 45/M | None/none | Headache (9 months), blurred vision (3 weeks) | Meningoencephalitis | Pm/Autopsy (disseminated meningoencephalitis with pituitary abscess and left optic nerve involvement) | ND | Aspergillus spp. (microscopy smear of pituitary abscess + autopsy) | NA | None | Death 4 days postoperatively |
| Naidoff et al., 197551 | 29/F | Kidney transplant/End stage kidney disease | NR | Meningoencephalitis | Pm/Autopsy.disseminated aspergillosis (heart, lung, liver, spleen, thyroid, brain, eye, meninges) | ND | Aspergillus fumigatus (autopsy culture) | NA | None | Death in a few days |
| Kaufman et al., 197652 | 31/F | IVDA (heroin)/None | Headache (9 months), blurred vision (2 months), intermittent diplopia, hearing loss | Meningo-encephalitis | L/Lobectomy; CSF/Autopsy (granulomatous basilar leptomeningitis; aspergilloma left frontal gyrus; transtentorial and tonsillar herniation) | WBC 1150/μL (PMNs 83%); glucose 20 (s 119) mg/dL; | Aspergillus fumigatus (CSF + frontal granuloma culture) | NA | AMFB (2 weeks) | Death after 3 weeks |
| Horton et al., 197653 | 17/F | Fungal endocarditis/Aortic stenosis | Headache, incoordination, right-sided numbness, seizure | Meningoencephalitis | Pm/Autopsy (mycotic aneurism of the middle cerebral artery with subarachnoid hemorrhage) | NR | Aspergillus fumigatus (CSF culture) | NA | None | Death after 9 days |
| Galassi et al., 197854 | 59/F | Neurosurgery/Meningioma | Intermittent fever, seizures, aphasia, hemiparesis/12 months | Meningoencephalitis | L/Surgery of dura granulomas; CSF/Autopsy (diffuse purulent meningo-enecephalitis) | NR | Aspergillus fumigatus (CSF culture) | NA | AMFB (3 months) | Death after 3 months |
| Peacock et al., 198455 | 23/M | Post-chemotherapy/Refractory anemia | Fever, headache, lethargia (57 days post-chemo) | Meningoencephalitis | L/Biopsy (pulmonary); Autopsy (Aspergillus leptomeningitis; necrotizing vasculitis (pons and basal ganglia); tonsillar herniation; necrotizing pneumonia) | WBC 117-1126/μL (PMNs 88–99%); glucose 13–48 mg/dL; protein 540–3460 mg/L | Aspergillus terreus (culture lung biopsy); CSF Aspergillus antigen | Positive (RIA) | AMFB +5-FLU + rifampicin (NR) | Death after 65 days |
| Ouammou et al., 198656 | 3/M | Neurosurgery/Encephalomeningocele | Fever (37.8 °C), frontal subcutaneous abscess/3 days | Meningoencephalitis | L/CSF; surgery: meningeal mycetoma. Autopsy: encephalitis (cerebral hemispheres, brain stem) | WBC 52/μL (PMNs 70%); glucose 10 mg/dL; protein 1200 mg/L; | Aspergillus fumigatus (CSF culture) | NA | Griseofulvin (3 months) | Death after 3 months |
| Cox et al., 199057 | 31/M | None/AIDS | Headache, fever (38.2 °C), confusion, vomiting | Meningoencephalitis | PM/Autopsy (Aspergillus meningitis; mycotic aneurysms; endocarditis; myocarditis) | ND | Aspergillus spp. (autopsy histology) | NA | None | Death after few days |
| Breneman et al., 19925 | 50/M | IVDA; steroid therapy/COPD | Fever (38.6 °C), dyspnea, headache; stiff neck, progressive mental status change (3 days) | Meningoencephalitis | L/brain biopsy | WBC 4100/μL (PMNs 96%); glucose 33 mg/dL; protein 1340 mg/L | Aspergillus fumigatus (Brain biopsy culture) | NA | AMFB (few days) | Death after few days |
| Van der Knaap et al., 199358 | 3/M | None/Galactosemia | Fever (40 °C), nuchal rigidity, convulsions, left hemiparesis | Meningoencephalitis | L/CSF positive antigen | Normal | Aspergillus spp. | Positive (NR) | AMFB + 5-FLU (NR) | Improvement |
| Mikolich et al., 19966 | 25/F | None/None | Worsening headache (3 months); vomiting; photophobia (1 month); papilledema | Meningoencephalitis | L/brain biopsy | WBC 200/μL (PMNs 2%); glucose 40 mg/dL; protein 920 mg/L | Aspergillus fumigatus (brain biopsy) | NA | Itraconazole (24 months) | Alive after 4 years |
| Darras-Joly et al., 199623 | 17/F | Neurosurgery/Ependymoma | Fever (40 °C), neck stiffness/7 days after surgery | Meningoencephalitis; ventricultis | L/Surgical drainage | WBC 1900/μL (PMNs 97%); glucose 36 mg/dL; protein 1100 mg/L | Aspergillus fumigatus (surgical culture) | Negative (NR) | AMFB (72 days) + itraconazole (30 days) | Death after 96 days |
| Schwartz et al., 199759 | 18/M | Chemotherapy/ALL | Meningism, fever/(92 days post-chemotherapy) | Meningoencephalitis | L/Brain biopsy | WBC 1056/μL (PMNs 96%) | Aspergillus spp. (Brain biopsy) | ND | Itraconazole (4 weeks); voriconazole (6 months) | Death after 6 months |
| Koh et al., 199860 | 15/F | Chemotherapy/ALL | Flaccid weakness lower extremities, slurred speech, urinary retention | Meningomieloencephalitis | Pm/Autopsy (Multifocal leptomeningeal exudates; fungal abscess/necrosis in spinal cord) | ND | Aspergillus spp. (autopsy histology) | ND | ND | Death 21 days later |
| Payot et al., 199961 | 29/M | None/AIDS | Headache (3 weeks), nausea (1 week), fever (39 °C), nuchal rigidity | Meningoencephalitis | Pm/Autopsy (Aspergillus purulent basal meningitis + bulbar encephalitis) | WBC 19/μL (PMN 50%); protein 1080 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Death after 7 days |
| Fasciano et al., 199962 | 26/M | Steroid treatment/Chronic asthma | Fever, quadriplegia, areflexia; hydrocephalus (2 weeks) | Meningoencephalitis | L/Brain biopsy/Autopsy: (Aspergillosis of brain, meninges, cauda equina, lungs, thyroid; bilateral uncal herniation) | WBC 1300/μL (PMNs 98%); glucose 40 mg/dl; protein 1100 mg/L | Aspergillus fumigatus (brain biopsy) | ND | AMFB iv and intratechal + 5-FLU (2 weeks) | Death after 6 weeks |
| Chandra et al., 200063 | 40/F | None/Ethmoid and sphenoid sinusitis | Headache, fever, vomiting (1 week); left proptosis | Meningoencephalitis | L/Brain biopsy | NR | Aspergillus fumigatus (biopsy) | ND | NR | NR |
