Summary
Background
Convalescent blood therapy has been a promising form of treatment for Ebola Virus Disease (EVD), but less attention has been focused on it for treatment.
Method
We assessed the effectiveness of convalescent whole blood (CWB) in the treatment of consented EVD patients. We recruited 69 subjects in December 2014 up to April 2015, at the 34 Military Hospital in Wilberforce and the PTS 1 Ebola Treatment Unit in Hastings, Freetown. Forty-four were given CWB, and 25 who consented but preferred to be exempted from the CWB treatment were used to compare clinical outcomes. All were given routine treatment used at the Ebola Treatment Unit.
Results
One of 44 subjects treated with CWB dropped out of the study and 31 recovered while 12 succumbed to the disease with a case fatality rate of 27.9%. For the group that was given routine treatment without CWB, 11 died with a case fatality rate of 44%. There was a significant difference between admission viral load and viral load after the first 24 h of treatment with convalescent whole blood (P < 0.01). The odds ratio for survival with CWB was 2.3 (95% CI, 0.8–6.5).
Conclusion
CWB is promising for treating EVD in resource-poor settings, especially in the early phases of outbreaks when resource-mobilization is done. Even though our sample size was small and the evaluation was not randomised, our results contribute to existing evidence that convalescent whole blood could be considered as a useful candidate for treating EVD. Further studies that are randomised will be required to further assess the efficacy of CWB as treatment option during any EVD outbreak.
Keywords: Convalescent whole blood, EVD, Treatment, Sierra Leone
Highlights
-
•
We evaluated convalescent whole blood (CWB) to treat EVD.
-
•
We recruited 69 subjects: 44 were enrolled on CWB.
-
•
There was a significant difference between admission viral load and viral load after 24 h of treatment with CWB.
-
•
Case fatality rates were 27.9% for the CWB group and 44% for the control group.
-
•
CWB could still be important in the treatment of EVD.
Background
Convalescent blood therapy has been seeming readily available and a potent form of therapy for Ebola, since the first outbreak of the Ebola Virus Disease (EVD) in 1976, but less attention has been focussed on it for treatment. Early signs of the value of convalescent blood therapy against Ebola were revealed by the recovery of a British laboratory worker in 1977, with occupational exposure to EVD, after treatment with convalescent serum and human interferon1 and by 1979 convalescent plasma was considered a ‘specific treatment’ for Ebola.2 Further evidence of the value of convalescent blood therapy (CBT) was provided by Mupapa and colleagues in 19953 after treating eight subjects with CWB, and only one of them died. The treated patients may have already developed antibodies for EVD and the recovery of the patients was not wholly attributable to the CWB, but it could not also be ruled out as the primary cause of the recovery.
Subsequently, doubts were cast on passive immunotherapy with whole blood when in 1999, Sadek and colleagues4 proved statistically that there was no survival benefit of transfusion of blood from convalescent patients. However, statistical significance does not always correlate with clinical significance. Also, an experiment was conducted to test the effectiveness of convalescent whole blood on naïve monkeys that had been infected with EVD, but it did not lead to recovery,5 creating further doubt on the efficacy of CWB. Again, the volume of CWB used (6 ml/kg) may not have been sufficient enough to cause a recovery in the monkeys and the blood used was obtained after 30 days of reinfection of convalescent monkeys with 1000 pfu of the EVD virus.
Despite the critiques, especially for treating EVD, convalescent blood therapy remains plausible for dealing with hard-to-treat or emerging infectious diseases and is a mode of treatment that existed and was proven before EVD and before the advent of “modern” pharmaceuticals in the 1950s.6 Human-derived and animal-derived convalescent blood were the standard of care for treatment of many pathogen-mediated and toxin-mediated diseases such as influenza in 19186, polio7 and herpes zoster.8 In recent times, convalescent blood products have been used against hard-to-treat infectious diseases such as severe acute respiratory syndrome or SARS[9], [10] and the Middle East Respiratory Syndrome corona virus infection (MERS-CoV)11 with successful outcomes. Additionally, severe pandemic influenza A (H1N1) 2009 virus infection12 and even Ebola[13], [14] have benefitted from CWB during their onsets, but no recent report on CWB for Ebola has been reported.
