Abstract
Objective
To assess the preparedness of emergency departments (EDs) in the United Kingdom (UK) for the management of potential biological incidents.
Methods
We telephoned all hospitals in the UK listed as having a major ED. We surveyed their ED facilities and procedures for managing patients with infectious diseases. We determined how many of the EDs had an isolation room available and, if present, whether this had an independent ventilation system and separate access from outside the ED. In addition, we determined how many of the EDs would isolate patients with suspected cases of chickenpox, tuberculosis (TB), severe acute respiratory syndrome (SARS) and other suspicious infections.
Results
We obtained complete data from 203 (79%) of the 257 hospitals approached. Only 49 (24%) of these hospitals had isolation facilities available in the ED. Of these 49 EDs, 30 (61%) reported an independent ventilation system and 18 (37%) reported a separate access from outside the ED. The majority of EDs would isolate patients with potential infectious diseases, however, 47 (23%) would not isolate patients with suspected chickenpox, 37 (18%) EDS would not isolate patients with suspected TB, 12 (6%) EDS would not isolate patients with suspected SARS and 55 (27%) EDS would not isolate patients with other suspicious infections.
Conclusion
EDs in the UK are not prepared for emerging biological threats and bioterrorism. With current facilities and procedures it is highly likely that an infectious agent will spread to staff and other patients in any future biological incident.
Keywords: Disaster planning, Disease outbreaks, Bioterrorism
Introduction
Concern is growing about the re-emergence of infectious diseases as a significant health threat in the developed world. Periodic natural outbreaks of new and emerging infectious diseases, such as the recent severe acute respiratory syndrome (SARS) outbreak in South East Asia,1 the possibility of an influenza pandemic,2, 3, 4 and the threat of the terrorist use of biological weapons against civilian populations,5, 6 have all led to increasing concern among emergency planners and first responders who may not be prepared to respond safely to such incidents.7, 8, 9, 10
Unlike most health services' major incidents, the onset of a biological incident may be insidious, geographically widespread and may demonstrate features unfamiliar to the clinician. It is therefore essential that the emergency departments (EDs) have facilities and procedures in place to manage patients who may present with features associated with a biological agent. It is highly likely that in any future biological incident patients will present with clinical features suggestive of infectious disease prior to the nature of the biological agent being known.
The objective of this study was to assess current facilities and procedures in EDs in the United Kingdom (UK) for the management of potential biological incidents.
Materials and methods
We telephoned all 261 hospitals in the UK listed as having a major ED in the 2004 directory of the British Association for Emergency Medicine. In the UK a major ED is defined as one that accepts patients 24 h per day, 365 days per year and is staffed by accredited emergency physicians. Major EDs range in size from small district general hospital EDs which see less than 25 000 patients per year to large inner-city EDs which see greater than 100 000 patients per year. As these are the only health care facilities that provide care 24 h per day, 365 days per year they are therefore at greatest risk of receiving patients with potential infectious diseases.
Telephone calls were made to the duty sister/charge nurse or duty shift leader in the ED of each hospital.
An initial approach was made in July 2004. Follow-up telephone calls to initial non-responders were made in October 2004 and December 2004.
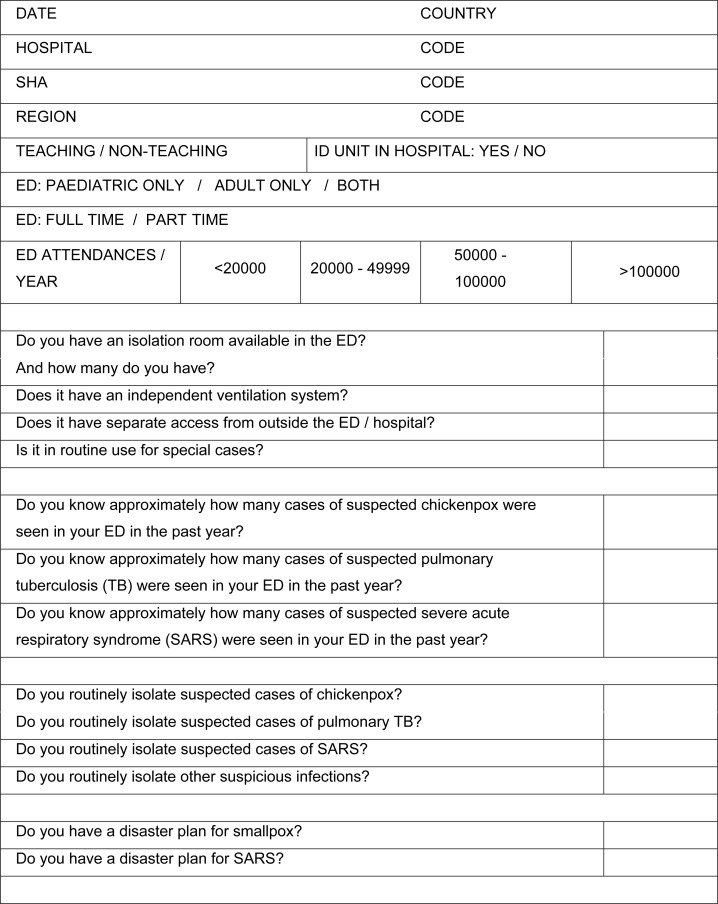
Data were collected using a standardised data collection sheet (Appendix 1).
