Summary
Objectives
Primary care is thought to bear half the cost of treating infections in the UK. We describe the seasonal variation in NHS Direct respiratory calls (a new source of primary care data) and estimate the contribution of specific respiratory pathogens to this variation.
Methods
Linear regression models were used to estimate the weekly contribution of specific respiratory pathogens to the volume of NHS Direct respiratory calls (England and Wales, 2002–2004, all ages and 0–4 years).
Results
Annual peaks in NHS Direct cough and difficulty breathing calls occurred in late December, with peaks in ‘cold/flu’ and fever calls occurring between November and April. The main explanatory variables were influenza (estimated to account for 72.5 calls per 100,000/year; 22% of ‘cold/flu’ calls; 15% of cough; and 13% of fever) and Streptococcus pneumoniae (55.5 per 100,000; 33% of ‘cold/flu’ calls; 20% of cough; and 15% of fever (0–4 years)).
Conclusions
It is estimated that respiratory viruses, notably influenza and RSV, are responsible for at least 50% of the seasonal variation in NHS Direct respiratory calls. These results provide estimates of the burden of specific respiratory diseases reported to NHS Direct, and will help interpret syndromic surveillance data used to provide early warning of rises in community morbidity.
Keywords: NHS Direct, Respiratory pathogens, Seasonality, Linear regression, Influenza, Streptococcus pneumoniae, Syndromic surveillance
Introduction
Primary care is thought to bear over half the cost of treating infections in the UK (£6 billion per year) with 5.5 million GP consultations for respiratory infections alone.1 NHS Direct2 a nurse led national telephone health helpline established in 1999, provides the opportunity to examine a new source of reported respiratory disease in England and Wales, some of which may go unrecorded by traditional information and surveillance systems (GP and hospital). Published work about NHS Direct ‘respiratory’ calls suggests that some of the temporal variation may be related to the seasonality of influenza.3 Many other pathogens (viral and bacterial) may cause respiratory disease, however, and the relative contribution of these pathogens to NHS Direct calls has not been estimated. Describing and quantifying the burden of respiratory disease is necessary to identify health priorities and provide evidence to support future research and development.
Annual rises in respiratory diseases such as influenza, the emergence of new infections such as SARS and ‘avian flu’, and the potential of bio-terrorist attacks to cause widespread disease, means timely and representative disease surveillance data are desirable. NHS Direct call centre data have been monitored for surveillance purposes since 2001 (the NHS Direct Syndromic Surveillance System4) in order to provide early warning of a rise in community morbidity. Syndromic surveillance systems use a variety of pre-diagnostic data sources (e.g. ambulance encounters,5 A&E admissions,6 pharmacy sales,7 calls to health help-lines4 in an attempt to identify outbreaks and incidents of public health importance. Although NHS Direct syndromic data have alerted public health teams to national or local rises in illness 4 there is no mechanism for routine microbiological confirmation of the cause of NHS Direct calls about presumed infections. Comparison of trends in NHS Direct calls against laboratory reports may, therefore, help elucidate a likely cause of NHS Direct respiratory calls, and help interpret surveillance trends.
In this report we describe the seasonal variation in NHS Direct respiratory calls and use a multiple linear regression model to estimate the contribution of different respiratory pathogens to this variation. A similar technique has been used previously to estimate the contribution of respiratory syncytial virus (RSV) and other respiratory pathogens to hospital admissions for lower respiratory tract infections,8 and the contribution of pneumococcal disease to GP consultations.9
Methods
Weekly counts of NHS Direct calls about ‘cold/flu’ (CF), cough (C), fever (F), and difficulty breathing (DB) in England and Wales were extracted from the NHS Direct syndromic surveillance database for the period from October 2002 to October 2004 (all ages and 0–4 years separately). The appropriateness of classifying fever as a respiratory call is discussed later. NHS Direct data for cough calls (0–4 years) were only available for December 2002–October 2004 and difficulty breathing calls (0–4 years) for April 2003–October 2004. There are no formal case definitions for NHS Direct respiratory syndromes (as symptoms are self-reported and triaged remotely) and data extraction was based on the clinical algorithms (‘cold/flu’, ‘cough’, ‘fever’ or ‘difficulty breathing’) selected by the NHS Direct nurses handling the calls.
