Abstract
A single amino acid substitution, from histidine to tyrosine at position 274 of the neuraminidase gene has converted Oseltamivir sensitive H5N1 influenza A virus into a resistant strain. Currently, Oseltamivir is being stockpiled in many countries potentially affected by the influenza A virus subtype H5N1 epidemic. To identify this change in Oseltamivir-treated patients, a method based on real-time PCR using two labeled TaqMan probes was developed for its rapid detection. In order to validate the method, Oseltamivir specimen from treated (Oseltamivir-resistant strain from a Vietnamese patient, two Oseltamivir-treated tigers) and untreated subjects have been used for this study. The results thus obtained as well as those derived from clone selection and sequencing showed that TaqMan probes could clearly discriminate wild type H274 from the mutant 274Y variant. The sensitivity of this assay was as low as 10 copies/μl and allowed the detection of the mutation in a mixture of wild type and mutant. Overall, the assay based on real-time PCR with two labeled TaqMan probes described here should be useful for detecting Oseltamivir-resistant H274Y H5N1 influenza A virus in many species and various sources of specimens with high sensitivity and specificity. Such studies can address potential differences in the diagnostic outcomes between patients who develop detectable Oseltamivir resistance and those who retain only the wild type strain of H5N1.
Keywords: H5N1, Influenza A virus, Oseltamivir resistance, Real-time PCR
1. Introduction
Influenza virus is a RNA virus from the Orthomyxoviridae family. Annually, influenza viruses may develop symptomatic influenza in 20% of children and 5% of adults worldwide (Turner et al., 2003). From the three types A–C only A and B cause widespread outbreaks. Further subtyping of influenza A virus is based on the antigenic differences between two surface glycoproteins: haemagglutinin (HA) and neuraminidase (NA). Nowadays, 16 HA (H1–H16) and 9 NA (N1–N9) subtypes have been described (Fouchier et al., 2005, Nicholson et al., 2003). Since 2004, the influenza A virus subtype H5N1 has been the cause of severe disease in various poultry and mammals. The clinical spectrum of avian influenza (H5N1) in humans comprises initial symptoms of high fever (exceeding 38 °C), lower respiratory tract symptoms, clinically significant lymphopenia, abnormalities on chest radiography, and in some cases diarrhea, vomiting (Tran et al., 2004) and encephalitis. The overall fatality rate among hospitalized patients with avian influenza A (H5N1) infection has amounted to 57% (WHO, 2006). Two groups of antiviral agents are currently available for the treatment of influenza infection. The Adamantanes (Amantadine and Rimantadine) block the function of the M2 protein; however, drug resistance in patients has increased to 30% (Hayden and Hay, 1992). The more recently developed class of viral neuraminidase inhibitors includes Zanamivir (Relenza) and Oseltamivir (Tamiflu). An important antiviral medication used against all strains of influenza A virus is Oseltamivir, which is the first orally active neuraminidase inhibitor in the form of a capsule or powder for liquid suspension (Kim et al., 1997). The neuraminidase inhibitor (NAI) Oseltamivir imitates natural neuraminidase substrate molecules and binds to the active site of the enzyme in addition to interfering with the release of progeny influenza virus from infected host cells (Moscona, 2005a). Therefore, neuraminidase (NA) cannot cleave a terminal N-acetylneuraminic acid residue from an oligosaccharide chain and thus, the virions self-aggregate and bind to the surface of infected cells.
Oseltamivir resistance due to neuraminidase mutations have arisen both in challenge studies and in patients with naturally acquired infections. Rates of resistance are estimated at around 1% in the adult population and 5% in pediatric patients (Jackson et al., 2000, Whitley et al., 2001). In 2004, Kiso et al. (2004) analyzed influenza A viruses (H3N2) collected from 50 children before and during treatment with Oseltamivir. Eighteen percent of the children (N = 9/50) had neuraminidase mutations at Arg292Lys (N = 6/9) or Glu119Val (N = 2/9) or Asn294Ser (N = 1/9). Volunteers experimentally infected with influenza A/Texas/36/91 (H1N1) virus and treated with oseltamivir have shown an H274Y substitution at the neuraminidase active site (Gubareva et al., 2001). This mutation in response to oseltamivir phosphate treatment leaves the virus severely compromised both in vitro and in vivo (Ives et al., 2002) and confers about 400–600-fold resistance (Wetherall et al., 2003). The mutation at position 274 can influence the sensitivity of influenza N1 NA yet not of N2 NA to Oseltamivir carboxylate by rearranging the shape of the active site to create a pocket for Oseltamivir (Gubareva, 2004, Moscona, 2005b, Wang et al., 2002).