| Viscoli et al., 200264 | NR | BMT/Acute lymphoblastic leukemia | Fever, neurological deficit, seizures/5 days post-BMT | Meningoencephalitis | Pm/Autopsy (diffuse meningeal and parenchimal infiltration) | NR | Aspergillus spp. (meningeal and parenchimal) | 578 (s 25.7) (Platelia) | NR | Death |
| Wang et al., 200365 | 39/M | Steroid treatment/SARS | Tentorial herniation | Meningoencephalitis | Pm/Autopsy: (Aspergillus meningitis; multiple brain abscess containing aspergillus; disseminated aspergillosis heart, kidney, spleen, pancreas, adrenal glands) | ND | Aspergillus spp. (autopsy histology and culture) | ND | None | Death |
| Roberts et al., 200466 | 71/F | None/Sinusitis | Fever (38.3 °C), severe headache, diplopia, confusion (5 weeks) | Meningoencephalitis | Pm/Autopsy (Aspergillus granulomatous meningitis; thrombosis of basilar artery) | WBC 286/μL (PMNs 38%); glucose 23 mg/dL (s 99); protein 850 mg/L | Aspergillus spp. (autopsy histology) | ND | None | Death after 10 days |
| Botturi et al., 200667 | 59/F | Steroid treatment/Sphenoid sinusitis/ | Headache, diplopia; bilateral 6th nerve palsy (5 weeks) | Meningoencephalitis | L/Brain biopsy | WBC 920/μL (PMNs 96%); glucose 0 mg/dL; protein 180 mg/L | Aspergillus spp. (biopsy) | ND | AMFB (8 weeks); voriconazole (6 months) | Alive after 23 months |
| Gabelmann et al., 200768 | 43/F | Chemotherapy/AML; sinusitis | NR | Meningoencephalitis | Pm/Autopsy | NR | Aspergillus spp. (autopsy histology) | ND | NR | Death after 41 days |
| Van de Beek et al., 200836 | 62/F | Kidney-pancreas transplant/End stage disease | Headache (6 months), altered consciousness | Meningoencephalitis | L/Autopsy (cerebral aspergillosis) | WBC 286/μL (PMNs 90%); glucose 27 mg/dL; protein 830 mg/L | Aspergillus spp. (autopsy histology) | 2.72 (s 0.06) (Platelia) | ABLC | Death after 12 days |
| Spinal arachnoiditis | ||||||||||
| Bryan et al., 198069 | 26/M | IVDA (heroin)/None | Headache, nausea, vomiting (weeks), low back pain; hydrocephalus | Spinal arachnoiditis | L/Lumbar biopsy (lesion L3-5) | WBC 1857/μL (PMNs 43%); glucose 6 mg/dL; protein 5170 mg/L | Aspergillus flavus (immunofluorescence on biopsy) (CSF) | NA | AMFB + rifampicin (10 weeks) | Alive after 14 months |
| Stein et al., 198270 | 24/F | IVDA (heroin)/Chronic alcoholism | Low back pain (4 months), left leg weakness, frequent headache fever (38 °C); confusion and signs of meningeal irritation | Spinal arachnoiditis | L/CSF | WBC 62/μL (PMNs 30%); glucose 70 (105) mg/dL; protein 350 mg/L | Aspergillus terreus (2 CSF cultures)f | NA | AMFB (NR) | Death 26 days after laminectomy |
| Van de Wyngaert et al., 198671 | 30/M | None (splinter stuck on his hand)/None | High fever, painful stiffness of spine, headache, photophobia, nausea | Spinal arachnoiditis | L/CSF | WBC 3200/μL (PMNs 90%); glucose 30 mg/dL; protein 1530 mg/L | Aspergillus fumigatus (CSF) precipitin | NA | AMFB (3 months)+ rifampin (10 days)+ 5-FLU (3 months) | Alive after 229 days |
| Endo et al., 200172 | 55/M | Neurosurgery/Pituitary adenoma | Diplopia, retro-orbital pain (1 year), loss of vision/9 years | Arachnoiditis; subdural abscess | L/Abscess aspiration | NR | Aspergillus fumigatus (abscess culture) | ND | AMFB + fluconazole (4 weeks) | Death after 1 month |
| Genzen et al., 200973 | 37/F | Spinal anesthesia (12 months prior pregnancy) | Headache (months); fever (37.4 °C), blurred vision, numbness left lower extremity | Arachnoiditis | L/Laminectomy & tissue biopsy | WBC 970/μL (PMN 92%); glucose 50 mg/dL; protein 1010 mg/L | Aspergillus terreus (biopsy culture) | ND (s 0.47) | Voriconazole (78 days); voriconazole + caspofungin (54 days); AMFB (6 days); ABLC (50 days) | Alive after 9 months |
| Ventriculitis | ||||||||||
| Morrow et al., 19834 | 36/M | IVDA (heroin)/None | Fever, generalized seizures, nuchal rigidity (1 day) | Ventriculitis | Pm/Autopsy (ventriculitis & hydrocephalus) | WBC 549/μL (PMNs 27%); glucose 29 (s 90) mg/dl; protein 1200 mg/L | Aspergillus flavus (serology)h | NA | None | Death after 40 days |
| Hummel et al., 200674 | 4/F | Chemotherapy/ALL | NR | Ventriculitis & multiple abscess | L/CSF (Ommaya reservoir) | NR | Aspergillus fumigatus (PCR CSF) | Positive (Platelia) | Voriconazole + caspofungin (5 weeks); intraventricular AMFB (4 weeks); voriconazole (2 months) | Alive after 3 months |
| Sutton et al., 200975 | 18/M | Lung transplant/End stage pulmonary disease | Headache, seizure, low grade fever, altered mental status | Ventriculitis | Pm/Autopsy (necrotizing granulomatous inflammation of meninges) | WBC 1100/μL (PMN 79%); glucose 41 mg/dL (s 122); protein 1090 mg/L | Aspergillus granulosus (autopsy culture) | ND | Voriconazole then ABLC and posaconazole | Death after 87 days |
| Antachopoulos et al., 201176 | 5/F | VP shunt | Fever (40 °C), tonic/clonic seizures | Ventriculitis | L/VP | WBC 400/μL (Neutrophil predominance); glucose 25 mg/dL (s 110 mg/dL); protein 1000 mg/L | Aspergillus fumigatus (Culture VP catheter; PCR CSF) | 5.5 (Platelia) | L-AMB (4 months)+ voriconazole (5 months) | Death after 9 months |
M = male; F = female; IVDA = intravenous drug abuser; CSF = cerebrospinal fluid; L = life; Pm = post-mortem; Ag GMN = galactomannan antigen; s = serum; WBC = white blood cells; PMNs = polymorphonuclear; NA = not available; ND = not done; NR = not reported; AMB = amphotericin B dehoxycholate; 5FLU = 5-fluorocytosine; L-AMB = liposomal amphotericin B; ABLC = amphotericin B lipid complex; ALL = acute lymphoblastic leukaemia; CML = chronic myelogenous leukemia; RAEB = refractory anemia with excess blasts; C4def = hereditary complete C4 deficiency; PR = present report; PCR = polymerase chain reaction; VP = ventriculoperitoneal; sa = spinal anaesthesia.
One of these four patients had meningism and headache.
Reported also in reference 77 (updated the follow-up).
Symptoms appeared 2–21 days after spinal anaesthesia (mean 7.8 days).
Random values of blood glucose were reported.
Reported also in reference 78.