Weekly counts of laboratory reports (by earliest specimen date) of the following main causes of respiratory disease were extracted from the Health Protection Agency Centre for Infections database of laboratory reports for England and Wales (LabBase), from October 2002 to October 2004 (all ages and 0–4 years separately):
Respiratory syncytial virus (RSV)
Influenza
Parainfluenza
Rhinovirus
Adenovirus
Coronavirus
Invasive Streptococcus pneumoniae
Mycoplasma pneumoniae
Klebsiella pneumoniae
Coxiella burnetii
Legionella species
Bordetella pertussis
Invasive Haemophilus influenzae
Chlamydia pneumoniae
Chlamydia psittaci
Moraxella catarrhalis
LabBase is a national HPA Centre for Infections database that collects laboratory reports of all micro-organisms isolated at approximately 400 NHS and other laboratories throughout England, Wales, and Northern Ireland. Although enhanced and separate community surveillance systems exist for some pathogens (e.g. influenza,10 legionella11) a single source of laboratory data was preferred to reduce selection bias between different systems.
For each pathogen we compared trends in laboratory reports for all ages and 0–4 years. If both age groups exhibited a similar seasonality then all ages data were used to make the seasonal pattern more distinct. Two binary dummy variables (‘Christmas bank holiday week’ and ‘other public holiday weeks’) were created to account for excess out-of-hours demand for NHS Direct during public holiday periods (i.e. when many GP surgeries are closed).
Using methods previously described,12 multiple linear regression models were constructed to estimate the weekly proportion of NHS Direct respiratory calls (all ages and 0–4 years separately) attributable to respiratory pathogens (explanatory variables) (SPSS v13.0 was used). This method uses a regression model to estimate how the seasonal variation in laboratory reports is reflected within the variation in NHS Direct calls. Linear regression models assume that the relationship between the dependent and explanatory variables is linear and that the model errors are distributed normally and do not exhibit serial correlation. A constant number of NHS Direct calls due to other infectious or non-infectious disease (other causes) was assumed within each model. Variables that contributed little to the model were removed by backward stepwise regression. This technique gradually removes the variable that causes the smallest reduction in R 2 (goodness of fit of the model) until removal of a further variable causes a significant reduction in R 2 (by the F-test). Once non-significant variables were removed, any remaining significant variables with negative coefficients were also removed from the model as it was considered biologically implausible that they negatively influence the number of NHS Direct calls. The model was then re-estimated with the remaining variables (Model1). Possible model misspecification was tested by constructing alternative models to examine the changes in coefficients of the final model (Model1) to sequential deletion of significant variables. Model residuals were examined for autocorrelation.
Estimates were made of the proportion of NHS Direct calls attributable to each significant respiratory pathogen over the 2 year period and by week. We also estimated the proportion of NHS Direct calls attributable to influenza and RSV during periods of high activity (influenza and RSV ‘seasons’). Influenza seasons were defined as continuous periods during which the weekly number of influenza reports exceeded 10 (this accounted for 92% of total influenza reports). RSV seasons were continuous periods when the weekly number of RSV reports exceeded 100 (87% of total RSV reports). From the estimated proportion of calls about specific pathogens, the estimated incidence per 100,000 of NHS Direct calls due to specific pathogens was calculated for England and Wales.
Results
NHS Direct respiratory calls
Between October 2002 and October 2004 there were 601,454 calls about the four respiratory syndromes, 45% classified as fever, 32% cough, 13% difficulty breathing and 10% cold/flu ( Table 1). These four syndromes comprised 8% of total NHS Direct calls. Of the 292,867 respiratory calls about children under 5 years, 62% were classified as fever, 29% cough, 8% difficulty breathing and 1% cold/flu. There were two peaks in calls about cold/flu and fever occurring in February–April 2003 and November 2003. Peaks in cough and difficulty breathing calls occurred at the end of December (week 52) during 2002 and 2003.
Table 1.
Numbers of NHS Direct calls for respiratory symptoms/syndromes in England and Wales (October 2002–October 2004)
| NHS Direct symptom/syndrome | Number of calls (all ages) | Number of calls (0–4 years) |
|---|---|---|
| Fever | 272812 | 182972 |
| Cough | 190578 | 83476a |
| Difficulty breathing | 77317 | 22471b |
| Cold/flu | 60747 | 3948 |
| Total | 601454 | 292867 |
Data for cough calls (0–4 years) from weeks 52/02 to 45/04.
Data for difficulty breathing calls (0–4 years) from weeks 15/03 to 45/04.