Safeguarding against a potential influenza A virus subtype H5N1 epidemic, many countries now stockpile Oseltamivir. It has recently been reported that Oseltamivir-resistant influenza A (H5N1) viruses with the H274Y mutation have been isolated from three patients. H5N1 viruses with pronounced Oseltamivir resistance were isolated from two of eight Vietnamese patients during Oseltamivir treatment. Both patients died in January 2005 and another resistant case died in February 2005 (Beigel et al., 2005, de Jong et al., 2005, Le et al., 2005).
As an increase in Oseltamivir-resistant viruses seems likely, a method aimed at rapidly identifying resistant H5N1 strains applying real-time PCR using TaqMan probes was designed. The assay enables to identify the H274Y mutation from samples originated directly from infected tissue and plasma.
2. Materials and methods
2.1. Sources of clinical specimens
Oseltamivir-treated and non-treated specimens of several species infected with avian influenza A subtype H5N1, previously detected using the method described by Payungporn et al. (2005), were used. The Oseltamivir-treated specimens were: H5N1 Oseltamivir-resistant strain in a Vietnamese patient (N = 1), Oseltamivir-treated tiger CU-T7; Panthera tigris tigris (N = 1), white tiger KU-11; P. tigris tigris (N = 1). The Oseltamivir untreated specimens were: plasma of H5N1 infected human (N = 1) (Chutinimitkul et al., 2006), several tissues from different organs of tiger, lung (N = 1), spleen (N = 1), kidney (N = 1), liver (N = 1), brain of leopard (Panthera pardus) (N = 1), allantoic fluid of embryonated chicken eggs inoculated with the virus according to the method described by the Office International des Epizooties (OIE) originating from a cat; Felis catus (N = 1), a dog; Canis familiaris (N = 1), a quail (N = 1), an ostrich (N = 1) and chicken (N = 6). These specimens were isolated and provided by: (1) the Faculty of Veterinary Science, Chulalongkorn University, Bangkok, Thailand; (2) the Department of Livestock Development, Bangkok, Thailand; (3) Faculty of Veterinary Science, Kasetsart University, Kampaengsaen Campus, Nakorn Pathom, Thailand; (4) Department of Pediatrics, Faculty of Medicine, Srinakharinwirot University, Nakhon Nayok, Thailand; (5) National Institute of Hygiene and Epidemiology, Hanoi, Vietnam.
2.2. Primer and TaqMan probe design
The nucleotide sequences (N = 246) of the neuraminidase gene of influenza A virus (H5N1) were taken from the Genbank database going back as far as 2003–2006 and hence, comprising entries isolated from various species, such as avian, cats, dog, tigers, swine and humans, including DQ250165, the sequence of one Vietnamese Oseltamivir-resistant patient (A/Vietnam/CL2009/2005(H5N1)). The alignments were performed using CLUSTAL X (Version 1.81 from ftp://ftp-igbmc.u-strasbg.fr/pub/ClustalX) and BioEdit sequence alignment Software Version 5.0.9 (http://www.mbio.ncsu.edu/BioEdit/bioedit.html).
Assay target regions were first identified by visual inspection of the sequence alignment. Primers were chosen from constant regions of all sequences specific for the neuraminidase gene N1 of influenza A virus most closely related to the probes. MGB TaqMan probes were chosen from the region covering the drug resistant area (H274Y) and designed to be specific for both wild type and mutant. Both primers and probes were analyzed using the primer design software (OLIGOS Version 9.1 by Ruslan Kalendar, Institute of Biotechnology, University of Helsinki, Finland) and Primer Express Software Version 2.0 (Applied Biosystems, CA). The wild type (H) and mutant (Y) MGB TaqMan probes were labeled with FAM and VIC with emission wavelengths at 530 and 560 nm, respectively. The primers and probes used in this study are shown in Table 1 .
Table 1.