Discarded as contaminant.
Reported also in reference 79 (updated the follow-up).
Serological speciation made a result compatible with A. flavus.
Table 2.
Characteristics of patients with aspergillus meningitis.
| Immunocompetent patients, n = 52 (%) | Immunocompromised patients, n = 41 (%) | Total, n = 93 (%) | |
|---|---|---|---|
| Age, years median (range) | 34.5 (3–73) | 39 (4–75) | 37 (3–75) |
| Sex, female (%) | 34 (65.4) | 15/40 (37.5) | 49/92 (53.3) |
| Diagnosis during life | 36/52 (69.2) | 16/41 (39) | 52/93 (55.9) |
| Death after diagnosis in life | 18/36 (50.0) | 9/16 (56.3) | 27/54 (50.0) |
| Total deaths | 33/52 (63.5) | 34/41 (82.9) | 67/93 (72.1) |
| Clinical picture | |||
| Meningitis | 27 (51.9)a | 19 (46.3) | 46 (49.5) |
| Meningoencephalitis | 10 (19.2) | 13 (31.7) | 23 (24.7) |
| Chronic meningitis/pachimeningitis | 8 (15.4)b | 7 (17.1) | 15 (16.1) |
| Spinal arachnoiditis | 5 (9.6)c | −(0.0) | 5 (5.4) |
| Ventriculitis | 2 (3.8) | 2 (4.9) d | 4 (4.3) |
| CSF characteristics | |||
| Positive culture | 17/46 (36.9) | 4/22 (18.2) | 21/68 (30.9) |
| Positive PCR | 3/3 (100) | 3/3 (100) | 6/6 (100) |
| Median WBCs/μL (range) | 640 (5–8800) | 988 (0–4100) | 678 (0–8800) |
| Neutrophils predominance (≥60%) | 25/37 (67.6) | 14/20 (70) | 39/57 (68.4) |
| Hypoglicorrachia | 9/14 (64.3) | 1/2 (50) | 10/16 (62.5) |
| Median glucose level (mg/dL) | 30 (1–77) | 33 (0–102) | 32.5 (0–102) |
| Glucose ≤ 25 mg/dl | 16/39 (41.1) | 4/17 (23.5) | 20/56 (35.7) |
| Median protein level (range) (mg/L) | 995 (100–7900) | 1090 (180–7300) | 1007 (100–7900) |
| Median galactomannan antigen (range) | 7.05 (5.5–10.4) | 4.58 (2.2–578) | 6.58 (2.2–578) |
| Positive | 6/8 (75) | 7/7 (100) | 13/15 (86.7) |
1 patient also had empyema,1 abscess, 1 spinal arachnoiditis.
1 patient had concomitant ventriculitis + arachnoiditis.
1 patient had concomitant subdural abscess.
1 patient had concomitant multiple abscess.
In almost half of the cases (n = 44) Aspergillus was identified by histology or culture without speciation; all other infections were caused by A. fumigatus (n = 34), A. flavus (n = 8) and A. terreus (n = 3) while A. oryzae, A. granulosus and A. candidus were identified in one case each. Forty-one patients were considered immunocompromised hosts (5 AIDS patients; 3 with autoimmune diseases treated with steroids; 9 solid organ transplant recipients; 10 hematologic patients undergoing chemotherapy or bone marrow transplantation; 5 subjects under steroid therapy for chronic obstructive pulmonary disease (COPD), and Severe Acute Respiratory Syndrome; 7 patients with diabetes and, finally, 1 each with Cushing's disease and sarcoidosis). In the fifty-two patients without classic risk factors for invasive aspergillosis, central nervous system involvement was presumed to be the result of: direct extension of Aspergillus from the orbit, ear or paranasal sinuses in 6 patients (11.5%); iatrogenic direct inoculation of Aspergillus through spinal anesthesia (13 patients, 25%), neurosurgery (13 patients, 25%) or epidural steroid injections (1 patient). In six intravenous drug abusers (11.5%) the infection was probably acquired by the hematogenous route. Among the remaining subjects, no predisposing factor could be identified in six patients while one patient each were notable for the presence of the following: pregnancy, alcohol abuse, fungal endocarditis and near drowning. The most common syndrome was acute meningitis which was observed in 46 patients, followed by meningoencephalitis (n = 23). A chronic course of meningitis was observed in 15 patients; five patients showed a picture of spinal arachnoiditis (in 1 case with associated meningitis), and 4 ventriculitis (Table 2). An acute course characterized by rapid deterioration of the clinical picture usually ending with death was observed among immunocompromised hosts and in patients who had direct inoculation of the fungus into the cerebrospinal fluid or the subarachnoid space. By contrast, a sub-acute or chronic form of meningitis going unrecognized for several weeks and sometimes displaying a relapsing character was the most frequent presentation among immunocompetent patients, intravenous drug abusers and patients with diabetes. However, the latter clinical picture was also observed among several patients who had undergone neurosurgery.
Cerebrospinal fluid culture was positive for Aspergillus spp. in 31% of cases with a slightly higher prevalence among immunocompetent (36.9%), as opposed to immunocompromised hosts (18.2%) (Table 2). In nine patients, Aspergillus spp. was cultured from CSF only after repeated attempts (median number of lumbar punctures: 4, range 3–9). Antigen-based assays were employed in fifteen patients: GM antigen by use of the Platelia Elisa in 10 patients, with an unspecified assay in 2 patients, with Pastorex assay in 1 patient and 1,3-β-d-glucan in 2 individuals. GM antigen was detected in CSF specimens of 6 out of 8 immunocompetent patients and in all immunocompromised hosts in whom it was assessed (7/7, 100%) with an overall sensitivity of 86.7%. The median CSF GM index was 6.58 (range 2.2–578).
Serum GM was concomitantly measured in 8 cases and turned positive in 3. In 3 patients, CSF GM was serially determined (3–10, median 7), showing a good correlation with response to therapy. 1-3-β-d-glucan was evaluated in 2 patients with positive results in both. CSF pleocytosis was detected in 61/64 (95.3%) of available specimens with a median cell count of 678/μL and with a neutrophil predominance in 68.4% of cases. Hypoglycorrhachia was shown to be present in 62.5% of cases with a median glucose level of 32.5 mg/dL.
Fifty-six patients received antifungal therapy : amphotericin B dehoxycholate (AMFB) alone or associated with 5-fluorocytosine (11 pts), rifampicin (5 pts), itraconazole (3 pts) or fluconazole (1pt) was used in 36 cases; liposomal amphotericin B (L-AMB) was employed in the treatment of 6 individuals; fluconazole was used in five patients (in three patients as the only drug). Two patients received 5-fluorocytosine, alone in one case and with miconazole and fluconazole in the other case. Fifteen patients received voriconazole (in three cases associated with caspofungin), and in 4 following AMFB use. AMFB was the main antifungal employed until 1996 when oral itraconazole was used for the first time. Voriconazole and L-AMB were used for the first time in 1997, whereas caspofungin in 2006.
Of those patients who had received at least one dose of antifungal agent, 30 (51.7%) died after an interval of time ranging from few days up to 6 years. All patients with chronic meningitis were initially treated with antibiotics and 6 had also received anti-tubercular therapy. An overall case-fatality rate (CFR) of 72.1% was observed, with significant differences between immunocompetent (63.5%) as opposed to immunocompromised patients (82.9%) patients.