Laboratory reports of respiratory pathogens
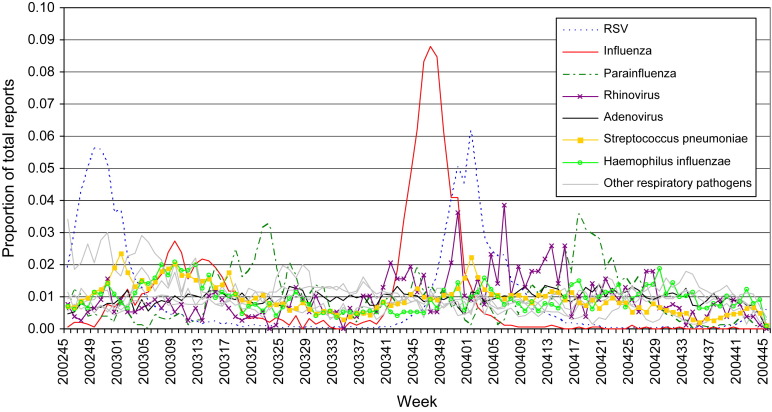
For the 2 year period there were 49,652 laboratory reports, 20,257 (41%) of which were about children under 5 years. RSV was the most commonly recorded pathogen for all ages (13,544 reports) and children under 5 years (8048). The seasonality of respiratory pathogens varied between those with distinct winter peaks (e.g. RSV, weekly range 1–835 reports) ( Fig. 1) and those with no clear seasonality (e.g. adenovirus, range 22–70 reports).
Figure 1.
Weekly variation in laboratory reports of respiratory pathogens (October 2002–October 2004), displayed as a proportion of total reports for each pathogen. (Pathogens that significantly influenced the models are colour coded; pathogens with <100 reports per year are not displayed).
Model results
The models explained 79%, 91%, 71% of the seasonal variation in cold/flu (Model CF1), cough (Model C1), fever (Model F1) ( Table 2). For the 0–4 year age group, the models explained 88% of the variation in cough calls (Model C1 (0–4 years)) and 76% of the variation in fever calls (Model F1 (0–4 years)) (Table 2). Model CF1 (0–4 years) explained 75% of the variation on cold/flu calls. However, the NHS Direct cold/flu clinical algorithm is rarely used to handle calls about children under 5 years (averaging only 37 calls per week in England and Wales) so full results of Model CF1 (0–4 years) are not presented in Table 2. Detailed results of the difficulty breathing models are also not reported as the power of both models was low (Model DB1: R 2 = 0.23, Model DB (0–4 years): R 2 = 0.48).
Table 2.
Estimated proportion (%) of NHS Direct respiratory calls attributable to specific pathogens for England and Wales (October 2002–October 2004), and the sensitivity of the model results (R2)
| Pathogen | Cold/flu calls (all ages) |
Cough calls (all ages) |
Cough calls (0–4 years) |
Fever (all ages) |
Fever (0–4 years) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model CF1 final model | Model CF2 | Model CF3 | Model C1 final model | Model C2 | Model C3 | Model C1 (0–4 years) final model | Model C2 (0–4 years) | Model C3 (0–4 years) | Model F1 final model | Model F1 (0–4 years) final model | Model F2 (0–4 years) | |
| Influenza | 22 | 25 | 26 | 15 | 17 | – | 19 | 20 | 23 | 13 | 13 | 14 |
| RSV | – | – | – | 12 | 15 | 18 | 16 | 17 | – | – | – | – |
| Rhinovirus | 8 | 10 | – | 6 | – | – | 10 | – | – | – | – | – |
| Parainfluenza | – | – | – | – | – | 6 | – | – | – | – | – | |
| Streptococcus pneumoniae | 33 | – | – | 20 | – | – | – | – | – | 19 | – | |
| Haemophilus influenzae | – | – | – | – | – | – | – | – | – | 19 | – | – |
| Mycoplasma pneumoniae | – | – | – | – | – | 3 | – | – | – | – | – | |
| Christmas and other bank holidays | – | – | – | 3 | 4 | 2 | 2 | 2 | 2 | – | – | – |
| Other causes | 37 | 65 | 74 | 43 | 64 | 80 | 44 | 61 | 75 | 68 | 68 | 86 |
| R2 | 0.79 | 0.72 | 0.71 | 0.91 | 0.87 | 0.50 | 0.88 | 0.86 | 0.54 | 0.71 | 0.76 | 0.68 |
Estimated contribution of respiratory pathogens to NHS Direct calls
Table 2 presents the estimated proportion of NHS Direct calls attributable to specific respiratory pathogens. The best-fitting parsimonious model suggested that over the 2 year period, influenza accounted for 22% of cold/flu calls (all ages), 15% of cough calls (all ages), 19% of cough calls (0–4 years), 13% of fever calls (all ages) and 13% of fever calls (0–4 years), with RSV accounting for 12% and 16% of cough calls (all ages and 0–4 years). The contribution of influenza and RSV to NHS Direct respiratory calls, however, was confined mainly to the influenza season (weeks 51/02–19/03 and 41/03–02/04) and RSV seasons (45/02–05/03 and 47/03–09/04) ( Figure 2, Figure 3, Figure 4). During the two influenza seasons influenza was estimated to account for 25% and 51% of cold/flu calls (all ages), and 17% and 41% of fever calls (0–4 years). RSV accounted for 19% and 37% of cough calls (all ages) and 25% and 38% of cough (0–4 years) during successive RSV seasons. The other main contributory variable was S. pneumoniae, estimated to account for 33% of cold/flu calls (all ages), 19% of fever calls (0–4 years), and 20% of cough calls (all ages) over 2 years.