H274Y detection primers and TaqMan MGB probes and series of mutagenesis primers at amino acid position 274
| Primer/probe | Sequence (5′–3′) | Positiona | Strand |
|---|---|---|---|
| Primer_F | 5′-ATACTGAGAACTCAAGAGTC-3′ | 583–602 | Sense |
| Primer_R | 5′-TTATCCCTGCACACACATG-3′ | 800–702 | Antisense |
| Probe_H274 | 5′-6FAM-TCCTCATAGTGRTAATT-MGBNFQ-3′ | 749–733 | Antisense |
| Probe_274Y | 5′-VIC-TCCTCATAGTARTAATT-MGBNFQ-3′ | 749–733 | Antisense |
| N1MuF | 5′-GGGGCTGTGGCTGTATTG-3′ | 517–534 | Sense |
| N1MuR | 5′-GGGGCGTGGATTGTCTCC-3′ | 900–883 | Antisense |
| N1Mu1F | 5′-ATTATCACTATGAGGAATGCTC-3′ | 734–755 | Sense |
| N1Mu1R | 5′-GAGCATTCCTCATAGTGATAAT-3′ | 755–734 | Antisense |
| N1Mu2F | 5′- ATTATTACTATGAGGAATGCTC-3′ | 734–755 | Sense |
| N1Mu2R | 5′-GAGCATTCCTCATAGTAATAAT-3′ | 755–734 | Antisense |
| N1Mu3F | 5′-ATTACCACTATGAGGAATGCTC-3′ | 734–755 | Sense |
| N1Mu3R | 5′-GAGCATTCCTCATAGTGGTAAT-3′ | 755–734 | Antisense |
| N1Mu4F | 5′-ATTACTACTATGAGGAATGCTC-3′ | 734–755 | Sense |
| N1Mu4R | 5′-GAGCATTCCTCATAGTAGTAAT-3′ | 755–734 | Antisense |
The neuraminidase gene of A/chicken/Nakorn-Patom/Thailand/CU-K2/2004 GenBank accession number AY590567 served as reference.
2.3. Oligonucleotides designed for H274Y mutagenesis
An RNA sample extracted from embryonated chicken eggs and previously identified as influenza A virus subtype H5N1 (A/chicken/Nakorn-Patom/Thailand/CU-K2/2004(H5N1)) was applied to design a series of mutagenesis. The oligonucleotides depicted in Table 1 were used to generate the series of mutagenesis at amino acid position 274 of the neuraminidase N1 gene which served as a control for all possible patterns of nucleotide change in the area of probe binding. The primers N1MuF and N1MuR served as the outer primers of each mutagenesis group, which paired with the mutagenesis primers. Mutagenesis primer group 1 for H274 is N1Mu1F and N1Mu1R. Mutagenesis primer group 2 for 274Y is N1Mu2F and N1Mu2R. Mutagenesis primer groups 3 and 4 were designed for possible varied strains occasionally found. The mutagenesis products of groups 1 and 2 were used to construct mutagenesis groups 3 and 4. Mutagenesis group 3 for H274 is N1Mu3F and N1Mu3R. Mutagenesis group 4 for 274Y is N1Mu4F and N1Mu4R. The primary mutagenesis PCR reaction mixture comprised 0.5 μl of cDNA CU-K2, 0.5 μM forward primer (outer or mutagenesis primer), 0.5 μM reverse primer (outer or mutagenesis primer), 10 μl of 2.5× MasterMix (Eppendorf, Hamburg, Germany) and nuclease-free water to a final volume of 25 μl. The secondary mutagenesis PCR reaction mixture comprised 0.5 μl PCR product representative for each mutagenesis group, 0.5 μM N1MuF, 0.5 μM N1MuR, 10 μl 2.5× MasterMix (Eppendorf) and nuclease-free water to a final volume of 25 μl. Both amplification reactions were performed in a Mastercycler personal (Eppendorf) under the following conditions: predenaturation at 94 °C for 2 min followed by 40 amplification cycles consisting of 30 s denaturation at 94 °C, 30 s annealing at 52 °C and 1 min extension at 72 °C and concluded by a final 7 min extension at 72 °C. Four groups of mutagenesis PCR products were separated by 2% agarose gel electrophoresis and purified using the Gel Extraction Kit (Perfectprep Gel Cleanup, Eppendorf, Hamburg, Germany). These purified products were inserted into the pGEM-T Easy Vector System (Promega, Madison, WI) and plasmids were purified by using the High Pure Plasmid Isolation Kit (Roche, GmbH, Germany) according to the manufacturer's specifications. The series of H274Y mutations were sequenced and used as controls.
