Highlights
-
•
Evaluating an ingestible capsule and a skin sensor.
-
•
Measuring body temperature in patients with fever caused by an acute infectious disease.
-
•
The remote control in real time offers new opportunity for future investigation of fever.
Keywords: Body temperature measurement, Ingestible capsule sensor, Skin sensor, Peripheral temperature, Febrile patient
Summary
Backgrounds
Reliable non-invasive methods for measuring body temperature are essential for the diagnosis and monitoring of infectious disease.
Methods
This study used Intraclass Correlation Coefficients (ICC) and the Bland- Altman plot to analyse the agreement between temperature measurements using an ingestible capsule sensor, a skin sensor and two non-invasive peripheral temperature measurements (axillary and infrared non-contact), collected from a population of febrile patient admitted for infectious disease.
Results
Of the 77 febrile patients screened, 26 patients were enrolled. The ICC between axillary temperature measurements (Taxi) vs. non-contact measurements (Tno-c) were 0.34 [−0.18; 0.63], 0.87 [0.55; 0.94] between Taxi vs. ingestible capsule measurements (Tcap) and 0.12 [−0.09; 0.37] between Taxi vs. Tetac. The mean difference between Taxi vs Tno-c was −1.18 °C with limits of agreement (LoA) from −2.96 to 0.58 °C. The mean difference between Taxi vs Tcap was 0.48 °C, with LoA from −0.60 to 1.56 °C. The mean difference between Taxi vs Tetac was −4.23 °C with LoA from −7.22 to −1.23 °C.
Conclusions
Ingestible capsule measurements are reliable enough to adequately estimate the core body temperature in clinical practice. Its non-invasiveness, and the real-time remote control offer new opportunities for future research into fever during infectious diseases.
Introduction
Measuring human body temperature has been recognised as a major clinical sign for more than 150 years. Body temperature influences clinical management decisions and the diagnosis of certain diseases, but is also an important indicator for estimating body metabolism, body movement and physical activity [1,2].
When an infectious disease occurs, fever is one of many important indicators; the febrile response means that the body is fighting the infection [3]. It is referred to as a “fever” when the core temperature (head and thorax) is above 38.3 °C [4]. The normal core temperature range is between 36.5 °C and 37.3 °C; the periphery is 2–4 °C lower than that of the core [2].
There are several non-vascular methods to assess core temperature, including oesophageal and urinary bladder measurements [5]. However, these non-vascular methods are invasive because they require the use of a catheter and measuring rectal temperature creates a sense of humiliation and discomfort. On the other hand, peripheral temperature measurements, such as axillary temperature, tympanic temperature and temporal temperature are non-invasive but may underestimate the core temperature and increase contact transmissions [6]. Peripheral temperature measurements could be influenced by the following reasons: patient activity, basal metabolism rate, fat mass, skin blood flow, measurement errors (incorrect thermometer positioning) and ambient temperature.
Non-contact methods are particularly valued in highly contaminated environments. The ideal measurement method must be accurate, precise and non-invasive; in addition, the ideal site for measurements must meet the following requirements: not be influenced by ambient temperature; reflect the core temperature quantitatively and quickly; and be as non-invasive as possible [7].
In clinical practice, axillary thermometers, tympanic and temporal infrared thermometers are used frequently. However, a recent meta-analysis showed that measurements taken by peripheral thermometers were highly variable. This analysis included 75 studies, involving 8682 patients from 21 countries. This analysis concluded that most peripheral thermometers were not accurate enough to be considered as clinically acceptable core temperature measurements [8].
Ingestible telemetric body core temperature sensors have been extensively used in sports medicine specially to track core temperature during exercises. These non-invasive temperature measurement methods have been established as valid index of core temperature in several studies and have been suggested some time ago as having a good potential for ambulatory monitoring [9,10]. A recent study compared four different models of ingestible capsules and demonstrated the excellent consistency and accuracy of this device [11]. In clinical medicine and, specifically, in infectious diseases, measuring the temperature of bedridden patients is essential, yet takes nursing time and disturbs patients during the night. While ingestible telemetric body core temperature sensors have been shown to correlate with rectal temperature [12], they have not yet been compared to routine temperature measurements in clinical care in patients with fever.
This study assessed the agreement between peripheral temperature measurements used in clinical practice (axillary, non-contact) and both skin temperature recorded by skin sensor and core temperature measurements taken by an ingestible capsule in a single cohort of febrile patients.