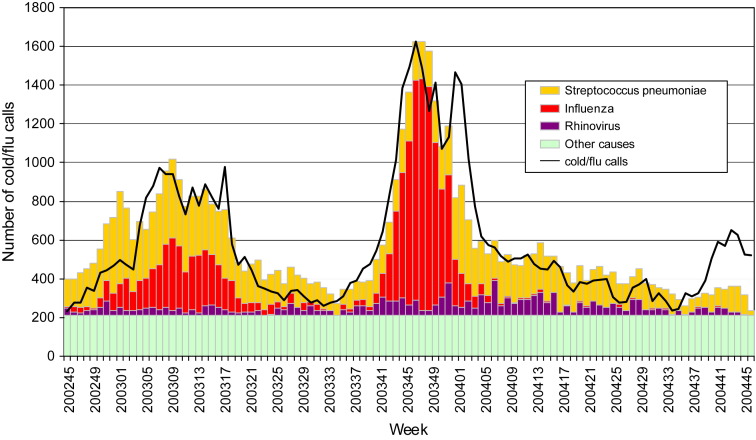
Figure 2.
Comparison of the observed number of NHS Direct ‘cold/flu’ calls (all ages) with the estimated numbers due to influenza, Streptococcus pneumoniae, rhinovirus and other causes (October 2002–October 2004) (model CF1).
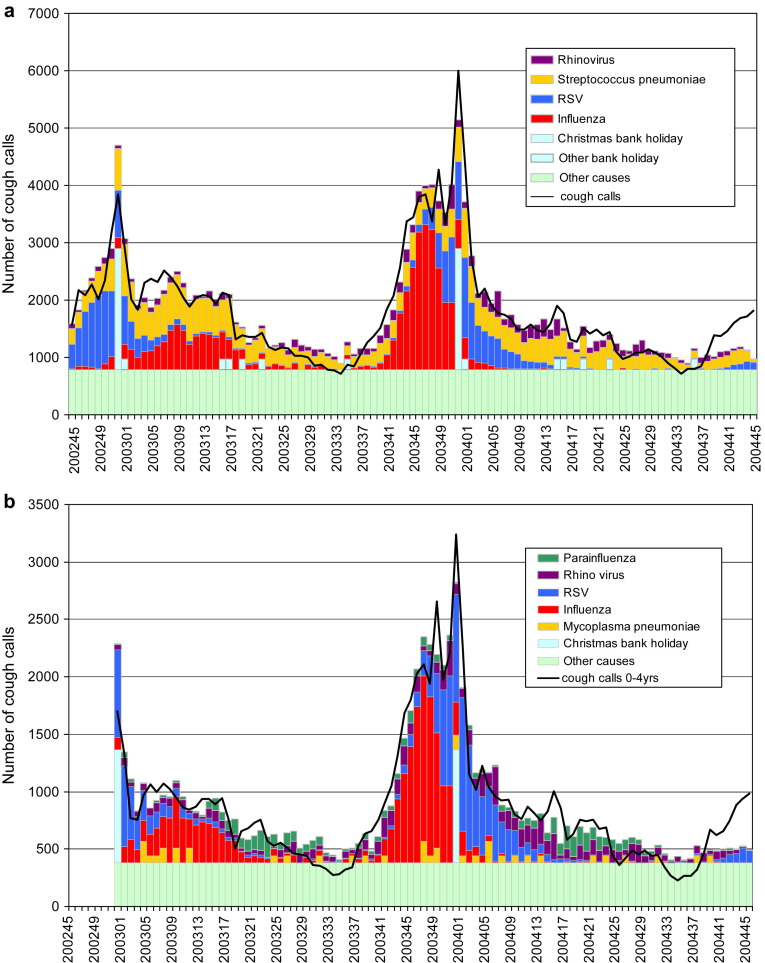
Figure 3.