2.4. RNA extraction and reverse transcription
Viral RNA was extracted from 140 μl samples of the allantoic fluid of inoculated embryonated eggs, plasma and the supernatant resulting from tissue extraction using the QIAmp viral RNA mini kit (Qiagen, GmbH, Germany) according to the manufacturer's specifications. Reverse transcription was performed on 12 μl of each RNA sample at 37 °C for 1 h using 200 units of M-MLV reverse-trancriptase (Promega), 5 μl of 5× M-MLV reaction buffer (Promega), 5 μl of 10 mM dNTP (Promega), 25 units of rRnasin® Ribonuclease Inhibitor (Promega), 1 μM universal primer as described by Hoffmann et al. (2001). Twelve microliters of RNA from the RNA extraction kit were heated to 70 °C for 5 min and cooled on ice before adding nuclease-free water to a final volume of 25 μl.
2.5. Real-time PCR conditions
Real-time PCR was performed using the Biotools QuantiMix EASY PROBES KIT (Biotools, Madrid, Spain). Both probes and primer pairs depicted in Table 1 were used in multiple formats, each primer and probe at a final concentration of 0.5 μM and 0.20 μM, respectively. A combination of 0.5 μl cDNA from embryonated eggs or 2 μl cDNA from tissue, serum or plasma with a reaction mixture containing 10 μl of QUANTIPROBES, 4.0 mM MgCl2 and nuclease-free water was adjusted to a final volume of 20 μl. Real-time PCR amplification was carried out in a Rotor-Gene 3000 Instrument (Corbett Research, Sydney, Australia). The amplification reaction consisted of a preincubation step at 95 °C for 10 min to activate the HotStarTaq DNA polymerase. This was followed by 40 cycles of amplification including denaturation at 95 °C for 10 s, annealing at 55 °C for 15 s and extension at 72 °C for 20 s. Two fluorescent signals were obtained once per cycle at the end of the extension step with detectors corresponding to the FAM (530 nm) and VIC (560 nm) channels, respectively. Data acquisition and analysis of the real-time PCR assay were performed using the Rotor-Gene data analysis software, Version 6.0 (Corbett research supporting program).
2.6. Selection of drug resistant clones
cDNAs were amplified by PCR in a reaction mixture containing 10 μl of 2.5× MasterMix (Eppendorf) 0.5 μM primer_F: 5′-ATACTGAGAACTCAAGAGTC-3′, 0.5 μM primer_R: 5′-TTATCCCTGCACACACATG-3′ and nuclease-free water to a final volume of 25 μl. The amplification reaction was performed in a Mastercycler personal (Eppendorf) under the following conditions: predenaturation at 94 °C for 2 min followed by 40 amplification cycles comprising denaturation at 94 °C for 30 s, annealing at 55 °C for 30 s and extension at 72 °C for 30 s and concluded by a final extension at 72 °C for 7 min. The PCR products were separated by 2% agarose gel electrophoresis and purified using the Gel Extraction Kit (Perfectprep Gel Cleanup, Eppendorf, Hamburg). The purified products were inserted into pGEM-T Easy Vector System (Promega), according to the manufacturer's protocol. Ten clones were randomly selected from the resultant white colonies and plasmids were purified using the High Pure Plasmid Isolation Kit (Roche, GmbH) according to the manufacturer's specifications. For automated DNA sequencing, all plasmids were amplified using the Gene Amp PCR System 9600 (Perkin-Elmer, MA). The sequenced products were subjected to a Perkin-Elmer 310 Sequence Analyzer (Perkin-Elmer).
2.7. Specificity and sensitivity test
The specificity of the dual probe real-time PCR was evaluated by cross-reaction tests carried out between RNA extracts from isolates or clinical specimens expressing the entire spectrum of NA subtypes (N2-N9) of WHO reference strain influenza and other viral pathogens, such as Newcastle disease virus (NDV), respiratory syncytial virus (RSV) subgroups A and B, human metapneumovirus (HMPV), coronavirus OC43, coronavirus 229E, infectious bursal disease virus (IBDV) and infectious bronchitis virus (IBV). The sensitivity was established with plasmids containing a copy of the wild type H274 and mutant 274Y serving as reference. The wild type H274 and mutant 274Y plasmids were used to determine the capacity of the real-time PCR assay to detect wild type and Oseltamivir-resistant codon 274 mutants in a single sample. DNA concentration was determined by measuring absorbance at 260 and 280 nm. The two control plasmids were diluted to 104, 103, 102 and 10 copies/μl and each resulting concentration was mixed at 100:0, 75:25, 50:50, 25:75 and 0:100 wild type-to-variant ratios. Real-time PCR analysis of potential codon 274 variants was performed on each ratio at each concentration under the conditions described above.