Materials and methods
Study design
This open-label study was conducted in the department of infectious diseases at the University Hospital Institute Méditerranée-Infection located in Marseille, France. All the procedures for this study were approved by the Ethics Committee of Sud-Méditerranée IV (N° 180204) and the study was registered on the French register for clinical trial (ANSM) under N° ID-RCB: 2018-A0014748 and in the European clinical trials database EudraCT under number 2018-004812-23. In accordance with medical research ethics, all participating patients are protected (in accordance with the principles that originate in the Declaration of Helsinki). Each eligible patient was included in the study after providing their written informed consent. Patients were informed by the investigator or co-investigator of the study to the extent possible, based on their understanding.
To measure axillary temperature, this study used a mercury-free thermometer (GerathermⓇ Classic medical thermometer, CE0197, certified by NF EN ISO 13485); a new sensor, the eTactⓇ (BodyCap©, Caen, France) was used for skin temperature. An infrared thermometer was used for non-contact forehead measurement in this study (HYLOGY Non-contact Infrared Thermometer, Model: MD-H26, CE0123, US FDA approved).
An ingestible sensor (e-Celsius performance pillⓇ, BodyCap©, Caen, France) was used for core temperature measurement. This ingestible capsule is a class IIB medical device and holds certification ISO13 485 and the CE mark, providing continuous measurement of gastrointestinal temperature (more detail, see Supplementary Appendix User Guide e-CELSIUS Performance). All calibrations of the devices were performed by the manufacturer in the 2018 version [12].
Subjects
This study included all patients who presented fever upon at admission. Most were patients with acute infectious diseases: pneumonia, urinary tract infections, soft tissue infections, and all types of fever could be included in this study. All participants were social security insurance beneficiaries aged 18 years or older.
The exclusion criteria included: (1) pregnant or lactating women, (2) patients with or presenting a risk of intestinal disorders that can lead to obstruction of the digestive tract, including diverticulitis, (3) patients with motility disorders of the gastrointestinal tract, (4) patients who had undergone surgical procedures in the gastrointestinal tract, (5) patients with known swallowing disorders, (6) patients who had to undergo MRI scans (and who should thus avoid strong electromagnetic fields during the period of use of the system), (7) patients weighing less than 40 kg and vulnerable persons.
Study protocol
During the study, we collected each the pathologies, demography, medical history and medications of each patient using a bedside recording system developed in the institute (Florea O, Boudjema S, Magnin C, Brouqui P, Dufour JC, manuscript in preparation).
For every patient participating in this study, temperatures were recorded over a 48-hour observation period with axillary and non-contact forehead temperature measured by a mercury-free thermometer and infrared thermometer every two hours (8.30am, 10.30am, 12.30pm, 2.30pm, 4.30pm); skin temperature was measured by eTact patch every minute. The core temperature was measured by the ingestible capsule (BodyCap©) every five minutes.
Axillary temperature measurements were taken from the patient's left arm and environment temperature was kept at 25 °C (to minimise the influence of environment) and non-contact forehead temperature measurements were measured 5 cm in front of the central forehead. Both temperature measurements were recorded in the patient's case report, which was approved by the Independent Ethics Committee. The ingestible capsule and eTact temperature measurements were stored in the e-Viewer Performance monitor and eTact monitor, then transferred to a computer in Excel format and all data were analysed by SPSS21 and R 3.4.2 (for Bland-Altman plot).
Statistical analysis
The primary objective was to assess the agreement and Intraclass Correlation Coefficients (ICC) between the different types of body temperature measurement devices: ingestible capsule, axillary, non-contact forehead and eTact (skin) temperature. The sample size requirement for assessing ICC is 22 subjects (with power = 80%; alpha = 0.05; p = 0.4; three observations per subject and R0 was set at zero). The normality of distribution was assessed by analysis of Skewness and Kurtosis.
This study analysed the correlation coefficient (r) between axillary temperature measurements and other temperature measurement devices. However, the assessment of the relationship between the two methods is insufficient to demonstrate the degree of agreement and their difference [13]. Consequently, to evaluate whether both methods give identical readings, assessing the agreement (concordance) between series of repeated quantitative variables, it is necessary to analyse the ICC. To calculate ICC, McGraw and Wong defined 10 forms of ICC based on three “models” (one-way random effects, two-way random effects, or two-way fixed effects) and two “types” (single rater/measurement or the mean of k raters/measurements). This study chose the two-way mixed-effects model because repeated measurements cannot be considered to be randomised samples. To complete the agreement analysis, the Bland-Altman plot was used to assess the mean difference and construct the limits of agreement [14,15].