(a) Comparison of the observed number of NHS Direct cough calls (all ages) with the estimated numbers due to influenza, RSV, Streptococcus pneumoniae, rhinovirus, bank holidays and other causes (October 2002–October 2004) (model C1). (b) Comparison of the observed number of NHS Direct cough calls (0–4 years) with the estimated numbers due to influenza, RSV, Mycoplasma pneumoniae, rhinovirus, parainfluenza, bank holidays and other causes (October 2002–October 2004) (model C1 (0–4 years)).
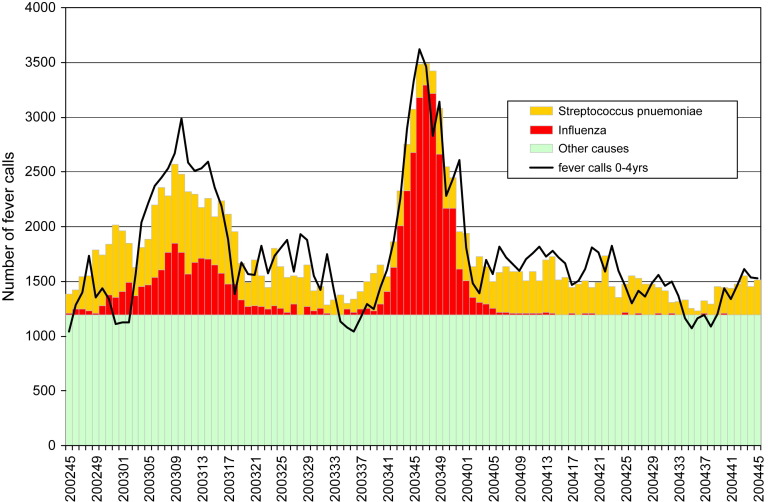
Figure 4.
Comparison of the observed number of NHS Direct fever calls (0–4 years) with the estimated numbers due to influenza, Streptococcus pneumoniae and other causes (October 2002–October 2004) (model F1).
Figure 2, Figure 3, Figure 4 show the weekly estimates of the contribution of respiratory disease pathogens to NHS Direct cold/flu calls, cough calls (all calls and 0–4 years separately), and fever calls (0–4 years). They illustrate the relatively high but short lived contribution of influenza and RSV during seasonal bursts, and the year round contribution, with December/January peaks, of S. pneumoniae. The model estimates generally corresponded to the observed number of NHS Direct calls, although the cold/flu and cough models provided poor estimates for weeks 39/04 to 45/04 (Figs. 2 and 3a,b).
There appeared to be little confounding between diseases with similar seasonality and clinical presentation (e.g. influenza and RSV) as removing either of these variables from the final models resulted in only minor increases in the estimated contribution of the remaining variables. For example, dropping RSV, rhinovirus and parainfluenza from model C1 (0–4) led to a small estimated increase in the contribution of influenza from 19% to 23% (model C3 (0–4)) (Table 2).
Estimated incidence
The estimated mean annual incidence of NHS Direct respiratory calls (cold/flu + cough + fever calls) attributable to influenza was 72.6 per 100,000, and to S. pneumoniae (cold/flu + cough) 55.5 per 100,000 ( Table 3). The estimated incidence of NHS Direct cough calls attributable to RSV was 21.3 per 100,000. NHS Direct respiratory calls about children under 5 years attributable to influenza were estimated to be 630.9 per 100,000, 210.2 per 100,000 for RSV and 565.5 per 100,000 for S. pneumoniae.
Table 3.