3. Results
3.1. Detection of oseltamivir resistance by real-time PCR using two labeled TaqMan probes
The result was obtained by using two TaqMan probes labeled with the FAM and VIC fluorescent signal for wild type and mutant detection, respectively. The fluorescent signal resulting from real-time PCR can be interpreted as shown in Fig. 1 . A sample containing only the wild type strain will emit the fluorescent signal exclusively via the FAM channel (530 nm) whereas a sample containing the Oseltamivir-resistant variant with a nucleotide alteration at position 274 of the neuraminidase gene will emit the fluorescent signal via the VIC channel (560 nm). In order to develop and optimize the assay these probes were tested on four sets of mutagenesis and obtained clearly discernible results irrespective of the concentrations of wild type and mutant plasmids or the ratio in which they had been mixed. The clinical samples tested in this assay were isolated from humans, tigers, leopard, cat, dog and various avian species previously infected with H5N1. Two human specimens in this experiment were investigated. The first one isolated from human plasma and collected in Nakhon-nayok province showed a positive result for the wild type only. In contrast, the second one obtained from a Vietnamese patient previously reported by Le et al. (2005) emitted signals specific for both wild type and mutant. The remaining specimens originating from tiger lung, spleen, kidney and liver, leopard brain and the allantoic fluid of various avian species, cat and dog displayed positive results specific for the wild type only.
Fig. 1.
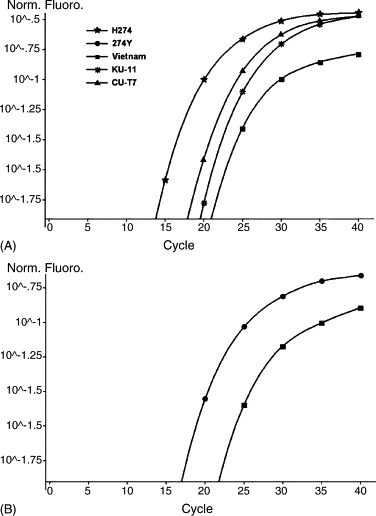
Two fluorescent signals for wild type H274 and mutant 274Y detection emitted by TaqMan probes labeled with FAM (A) and VIC (B), respectively. H274: positive control plasmid, 274Y: positive control plasmid; Vietnam: Oseltamivir-treated Vietnamese patient (Le et al., 2005) showing both fluorescence signals indicative of a combination between wild type and resistant strain, KU-11: Oseltamivir-treated white tiger, CU-T7: Oseltamivir-treated tiger showing only the wild type signal.
3.2. Selection of drug resistant clones
Three specimens, treated with Oseltamivir, were chosen to be cloned into plasmids for confirmation. The first specimen was from a tiger (A/Tiger/Thailand/CU-T7/04) isolated from zoo tigers that had perished during the mid-October 2004 H5N1 influenza outbreak. CU-T7 was isolated from a nasal swab of a tiger that eventually perished but had been treated with Oseltamivir at 75 mg/60 kg twice daily for 4 days prior to specimen collection (Amonsin et al., 2006, Thanawongnuwech et al., 2005) and inoculated into SAN-fowl eggs according to the method described by the Office International des Epizooties (OIE). Ten clones of CU-T7 were randomly selected and sequenced. All the clones were sensitive to Oseltamivir. The second specimen was white tiger (A/Tiger/Thailand/KU-11/04) was isolated from a sick white tiger found positive for H5N1 by nasal swab and subsequently treated with Oseltamivir at 75 mg/60 kg twice daily for 4 days. This tiger survived and a rectal swab was taken. This specimen was inoculated into SAN-fowl eggs. Ten clones of KU-11 were randomly selected and sequenced. All the clones were sensitive to Oseltamivir. The third specimen was cDNA from a Vietnamese patient (Le et al., 2005). Ten clones of this strain were randomly selected and sequenced. Nine of the 10 clones were resistant to Oseltamivir and only 1 clone was sensitive.