The distinct forms of convalescent blood therapy are: CWB which was used in this study, convalescent blood plasma (CBP) or convalescent blood serum (CWS) which was recently used for treating EVD in Guinea13 and in other studies.15 Blood serum and blood plasma have the same features, except that serum lacks blood clotting factors while plasma has blood clotting factors, but they perform the same function in passive immunotherapy against EVD.16 Additional CBT are pooled human immunoglobulin (Ig) which is an intravenous immunoglobulin preparation mostly for immunomodulation17; recombinantly produced monoclonal antibodies (mABs) such as ZMapp18 and polyclonal antibodies (pABs)19; the difference between the two is that mABs are produced by a single clone of B lymphocytes, while pABs are secreted by a mixture of B lymphocyte clones. CWB is easier to use and adaptable for application in resource-poor settings with limited kits and burden of hard-to-treat diseases such as EVD. The blood may only require screening for transfusion transmissible infections (TTIs) such as viral hepatitis and HIV and to ensure that the blood is safe and matching the ABO blood groups of recipients. In the case of convalescent plasma, its use may require plasmapheresis, which is the separation of blood cells from the liquid plasma, before use. Also, the IgG in plasma could be enriched by fractionation.15
In resource-poor environments, lacking basic amenities and prone to diseases such as Ebola, the use of CWB is important. In recognition of this fact, the World Health Organisation (WHO) in September 2014, provided interim guidance for the evaluation of CWB and CBP for the treatment of EVD.20
However, little research has been done on CBT, and the few studies done had a small sample size. In this study, we assessed the effectiveness of CWB in the treatment of infected patients using a non-randomised study design.
Methods
Study location
The study was carried out at the 34th Regiment Military Hospital in Wilberforce, Freetown, and the PTS 1 Ebola Treatment Centre in Hastings Freetown. Both treatment centres were established through partnership of the Sierra Leone MOHS, Ministry of Defence and WHO. Both treatment units were operated mainly by Sierra Leoneans. The Hastings unit had earlier recorded a case fatality rate of 31.5% resulting from treating 581 EVD patients with IV fluids, IM vitamin K, IM artemether, IV ceftriaxone, IV metronidazole, Ringer's Lactate, dextrose saline, Ibuprofen tablets, Immunoboost nutrition supplement, zinc sulphate tablets, artesunate–lumefantrine combination therapy tablets, oral rehydration salts and other drugs.21
Study design
The study was a non-randomised, double-site, case series of patients treated with convalescent whole blood and those not treated with CWB during the 2014/2015 EVD outbreak.
This study started in the month of December 2014 and ended in April 2015. We recruited 69 consented patients. Recruitment was based on whether they were willing to be part of the study and if they agreed to have CWB transfusion and if a matching blood was available for transfusion. All those that agreed to having a CWB transfusion were 44 subjects while 25 did not agree to having blood transfusion with CWB.
Routine care described previously by Ansumana et al.21 was given to all the patients; briefly, patients were given IV fluids, multivitamins, antipyretics, analgesics, antibiotics, anthelmintics and antimalarial drugs when deemed necessary.
Data collection
Demographic data of the patients and their clinical stages were recorded during recruitment. Four clinical stages of EVD were identified. Stage 1, was characterised by fever, sore throat, headache, stomach ache and body aches and was also called ‘dry phase’. Stage 2 was characterised by vomiting, haematemesis, rash, dehydration, weakness, eye redness, and chest pain and was also called ‘wet phase’. Stage 3, was mainly characterised by bleeding and reduced level of consciousness or irresponsiveness and was also called ‘multiple/single organ dysfunction phase’. The final stage, stage 4, was the recovery phase. Symptoms were recorded on a form at recruitment with other metadata such as age, sex and weight.