Results
The inclusion period ran from April 2018 to June 2018, during which 77 febrile patients were admitted and hospitalised. A total of 26 patients were deemed eligible and participated in this study.
Failure to obtain informed consent was the major cause of exclusion (20.78%, n = 16), eight eligible patients were not communicative, one was under guardianship, one was not conscious enough and six eligible patients refused to participate. The second most common cause for exclusion was the hypothetical requirement of MRI scans (15.58%, n = 12). The third cause for exclusion was swallowing disorders (12.99%, n = 10) and other disorders (12.99%, n = 10). The last cause for exclusion was digestive system disorders (3.9%, n = 3).
Table 1 reports the characteristics of the 26 patients: 12 females and 14 males, aged 48.6 ± 17.5 years old (mean ± SD); their mean body weight was 65.9 (±13.66) kg and blood pressure was 118.6 (±17.87)/ 64.3 (±12.98) mm Hg. The mean capsule transit time (during 48 h of observation) was 37.3 (±14.8) hours. The shortest duration was four hours (one patient).
Table 1.
Characteristics of the 26 patients. This table shows patient demography, medication and medical history.
| Sex | n | (%) |
|---|---|---|
| Female | 12 | (46.2) |
| Male | 14 | (53.8) |
| Baseline | Mean | (SD) |
| Age (years) | 48.6 | (17.5) |
| Body weight (kg) | 65.9 | (13.66) |
| Blood pressure (mm Hg) | ||
| Systolic pressure | 118.6 | (17.87) |
| Diastolic pressure | 64.3 | (12.98) |
| Pulse (bpm) | 95.4 | (15.5) |
| Body temperature during inclusion (°C) | 38.73 | (0.74) |
| Capsule transit time (hours) | 37.3 | (14.8) |
| Treatments | n | (%) |
| Antibiotics | 19 | (33.92) |
| Antipyretic | 8 | (14.28) |
| Antivirus | 4 | (7.14) |
| Antimalarial | 1 | (1.78) |
| Other | 24 | (42.85) |
| Medical history | n | (%) |
| Surgical | 7 | (19.44) |
| Cardiovascular | 8 | (22.22) |
| Metabolic disorders | 6 | (16.66) |
| Pulmonary | 2 | (5.55) |
| Urinary | 2 | (5.55) |
| Gastro-intestinal | 3 | (8.33) |
| Infectious | 8 | (22.22) |
Following the collection body temperature measurements from four different devices over the 48-hour observation period, Table 2 summarises the percentages of missing measurements, mean temperature, standard deviation, and maximum and minimum variable.
Table 2.
Descriptive statistics of axillary temperature, non-contact temperature, ingestible capsule temperature and eTact temperature measurements during 48-h observation period.
| Total N (measurement points) | Valid N | Missing (n, %) | Mean (°⁰C) | Standard deviation | Max (°C) | Mini (°C) | |
|---|---|---|---|---|---|---|---|
| Axillary temperature (Taxi) | 255 | 213 | 42 (16.5) | 37.84 | 1.02 | 41.5 | 36.3 |
| Non-contact forehead temperature (Tno-c) | 255 | 216 | 39 (15.3) | 36.66 | 0.61 | 39.4 | 34.5 |
| Ingestible capsule temperature (Tcap) | 255 | 213 | 42 (16.5) | 38.26 | 1.01 | 40.5 | 35.7 |
| eTact temperature (Tetac) | 255 | 225 | 30 (11.8) | 33.59 | 1.84 | 38.37 | 24.03 |
There is a 16.5% gap in temperature measurements for ingestible capsules. The main cause of these missing measurements was the evacuation of the capsule before the 48-hour observation period or a synchronisation problem between the monitor and the capsule (n = 42, 11 patients). eTact patches had fewer missing measurements at only 11.8% due to battery shutdown (n = 18, 5 patients) or removal of the device by the patient (n = 12, 2 patients). As for axillary and non-contact measurements, there was a missing measurement rate of 16.5% (n = 42) and 15.3% (n = 39) respectively, due to the absence of the patients at the time of recording and during the weekend.