Estimated annual incidence of NHS Direct respiratory calls due to specific pathogens (per 100,000 with 95% confidence intervals) for England and Wales (October 2002–October 2004)
| Cold/flu (all ages) |
Cough (all ages) |
Fever (all ages) |
Total (all ages) | Cold/flu (0–4 years) |
Cough (0–4 years) |
Fever (0–4 years) |
Total (0–4 years) | |
|---|---|---|---|---|---|---|---|---|
| Model CF1 | Model C1 | Model F1 | Model CF1 (0–4 years) | Model1 (0–4 years) | Model F1 (0–4 years) | |||
| Influenza | 12.8 (11.2–14.5) | 27.2 (23.9–30.4) | 32.6 (28.3–36.9) | 72.6 (63.4–81.8) | 16.3 (13.9–18.7) | 247.1 (213.3–280.5) | 367.5 (321.4–413.9) | 630.9 (548.6–713.1) |
| RSV | – | 21.3 (17.2–25.4) | – | 21.3 (17.2–25.4) | 7.3 (4.6–10.2) | 202.9 (161.4–244.4) | – | 210.2 (166–254.6) |
| Streptococcus pneumoniae | 19.1 (12.7–25.5) | 36.2 (21.6–50.6) | – | 55.5 (34.3–76.1) | 23.5 (14.1–32.8) | – | 542 (360.2–723.8) | 565.5 (374.3–756.6) |
| Haemophilus influenzae | – | – | 48.9 (29.6–68.2) | 48.9 (29.6–68.2) | – | – | – | – |
| Mycoplasma pneumoniae | – | – | – | – | – | 39.3 (4.8–73.9) | – | 39.3 (4.8–73.9) |
| Rhinovirus | 4.4 (0.5–8.1) | 11.2 (3.1–19.2) | – | 15.6 (3.6–27.3) | – | 126.6 (39.8–213.4) | – | 126.6 (39.8–213.4) |
| Parainfluenza | – | – | – | – | – | 81.5 (10.7–152.3) | – | 81.5 (10.7–152.3) |
Discussion
Annual peaks in NHS Direct cough and difficulty breathing calls occurred in late December, whereas peaks in cold/flu and fever calls were less predictable and occurred between November and April. The regression models estimated that at least half of the seasonal variation in NHS Direct respiratory calls was due to the seasonality of influenza and RSV. During short lived winter periods, influenza and RSV accounted for half of the NHS Direct calls about cold/flu, cough and fever. Rhinovirus accounted for a tenth of cold/flu and cough calls, distributed evenly throughout the year, with parainfluenza estimated to account for a quarter of cough calls (0–4 years) during spring. The main bacterial cause of NHS Direct respiratory calls was S. pneumoniae, with an estimated year round contribution, peaking during mid-winter. The cough models demonstrated the importance of incorporating a bank holiday factor when modelling NHS Direct call data and provide evidence that closure of GP surgeries during bank holidays stimulates acute demand for NHS Direct: a third of all cough calls during Christmas week were accounted for by this bank holiday effect.
Although a good fit was achieved for the final cold/flu, fever and cough models, methodological problems were encountered. Dropping variables with negative coefficients from the models before re-estimating is an inelegant approach to multiple linear regression. Resulting bias due to this is considered negligible, however, as the removal of these variables did not greatly alter the values of the significant positive coefficients (e.g. RSV, influenza, S. pneumoniae) in the final models. The statistical models described here use laboratory data which are subject to case ascertainment bias. For example, common causes of respiratory infections (e.g. coronavirus,13 and human metapneumovirus14) that peak during winter, are rarely tested for and are therefore present in low numbers within LabBase. These pathogens do contribute to the intercept (other causes), however, and are therefore implicitly included within our models. Consequently, over estimation of the contribution of significant variables (e.g. RSV, influenza, and S. pneumoniae) is considered negligible.
The low sensitivity of the two difficulty breathing models (R 2 = 0.23 and 0.48) may have been improved by adding environmental factors (e.g. pollen, air quality) as explanatory variables. This could also have improved the model estimates of the number of cough calls during October–November 2004, when large model residuals were encountered. Previous work has implicated environmental pollutants in sudden increases in difficulty breathing calls15 and further work is needed to explore non-microbiological influences on NHS Direct respiratory calls. Not surprisingly, we noted a relatively high estimated proportion of fever calls due to other causes (>60% in models F1 and F1 (0–4 years)), which are likely to be caused by a variety of exanthema, gastrointestinal illness and other diseases.
NHS Direct currently handles approximately 7 million clinical calls per year compared to 190 million GP consultations16 and 14 million A&E admissions in England and Wales.17 The estimates of specific respiratory diseases reported to NHS Direct provide additional baseline data to be placed alongside GP and hospital data when assessing the burden of disease and evaluating the potential impact of vaccination strategies (e.g. for pneumococcal vaccine18). The results highlight the importance of influenza, RSV and S. pneumoniae infections in respiratory symptoms reported to NHS Direct, supporting previous work showing these diseases also impact substantially on GP consultations9, 19 and hospitalisations8, 14 in the UK. The contribution of S. pneumoniae disease to NHS Direct respiratory calls (an estimated 92,000 calls per year; one-sixth of total NHS Direct respiratory calls) compares to an estimated 700,000 annual GP consultations (approximately 25% of community acquired pneumonia (CAP) and otitis media),9 and 29% of patients admitted to hospital with CAP20 (20% for children under 5 years8). The NHS Direct estimate is likely to be lower because the NHS Direct denominator (total respiratory calls) covers a wider and potentially milder spectrum of disease than the GP denominator (GP CAP and otitis media) and hospital denominator (admissions for CAP).