Data were collected on hospital characteristics, facilities for isolation of patients presenting to the ED with potential infectious diseases, and procedures for the management of patients with known infectious diseases. The questions used were derived from national guidance current in the UK at the time the survey was undertaken and from experts in infectious diseases, public health medicine and emergency medicine.
Results
Four hospitals no longer had major EDs. We obtained complete data from 203 (79%) of the remaining 257 hospitals approached. Only 49 (24%) of these hospitals had isolation facilities available in the ED. Of these 49 EDs 37 (76%) had one isolation room available, seven (14%) had two isolation rooms available, four (8%) had three isolation rooms available and one (2%) had six isolation rooms available. Thirty (61%) reported an independent ventilation system and 18 (37%) reported a separate access from outside the ED. The majority of EDs would isolate patients with potential infectious diseases, however, 47 (23%) would not isolate patients with suspected chickenpox, 37 (18%) EDS would not isolate patients with suspected pulmonary TB, 12 (6%) EDS would not isolate patients with suspected SARS and 55 (27%) EDS would not isolate patients with other suspicious infections.
Results for approximately how many cases of suspected chickenpox, pulmonary tuberculosis (TB) and SARS were seen in EDs in the past year were generally not available and consequently are not reported.
Table 1 shows the facilities and procedures in UK EDs for the management of infectious diseases patients.
Table 1.
The facilities and procedures in United Kingdom emergency departments for the management of infectious diseases patients
| Emergency department (ED) attendances per year | Facilities |
Procedures |
|||||
|---|---|---|---|---|---|---|---|
| Isolation room available | Independent ventilation system if isolation room available | Separate access from outside the ED if isolation room available | Routinely isolate suspected chickenpox cases | Routinely isolate suspected TB cases | Routinely isolate suspected SARS cases | Routinely isolate suspicious infections | |
| <20 000 | 0/7 (0%) | 0/0 (0%) | 0/0 (0%) | 6/7 (86%) | 5/7 (71%) | 5/7 (71%) | 6/7 (86%) |
| 20 000–49 999 | 22/97 (23%) | 15/22 (68%) | 8/22 (36%) | 75/97 (77%) | 79/97 (81%) | 91/97 (94%) | 73/97 (75%) |
| 50 000–100 000 | 26/96 (27%) | 14/26 (54%) | 9/26 (35%) | 73/96 (76%) | 79/96 (82%) | 92/96 (96%) | 67/96 (70%) |
| >100 000 | 1/3 (33%) | 1/1 (100%) | 1/1 (100%) | 2/3 (67%) | 3/3 (100%) | 3/3 (100%) | 2/3 (67%) |
| Total | 49/203 (24%) | 30/49 (61%) | 18/49 (37%) | 156/203 (77%) | 166/203 (82%) | 191/203 (94%) | 148/203 (73%) |
Discussion
Statement of principal findings
This survey has shown that the majority of EDs in the UK do not have isolation facilities available for the management of patients with potential infectious diseases; even when isolation facilities are available they may be of an inadequate standard. In addition, significant numbers of EDs do not have adequate infection control procedures for the management of patients presenting with known infectious diseases that may mimic a more serious biological incident.
Strengths and weaknesses of the study
We chose to telephone a senior member of operational nursing staff rather than to formally write to each ED as we felt that this was more likely to reveal the true departmental response. It is possible that some of the EDs reporting no infection control procedures for the management of patients presenting with known infectious diseases do in fact have such procedures; however, if these are not known to the senior nursing staff then they are clearly ineffective. As with all studies of this type we have only been able to assess what people say that they will do rather than what they will do in practice. However, we see no reason why those contacted would deliberately under report their EDs response. While up to three approaches were made to collect data there is no reason to suspect ‘survey fatigue’ since the answers were sought from the duty sister/charge nurse or duty shift leader in the ED of each hospital rather than from a specific individual.