Autopsy was available in 49 cases and it was the method by which diagnosis was made for 40 patients (81.6%). In twelve cases basilar meningitis was identified; spinal cord involvement was observed in 5 patients; the presence of a mycotic aneurism involving either the internal carotid artery or the basilar artery was shown in 12 patients with concomitant subarachnoid hemorrhage. Transtentorial, tonsillar or uncal herniation was present in three patients.
Discussion
In a 1969 review of the literature, Mukoyama et al., reported 33 cases of aspergillosis involving the CNS of whom 10 had meningitis and 3 had meningoencephalitis. However, Aspergillus isolation failed in all 10 cultured cerebrospinal fluid specimens.7
In a clinical-pathological study of central nervous system aspergillosis only 1 patient had signs of meningeal irritation during life while at autopsy the meninges were focally affected in nearly half of the cases.8
In the present series regarding 93 patients, a picture of pure meningitis was observed in 65.6% of cases,3, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49 while meningoencephalitis was diagnosed in about 25% of patients.5, 6, 36, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68
In patients with a diagnosis of meningitis fever and headache were the most common presenting symptoms (78.8%) followed by neck stiffness in 28.2% (24/85).3, 4, 5, 6, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76 However, only 16.5% (14/85) of patients presented with three of the four signs and symptoms of headache, fever, neck stiffness and altered mental status.5, 10, 18, 19, 20, 25, 33, 34, 35, 36, 40, 57, 61, 66, 70 Cranial nerve palsies were reported in 17.6% (15/85) and seizures (11/86) in 12.8% of patients.
The diagnosis of Aspergillus meningitis is very difficult and challenging. In fact, a diagnosis during life was obtained only in 55.9% of patients although with a much higher frequency among immunocompetent patients (69.2%)3, 6, 10, 12, 13, 15, 22, 23, 25, 26, 27, 29, 32, 33, 39, 44, 45, 47, 52, 54, 56, 58, 63, 69, 70, 71, 72, 73, 76, 78, 79 PR as opposed to immunocompromised individuals (39%).5, 9, 28, 29, 34, 36, 40, 42, 46, 48, 55, 59, 74 This difference might be explained by a more aggressive and acute course of the disease observed in immunosuppressed hosts. A culture-based diagnosis of Aspergillus meningitis is hampered by the lack of sensitivity as shown by the 31% of positive results observed in our review of published cases.3, 9, 13, 22, 23, 25, 26, 29, 33, 35, 37, 40, 45, 52, 53, 54, 56, 70 PR It has been previously suggested that a minimum of 5 mL of cerebrospinal fluid should be cultured when a mycosis is suspected or that repeated culture of large volumes of CSF are critical for successful in vitro isolation. However, such large volumes are not easy to obtain in clinical practice.80 On the other hand, serial lumbar puncture does indeed seem to have a role since in 9 cases, the fungus could be successfully isolated from cerebrospinal fluid only after several attempts.3, 25, 26, 29, 35, 37, 40, 45
Non-culture based diagnostic methods for the diagnosis of aspergillosis were employed on CSF in fifteen patients and seem to outperform traditional culture, with a overall sensitivity of 87%.23, 25, 28, 29, 34, 36, 48, 49, 64, 75, 76 PR Although a cut-off value of the GM index has not yet been formally established for the diagnosis of CNS aspergillosis, it has been proposed that it might be lower than that used for serum samples due to the lower back-ground reactivity of CSF.25, 81
The median CSF GM index in this series was 6.58 which is a value higher than what is usually observed in serum and well above the cut-off of 0.5 when two serial serum determinations are used among immunocompromised patients or the 0.7–1 value when a single determination is employed in non-hematological patients.82, 83 Notably, when both serum and CSF GM were screened concomitantly, negative results were observed in three cases in serum and the index value was always higher in CSF than in serum.29, 34, 36, 64 PR Although serial determinations on CSF were available only in three cases they may provide useful information on the therapeutic response.25, 29 PR Finally, it seems that the Platelia GM test works well irrespective of the species of Aspergillus involved as shown by the cases described by Verveij, Moling and ourselves in whom A. fumigatus, A. candidus and A. flavus were respectively cultured from the CSF.25, 29 PR
Our review shows that Aspergillus meningitis has an ominous prognosis with a global case-fatality rate (CFR) of 72.1% but with a much better outcome among immucompetent patients in whom a CFR of 63.5% was observed versus a 83% CFR registered among immunocompromised patients. Our data are only slightly better than the 88% CFR reported by Lin et al. in a literature-based survey published before 2001.84
The Infectious Diseases Society of America (IDSA) guidelines recommend voriconazole for the treatment of central nervous system aspergillosis but these recommendations are mainly based upon studies regarding patients with hematological disorders and there is no specific mention as to the treatment of Aspergillus meningitis.85 In our present review, that encompasses a long period of time before the introduction of voriconazole (i.e., 2002), most patients (64.3%) were treated with amphotericin B dehoxycholate and less than 30% received voriconazole at some time of their disease.32, 33, 34, 36, 48, 49, 67, 73, 74, 75, 76 PR In a recent analysis conducted by Schwartz et al. on 120 cases of CNS aspergillosis a 47% response rate and a median survival of 159 days among patients treated with voriconazole was shown.86 Voriconazole shows excellent penetration into the CNS as demonstrated by studies conducted in healthy guinea pigs in whom high cerebrospinal fluid to plasma ratio (0.68) together with rapid penetration across the blood brain barrier were observed.87 Including the present report, determination of cerebrospinal fluid concentrations of voriconazole were available in four cases, with reported values ranging from 0.8 to 5.86 mg/L and with a CSF/plasma ratio ranging from 38% to 76 %.25, 59 PR Hope recently proposed that in the busy clinical setting, voriconazole therapeutic drug monitoring (TDM) should be obtained at the end of day 2 and subsequently in the first week of therapy.88 An association between poor outcome and voriconazole concentrations has been initially observed by Pascual and coworkers.89 In addition Miyakis et al. recently showed an 11-fold increased risk of death among patients with invasive mycoses treated with voriconazole who had an initial trough concentration of less than 0.35 mg/L.90 By contrast, several studies and expert opinion suggest that the optimal maximum voriconazole concentrations should not exceed 5.5–5.8 mg/L89, 91, 92
Another crucial issue not yet addressed so far is the optimal length of antifungal therapy in patients with Aspergillus meningitis, as well as for cerebral aspergillosis. In our patient, antifungal treatment was administered for 7 months, 5 of which employing voriconazole but, just before losing the patient to follow-up we were uncertain how long it would have been necessary to continue the specific treatment. Our analysis of the literature regarding patients with Aspergillus meningitis who were treated with voriconazole shows very different lengths of treatment, ranging from 8–14 weeks to 5–12 months.25, 32, 33, 34, 67, 74, 76 PR
However, it should be pointed out that in most cases the outcome following drug discontinuation is not reported. The long term duration of voriconazole treatment for patients with Aspergillus meningitis or with CNS involvement is a matter not only of efficacy but also of toxicity. In this regard, the risk of phototoxicity and, above all, the risk of inducing squamous cell carcinoma should be mentioned.93
Caspofungin was employed in 5 patients, (in 4 of whom in combination with voriconazole), but its role, if there is any, as a single agent in the treatment of aspergillus meningitis is hampered by the lack of significant penetration across the blood–brain barrier of this drug.94 Except one apparently successful case, flucytosine has been used only in association with AMFB and its role in the treatment of aspergillosis remains anecdotal.9, 95
In conclusion, our review shows that Aspergillus meningitis is a rare clinical entity that is much more frequently observed among immunocompetent patients. It is characterized by CSF neutrophil pleocytosis in 68% of cases and hypoglycorrhachia in 62% of cases. Cultures of CSF are positive only in one third of cases, but the GM antigen test is very useful, with a sensitivity reaching 87%. Although our data show a poor prognosis, we believe that the more widespread use of diagnostic methods with greater sensitivity (i.e., PCR and GM), together with the availability of voriconazole therapy, may allow improved outcomes provided that the diagnosis is achieved earlier. The optimal length of antifungal therapy however remains to be determined.