Blood transfusion
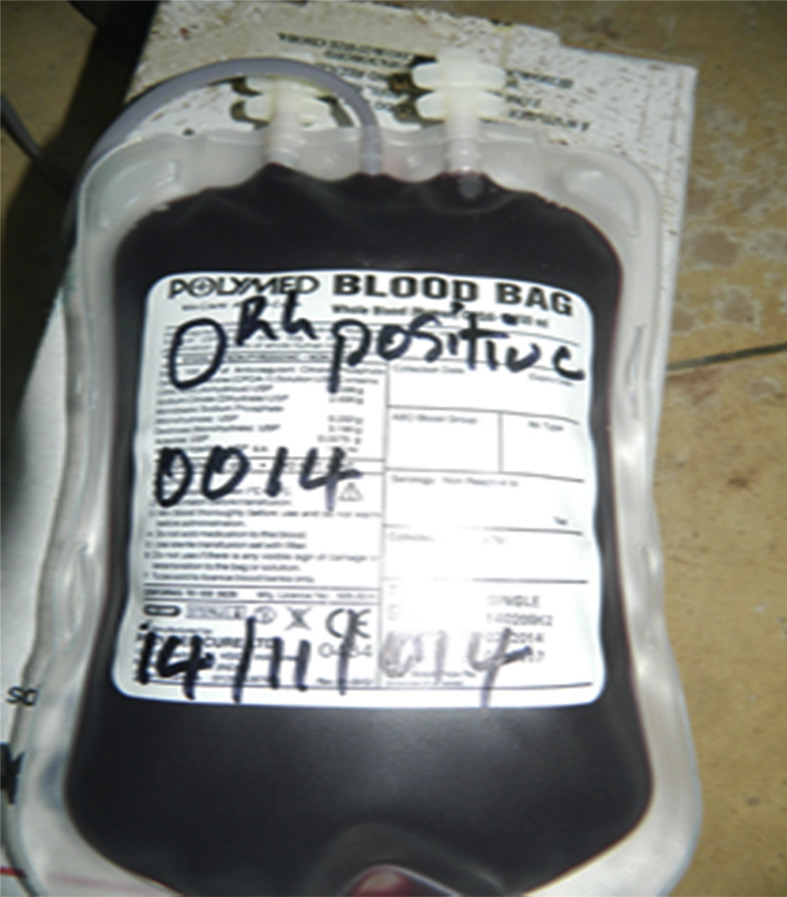
Convalescent whole blood (CWB) was administered within the first 24 h of admission according to the WHO ‘Interim Guidance for National Health Authorities and Blood Transfusion Services’.20 One unit (450 ml) of ABO compatible blood was administered to consented subject over a period of one to four hours. There was no adverse reaction from the transfusions. To prevent adverse reactions, ABO compatibility tests were done on the donated blood, the collection date recorded and the donor ID recorded on the blood bag (Fig. 1 ). The blood was obtained and tested by blood services technicians of the Sierra Leone Ministry of Health and Sanitation from 60 consented blood donors that had recovered from Ebola in Kenema Town, Eastern Sierra Leone. Donated blood was obtained after three months of recovery. The earlier cases of the epidemic in Sierra Leone affected people from Eastern Sierra Leone, so it was easier to get convalescent blood donors that had recovered over 3 months at the time of blood collection. The average age of the blood donors was 28 (±26.2) years, 35 were females, and 25 were males. Apart from being clinically asymptomatic and testing negative twice by PCR for Ebola prior to discharge, the blood of donors was again screened using ELISA at the Kenema Government Lassa Fever Laboratory to ensure that there were no Ebola antigens. Donated blood was also screened for transfusion transmissible infections (TTIs) using SD Bioline (Standard Diagnostics, Seoul, Korea) lateral flow immunoassays for viral hepatitis, syphilis and HIV and also Alere Determine™ HIV-1/2 (Alere Medical Co Ltd. Matsudo-shi, Chiba, Japan) in the case of HIV.
Figure 1.
An example of EVD convalescent blood for transfusion.
Statistical analyses
Simple rates and proportions were used in this study. A two-sample t-test for independent samples was used to compare Ct values of patients on admission and 24 h after admission. Odds ratios, mean and median values were computed. Mean and standard deviations were reported as Mean ± SD. The Ct values were obtained as part of the real-time PCR results. Fisher-exact probabilities were computed at a level of α = 0.05. All statistical analyses were done with the Vassarstats Online Statistics App (http://vassarstats.net/).
Ethics procedure
Ethical clearance was obtained from the Sierra Leone Ethics and Scientific review committee. All subjects included in the study consented to participate.
Results
Sixty-nine EVD subjects were assessed; 95.5% (95% CI, 87.8–98.5) were weak on admission, 79.4% (95% CI, 68.4–87.3) had body aches on admission, 67.7% (95% CI, 55.9–77.6) were vomiting, 64% (95% CI, 52.85–75%) were febrile; 51.47% (95% CI, 39.8–63) had headaches, 44% (95% CI, 33–56) had stomach pain, 30.1% (95% CI, 21.2–42.6) had red eyes on admission, 16.2% (95% CI, 9.2–26.7) had sore throat, 13% (95% CI, 7.1–23.3) had chest pain and 10% (95% CI, 5.1–19.8) were bleeding on admission.
The average age and weight of the CWB-group (44 subjects) were 28.4 (±14.3) years and 66.6 (±34) kg respectively; 21 were males and 23 were females. The mean age and weight of the Non-CWB group (25 subjects) were 33.6 (±15.9) years and 55.8 (±18.7) kg respectively; thirteen were males and twelve females. The CWB-group took an average of 1.97 ± 0.66 days after onset of symptoms before admission to the holding centre and another 1.61 ± 0.8 days before admission to the Ebola treatment unit (ETU). The Non-CWB group (25 subjects) took an average of 2.09 ± 0.9 days after onset of symptoms before admission to a holding centre and another 1.52 ± 0.5 days before admission to an ETU.