With regard to influenza, a pilot study has demonstrated that when NHS Direct callers self-sampled for influenza and posted diagnostic samples to a central laboratory over a 3 month winter period, 16% had laboratory confirmed influenza, with positivity rising above 30% during peak weeks.21 These data support our model estimates (one in three cold/flu calls attributable to influenza during the flu season). Perhaps it is not surprising that an adult suffering from what they consider to be an unusually severe respiratory illness (likely to be more than a common cold) will phone NHS Direct. Common respiratory viruses that cause mild to moderate upper respiratory infections had a smaller estimated contribution to NHS Direct calls (e.g. rhinovirus) or were not significant within our models (e.g. adenovirus). Finally, the two winters covering the study period were characterised by low levels of influenza activity.22, 23 The estimated contribution of influenza to NHS Direct respiratory calls, 13–22% during our study, is dependent on epidemiological conditions and would be greater during years with more virulent strains of influenza.
The weekly estimates of the contribution of different pathogens to NHS Direct respiratory calls will provide greater confidence in interpreting sudden rises in calls detected through syndromic surveillance. For example, a sharp rise in cold/flu calls from adults and/or rise in fever calls about children may represent an increase in influenza circulating in the community. A rise in cough calls during November/December may indicate a rise in RSV and also influenza; a rise during January to March suggest only influenza; and a rise during spring may indicate a rise in parainfluenza infections. The use of this intelligence within the NHS Direct syndromic surveillance system will complement other primary care surveillance systems: the weekly returns service of the RCGP10 and the newly established Q-Research system.24 These pathogen specific estimates may also be of use for NHS winter planners in managing elective hospital admissions and in informing the health service of impending problems. Similarly, analysis of emergency department respiratory syndrome data in the US suggests these data could be a useful early indicator of influenza and RSV circulation.25
This work has provided a detailed weekly picture of the type of respiratory infections, throughout the year, that cause people to phone NHS Direct. This has implications for the advice offered by NHS Direct nurses in handling respiratory calls (currently 8% of total symptomatic calls). The supporting clinical advice and rationales within the decision support system used by NHS Direct nurses (NHS CAS) can be modified to reflect awareness of the prevailing respiratory infections. For example, this would include specific advice on seeking urgent help in the event of RSV being the likely cause of significant acute respiratory impairment in a child (bronchiolitis).
Conclusion
In this report we have described the seasonality of NHS Direct respiratory calls and have used a relatively straightforward modelling technique to estimate the proportions of NHS Direct calls attributable to specific microbiological causes. This suggests that at least half of the variation in NHS Direct respiratory calls is explained by the seasonality of common respiratory viruses, notably influenza and RSV. There is also a significant year round contribution of S. pneumoniae infections, peaking during winter. The results of this work will be used to provide detailed estimates of the burden of specific respiratory diseases reported to NHS Direct; advise NHS Direct on the timing and aetiology of respiratory calls; and help interpret syndromic surveillance data used to provide early warning of community rises in respiratory infections.
Acknowledgements
We would like to thank NHS Direct for providing NHS Direct call data and Neville Verlander of the Health Protection Agency Centre for Infections for advice on the statistical aspects of this work.
References
- 1.Health protection in the 21st Century: understanding the burden of disease; preparing for the future. Health Protection Agency. 2005 [Google Scholar]
- 2.NHS Direct Online. Available from http://www.nhsdirect.nhs.uk/
- 3.Cooper D.L., Smith G.E., Hollyoak V.A., Joseph C.A., Johnson L., Chaloner R. Use of NHS direct calls for the surveillance of influenza – a second year's experience. Commun Dis Public Health. 2002;5(2):132–136. [PubMed] [Google Scholar]
- 4.Baker M., Smith G.E., Cooper D.L., Verlander N.Q., Chienmana F., Cotterill S. Early Warning and NHS Direct: a role in community surveillance? J Public Health Med. 2004;25:362–368. doi: 10.1093/pubmed/fdg096. [DOI] [PubMed] [Google Scholar]