Funding
No particular funding was received to support this work.
Conflict of interest
Spinello Antinori none Mario Corbellino none Luca Meroni none Federico Resta none Salvatore Sollima none Massimo Tonolini none Anna Maria Tortorano none Laura Milazzo none Lorenzo Bello none Elisa Furfaro none Massimo Galli none Claudio Viscoli none.
Acknowledgments
We thank Rosamaria Rotolo, Virginia Zanzottera, and Rossella Garlaschelli of the Biblioteca “Alberto Malliani” of the University of Milano for their excellent help in the retrieval much of the articles.
References
- 1.Denning D.W., Stevens D.A. Antifungal and surgical treatment of invasive aspergillosis: review of 2,121 published cases. Rev Infect Dis. 1990;12:1147–1201. doi: 10.1093/clinids/12.6.1147. [DOI] [PubMed] [Google Scholar]
- 2.Denning D.W. Therapeutic outcome of invasive aspergillosis. Clin Infect Dis. 1996;23:608–615. doi: 10.1093/clinids/23.3.608. [DOI] [PubMed] [Google Scholar]
- 3.Gordon M.A., Holzman R.S. Aspergillus oryzae meningitis. JAMA. 1976;235:2122–2123. [PubMed] [Google Scholar]
- 4.Morrow R., Wong B., Finkelstein W.E., Sternberg S.S., Armstrong D. Aspergillosis of the cerebral ventricles in a heroin abuser. Arch Intern Med. 1983;143:161–164. [PubMed] [Google Scholar]
- 5.Breneman E., Colford J.M., Jr. Aspergillosis of the CNS presenting as aseptic meningitis. Clin Infect Dis. 1992;15:737–738. doi: 10.1093/clind/15.4.737. [DOI] [PubMed] [Google Scholar]
- 6.Mikolich D.J., Kinsella L.J., Skowron G., Friedman J., Sugar A.M. Aspergillus meningitis in an immunocompetent adult successfully treated with itraconazole. Clin Infect Dis. 1996;23:1318–1319. doi: 10.1093/clinids/23.6.1318. [DOI] [PubMed] [Google Scholar]
- 7.Mukoyama M., Gimple K., Poser C.M. Aspergillosis of the central nervous system. Report of a brain abscess due to A. fumigatus and review of the literature. Neurology. 1969;19:967–974. doi: 10.1212/wnl.19.10.967. [DOI] [PubMed] [Google Scholar]
- 8.Walsh T.J., Hier D.B., Caplan L.R. Aspergillosis of the central nervous system: clinicopathological analysis of 17 patients. Ann Neurol. 1985;18:574–582. doi: 10.1002/ana.410180511. [DOI] [PubMed] [Google Scholar]
- 9.Atkinson G.W., Israel H.L. 5-fluorocytosine treatment of meningeal and pulmonary aspergillosis. Am J Med. 1973;55:496–504. [Google Scholar]
- 10.Feely M., Steinberg M. Aspergillus infection complicating transsphenoidal yttrium-90 pituitary implant. J Neurosurg. 1976;46:530–532. doi: 10.3171/jns.1977.46.4.0530. [DOI] [PubMed] [Google Scholar]
- 11.Mohandas S., Ahuja G.K., Sood V.P., Virmani V. Aspergillosis of the central nervous system. J Neurol Sci. 1978;38:229–233. doi: 10.1016/0022-510x(78)90069-2. [DOI] [PubMed] [Google Scholar]
- 12.Aung B.U.K., Lin U.K., Nyunt U.S. Leptomeningeal aspergillosis causing internal carotid artery stenosis. B J Radiol. 1979;52:328–329. doi: 10.1259/0007-1285-52-616-328. [DOI] [PubMed] [Google Scholar]
- 13.Beal M.F., O'Carroll P.C., Kleinmann G.M., Grossman R.I. Aspergillosis of the nervous system. Neurology. 1982;32:473–479. doi: 10.1212/wnl.32.5.473. [DOI] [PubMed] [Google Scholar]
- 14.Diendogh J.V., Barnard R.O., Thomas D.G.T. Aspergillosis of the nervous system. Report of two cases. Neuropathol Appl Neurobiol. 1983;9:477–484. doi: 10.1111/j.1365-2990.1983.tb00131.x. [DOI] [PubMed] [Google Scholar]
- 15.Hajjar J., Brunon J., Jaubert J., Aubert G., Duthel R., Delorme C. Cerebral aspergillosis. Report on four cases. Neurochirurgie. 1987;33:142–147. [PubMed] [Google Scholar]
- 16.Asnis D.S., Chitkara R.K., Jacobson M., Goldenstein J.A. Invasive aspergillosis: an unusual manifestation of AIDS. NY State J Med. 1988;88:653–655. [PubMed] [Google Scholar]
- 17.Carrazana E.J., Rossitch E., Jr., Morris J. Isolated central nervous system aspergillosis in the acquired immunodeficiency syndrome. Clin Neurol Neurosurg. 1991;93:227–230. doi: 10.1016/s0303-8467(05)80008-3. [DOI] [PubMed] [Google Scholar]
- 18.Komatsu Y., Narushima K., Kobayashi E., Tomono Y., Nose T. Aspergillus mycotic aneurysm-case report. Neurol Med Chir (Tokyo) 1991;31:346–350. doi: 10.2176/nmc.31.346. [DOI] [PubMed] [Google Scholar]
- 19.Lammens M., Robberecht W., Waer M., Carton H., Dom R. Purulent meningitis due to aspergillosis in a patient with systemic lupus erythematosus. Clin Neurol Neurosurg. 1992;94:39–43. doi: 10.1016/0303-8467(92)90117-l. [DOI] [PubMed] [Google Scholar]
- 20.Torre-Cisneros J., Lopez O.L., Kusne S., Julio Martinez A., Starzl T.E., Simmons R.L. CNS aspergillosis in organ transplantation: a clinicopathological study. J Neurol Neurosurg Psichiatr. 1993;56:188–193. doi: 10.1136/jnnp.56.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miaux Y., Ribaud P., Williams M., Guermazi A., Gluckman E., Brocheriou C. MR of cerebral aspergillosis in patients who have had bone marrow transplantation. Am J Neuroradiol. 1995;16:552–562. [PMC free article] [PubMed] [Google Scholar]
- 22.Adunsky A., Rubinstein E., Goldsmith A. Aspergillus flavus meningitis and pontine hemorrhage in an older patient. J Amer Geriatr Soc. 1996;44:739–740. doi: 10.1111/j.1532-5415.1996.tb01852.x. [DOI] [PubMed] [Google Scholar]
- 23.Darras-Joly C., Veber B., Bedos J.P., Gachot B., Regnier B., Wolff M. Nosocomial cerebral aspergillosis: a report of 3 cases. Scand J Infect Dis. 1996;28:317–319. doi: 10.3109/00365549609027182. [DOI] [PubMed] [Google Scholar]
- 24.Monlun E., De Blay F., Berton C., Gasser B., Jaeger A., Pauli G. Invasive pulmonary aspergillosis with cerebromeningeal involvement after short-term intravenous corticosteroid therapy in a patient with asthma. Respir Med. 1997;91:435–437. doi: 10.1016/s0954-6111(97)90259-6. [DOI] [PubMed] [Google Scholar]