3.3. Specificity and sensitivity test
The specificity of the assay by cross-contamination tests were evaluated and found no cross-reactivity to total human DNA, any of the different NA subtypes of influenza A virus, Newcastle disease virus (NDV), respiratory syncytial virus (RSV) subgroups A and B, human metapneumovirus (HMPV), coronavirus OC43, coronavirus 229E, infectious bursal disease virus (IBDV) and infectious bronchitis virus (IBV). Likewise, any significant false positive or non-specific signal in any of the samples tested was not observed. Overall, the results obtained on Oseltamivir resistance with the two labeled probes indicate a high specificity of both primers and probes used for amplification. As for the sensitivity of real-time PCR, the threshold concentration for detecting both wild type (H274) and mutant (274Y) was 10 copies/μl. Furthermore, in order to establish the limits of real-time PCR to detect both wild type and mutant in the same sample, wild type and mutant plasmids were mixed in various ratios and diluted them over a range of concentrations 100:0, 75:25, 50:50, 25:75 and 0:100 ratios of wild type and mutant. The result showed the high sensitivity of the detection that can be detected although the reaction had 7.5:2.5 plasmid copies/μl of wild type and mutant.
4. Discussion
At present, there is a substantial risk of a global influenza A virus subtype H5N1 epidemic not only affecting poultry but also mammalian species including humans. A medication capable of preventing the spread to humans is the neuraminidase inhibitor Oseltamivir. Yet, influenza A virus subtype H5N1 has already developed drug resistance by mutations in the neuraminidase gene leading to amino acid substitutions predominantly at positions 119, 152, 274 and 292 (N2 numbering system) of the enzyme's active site (Gubareva et al., 2000). The amino acid substitution at position 274 identified in mutants selected in the presence of NA inhibitors both in vivo and in vitro has exclusively been found in N1 (Gubareva et al., 2002). In 2005, H5N1 virus resistant to oseltamivir due to an amino acid change from Histidine (H) to Tyrosine (Y) based on a single nucleotide alteration at position 274 has been isolated from three Vietnamese patients one of whom, a 14 years old, recovered (Le et al., 2005) while the remaining two, a 13 and 18 years old, succumbed to the infection (de Jong et al., 2005). Hence, patients found positive for H5N1 infection ought to be monitored for the nucleotide change at position 274 causing resistance to Oseltamivir before the onset of treatment. With the mutation detected in time, alternative treatment applying, for example Zanamivir might save the patient's life.
In this experiment, both probes and primers were specifically designed to detect the nucleotide change causing Oseltamivir resistance. The amino acid substitution of Histidine (H) with Tyrosine (Y) is the consequence of a single nucleotide in the first codon of this amino acid change from C to T. The alignment of theH5N1 neuraminidase gene sequence with more than 200 sequences stored in the Genbank database showed a nucleotide change in the specific probe area yet at a position not triggering the critical amino acid alteration. Hence, the probe was designed to allow for this inconsequential mutation by using a degenerate nucleotide at that position thus closely mimicking the natural situation. Moreover, since the conserved area of the gene restricted the probe's length to 17 nucleotides TaqMan MGB was chosen. The probe was coupled with a minor groove binder enhancing its Tm and had a non-fluorescent quencher attached to the 3′ end, which does not interfere with fluorescent signal detection. After having tested the probes with the mutagenesis control, the result showed high sensitivity and correct distinction between wild type and mutant upon mixing different ratios of wild type and mutant plasmid at low concentrations.
In conclusion, real-time PCR using two labeled TaqMan probes provides a highly specific and sensitive method to detect the amino acid alteration at position 274 of the influenza A subtype H5N1 neuraminidase gene causing oseltamivir resistance. Studies as the one described here could address the potential differences in diagnostic outcomes between patients who develop detectable Oseltamivir resistance and patients who retain only the wild type strain of H5N1. However, the other point mutations of Oseltamivir resistance in H5N1 infected mammalian species need for the further investigation.
Acknowledgements
We would like to express our deep gratitude to the Thailand Research Fund (Senior Research Scholar), Royal Golden Jubilee Ph.D. Program, Center of Excellence in Viral Hepatitis Research, Chulalongkorn University for supporting this study and Roche diagnostics, Thailand for providing mutagenesis primers, plasmid purification kit. We also would like to thank Dr. Surangrat Srisuratanon, Department of Pediatrics, Faculty of Medicine, Srinakharinwirot University, Nakhon Nayok, for her assistance and Ms. Petra Hirsch for critically reviewing the manuscript.