Out of 44 subjects that were treated with CWB, 1 dropped out of the study and 31 recovered while 12 succumbed to the disease with a case fatality rate of 27.9%. For the control group that were given routine treatment without convalescent whole blood, 11 died with a case fatality rate of 44%. Patients treated with convalescent whole blood took an average of 10.6 ± 3.4 days to recover while the control patients that recovered took an average of 12.23 ± 4.8 days to recover. Recovery was marked by a gradual decrease in viral load during the treatment. The Ct values for 16 patients on CWB that recovered were recorded. Similarly, the Ct values of five Non-CWB patients were obtained on admission and 24 h after transfusion or admission. Ct values are inversely related to viral load such that lower Ct values mean higher viral load and vice versa. The average Ct value on admission was 23.37 ± 5.0 and the average 24 h after transfusion was 29.99 ± 5.9 (Table 1 ). For the Non-CWB, the average Ct value on admission was 31.97 ± 8.4 and average Ct value after 24 h of admission was 31.25 ± 7.5 Similarly, Ct value for seven Non-CWB subjects that died and four subjects on convalescent blood that died were obtained. The average Ct value for Non-CWB patients that died was 23.69 ± 3.5 on admission and 22.98 ± 4.1 obtained 24 h after admission. For those on convalescent blood that died, the Ct value was 21.77 ± 4.9 on admission and 24.40 ± 5.4 obtained 24 h after transfusion (Table 2 ). The median number of days to death was 4 days for the control group and it was five days for the treatment group. There was a significant difference between admission viral load and viral load after the first 24 h of treatment with convalescent whole blood (P < 0.01). The reduction in viral load was observable in subjects with convalescent blood than those in the Non-CWB group of the study. The odds ratio for survival with CWB was 2.3 (95% CI, 0.8–6.5) (Table 3 ).
Table 1.
Viral load (CT values) for recovered CWB and Non-CWB subjects.
| PID | Sex | Age | Blood group | Weight (kg) | Days before isolation | Days in holding centre | Clinical stage of infection | Date of admission to ETU | Number of Days in ETU | Blood group of donor | Blood expiration date |
Ct Value on admission | Ct Value 24 h after transfusion | Group |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 002 | F | 45 | A Rh+ | 197 | 1 | 2 | 2 | 1/02/15 | 16 | A Rh+ | 10/02/15 | 28.37 | 31.62 | CWB-group |
| 003 | F | 20 | O Rh+ | 50 | 2 | 1 | 1 | 4/01/15 | 16 | O Rh+ | 10/02/15 | 36.78 | 40 | |
| 004 | F | 35 | A Rh+ | 100 | 2 | 1 | 2 | 4/01/15 | 16 | A Rh+ | 10/02/15 | 30.87 | 34.9 | |
| 006 | F | 24 | B Rh+ | – | 1 | 2 | 2 | 6/01/15 | 14 | B Rh+ | 10/02/15 | 23.36 | 34.48 | |
| 007 | F | 35 | B Rh+ | 58 | 2 | 2 | 2 | 23/02/15 | 7 | B Rh+ | 25/02/15 | 28.52 | 33.43 | |
| 008 | M | 14 | A Rh+ | 55 | 2 | 2 | 2 | 24/01/15 | 11 | A Rh+ | 5/02/15 | 23.85 | 19.62 | |
| 009 | F | 33 | A Rh+ | 60 | 1 | 1 | 2 | 29/01/15 | 9 | A Rh+ | 5/02/15 | 30.96 | 33.99 | |
| 010 | M | 35 | O Rh+ | – | 1 | 1 | 2 | 31/01/15 | 8 | O Rh+ | 9/02/15 | 23.09 | 27.01 | |
| 011 | M | 22 | B Rh+ | 55 | 2 | 1 | 2 | 12/02/15 | 8 | B Rh+ | 25/02/15 | 16.97 | 20.49 | |
| 012 | M | 40 | O Rh+ | 70 | 2 | 2 | 2 | 23/12/14 | 17 | O Rh+ | 24/12/14 | 25.66 | 32.01 | |
| 013 | F | 11 | O Rh+ | 37 | 3 | 2 | 1 | 20/12/14 | 10 | O Rh+ | 23/12/14 | 27.68 | 30.1 | |