- 25.Verweij P.E., Brinkman K., Kremer H.P.H., Kullberg B.-J., Meis J.F.G.M. Aspergillus meningitis: diagnosis by non-culture-based microbiological methods and management. J Clin Microbiol. 1999;37:1186–1189. doi: 10.1128/jcm.37.4.1186-1189.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mariushi W.M., Arruda W.O., Tsubouchi M.E., Ramina R. Chronic Aspergillus sp. meningitis successfully treated with fluconazole. Arq Neuropsiquiatr. 1999;57:288–291. doi: 10.1590/s0004-282x1999000200020. [DOI] [PubMed] [Google Scholar]
- 27.Arabi Y. Nosocomial meningoencephalitis in medical patients. Internet J Infect Dis. 2001;1:2. [Google Scholar]
- 28.Nenoff P., Kellermann S., Horn L.-C., Keiner S., Bootz F., Schneider S. Mycotic arteritis due to Aspergillus fumigatus in a diabetic with retrobulbar aspergillosis and mycotic meningitis. Mycoses. 2001;44:407–414. doi: 10.1046/j.1439-0507.2001.00687.x. [DOI] [PubMed] [Google Scholar]
- 29.Moling O., Lass-Floerl C., Verveij P.E., Porte M., Prugger M., Gebert U. Chronic and acute Aspergillus meningitis. Mycoses. 2002;45:504–511. doi: 10.1046/j.1439-0507.2002.00789.x. [DOI] [PubMed] [Google Scholar]
- 30.Kleinschmidt-DeMasters B.K. Central nervous system aspergillosis: a 20-year retrospective series. Hum Pathol. 2002;33:116–124. doi: 10.1053/hupa.2002.30186. [DOI] [PubMed] [Google Scholar]
- 31.Pandian J.D., Sarada C., Radhakrishnan V.V., Kishore A. Iatrogenic meningitis after lumbar puncture- a preventable health hazard. J Hosp Infect. 2004;56:119–124. doi: 10.1016/j.jhin.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 32.Kolbe A.B., Mckinney A.M., Kendi A.T., Misselt D. Aspergillus meningitis and discitis from low-back procedures in an immunocompetent patient. Acta Radiol. 2007;6:687–689. doi: 10.1080/02841850701342153. [DOI] [PubMed] [Google Scholar]
- 33.Gunaratne P.S., Wijeyaratne C.N., Seneviratne H.R. Aspergillus meningitis in Sri-Lanka- A post-tsunami effect? N Engl J Med. 2007;356:754–756. doi: 10.1056/NEJMc062547. [DOI] [PubMed] [Google Scholar]
- 34.Saitoh T., Matsushima T., Shimizu H., Yokohama A., Irisawa H., Handa H. Successful treatment with voriconazole of Aspergillus meningitis in a patient with acute myeloid leukemia. Ann Hematol. 2007;86:697–698. doi: 10.1007/s00277-007-0292-8. [DOI] [PubMed] [Google Scholar]
- 35.Sundaram C., Goel D., Uppin S.G., Seethajayalakshmi S., Borgohain R. Intracranial mycotic aneurism due to Aspergillus spp. J Clin Neurosci. 2007;14:882–886. doi: 10.1016/j.jocn.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 36.van de Beek D., Patel R., Campeau N.G., Badley A., Parisi J.E., Rabistein A.A. Insidious sinusitis leading to catastrophic cerebral aspergillosis in transplant recipients. Neurology. 2008;70:2411–2413. doi: 10.1212/01.wnl.0000314690.18731.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palo J., Haltia M., Uutela T. Cerebral aspergillosis with special reference to cerebrospinal fluid findings. Eur Neurol. 1975;13:224–231. doi: 10.1159/000114678. [DOI] [PubMed] [Google Scholar]
- 38.Mielke B., Weir B., Oldring D., von Westarp C. Fungal aneurysm: case report and review of the literature. Neurosurgery. 1981;9:578–582. doi: 10.1227/00006123-198111000-00017. [DOI] [PubMed] [Google Scholar]
- 39.Weinstein J.M., Sattler F.A., Towfighi J. Optic neuropathy and paratrigeminal syndrome due to Aspergillus fumigatus. Arch Neurol. 1982;39:582–585. doi: 10.1001/archneur.1982.00510210052013. [DOI] [PubMed] [Google Scholar]
- 40.Salaki J.S., Louria D.B., Chmel H. Fungal and yeast infections of the central nervous system. Medicine. 1984;63:108–132. doi: 10.1097/00005792-198403000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Woods G.L., Goldsmith J.C. Aspergillus infection of the central nervous system in patients with acquired immunodeficiency syndrome. Arch Neurol. 1990;47:181–184. doi: 10.1001/archneur.1990.00530020087020. [DOI] [PubMed] [Google Scholar]
- 42.Murai H., Kira J., Kobayashi T., Goto I., Inoue H., Hasuo K. Hypertrophic cranial pachymeningitis due to Aspergillus flavus. Clin Neurol Neurosurg. 1992;94:247–250. doi: 10.1016/0303-8467(92)90097-m. [DOI] [PubMed] [Google Scholar]
- 43.Kurino M., Kuratsu J., Yamaguchi T., Ushio Y. Mycotic aneurism accompanied by aspergillotic granuloma: a case report. Surg Neurol. 1994;42:160–164. doi: 10.1016/0090-3019(94)90378-6. [DOI] [PubMed] [Google Scholar]
- 44.Mochizuki M., Murase S., Takahashi K., Shimada S., Kume H., Iizuka T. Serum itraconazole and hydroxyitraconazole concentration and interaction with digoxin in a case of chronic hypertrophic pachymeningitis caused by Aspergillus flavus. Jpn J Med Mycol. 2000;41:33–39. doi: 10.3314/jjmm.41.33. [DOI] [PubMed] [Google Scholar]
- 45.Kowacs P.A., Manteiro de Almeida S., Pinheiro R.L., Fameli H., Piovesan E.J., Correia A. Central nervous system Aspergillus fumigatus infection after near drowning. J Clin Pathol. 2004;57:202–204. doi: 10.1136/jcp.2003.010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ismail A.R., Clifford L., Meacock W.R. Compressive optic neuropathy in fungal hypertrophic cranial pachymeningitis. Eye. 2007;21:568–569. doi: 10.1038/sj.eye.6702649. [DOI] [PubMed] [Google Scholar]
- 47.Kagawa R., Okada Y., Moritake K. Fungal meningitic hydrocephalus with repeated shunt malfunction-case report. Neurol Med Chir. 2008;48:43–46. doi: 10.2176/nmc.48.43. [DOI] [PubMed] [Google Scholar]
- 48.Chan H.S., Yuen H.Y., Ng W.K., Vlantis A.C., Ahuja A.T., Tong C.F.M. Aspergillus pachymeningitis mimicking nasopharyngeal carcinoma. J Laryngol Otol. 2011;125:103–107. doi: 10.1017/S0022215110001623. [DOI] [PubMed] [Google Scholar]