- 5.Lazarus R., Kleinman K., Dashevsky I., DeMaria A., Jr., Platt R. Using automated medical records for rapid identification of illness syndromes (syndromic surveillance): the example of lower respiratory infection. BMC Public Health. 2001;1:9. doi: 10.1186/1471-2458-1-9. http://www.biomedcentral.com/1471-2458/1/9/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heffernan R., Mostashari F., Das D., Karpati A., Kulldorff M., Weiss D. Syndromic surveillance in public health practice, New York City. Emerg Infect Dis. 2004;10(5):858–864. doi: 10.3201/eid1005.030646. [DOI] [PubMed] [Google Scholar]
- 7.Das D., Metzger K., Heffernan R., Balter S., Weiss D., Mostashari F. Monitoring over-the-counter medication sales for early detection of disease outbreaks – New York City. MMWR. 2005;54(Suppl.):41–46. [PubMed] [Google Scholar]
- 8.Muller-Pebody B., Edmunds W.J., Zambon M.C., Gay N.J., Crowcroft N.S. Contribution of RSV to bronchitis and pneumonia-associated hospitalizations in English children, April 1995–March 1998. Epidemiol Infect. 2002;129:99–106. doi: 10.1017/s095026880200729x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melegaro A., Edmunds W.J., Pebody R., Miller E., George R. The current burden of pneumococcal disease in England and Wales. J Infect. 2006;52(1):37–48. doi: 10.1016/j.jinf.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Fleming D.M. Weekly returns service of the Royal College of General Practitioners. Commun Dis Public Health. 1999;2(2):96–100. [review] [PubMed] [Google Scholar]
- 11.Joseph C.A., Harrison T.G., Ilijic-Car D., Bartlett C.L. Legionnaires’ disease in residents of England and Wales: 1998. Commun Dis Public Health. 1999;2(4):280–284. [PubMed] [Google Scholar]
- 12.Ryan M.J., Ramsay M., Brown D., Gay N.J., Farrington C.P., Wall P.G. Hospital admissions attributable to rotavirus in England and Wales. J Infect Dis. 1996;174(Suppl.):12–18. doi: 10.1093/infdis/174.supplement_1.s12. [DOI] [PubMed] [Google Scholar]
- 13.Van Gageldonk-Lafeber A.B., Heijnen M.L., Bartelds A.I., Peters M.F., van der Plas S.M., Wilbrink B. A case-control study of acute respiratory tract infection in general practice patients in The Netherlands. Clin Infect Dis. 2005;41(4):490–497. doi: 10.1086/431982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicholson K.G., McNally T., Silverman M., Simons P., Stockton J.D., Zambon M.C. Rates of hospitalisation for influenza, respiratory syncytial virus and human metapneumovirus among infants and young children. Vaccine. 2006;24(1):102–108. doi: 10.1016/j.vaccine.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Cooper D.L., Smith G.E., Baker M., Chinemana F., Verlander N.Q., Gerard E. National symptom surveillance using calls to a telephone health advice service: United Kingdom, December 2001–February 2003. MMWR. 2004;53(Suppl.):179–183. [PubMed] [Google Scholar]
- 16.Rowlands S., Moser K. Consultation rates from the general practice research database. Br J Gen Pract. 2002;52:658–660. [PMC free article] [PubMed] [Google Scholar]
- 17.England Department of Health. Hospital activity statistics. Available from: http://www.performance.doh.gov.uk/hospitalactivity/index.htm.
- 18.Salisbury D., Begg N. HMSO; London: 1996. Immunisation against infectious diseases. [Google Scholar]
- 19.Zambon M.C., Stockton J.D., Clewley J.P., Fleming D.M. Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: an observational study. Lancet. 2001;358(9291):1410–1416. doi: 10.1016/s0140-6736(01)06528-x. [DOI] [PubMed] [Google Scholar]
- 20.Hawker J., Begg N., Blair I., Reintjes R., Weinberg J. Blackwell Science Limited; Oxford: 2001. Communicable disease control handbook. p. 21. [Google Scholar]
- 21.Cooper D.L., Smith G.E., Loveridge P., Chinemana F., Joseph C., Baker M. Can we use self-testing to augment syndromic surveillance? A pilot study using influenza. MMWR. 2005;54(Suppl.):186. [Google Scholar]
- 22.Cooke M.K., Crofts J.P., Joseph C.A., Goddard N.L., Ellis J., Zambon M. Influenza and other respiratory viruses surveillance in the United Kingdom: October 2003 to May 2004. Commun Dis Rep. 2004;(Suppl.):1–8. [Google Scholar]
- 23.Crofts J.P., Joseph C.A., Zambon M., Ellis J., Fleming D.M., Watson J.M. Surveillance in the United Kindgom: October 2002 to May 2003. Commun Dis Rep. 2003;(Suppl.):1–9. [Google Scholar]
- 24.Harcourt S, Smith GE, Hippisley-Cox J, Pringle M, Heaps M, Langford G, et al. Report of the first year of a pilot, national, primary care surveillance project. Proceedings of the Health Protection Agency annual conference 2005, p. 119.
- 25.Bourgeois F.T., Olson K.L., Brownstein J.S., McAdam A.J., Mandl K.D. Validation of syndromic surveillance for respiratory infections. Ann Emerg Med. 2006 Mar;47(3) doi: 10.1016/j.annemergmed.2005.11.022. 265.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]