| 014 | F | 14 | O Rh+ | 70 | 2 | 1 | 2 | 22/12/14 | 9 | O Rh+ | 24/12/14 | 25.31 | 32.6 | |
| 016 | M | 20 | O Rh+ | 50 | 1 | 3 | 2 | 7/1/15 | 11 | O Rh+ | 24/12/14 | 23.04 | 33.34 | |
| 017 | M | 25 | B Rh+ | – | 2 | 2 | 2 | 28/1/15 | 7 | B Rh+ | 10/02/15 | 20.67 | 30.2 | |
| 018 | F | 34 | B Rh+ | 50 | 2 | 1 | 2 | 12/2/15 | 9 | B Rh+ | 25/02/15 | 30.12 | 36.2 | |
| 019 | M | 44 | B Rh+ | 80 | 2 | 2 | 2 | 23/2/15 | 9 | B Rh+ | 25/02/15 | 24.99 | 32.2 | |
| Mean ± SD | 28.2 ± 10.9 | 71.7 ± 40.9 | 1.8 ± 0.6 | 1.7 ± 0.6 | 23.37 ± 5.0* | 29.99 ± 5.9* | ||||||||
| NS001 | M | 48 | – | – | 2 | 2 | 2 | 31/12/14 | 9 | – | – | 37.25 | 36.21 | Non-CWB group |
| NS002 | M | 32 | – | – | 2 | 1 | 2 | 31/12/14 | 8 | – | – | 25.22 | 26.03 | |
| NS003 | M | 24 | – | – | 1 | 2 | 2 | 5/1/15 | 14 | – | – | 38.85 | 35.21 | |
| NS004 | F | 25 | – | – | 1 | 1 | 1 | 22/1/15 | 18 | – | – | 20.74 | 20.75 | |
| NS005 | F | 23 | – | 25 | 2 | 2 | 2 | 9/12/14 | 5 | – | – | 37.79 | 38.08 | |
| Mean ± SD | 30.4 ± 10.5 | 1.6 ± 5.5 | 1.6 ± 5.5 | 10.8 ± 5.1 | 31.97 ± 8.4 | 31.25 ± 7.5 |
*P < 0.01; admission viral load is significantly different from viral load, 24 h after transfusion.
Table 2.
CT value for dead CWB and NCWB EVD cases.
| PID | Sex | Age | Blood group | Days before isolation | Days in holding centre | Clinical stage of infection | Date of admission to ETU | Number of days in ETU | Ct Value on admission | Ct Value 24 h after transfusion/admission | Symptoms prior to death | Drugs administered |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CW001 | F | 35 | O Rh+ | 3 | 2 | 2 | 6/01/15 | 10 | 28.94 | 31.63 | Headache, body aches, anorexia, vomiting, sore throat, stomach pain, weakness, insomnia, bleeding | IV fluids, IV ceftriaxone, Ciprofloxacin tabs, flagyl, PCM tabs |
| CW005 | F | 15 | O Rh+ | 1 | 2 | 2 | 6/01/15 | 5 | 19.37 | 23.55 | Fever, weakness, body pains, headache, anorexia, side pains, cough, insomnia, diarrhoea | IV ceftriaxone, IV metronidazole, pain tabs, ciprofloxacin tabs |
| CW015 | M | 14 | O Rh+ | 2 | 2 | 2 | 22/12/14 | 4 | 20.65 | 18.49 | Headache, Weakness, red eyes, chest pain | Intravenous fluids, vitamins, IV ceftriaxone, Inj. artemether, PCM tabs, immunoboost caps |
| CW020 | F | 8 | O Rh+ | 2 | 2 | 2 | 4/01/15 | 6 | 18.1 | 23.93 | Marked weakness, body pains, anorexia, chest tightness, diarrhoea, stomach pain, cough | IV fluids, vitamins, Inj. ceftriaxone, Inj. Flagyl, PCM tabs, ciprofloxacin tabs |
| Mean ± SD | 18 ± 11.7 | 2 ± 0.8 | 2 | 6.25 ± 2.6 | 21.77 ± 4.9 | 24.4 ± 5.4 | ||||||
| N001 | f | 55 | – | 2 | 2 | 2 | 13/1/15 | 5 | 23.08 | 20.21 | Sore throat, headache, body aches, stomach ache, vomiting, diarrhoea, weakness, hiccupping | IV fluids, vitamins, IV ceftriaxone, Inj. metronidazole, Inj. artesunate, PCM tabs |
| N002 | M | 20 | – | 3 | 1 | 2 | 11/12/14 | 4 | 19.21 | 19.02 | Sore throat, stomach ache, body aches, diarrhoea, anorexia, cough, weakness, red eyes | IV fluids, ceftriaxone, vitamins, PCM tabs, ciprofloxacin tabs |
| N003 | M | 54 | – | 1 | 2 | 2 | 11/12/14 | 4 | 28.32 | 28.20 | Headache, anorexia, vomiting, body aches, weakness, cough, diarrhoea | IV fluids, vitamins, IV ceftriaxone, Inj. metronidazole, PCM tabs, ciprofloxacin tabs |
| N004 | M | 45 | – | 2 | 1 | 2 | 10/1/15 | 8 | 24.81 | 25.03 | Head ache, body aches, rash, weakness, diarrhoea, cough and side pains | IV fluids, vitamins, ceftriaxone, Inj. metronidazole, Inj. artesunate, PCM tabs |