- 49.Kato H., Nakajima M., Ichikawa H., Kawamura M. Hypertrophic pachymeningitis in an immunocompetent adult with positive Aspergillus DNA in the cerebrospinal fluid. Neurol India. 2011;59:111–113. doi: 10.4103/0028-3886.76886. [DOI] [PubMed] [Google Scholar]
- 50.Golhammer Y., Lawton Smith J., Yates B.M. Mycotic intrasellar abscess. Tr Am Ophth Soc. 1974;77:65–78. [PMC free article] [PubMed] [Google Scholar]
- 51.Naidoff M.A., Green W.R. Endogenous Aspergillus endophthalmitis occurring after kidney transplant. Am J Ophthalmol. 1975;79:502–509. doi: 10.1016/0002-9394(75)90628-5. [DOI] [PubMed] [Google Scholar]
- 52.Kaufman D.M., Thal L.J., Framer P.M. Central nervous system aspergillosis in two young adults. Neurology. 1976;26:484–488. doi: 10.1212/wnl.26.5.484. [DOI] [PubMed] [Google Scholar]
- 53.Horton B.C., Abbott G.F., Porro R.S. Fungal aneurysms of intracranial vessels. Arch Neurol. 1976;33:577–579. doi: 10.1001/archneur.1976.00500080055008. [DOI] [PubMed] [Google Scholar]
- 54.Galassi E., Pozzati E., Poppi M., Vinci A. Cerebral aspergillosis following intracranial surgery. J Neurosurg. 1978;49:308–311. doi: 10.3171/jns.1978.49.2.0308. [DOI] [PubMed] [Google Scholar]
- 55.Peacock J.E., Jr., McGinnis M.R., Cohen M.S. Persistent neutrophilic meningitis. Report of four cases and review of the literature. Medicine. 1984;63:379–395. [PubMed] [Google Scholar]
- 56.Ouammou A., El Ouarzazi A., Belghmaidi M., El Faidouzi M. Cerebral aspergillosis and encephalomeningocele. Child’s Nerv Syst. 1986;2:216–218. doi: 10.1007/BF00706816. [DOI] [PubMed] [Google Scholar]
- 57.Cox J.N., di Dio F., Pizzolato G.P., Lerch R., Pochon N. Aspergillus endocarditis and myocarditis in a patient with the acquired immunodeficiency syndrome (AIDS) Virchows Archiv A Pathol Anat Histopathol. 1990;417:255–259. doi: 10.1007/BF01600142. [DOI] [PubMed] [Google Scholar]
- 58.van der Knaap M.S., Valk J., Jansen G.H., Kappelle L.J., van Nieuwenhuizen O. Mycotic encephalitis: predilection for grey matter. Neuroradiology. 1993;35:567–572. doi: 10.1007/BF00588394. [DOI] [PubMed] [Google Scholar]
- 59.Schwartz S., Milatovic D., Thiel E. Successful treatment of cerebral aspergillosis with a novel triazole (voriconazole) in a patient with acute leukemia. B J Haematol. 1997;97:663–665. doi: 10.1046/j.1365-2141.1997.972911.x. [DOI] [PubMed] [Google Scholar]
- 60.Koh S., Ross L.A., Gilles F.H., Nelson M.D., Jr., Mitchell W.G. Myelopathy resulting from invasive aspergillosis. Pediatr Neurol. 1998;19:135–138. doi: 10.1016/s0887-8994(98)00021-6. [DOI] [PubMed] [Google Scholar]
- 61.Payot A., Garbino J., Burkhardt K., Delavelle J., Pizzolato G., Kaiser L. Primary central nervous system aspergillosis: a case report and review of the literature. Clin Microbiol Infect. 1999;5:573–576. doi: 10.1111/j.1469-0691.1999.tb00438.x. [DOI] [PubMed] [Google Scholar]
- 62.Fasciano J.W., Ripple M.G., Suarez J.I., Bhardwaj A. Central nervous system aspergillosis: a case report and literature review. Hosp Physician. 1999;4:63–70. [Google Scholar]
- 63.Chandra S., Goyal M., Mishra N.K., Gaikwad S.B. Invasive aspergillosis presenting as a cavernous sinus mass in immunocompetent individuals: report of three cases. Neuroradiology. 2000;42:108–111. doi: 10.1007/s002340050025. [DOI] [PubMed] [Google Scholar]
- 64.Viscoli C., Machetti M., Gazzola P., De Maria A., Paola D., Van Lint M.T. Aspergillus galactomannan antigen in the cerebrospinal fluid of bone marrow transplant recipients with probable cerebral aspergillosis. J Clin Microbiol. 2002;40:1496–1499. doi: 10.1128/JCM.40.4.1496-1499.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang H., Ding Y., Yang L., Zhang W., Kang W. Fatal aspergillosis in a patient with SARS who was treated with corticosteroids. N Engl J Med. 2003;349:507–508. doi: 10.1056/NEJM200307313490519. [DOI] [PubMed] [Google Scholar]
- 66.Roberts M., Carmichael A., Martin P. Cerebral vasculitis caused by Aspergillus species in an immunocompetent adult. Infection. 2004;32:360–363. doi: 10.1007/s15010-004-3077-1. [DOI] [PubMed] [Google Scholar]
- 67.Botturi A., Salmaggi A., Pollo B., Lamperti E., Erbetta A., Boiardi A. Meningitis following relapsing painful ophthalmoplegia in aspergillus sphenoidal sinusitis: a case report. Neurol Sci. 2006;27:284–287. doi: 10.1007/s10072-006-0686-8. [DOI] [PubMed] [Google Scholar]
- 68.Gabelmann A., Klein S., Kern W., Kruger S., Brambs H.-J., Rieber-Brambs A. Relevant imaging findings of cerebral aspergillosis on MRI: a retrospective case-based study in immunocompromised patients. Eur J Neurol. 2007;14:548–555. doi: 10.1111/j.1468-1331.2007.01755.x. [DOI] [PubMed] [Google Scholar]
- 69.Bryan C.S., Di Salvo A.F., Huffman L.J., Kaplan W., Kaufman L. Communicating hydrocephalus caused by Aspergillus flavus. South Med J. 1980;73:1641–1644. doi: 10.1097/00007611-198012000-00032. [DOI] [PubMed] [Google Scholar]
- 70.Stein S.C., Corrado M.L., Friedlander M., Farmer P. Chronic mycotic meningitis with spinal involvement (arachnoiditis): a report of five cases. Ann Neurol. 1982;11:519–524. doi: 10.1002/ana.410110512. [DOI] [PubMed] [Google Scholar]
- 71.van de Wyngaert F.A., Sindle C.J.M., Rousseau J.J., Fernandes Xavier F.G., Bruche J.M., Laterre E.C. Spinal arachnoiditis due to Aspergillus meningitis in a previously healthy patient. J Neurol. 1986;233:41–43. doi: 10.1007/BF00313990. [DOI] [PubMed] [Google Scholar]
- 72.Endo T., Numagami Y., Jokura H., Ikeda H., Shirane R., Yoshimoto T. Aspergillus parasellar abscess mimicking radiation-induced neuropathy. Case report. Surg Neurol. 2001;56:195–200. doi: 10.1016/s0090-3019(01)00488-8. [DOI] [PubMed] [Google Scholar]