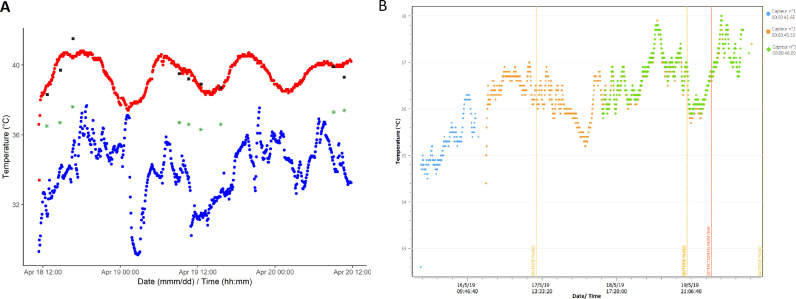
To highlight the usefulness of the ingestible capsule temperature measurements, Fig. 1 (A) indicates the time trend data of all measurements in one selected patient. Fig. 1(B) indicates the time trend data of one patient with hypothermia.
Fig. 1.
Time trend data.
(A) Time trend data of all measurements in one selected patient with acute community acquired pneumonia. Black squares represent axillary temperature measurements; red points represent ingestible capsule temperature measurements; green stars represent non-contact temperature measurements; blue points represent eTact temperature measurements. (B) Time trend data of a patient with hypothermia.
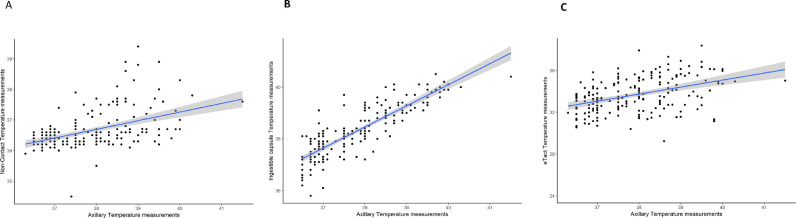
The regression line between the axillary temperature measurements (Taxi) and non-contact forehead temperature measurements (Tno-c), ingestible capsule temperature measurements (Tcap) as well as eTact temperature measurements (Tetac) are shown in Fig. 2 . The coefficient (r) between Taxi vs. Tno-c is 0.47 (95% IC: 0.36; 0.57, R² = 0.22, p < 0.001) and coefficient (r) is 0.85 (95% IC: 0.81; 0.98, R² = 0.72, p < 0.001) between Taxi vs. Tcap. The correlation between Taxi vs. Tetac is coefficient (r) = 0.42 (95% IC: 0.30; 0.52, R² = 0.17, p < 0.001). The ICC between Taxi vs. Tno-c is 0.34 (95% IC: −0.18; 0.63); 0.87 (95% IC: 0.55; 0.94) between Taxi vs. Tcap; and 0.12 (95% IC: −0.09; 0.37) between Taxi vs. Tetac. Table 3 summarises the comparison of each correlation and agreement between the three different devices and the axillary temperature measurements.
Fig. 2.
Regression line between the axillary temperature measurements (Taxi) and non-contact forehead temperature measurements (Tno-c), ingestible capsule temperature measurements (Tcap) as well as eTact temperature measurements (Tetac). With 95% confidence interval.
A, Regression line between the Taxi and Tno-c (r = 0.47, p < 0.001). B, Regression line between the Taxi and Tcap. (r = 0.85, p < 0.001). C, Regression line between the Taxi and Tetac (r = 0.42, p < 0.001).
Table 3.
Analyses of correlation (pearson) and agreement (intraclass correlations) among three different devices and axillary temperature measurements.
| Correlation coefficient |
Agreement |
||||||
|---|---|---|---|---|---|---|---|
| Pearson (r) | 95% CI | Sig. | R² | ICC | 95% CI | Sig. | |
| Non-contact forehead (Tno-c) | 0.47 | 0.36;0.57 | p < 0.001 | 0.22 | 0.3445 | −0.18; 0.63 | p < 0.001 |
| Ingestible capsule (Tcap) | 0.85 | 0.81;0.98 | p < 0.001 | 0.72 | 0.8730 | 0.55; 0.94 | p < 0.001 |
| eTact (Tetac) | 0.42 | 0.30;0.52 | p < 0.001 | 0.17 | 0.1229 | −0.09; 0.37 | p < 0.001 |
We also assessed the correlation at the time of each recording (10 recordings in 48 h); no statistically significant differences were found during the 48-h observation period.