| N005 | F | 6 | – | 1 | 1 | 2 | 19/1/15 | 8 | 21.01 | 21.23 | Weakness, stomach ache, body aches, anorexia, diarrhoea, gum bleeding, restless | IV fluids, vitamins, IV ceftriaxone, Inj. artesunate, Inj. metronidazole, PCM tabs |
| N006 | M | 28 | – | 4 | 2 | 2 | 12/2/15 | 2 | 27.83 | 28.16 | Body aches, weakness, red eyes, cough, anorexia, chest pain, diarrhoea | IV fluids, vitamins, IV ceftriaxone, Inj. metronidazole, Inj. artesunate, PCM tabs |
| N007 | F | 40 | – | 3 | 2 | 2 | 12/2/15 | 3 | 21.60 | 19.01 | Fever, vomiting, weakness, bed ridden, red eyes, diarrhoea | IV fluids, vitamins, IV ceftriaxone, Inj. metronidazole, Inj. artesunate, PCM tabs |
| Mean | 35.4 ± 18.3 | 2.3 ± 1.1 | 1.57 ± 0.5 | 4.86 ± 2.3 | 23.69 ± 3.5 | 22.98 ± 4.1 |
CW: CWB group, N: NCWB group.
Table 3.
CWB and NCWB cases by sex and age.
| Age group | CWB-group |
Non-CWB group |
Fisher exact probability |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Survived | Died | CFR | Survived | Died | CFR | OR | 95% CI | p-Value | |
| 0–17 | 06 | 4 | 40.0% | 01 | 03 | 75.0% | 4.5 | 0.3–60.0 | 0.28 |
| 18–39 | 20 | 04 | 16.7% | 09 | 04 | 30.8% | 2.2 | 0.5–10.9 | 0.28 |
| ≥40 | 06 | 03 | 33.3% | 04 | 04 | 50.0% | 2.0 | 0.28–14.2 | 0.42 |
| Total | 32 | 11 | 25.6% | 14 | 11 | 44.0% | 2.3 | 0.8–6.5 | 0.09 |
| Sex | |||||||||
| Male | 14 | 05 | 26.3% | 07 | 06 | 46.2% | 2.4 | 0.5–10.7 | 0.22 |
| Female | 18 | 06 | 25% | 07 | 05 | 41.7% | 2.1 | 0.5–9.3 | 0.26 |
Patients were considered to have recovered after two negative PCR tests and lack of clinical signs of Ebola.
Discussions
Use of convalescent whole blood for the treatment of EVD is contingent on the availability of viable blood obtained from a willing recovered subject. These conditions could be easily attained even in highly resource-constrained environments that may experience EVD outbreaks. Further, the viability of blood is normally determined by its lack of infectious agents and must not be expired for use in transfusions and must match the blood type of the recipients: these conditions could also be met even under resource-poverty.
Our study provides additional evidence that convalescent whole blood treatment of EVD is viable. Apart from the transfusion that was only given to selected subjects, all subjects were provided treatment at the ETU as described previously.21 The differences in outcome observed in the patients treated with CWB could likely be as a result of the blood therapy. Viral load decreased significantly within the first 24 h of transfusion while viral load did not change significantly in the subjects that did not receive a transfusion. Additionally, the case fatality rate was less in the subjects that had the convalescent whole blood treatment, but higher in the subjects without CWB. The odds ratio for survival with CWB was twice that of NCWB.
On its own, we observed that viral load plays an important part in patient recovery as reported earlier.22 NCWB patients with low viral load recovered (n = 5, Ct value: 31.97) while those with high viral load died (n = 7, Ct value: 23.69) and the survival rate in the NCWB group hinged on reduced viral load and routine care was 40%. On the other hand, we observed that CWB increased survival rate for patients with high viral load, (n = 16, Ct value: 23.37) with a survival rate of 80% (Table 1).