- 73.Genzen J.R., Kenney B. Central nervous system Aspergillus infection after epidural analgesia: diagnosis, therapeutic challenges, and literature review. Diagn Microbiol Infect Dis. 2009;65:312–318. doi: 10.1016/j.diagmicrobio.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hummel M., Spiess B., Kentouche K., Niggemann S., Bohm C., Reuter S. Detection of Aspergillus DNA in cerebrospinal fluid from patients with cerebral aspergillosis by a nested PCR assay. J Clin Microbiol. 2006;44:3989–3993. doi: 10.1128/JCM.00466-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sutton D.A., Wickes B.L., Romanelli A.M., Rinaldi M.G., Thompson E.H., Fothergill A.W. Cerebral aspergillosis caused by Aspergillus granulosus. J Clin Microbiol. 2009;47:3386–3390. doi: 10.1128/JCM.00588-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Antachopoulos C., Stergiopoulou T., Simitsopoulou M., Georgiadou E., Kottas S., Marinopoulos D. Ventriculitis caused by Aspergillus fumigatus in a child with central nervous system tuberculosis. Mycoses. 2011;54:e627–e630. doi: 10.1111/j.1439-0507.2010.01940.x. [DOI] [PubMed] [Google Scholar]
- 77.Falkeis C., Mark W., Sergi C., Heininger D., Neumair F., Scheiring J. Kidney transplantation in patients suffering from hereditary complete complement C4 deficiency. Transplant Int. 2007;20:1044–1049. doi: 10.1111/j.1432-2277.2007.00555.x. [DOI] [PubMed] [Google Scholar]
- 78.Rodrigo N., Perera K.N.T., Ranwala R., Jayasinghe S., Warnakulasurya A., Hapuarachchi S. Aspergillus meningitis following spinal anesthesia for caesarean section in Colombo, Sri Lanka. Int J Obs Anesth. 2007;16:256–260. doi: 10.1016/j.ijoa.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 79.Stenson S., Brookner A., Rosenthal S. Bilateral endogenous necrotizing scleritis due to Aspergillus oryzae. Ann Ophthalmol. 1982;14:67–72. [PubMed] [Google Scholar]
- 80.McGinnis M.R. Detection of fungi in cerebrospinal fluid. Am J Med. 1983;75(1B):129–138. doi: 10.1016/0002-9343(83)90084-0. [DOI] [PubMed] [Google Scholar]
- 81.Klont R.R., Mennik-Kertsen M.A., Verveij P.E. Utility of Aspergillus antigen detection in specimens other than serum specimens. Clin Infect Dis. 2004;39:1467–1474. doi: 10.1086/425317. [DOI] [PubMed] [Google Scholar]
- 82.Maertens J.A., Klont R., Masson C., Theunissen K., Meersseman W., Lagrou K. Optimization of the cut-off for the Aspergillus double-sandwich enzyme immunoassay. Clin Infect Dis. 2007;44:1329–1336. doi: 10.1086/514349. [DOI] [PubMed] [Google Scholar]
- 83.Guinea J., Jensen J., Pelaez T., Gijón P., Alonso R., Rivera M. Value of a single galactomannan determination (Platelia) for the diagnosis of invasive aspergillosis in non-hematological patients with clinical isolation of Aspergillus spp. Med Mycol. 2008;46:575–579. doi: 10.1080/13693780801978968. [DOI] [PubMed] [Google Scholar]
- 84.Lin S.J., Schranz J., Teutsch S.M. Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis. 2001;32:358–366. doi: 10.1086/318483. [DOI] [PubMed] [Google Scholar]
- 85.Walsh T.J., Anaissie E.J., Denning D.W., Herbrecht R., Kontoyiannis D.P., Marr K.A. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:327–360. doi: 10.1086/525258. [DOI] [PubMed] [Google Scholar]
- 86.Schwartz S., Reisman A., Troke P.F. The efficacy of voriconazole in the treatment of 192 fungal central nervous system infections: a retrospective analysis. Infection. 2011;39:201–210. doi: 10.1007/s15010-011-0108-6. [DOI] [PubMed] [Google Scholar]
- 87.Lutsar I., Roffey S., Troke P. Voriconazole concentrations in the cerebrospinal fluid and brain tissue in guinea pigs and immunocompromised patients. Clin Infect Dis. 2003;37:728–732. doi: 10.1086/377131. [DOI] [PubMed] [Google Scholar]
- 88.Hope W.W. Population pharmacokinetics of voriconazole in adults. Antimicrob Agents Chemother. 2012;56:526–531. doi: 10.1128/AAC.00702-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pascual A., Calandra T., Bolay S., Buclin T., Bille J., Marchetti O. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis. 2008;46:201–211. doi: 10.1086/524669. [DOI] [PubMed] [Google Scholar]
- 90.Miyakis S., van Hal S.J., Ray J., Marriott D. Voriconazole concentrations and outcome of invasive fungal infections. Clin Microbiol Infect. 2010;16:927–933. doi: 10.1111/j.1469-0691.2009.02990.x. [DOI] [PubMed] [Google Scholar]
- 91.Kim S.-H., Yim D.-S., Choi S.-M., Kwon J.C., Han S., Lee D.G. Voriconazole-related severe adverse events: clinical application of therapeutic drug monitoring in Korean patients. Int J Infect Dis. 2011;15:e753–e758. doi: 10.1016/j.ijid.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 92.Pasqualotto A.C., Xavier M.O., Andreolla H.F., Linden R. Voriconazole therapeutic drug monitoring: focus on safety. Expert Opin Drug Saf. 2010;9:125–137. doi: 10.1517/14740330903485637. [DOI] [PubMed] [Google Scholar]
- 93.Epaulard O., Leccia M.-T., Blanche S., Chosidow O., Mamzer-Bruneel M.F., Ravaud P. Phototoxicity and photocarcinogenesis associated with voriconazole. Med Mal Infect. 2011;41:639–645. doi: 10.1016/j.medmal.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 94.Bellmann R. Clinical pharmacokinetics of systemically administered antimycotics. Curr Clin Pharmacol. 2007;2:37–58. doi: 10.2174/157488407779422311. [DOI] [PubMed] [Google Scholar]
- 95.Polak A.M., Scholer H.J., Wall M. Combination therapy of experimental candidiasis, cryptococcosis, and aspergillosis in mice. Chemotherapy. 1982;28:461–479. doi: 10.1159/000238138. [DOI] [PubMed] [Google Scholar]