References
- Amonsin A., Payungporn S., Theamboonlers A., Thanawongnuwech R., Suradhat S., Pariyothorn N., Tantilertcharoen R., Damrongwantanapokin S., Buranathai C., Chaisingh A., Songserm T., Poovorawan Y. Genetic characterization of H5N1 influenza A viruses isolated from zoo tigers in Thailand. Virology. 2006;344:480–491. doi: 10.1016/j.virol.2005.08.032. [DOI] [PubMed] [Google Scholar]
- Beigel J.H., Farrar J., Han A.M., Hayden F.G., Hyer R., de Jong M.D., Lochindarat S., Nguyen T.K., Nguyen T.H., Tran T.H., Nicoll A., Touch S., Yuen K.Y., Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 Avian influenza A (H5N1) infection in humans. N. Engl. J. Med. 2005;353:1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- Chutinimitkul S., Bhattarakosol P., Srisuratanon S., Eiamudomkan A., Kongsomboon K., Damrongwatanapokin S., Chaisingh A., Suwannakarn K., Chieochansin T., Theamboonlers A., Poovorawan Y. H5N1 influenza A virus and infected human plasma. Emerg. Infect. Dis. 2006;12:1041–1043. doi: 10.3201/eid1206.060227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong M.D., Tran T.T., Truong H.K., Vo M.H., Smith G.J., Nguyen V.C., Bach V.C., Phan T.Q., Do Q.H., Guan Y., Peiris J.S., Tran T.H., Farrar J. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 2005;353:2667–2672. doi: 10.1056/NEJMoa054512. [DOI] [PubMed] [Google Scholar]
- Fouchier R.A., Munster V., Wallensten A., Bestebroer T.M., Herfst S., Smith D., Rimmelzwaan G.F., Olsen B., Osterhaus A.D. Characterization of a novel influenza A virus hemagglutinin subtype (H16) obtained from black-headed gulls. J. Virol. 2005;79:2814–2822. doi: 10.1128/JVI.79.5.2814-2822.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubareva L.V. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 2004;103:199–203. doi: 10.1016/j.virusres.2004.02.034. [DOI] [PubMed] [Google Scholar]
- Gubareva L.V., Kaiser L., Hayden F.G. Influenza virus neuraminidase inhibitors. Lancet. 2000;355:827–835. doi: 10.1016/S0140-6736(99)11433-8. [DOI] [PubMed] [Google Scholar]
- Gubareva L.V., Kaiser L., Matrosovich M.N., Soo-Hoo Y., Hayden F.G. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J. Infect. Dis. 2001;183:523–531. doi: 10.1086/318537. [DOI] [PubMed] [Google Scholar]
- Gubareva L.V., Webster R.G., Hayden F.G. Detection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assay. Antiviral Res. 2002;53:47–61. doi: 10.1016/s0166-3542(01)00192-9. [DOI] [PubMed] [Google Scholar]
- Hayden F.G., Hay A.J. Emergence and transmission of influenza A viruses resistant to amantadine and rimantadine. Curr. Top. Microbiol. Immunol. 1992;176:119–130. doi: 10.1007/978-3-642-77011-1_8. [DOI] [PubMed] [Google Scholar]
- Hoffmann E., Stech J., Guan Y., Webster R.G., Perez D.R. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 2001;146:2275–2289. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- Ives J.A., Carr J.A., Mendel D.B., Tai C.Y., Lambkin R., Kelly L., Oxford J.S., Hayden F.G., Roberts N.A. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leave virus severely compromised both in vitro and in vivo. Antiviral Res. 2002;55:307–317. doi: 10.1016/s0166-3542(02)00053-0. [DOI] [PubMed] [Google Scholar]
- Jackson H.C., Roberts N., Wang Z.M., Belshe R. Management of influenza: use of new antivirals and resistance in perspective. Clin. Drug Invest. 2000;20:447–454. [Google Scholar]
- Kim C.U., Lew W., Williams M.A., Liu H., Zhang L., Swaminathan S., Bischofberger N., Chen M.S., Mendel D.B., Tai C.Y., Laver W.G., Stevens R.C. Influenza neuraminidase inhibitors possessing a novel hydrophobic interaction in the enzyme active site: design, synthesis, and structural analysis of carbocyclic sialic acid analogues with potent anti-influenza activity. J. Am. Chem. Soc. 1997;119:681–690. doi: 10.1021/ja963036t. [DOI] [PubMed] [Google Scholar]