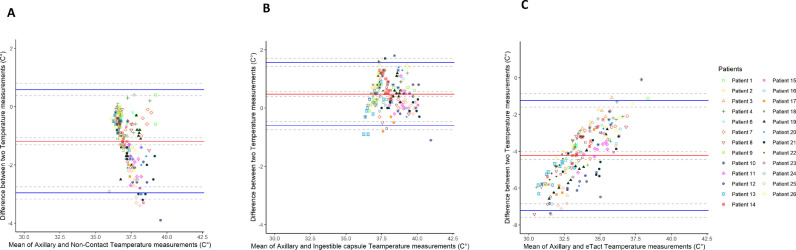
Finally, Table 4 summarises the details of the Bland-Altman plot. This table shows the mean difference of two paired of measurements as well as their standard deviation and the limits of agreement. The mean difference between Taxi vs. Tno-c is −1.18 °C with 95% limits of agreement of −2.96 °C to 0.58 °C. The mean difference between Taxi vs. Tcap is 0.48 °C with 95% limits of agreement of −0.60 °C to 1.56 °C. The mean difference between Taxi vs Tetac is −4.23 °C with 95% limits of agreement of −7.22 °C to −1.23 °C. Fig. 3 indicate the difference of two pairs of measurements.
Table 4.
Detail of Bland–Altman plot among three different devices and axillary temperature measurements.
| Mean difference (°C) | Standard deviation | Std. error mean | 95% confidence interval of the difference (°C) |
limits of agreement (d ± 1.96SD) (°C) |
|||
|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | ||||
| Tno-c vs. taxi | −1.1892 | 0.9049 | 0.062 | −1.06697 | −1.311433 | −2.9629 | 0.5845 |
| Tcap vs. taxi | 0.4804 | 0.5549 | 0.0409 | 0.3997 | 0.5611 | −0.6071 | 1.5680 |
| Tetac vs. taxi | −4.2316 | 1.5285 | 0.1091 | −4.4470 | −4.0163 | −7.2277 | −1.2356 |
Fig. 3.
Bland-Altman plot. Comparison of the difference between two measurements with the 95% limits of agreement. The red line represents the mean difference between two measurements, with 95% confidence interval (two grey dashed lines). Blue lines represent the upper and lower limits of agreement and grey dashed lines represent their 95% confidence interval.
(A) Comparison of the difference between the Taxi and Tno-c. The mean difference between Taxi vs. Tno-c (−1.18 °C). The upper and lower limits of agreement (−2.96 °C and 0.58 °C). (B) Comparison of the difference between the Taxi and Tcap. The mean difference between Taxi vs. Tcap (0.48 °C). The upper and lower limits of agreement (−0.60 °C and 1.56 °C). (C) Comparison of the difference between the Taxi and Tetac. The mean difference between Taxi vs Tetac (−4.23 °C). The upper and lower limits of agreement (−7.22 °C and −1.23 °C).
Discussion
While pulmonary arterial blood temperature is considered to be the gold standard for measuring core temperature, this invasive method cannot be used in non-ICU febrile patients. Ingestible telemetric body core temperature sensors have been shown to correlate with rectal temperature [11,16]. Rectal temperature has widely been dismissed in clinical practice due to its invasiveness and discomfort. Axillary temperature measurement is currently the non-invasive measurement that reflects the best core temperature (axillary temperature plus 0.5 °C) and has been recommended as the standard for neonatal care [1,17].
Several studies have shown that non-contact (forehead or temporal artery) temperature measurements are a reliable, comfortable and accurate option for measuring body temperature and screening for fever in the paediatric population 18, 19, 20, and they have been widely used in airports since the outbreak of severe acute respiratory syndrome (SARS) [21,22]. In 2004, the U.S. Food and Drug Administration (US FDA) approved the use of this thermometer in children [20]. However, some studies have shown this method is not clinically acceptable in adults 23, 24, 25, 26.
In this study, the non-contact forehead temperature measurements show a weak uphill linear relationship (r = 0.42) and poor strength of agreement (ICC < 0.40) with axillary temperature measurements. The Bland–Altman plot shows that more than 95% of points are within the limits of agreement, but 95% of points show that the difference between the Taxi vs. Tno-c is lower than zero. The mean difference between Taxi vs. Tno-c is −1.18 °C, which is higher than the clinically acceptable range (±0.5 °C). This method underestimates core temperature because non-contact forehead temperature measurements could be influenced by blood flow under the skin, body metabolic rate and the distance between the thermometer and forehead. Moreover, according to the Bland-Altman plot, the difference between the two temperature measurements increases as the temperature increases. Therefore, this method is neither sufficiently reliable nor clinically acceptable for screening for fever in adult febrile patients.