We chose chickenpox (varicella) as a marker of preparedness in light of its infectivity and its potential for confusion with smallpox (variola) early in the course of the disease.11 In the ED, isolation is the single most important intervention in patients in whom variola infection is suspected. Pulmonary TB was chosen as a marker of preparedness in light of its increasing prevalence and the emergence of multiple drug-resistant TB. National guidelines have been available for some time regarding the management of multiple drug-resistant TB12 and are currently being reviewed by the National Institute for Health and Clinical Excellence (NICE),13 although specific guidance about the isolation of patients in the ED has not been included. Specific questions regarding SARS were asked as we sought to determine how recent guidance from the Health Protection Agency for the management of SARS14 had been implemented in practice. The SARS guidance at the time stated that patients should be managed by appropriately protected staff in an isolation setting with an independent ventilation system and with a separate access from the main ED or Medical Assessment Unit (MAU). Any future influenza pandemic is likely to present in a similar way to SARS and similar precautions are advocated for cases of avian influenza.15
Strengths and weaknesses in relation to other studies, discussing particularly any differences in results
We are unaware of any other assessments of UK preparedness for biological incidents. Our findings are in keeping with assessments of UK preparedness for other types of major incident.16, 8, 9, 10
Meaning of the study: possible mechanisms and implications for clinicians or policymakers
The current availability of appropriate isolation facilities in EDs is inadequate. Such facilities must be provided to improve health services capability to manage patients with potential infectious diseases. The provision of new-build isolation facilities in all EDs is an expensive solution and would take a considerable time period to achieve. The designation (rather than dedication) of existing areas within EDs as potential isolation facilities is a less ideal but more easily achieved solution and all hospitals should be encouraged to undertake this exercise. In prolonged biological incidents mobile isolation facilities could be delivered to affected hospitals. However, this can only be achieved after the initial outbreak and does not address the underlying ED problem.
At times of heightened risk, such as the possibility of an influenza pandemic or the threat of bioterrorism, the first step to ensure an appropriate response is to raise awareness. The true first responders in a biological incident are the health care workers in EDs and other primary health care facilities.17 They must be made aware of the relevant signs and symptoms and taught to react appropriately. The Health Protection Agency has prepared educational material and training courses to improve the ability of health care workers from a variety of backgrounds to deal with biological incidents.18 However, these must be delivered to all front line staff, especially triage nurses in EDs, so that they can identify the effects of at least some of the most likely biological agents. A nationally funded training standard, the Structured Approach to Chemical Casualties course, has previously been successfully cascaded down to all EDs to improve preparedness for chemical incidents.19, 20 Once a biological incident is identified, be it natural, accidental or deliberate, a wider range of issues must be managed.21
Unanswered questions and future research
Our study can only demonstrate what persons say that they will do, not what they will do in practice. Such questions can only be answered by observational research to see how and where patients with potential infectious diseases are assessed in the emergency setting and if infection control guidelines are adhered to.
Acknowledgement
We wish to thank Dr Jennifer Hill for discussions that led to this study being undertaken.
Appendix 1.