Moreover the overall case fatality rate for CWB patients (n = 43) of 27·9% is lower than the 31% reported by Ansumana et al.21 in 2014 using IV fluids and other supportive treatment and also lower than the 31% risk of death for patients treated with CBP in Guinea.13 However, the case fatality rate of 44% for the NCWB patients is within the range of the CFR for the first 151 subjects treated at Hastings between September 27 and October 13, 2014.21
The reduced fatality from the use of CWB in our study is not as low as the 12.5% case fatality rate reported earlier by Mupapa and colleagues3 but overall, we also report a reduced fatality rate.
Conclusions
Convalescent whole blood appears to be suitable for treating EVD in resource-poor settings, especially in the early phases of outbreaks when resource-mobilization is done.
This study shows that assessment of viral load is important when admitting patients with EVD and in cases of high viral load, treatment with convalescent whole blood is beneficial for the recovery of patients.
Our study is important because it provides additional positive evidence for the use of CBT during an EVD outbreak. The CBT used in this study in Freetown, Sierra Leone, is different from the CBP evaluation report from Guinea, where 31% risk of death in patients and 38% risk of deaths in the control was reported.13 Together both studies show that convalescent blood therapy could be useful in future EVD outbreaks.
This study had several limitations as it was conducted during an emergency. One of the limitations was that it was not randomised and our sample size was relatively smaller compared to the Guinea study.13 Additionally, the subjects were not treated with convalescent whole blood exclusively. Convalescent blood was combined with routine supportive therapy described previously21 and the very low case fatality rate could be due to a synergistic effect of the supportive therapy and CWB. We were unable to get all the Ct values for the subjects because the tests were done offsite of the treatment unit. It is important for future studies to compare the clinical outcome of convalescent whole blood and convalescent blood plasma in treating EVD.
Competing interests
All authors declare that we have no competing interests.
Author contribution
MTA, CB, SF, IBR, RJWB, BS, NS, JW, OO, KO, KP, GO, GSM, FS & RA conceived the study. MTA, CB, SF, IBR, RJWB, BS, NS, JW, OO, KO, KP, GO, GSM, FS collected the data. FS, MTA, RA, JML, analysed the data. RA, FS and MTA drafted the manuscript. All authors reviewed and accepted the manuscript for submission.
Acknowledgements
We acknowledge the services of colleagues at the Ministry of Health and Sanitation, 34 Military Hospital, blood donors and patients that consented to participate in this study. We also acknowledge funders including WHO that provided funding for the study, Sierra Leone Government and others such as DTRA support provided to two of the coauthors were from the Joint Science and Technology Office through the College of Science of George Mason University with GMU sub-award reference: GMU-726-12.
References
- 1.Edmond R.T., Evans B., Bowen E.T., Lloyd G. A case of Ebola virus infection. Br Med J. 1977;2(6086):541–544. doi: 10.1136/bmj.2.6086.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Courtois D. Ebola virus three years later. Med Trop (Mars) 1979;39(6):675–684. [PubMed] [Google Scholar]
- 3.Mupapa K., Massamba M., Kibadi K., Kuvula K., Bwaka A., Kipasa M. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. International Scientific and Technical Committee. J Infect Dis. 1999;179(Suppl. 1):S18–S23. doi: 10.1086/514298. [DOI] [PubMed] [Google Scholar]
- 4.Sadek R.F., Khan A.S., Stevens G., Peters C.J., Ksiazek T.G. Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995: determinants of survival. J Infect Dis. 1999;179(Suppl. 1):S24–S27. doi: 10.1086/514311. [DOI] [PubMed] [Google Scholar]
- 5.Jahrling P.B., Geisbert J.B., Swearengen J.R., Larsen T., Geisbert T.W. Ebola hemorrhagic fever: evaluation of passive immunotherapy in nonhuman primates. J Infect Dis. 2007;196(2):S400–S403. doi: 10.1086/520587. [DOI] [PubMed] [Google Scholar]