Skin sensors (eTact patches) exhibit a weak uphill linear relationship (r = 0.42) and a poor strength of agreement (ICC < 0.40) with axillary temperature measurements. Skin temperature can be influenced by many factors such as blood flow under the skin, the body's metabolic rate and ambient temperature [27]. Thus, this method was less consistent than the core temperature measurements (SD of eTact measurements was 1.84 and the SD of ingestible capsule measurements was 1.01). The Bland–Altman plot shows that 95% of points were within the limits of agreement, but many of the points were further from zero. The mean difference was −4.23 °C, as the theory indicated; the skin temperature was 2–4 °C below the core temperature. However, this method did not correlate well with the reference temperature, so it is not acceptable for fever screening.
In our study, the ingestible capsule shows a strong uphill linear relationship (r = 0.85) and an excellent degree of agreement (ICC > 0.77) with the axillary temperature measurements. According to the Bland–Altman plot, 95% of points are within the limits of agreement, and the mean difference between Taxi vs Tcap is 0.48 °C, which is within the clinically acceptable range (±0.5 °C). This difference between axillary temperature measurements and temperature measurements of ingestible capsules is, as the theory indicates, in the range of 0.5–1 °C. Compared to other core temperature measurement methods, the ingestible capsule is less invasive and more comfortable method for patients. This method produces continuous body temperature measurements during gastro-intestinal transit. However, cold or hot food and drink intake can influence capsule temperature measurements [28]. According to Domitrovich, measurements of ingestible capsules are reliable after only 40 min of ingestion (when the sensor passes the stomach) [29]. In our study, we therefore took this constraint into account when analysing the data. Ingestible temperature sensors are an easy way to follow and monitor core temperature; it has been reported that continuous core temperature measurements help to predict the early diagnosis of hospital-acquired sepsis [30]. Continuous core temperature measurements could offer a different perspective on patterns of fever and detect abnormal core temperature curves at an earlier stage. Monitoring core body temperature in real time on a continuous basis might be very useful in cases of factitious fevers, chronic infections and fevers of unknown origin. Non aggressive, continuous real time recording of the body temperature during infection offers a new tool to study the relationship between temperature and the infectious process [31]. However, ingestible telemetric body core temperature sensors have some limitations: the main one being the gastrointestinal transit time, as transit time varies for each individual due to age, gender, diet and pathology. The variability of the transit time ranges from 0.52 day to 5.6 days and the mean transit time is 2 ± 1.5 days [32]. This resulted in missing measurements in our study, due to the absence of indications from the capsule. However, if needed, capsules can be prescribed every three days and the monitor can follow four capsules at the same time. Another inconvenience was the exclusion of patients who might require an MRI scan, who represented 15% of febrile patients in our cohort. However, one final positive aspect of this type of measurement is that, in our experience, the time spent by the nurse waiting for axillary temperature readings was calculated in our study as 2.83 ± 0.66 min. The cumulated time spent by nurses waiting to collect axillary temperature readings in our study was estimated at 12.26 h. Although a full medico-economic study is required, it is likely that the capsule would save time.
Conclusions
Of existing temperature measurement sensors, only the ingestible capsule has a good correlation and agreement with axillary temperature measurement. It is sufficiently reliable to adequately estimate the body temperature in clinical care. In addition, the capsules offer real-time measurement (every 30 s, one minute, two minutes or five minutes). The number of collection points, its non-invasiveness, and the remote control in real time offer new opportunity for future investigation of fevers during the course of infectious diseases.
CRediT authorship contribution statement
Huang Fanyu: Formal analysis, Investigation, Writing - original draft. Chloe Magnin: Methodology, Supervision. Philippe Brouqui: Conceptualization, Funding acquisition, Supervision, Writing - review & editing.
Declaration of Competing Interest
All authors are no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Acknowledgments
Acknowledgments
We would like to thank the nurses and the medical team from the University Hospital Institute Méditerranée-Infection who have been very helpful. We also thank all the patients for their willingness to participate in this study.
The English language in this text was edited by TradonlineⓇ. Plagiarism was tested by UrkundⓇ.
Financial support
This work was supported by ANR “Investissements d'avenir”, Méditerranée infection 10-IAHU-03. Ingestible capsule sensors, monitor and e-tact sensors were provided by BodyCap©, e-Celsius performanceⓇ thanks to Sébastien Moussay.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2019.11.003.
Contributor Information
Fanyu Huang, Email: fanyu.huang@etu.univ-amu.fr.