References
- 1.World Health Organisation . World Health Organisation; Geneva: 2004. WHO guidelines for the global surveillance of severe acute respiratory syndrome (SARS)<http://www.who.int/csr/resources/publications/WHO_CDS_CSR_ARO_2004_1.pdf> Updated recommendations 2004. [accessed 18.11.05] [Google Scholar]
- 2.Department of Health . Department of Health; London: October 2005. UK Health Departments' influenza pandemic contingency plan.<http://www.dh.gov.uk/assetRoot/04/12/17/44/04121744.pdf> [accessed 18.11.05] [Google Scholar]
- 3.World Health Organisation . World Health Organisation; Geneva: 2005. WHO global influenza preparedness plan.<http://www.who.int/csr/resources/publications/influenza/WHO_CDS_GIP_2005_5.pdf> [accessed 18.11.05] [Google Scholar]
- 4.World Health Organisation . World Health Organisation; Geneva: 2005. Avian influenza: assessing the pandemic threat.<http://www.who.int/csr/disease/influenza/H5N1-9reduit.pdf> [accessed 18.11.05] [Google Scholar]
- 5.Beeching N.J., Dance D.A.B., Miller A.R.O., Spencer R.C. Biological warfare and bioterrorism. British Medical Journal. 2002;324:336–339. doi: 10.1136/bmj.324.7333.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Chief Medical Officer . Department of Health; London: 2002. Getting ahead of the curve: a strategy for combating infectious diseases (including other aspects of health protection)<http://www.dh.gov.uk/assetRoot/04/06/08/75/04060875.pdf> [accessed 18.11.05] [Google Scholar]
- 7.The Royal Society . The Royal Society; London: 2004. Making the UK safer: detecting and decontaminating chemical and biological agents.<http://www.royalsociety.org/displaypagedoc.asp?id=5689> [accessed 18.11.05] [Google Scholar]
- 8.National Audit Office . The Stationery Office; London: 2002. Facing the challenge: NHS emergency planning in England.<http://www.nao.org.uk/publications/nao_reports?02–03?020336.pdf> [accessed 18.11.05] [Google Scholar]
- 9.House of Commons Defence Committee . Defence and security in the UK. The Stationery Office; London: 2002. Sixth report of session 2001–2002.<http://www.parliament.the-stationery-office.co.uk/pa/cm200102/cmselect/cmdfence/518/518.pdf> [accessed 18.11.05] [Google Scholar]
- 10.Carley S., Mackway-Jones K. Are British hospitals ready for the next major incident? Analysis of hospital major incident plans. British Medical Journal. 1996;313:1242–1243. doi: 10.1136/bmj.313.7067.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American College of Physicians. Bioterrorism – variola (smallpox) and its mimics. <http://www.acponline.org/bioterro/smallpox_mimics.htm> [accessed 18.11.05].
- 12.The Interdepartmental Working Group on Tuberculosis . Department of Health; London: 1998. The prevention and control of tuberculosis in the United Kingdom: UK guidance on the prevention and control of transmission of 1. HIV-related tuberculosis 2. Drug-resistant, including multiple drug-resistant, tuberculosis.<http://www.dh.gov.uk/assetRoot/04/11/52/99/04115299.PDF> [accessed 18.11.05] [Google Scholar]
- 13.National Institute for Health and Clinical Excellence . National Institute for Health and Clinical Excellence; London: 2005. Tuberculosis: National clinical guideline for diagnosis, management, prevention and control. Draft for second consultation.<http://www.nice.org.uk/pdf/TB_fullguideline_2nd_consultation.pdf> [accessed 18.11.05] [Google Scholar]
- 14.Health Protection Agency . Health Protection Agency; London: 2004. SARS – hospital infection control guidance.<http://www.hpa.org.uk/infections/topics_az/SARS/pdfs/hosp_infect_cont.pdf> [Reviewed on 11th January 2005] [accessed 18.11.05] [Google Scholar]
- 15.World Health Organisation . World Health Organisation; Geneva: 2004. Influenza A (H5N1): WHO interim infection control guidelines for health care facilities.<http://www.who.int/csr/disease/avian_influenza/guidelines/Guidelines_for_health_care_facilities.pdf> [accessed 18.11.05] [Google Scholar]
- 16.The Royal Society . The Royal Society; London: 2004. Making the UK safer: detecting and decontaminating chemical and biological agents.<http://www.royalsociety.org/displaypagedoc.asp?id=5689> [accessed 18.11.05] [Google Scholar]
- 17.Ollerton J.E. Emergency department response to the deliberate release of biological agents. Emergency Medicine Journal. 2004;21:5–8. doi: 10.1136/emj.2003.005439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Health Protection Agency. Emergency preparedness and response training programme. <http://www.hpa.org.uk/emergency/training.htm> [accessed 18.11.05].
- 19.Crawford I., Mackway-Jones K., Murray V. Preparedness of London hospitals for a chemical weapons attack. Lancet. 2003;361:1474–1475. doi: 10.1016/S0140-6736(03)13118-2. [DOI] [PubMed] [Google Scholar]
- 20.Crawford I.W.F., Mackway-Jones K., editors. The structured approach to chemical casualties. 2nd ed. Advanced Life Support Group; Manchester: 2002. [Google Scholar]
- 21.Tham K. An emergency department response to severe acute respiratory syndrome: a prototype response to bioterrorism. Annals of Emergency Medicine. 2004;43:1–9. doi: 10.1016/j.annemergmed.2003.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]