- 6.Parry R.P., Tettmar K.I., Hoschler K., Brailsford S.R., Samuel D., Ashford M. Strategies for screening blood donors to source convalesc ent H1N1v plasma for intervention therapy. Vox Sang. 2012;103(2):107–112. doi: 10.1111/j.1423-0410.2012.01599.x. [DOI] [PubMed] [Google Scholar]
- 7.HUBER H.G. [Status of treatment with poliomyelitis convalescent serum] Kinderarztl Prax. 1953;21(7):311–314. [PubMed] [Google Scholar]
- 8.Gundersen T. Convalescent blood for treatment of herpes zoster pphthalmicus: second report. Trans Am Ophthalmol Soc. 1940;38:124–137. [PMC free article] [PubMed] [Google Scholar]
- 9.Wong V.W.S., Dai D., Wu A.K.L., Sung J.J.Y. Treatment of severe acute respiratory syndrome with convalescent plasma. Hong Kong Med J. 2003;9(3):199–201. [PubMed] [Google Scholar]
- 10.Yeh K.M., Chiueh T.S., Siu L.K., Lin J.C., Chan P.K.S., Peng M.Y. Experience of using convalescent plasma for severe acute respiratory syndrome among healthcare workers in a Taiwan hospital. J Antimicrob Chemother. 2005;56(5):919–922. doi: 10.1093/jac/dki346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mair-Jenkins J., Saavedra-Campos M., Baillie K., Cleary P., Khaw F.-M., Lim W.S. The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral aetiology: a systematic review and exploratory meta-analysis. J Infect Dis. 2015;211:80–90. doi: 10.1093/infdis/jiu396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hung I.F., To K.K., Lee C.K., Lee K.L., Chan K., Yan W.W. Convalescent plasma treatment reduced mortality in patients with severe pandemic influenza A (H1N1) 2009 virus infection. Clin Infect Dis. 2011;52(4):447–456. doi: 10.1093/cid/ciq106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Griensven J., Edwards T., de Lamballerie X., Semple M.G., Gallian P., Baize S. Evaluation of convalescent plasma for Ebola Virus Disease in Guinea. N Engl J Med. 2016;374(1):33–42. doi: 10.1056/NEJMoa1511812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Griensven J., De Weiggheleire A., Delamou A., Smith P.G., Edwards T., Vandekerckhove P. The use of Ebola convalescent plasma to treat Ebola Virus Disease in resource-constrained settings: a perspective from the field. Clin Infect Dis. 2016;62(1):69–74. doi: 10.1093/cid/civ680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burnouf T., Seghatchian J. Ebola virus convalescent blood products: where we are now and where we may need to go. Transfus Apher Sci. 2014;51(2):120–125. doi: 10.1016/j.transci.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson J.B., Mejabi P.F., Mejabi O.O., Tejan-Sie S.A. Convalescent serum therapy as rapid advance treatment for Ebola in West Africa. Int J African Dev. 2015;2(2):58–70. [Google Scholar]
- 17.Campbell D.E., Georgiou G.M., Kemp A.S. Pooled human immunoglobulin inhibits IL-4 but not IFN-gamma or TNF-alpha secretion following in vitro stimulation of mononuclear cells with Staphylococcal superantigen. Cytokine. 1999;11(5):359–365. doi: 10.1006/cyto.1998.0435. [DOI] [PubMed] [Google Scholar]
- 18.Qiu X., Wong G., Audet J., Bello A., Fernando L., Alimonti J.B. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature. 2014;514(7520):47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marano G., Vaglio S., Pupella S., Facco G., Catalano L., Liumbruno G.M. Convalescent plasma: new evidence for an old therapeutic tool? Blood Transfus. 2016;14:152–157. doi: 10.2450/2015.0131-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Organization World Health Use of convalescent whole blood or plasma collected from patients recovered from Ebola virus disease for transfusion, as an empirical treatment during outbreaks. Interim Guid Natl Heal Authorities Blood Transfus Serv. 2014:1–19. http://www.who.int/csr/resources/publications/ebola/convalescent-treatment/en/ WHO/HIS/SDS/2014.8. [Google Scholar]
- 21.Ansumana R., Jacobsen K.H., Sahr F., Idris M., Bangura H., Boie-Jalloh M. Ebola in Freetown area, Sierra Leone–a case study of 581 patients. N Engl J Med. 2015;372(6):587–588. doi: 10.1056/NEJMc1413685. [DOI] [PubMed] [Google Scholar]
- 22.Fitzpatrick G., Vogt F., Moi Gbabai O.B., Decroo T., Keane M., De Clerck H. The contribution of Ebola viral load at admission and other patient characteristics to mortality in a Médecins Sans Frontières Ebola Case Management Centre, Kailahun, Sierra Leone, June–October 2014. J Infect Dis. 2015;212(10):1752–1758. doi: 10.1093/infdis/jiv304. [DOI] [PMC free article] [PubMed] [Google Scholar]