Chloe Magnin, Email: chloe_magnin@yahoo.fr.
Philippe Brouqui, Email: philippe.brouqui@univ-amu.fr.
Appendix. Supplementary materials
References
- 1.Marui S., Misawa A., Tanaka Y., Nagashima K. Assessment of axillary temperature for the evaluation of normal body temperature of healthy young adults at rest in a thermoneutral environment. J Physiol Anthropol. 2017;36(1):18. doi: 10.1186/s40101-017-0133-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bindu B., Bindra A., Rath G. Temperature management under general anesthesia: compulsion or option. J Anaesthesiol Clin Pharmacol. 2017;33(3):306–316. doi: 10.4103/joacp.JOACP_334_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young P.J., Saxena M. Fever management in intensive care patients with infections. Crit Care. 2014;18(2):206. doi: 10.1186/cc13773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnow P.M., Flaherty J.P. Fever of unknown origin. Lancet. 1997;350(9077):575–580. doi: 10.1016/S0140-6736(97)07061-X. [DOI] [PubMed] [Google Scholar]
- 5.Robinson J.L., Seal R.F., Spady D.W., Joffres M.R. Comparison of esophageal, rectal, axillary, bladder, tympanic, and pulmonary artery temperatures in children. J Pediatr. 1998;133(4):553–556. doi: 10.1016/s0022-3476(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 6.Kimberger O., Thell R., Schuh M., Koch J., Sessler D.I., Kurz A. Accuracy and precision of a novel non-invasive core thermometer. Br J Anaesth août. 2009;103(2):226–231. doi: 10.1093/bja/aep134. [DOI] [PubMed] [Google Scholar]
- 7.Fox R.H., Solman A.J., Isaacs R., Fry A.J., MacDonald I.C. A new method for monitoring deep body temperature from the skin surface. Clin Sci. 1973;44(1):81–86. doi: 10.1042/cs0440081. [DOI] [PubMed] [Google Scholar]
- 8.Niven D.J., Gaudet J.E., Laupland K.B., Mrklas K.J., Roberts D.J., Stelfox H.T. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med. 2015;163(10):768–777. doi: 10.7326/M15-1150. [DOI] [PubMed] [Google Scholar]
- 9.Byrne C., Lim C.L. The ingestible telemetric body core temperature sensor: a review of validity and exercise applications. Br J Sports Med. 2007;41(3):126–133. doi: 10.1136/bjsm.2006.026344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chapon P.A., Gauthier A., Bulla J., Moussay S. Calibration and performance assessment of a temperature sensor prototype using a 1-point calibration procedure. Rev Sci Instrum. 2012;83(11) doi: 10.1063/1.4767244. [DOI] [PubMed] [Google Scholar]
- 11.Bongers C.C.W.G., Daanen H.A.M., Bogerd C.P., Hopman M.T.E., Eijsvogels T.M.H. Validity, reliability, and inertia of four different temperature capsule systems. Med Sci Sports Exerc. 2018;50(1):169–175. doi: 10.1249/MSS.0000000000001403. [DOI] [PubMed] [Google Scholar]
- 12.Bogerd C.P., Velt K.B., Annaheim S., Bongers C.C.W.G., Eijsvogels T.M.H., Daanen H.A.M. Comparison of two telemetric intestinal temperature devices with rectal temperature during exercise. Physiol Meas. 2018;39(3):03NT01. doi: 10.1088/1361-6579/aaad52. [DOI] [PubMed] [Google Scholar]
- 13.Fuhrman C., Chouaïd C. Concordance de deux variables : les approches numériques: concordance entre observations qualitatives -coefficient kappa-, concordance entre méthodes quantitatives. Revue des Maladies Respiratoires. 2004;21(1):123–125. doi: 10.1016/s0761-8425(04)71242-5. [DOI] [PubMed] [Google Scholar]
- 14.Koo T.K., Li M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bland J.M., Altman D.G. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–582. doi: 10.1080/10543400701329422. [DOI] [PubMed] [Google Scholar]
- 16.Gibson T.M., Redman P.J., Belyavin A.J. Prediction of oesophageal temperatures from core temperatures measured at other sites in man. Clin Phys Physiol Meas. 1981;2(4):247–252. doi: 10.1088/0143-0815/2/4/001. [DOI] [PubMed] [Google Scholar]