- Kiso M., Mitamura K., Sakai-Tagawa Y., Shiraishi K., Kawakami C., Kimura K., Hayden F.G., Sugaya N., Kawaoka Y. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet. 2004;364:759–765. doi: 10.1016/S0140-6736(04)16934-1. [DOI] [PubMed] [Google Scholar]
- Le Q.M., Kiso M., Someya K., Sakai Y.T., Nguyen T.H., Nguyen K.H., Pham N.D., Ngyen H.H., Yamada S., Muramoto Y., Horimoto T., Takada A., Goto H., Suzuki T., Suzuki Y., Kawaoka Y. Avian flu: isolation of drug-resistant H5N1 virus. Nature. 2005;437:1108. doi: 10.1038/4371108a. [DOI] [PubMed] [Google Scholar]
- Moscona A. Neuraminidase inhibitors for influenza. N. Engl. J. Med. 2005;353:1363–1373. doi: 10.1056/NEJMra050740. [DOI] [PubMed] [Google Scholar]
- Moscona A. Oseltamivir resistance—disabling our influenza defenses. N. Engl. J. Med. 2005;353:2633–2636. doi: 10.1056/NEJMp058291. [DOI] [PubMed] [Google Scholar]
- Nicholson K.G., Wood J.M., Zambon M. Influenza. Lancet. 2003;362:1733–1745. doi: 10.1016/S0140-6736(03)14854-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payungporn S., Chutinimitkul S., Chaisingh A., Damrongwantanapokin S., Buranathai C., Amonsin A., Theamboonlers A., Poovorawan Y. Single step multiplex real-time RT-PCR for H5N1 influenza A virus detection. J. Virol. Methods. 2005;131:143–147. doi: 10.1016/j.jviromet.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Thanawongnuwech R., Amonsin A., Tantilertcharoen R., Damrongwatanapokin S., Theamboonlers A., Payungporn S., Nanthapornphiphat K., Ratanamungklanon S., Tunak E., Songserm T., Vivatthanavanich V., Lekdumrongsak T., Kesdangsakonwut S., Tunhikorn S., Poovorawan Y. Probable tiger-to-tiger transmission of avian influenza H5N1. Emerg. Infect. Dis. 2005;11:699–701. doi: 10.3201/eid1105.050007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran T.H., Nguyen T.L., Nguyen T.D., Luong T.S., Pham P.M., Nguyen V.C., Pham T.S., Vo C.D., Le T.Q., Ngo T.T., Dao B.K., Le P.P., Nguyen T.T., Hoang T.L., Cao V.T., Le T.G., Nguyen D.T., Le H.N., Nguyen K.T., Le H.S., Le V.T., Christiane D., Tran T.T., de Jong M.D., Schultsz C., Cheng P., Lim W., Horby P., Farrar J., World Health Organization International Avian Influenza Investigative Team Avian influenza A (H5N1) in 10 patients in Vietnam. N. Engl. J. Med. 2004;350:1179–1188. doi: 10.1056/NEJMoa040419. [DOI] [PubMed] [Google Scholar]
- Turner D., Wailoo A., Nicholson K., Cooper N., Sutton A., Abrams K. Systematic review and economic decision modelling for the prevention and treatment of influenza A and B. Health Technol. Assess. 2003;7(iii–iv, xi–xiii):1–170. doi: 10.3310/hta7350. [DOI] [PubMed] [Google Scholar]
- Wang M.Z., Tai C.Y., Mendel D.B. Mechanism by which mutations at His274 alter sensitivity of influenza a virus N1 neuraminidase to oseltamivir carboxylate and zanamivir. Antimicrob. Agents Chemother. 2002;46:3809–3816. doi: 10.1128/AAC.46.12.3809-3816.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherall N.T., Trivedi T., Zeller J., Hodges-Savola C., McKimm-Breschkin J.L., Zambon M., Hayden F.G. Evaluation of neuraminidase enzyme assays using different substrates to measure susceptibility of influenza virus clinical isolates to neuraminidase inhibitors: report of the neuraminidase inhibitor susceptibility network. J. Clin. Microbiol. 2003;41:742–750. doi: 10.1128/JCM.41.2.742-750.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitley R.J., Hayden F.G., Reisinger K.S., Young N., Dutkowski R., Ipe D., Mills R.G., Ward P. Oral oseltamivir treatment of influenza in children. Pediatr. Infect. Dis. J. 2001;20:127–133. doi: 10.1097/00006454-200102000-00002. [DOI] [PubMed] [Google Scholar]
- World Health Oraganization, 2006. Cumulative number of confirmed human cases of Avian Influenza A/(H5N1) reported to WHO [online] http://www.who.int/csr/disease/avian_influenza/country/cases_table_2006_06_20/en/index.html. Accessed 23 June 2006.