- 17.Charafeddine L., Tamim H., Hassouna H., Akel R., Nabulsi M. Axillary and rectal thermometry in the newborn: do they agree? BMC Res Notes. 2014;7:584. doi: 10.1186/1756-0500-7-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sollai S., Dani C., Berti E., Fancelli C., Galli L., de Martino M. Performance of a non-contact infrared thermometer in healthy newborns. BMJ Open. 2016;6(3) doi: 10.1136/bmjopen-2015-008695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osio C.E., Carnelli V. Comparative study of body temperature measured with a non-contact infrared thermometer versus conventional devices. The first Italian study on 90 pediatric patients. Minerva Pediatr. 2007;59(4):327–336. [PubMed] [Google Scholar]
- 20.Teran C.G., Torrez-Llanos J., Teran-Miranda T.E., Balderrama C., Shah N.S., Villarroel P. Clinical accuracy of a non-contact infrared skin thermometer in paediatric practice. Child Care Health Dev. 2012;38(4):471–476. doi: 10.1111/j.1365-2214.2011.01264.x. [DOI] [PubMed] [Google Scholar]
- 21.Apa H., Gözmen S., Bayram N., Çatkoğlu A., Devrim F., Karaarslan U. Clinical accuracy of tympanic thermometer and noncontact infrared skin thermometer in pediatric practice: an alternative for axillary digital thermometer. Pediatr Emerg Care. 2013;29(9):992–997. doi: 10.1097/PEC.0b013e3182a2d419. [DOI] [PubMed] [Google Scholar]
- 22.Chan L.-.S., Cheung G.T.Y., Lauder I.J., Kumana C.R. Screening for fever by remote-sensing infrared thermographic camera. Journal of Travel Medicine. 2004;11(5):273–279. doi: 10.2310/7060.2004.19102. [DOI] [PubMed] [Google Scholar]
- 23.Kiekkas P., Stefanopoulos N., Bakalis N., Kefaliakos A., Karanikolas M. Agreement of infrared temporal artery thermometry with other thermometry methods in adults: systematic review. J Clin Nurs. 2016;25(7–8):894–905. doi: 10.1111/jocn.13117. [DOI] [PubMed] [Google Scholar]
- 24.Mogensen C.B., Wittenhoff L., Fruerhøj G., Hansen S.Forehead or ear temperature measurement cannot replace rectal measurements, except for screening purposes. BMC Pediatr [Internet]. 26 janv 2018 [cité 21 févr 2018];18. Disponible sur: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5787302/. [DOI] [PMC free article] [PubMed]
- 25.Fortuna E.L., Carney M.M., Macy M., Stanley R.M., Younger J.G., Bradin S.A. Accuracy of non-contact infrared thermometry versus rectal thermometry in young children evaluated in the emergency department for fever. J Emerg Nurs. 2010;36(2):101–104. doi: 10.1016/j.jen.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 26.Hausfater P., Zhao Y., Defrenne S., Bonnet P., Riou B. Cutaneous infrared thermometry for detecting febrile patients., cutaneous infrared thermometry for detecting febrile patients. Emerg Infect Dis. 2008;14(8, 8):1255–1258. doi: 10.3201/eid1408.080059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rastgar-Jazi M., Mohammadi F. Parameters sensitivity assessment and heat source localization using infrared imaging techniques. Biomed Eng Online. 21 2017;16:113. doi: 10.1186/s12938-017-0403-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roxane B., Ouma Chandrou K., Pierre Alexandre C., Christophe C., Bruno S., Stéphane B. Gastrointestinal thermal homogeneity and effect of cold water ingestion. J. Therm. Biol. 2018;78:204–208. doi: 10.1016/j.jtherbio.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Domitrovich J.W., Cuddy J.S., Ruby B.C. Core-Temperature sensor ingestion timing and measurement variability. J Athl Train. 2010;45(6):594–600. doi: 10.4085/1062-6050-45.6.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drewry A.M., Fuller B.M., Bailey T.C., Hotchkiss R.S. Body temperature patterns as a predictor of hospital-acquired sepsis in afebrile adult intensive care unit patients: a case-control study. Crit Care. 2013;17(5):R200. doi: 10.1186/cc12894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Plaza J.J.G., Hulak N., Zhumadilov Z., Akilzhanova A. Fever as an important resource for infectious diseases research. Intractable Rare Dis Res. 2016;5(2):97–102. doi: 10.5582/irdr.2016.01009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKenzie J.E., Osgood D.W. Validation of a new telemetric core temperature monitor. J Therm Biol. 2004;8(29):605–611. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.