Abstract
Airborne Newcastle disease (ND) viruses in the air of five chicken houses were detected and differentiated by reverse transcriptase polymerase chain reaction (RT-PCR) using degenerate primers. Fifteen air samples were collected with All Glass Impinger-30 (AGI-30) air samplers in each house. Airborne ND viruses were also isolated and virulence identified by in vivo tests. Avirulent viruses were detected both in air samples and swab samples in four houses by degenerate primers based RT-PCR. Virulent viruses were detected only in the air samples by degenerate primers based RT-PCR in two houses. Seven strains viruses were isolated from the RT-PCR positive air samples. Of the seven strains, three strains were virulent viruses and four strains were avirulent viruses identified by in vivo tests. The results showed that it was feasible to detect and differentiate NDV in the air samples using degenerate primers based RT-PCR. This technique could decrease the time it required identify NDV infected flocks while distinguishing between virulent and avirulent viruses. It will help effectively to control Newcastle disease.
Keywords: Airborne Newcastle disease virus, All Glass Impinger-30 (AGI-30), Degenerate primers, Reverse transcription polymerase chain reaction (RT-PCR)
1. Introduction
Airborne and droplet transmission are the major routes for transmission of animal viral diseases, such as Newcastle disease (ND), Avian Influenza, Porcine Reproductive and Respiratory Syndrome (PRRS) and Foot-and-Mouth disease. Newcastle disease (ND) is included in the World Organization (OIE) for Animal Health list of notifiable diseases (former list A). Historically, ND has been a devastating disease of poultry, and the disease remains one of the major problems affecting existing or developing poultry industries in many countries (Alexander, 1995, Alexander, 2003). Newcastle disease virus (NDV), the causative agent of ND, is a non-segmented, single-stranded, negative sense RNA virus that belongs to the genus Avulavirus within the Paramyxovirinae subfamily of the Paramyxoviridae family (Mayo, 2002). Its genome is approximately 15 kb in length and encodes six proteins, namely, nucleoprotein (NP), phosphoprotein (P), matrix (M), fusion (F), Hemagglutinin–Neuraminidase (HN) and large protein (L) or polymerase in the order 3′-leader-NP-P-M-F-HN-L-trailer-5′ (de Leeuw and Peeters, 1999, Pedersen et al., 2004). ‘Traditional’ routes of NDV transmission like direct animal contact, contaminated feed, water, implements, transport contact or transmission by people were identified (Alexander, 1988, Alexander, 2003). Airborne transmission was also one important route for transmission of Newcastle disease. Alexander, 1988, Alexander, 1995, Alexander, 2003 recognized that the majority of ND infections were attributable to the inhalation of small viral aerosols or viral droplets by susceptible chickens. Airborne transmission was considered a significant factor in the 1970–1971 ND outbreaks in England (Hugh-Jones et al., 1973) and the 1973 ND epidemic in Northern Ireland (McFerran, 1989). Airborne NDV can also infect humans and cause clinical symptoms such as mild conjunctivitis (Chang, 1981). Therefore, airborne NDV continues to be a major threat to chickens and people.
Conventionally, NDV was characterized by isolation of the virus followed by in vivo tests such as intracerebral pathogenicity index, intravenous pathogenicity index and mean death time in SPF chicken embryo/birds for pathotyping. These tests are cumbersome, labor intensive, inhumane and some times inconclusive (Tiwari et al., 2004). In order to meet the need of production and eradication of Newcastle disease as soon as possible, more rapid methods that enable detection and differentiation of pathotypes of the airborne virus are required. RT-PCR alone using degenerate primers designed from the ‘F’ gene for detection and differentiation of airborne NDV avirulent strains from virulent strains is described in the present report. This technique could decrease the time required to identify NDV infected flocks while distinguishing between virulent and avirulent viruses. It will help to control effectively Newcastle disease in future.
2. Materials and methods
2.1. Viruses and standard serum
The NDV vaccine strain La Sota (GenBank accession no. AF077761) and Chinese standard virulent NDV F48E9 strain (GenBank accession no. AY508514) were used as positive and negative controls of RT-PCR based degenerate primers. The control viruses were purchased from China Institute of Veterinary Drug Control. Other known viruses, such as SGM01 (GenBank accession no. DQ227248), WHZ03 (GenBank accession no. DQ363530), B1 (GenBank accession no. AF309418) were kindly provided by Research Center for Animal Disease Control Engineering, Shandong Agricultural University, China. Standard serum was purchased from China Animal Health and Epidemiology Center, which was used to identify NDV by the hemagglutination inhibition test.
2.2. Eggs and chickens
Specific pathogen free (SPF) chickens and 9- to 10-day old SPF embryonating chicken eggs were purchased from the Poultry Institute, Chinese Academy of Agricultural Sciences. Chickens were housed in positive and negative-pressure isolators and were supplied with water through automatic feeder and enough feed to sustain the chickens throughout the experiment. Chickens were utilized for the Intracerebral pathogenicity index (ICPI) and Intravenous pathogenicity index (IVPI) experiment, embryonated eggs were used for viral propagation, isolation and the mean death time (MDT) test.
2.3. Chicken houses studied
Five chicken houses were studied in this experiment. A description of these chicken houses is given in Table 1 . In addition, egg production fell at 170–180 days of ages, which was due to the infection with Newcastle disease virus in house C two years ago. There was no remarkable reduction in egg production history in the other four houses. The five flocks had no clinical ND or increased mortality at the time of air sampling.
Table 1.
Description of six chicken houses studied.
| Chicken house | Breeds | RDa | Layout (unit) | Days | Tb (°C) | RHc (%) | WSd (m s−1) | Vaccine historye |
||
|---|---|---|---|---|---|---|---|---|---|---|
| Route | Days | Vaccine | ||||||||
| A | Broiler | 11 | Cage | 33 | 25–26 | 41–42 | 0–1.5 | Intraocular | 28 | La sota |
| B | Broiler | 25 | Floor | 25 | 26–27 | 47–48 | 0 | DW/MIe | 20 | TVf |
| C | Layer | 8.6 | Cage | 240 | 23–24 | 43–45 | 0 | DW | 230 | La Sota |
| D | Layer | 10.8 | Cage | 162 | 24–25 | 71–72 | 0 | DW | 160 | La Sota |
| E | Breeder | 8.3 | Cage | 269 | 23–26 | 48–52 | 0–2 | MI | 250 | TVg |
RD: raising density;
T: temperature;
RH: relative humidity;
WS: wind speed.
DW: drinking water; MI: intramuscular injection.
Chickens were vaccinated at 20 days of age using triple vaccine (NDV (La Sota)–Infectious Bronchitis–Infections Bursal Disease) through drinking water (freeze-drying) and intramuscular injection (oil-based).
Triple vaccine (NDV (La Sota)–Infectious Bronchitis–Egg Drop Syndrome) (oil-based).
2.4. Sampling
Air samples were collected by liquid impingement with AGI-30 samplers (Ace Glass Co., Vineland, NJ) operated in the centre and four corners of each chicken house. The AGI-30 samplers, each containing 20 ml of collection buffer (0.1 M phosphate buffer, pH 7.2), were operated indoors at the manufacturer's suggested flow rate of 12.5 l/min for 20 min (Alvarez et al., 1995, Lin et al., 1997). Sampling height was set at 1 m from the ground. To avoid an extensive formation of foam that could interfere with the physical sampling process, antifoam A (Sigma Chemical Company, St. Louis) was added to the collection media prior to sterilization (Chinivasagam and Blackall, 2005). Four impingers were used at the same one sampling point per sampling time, facing the same direction. They were mixed as one sample. Three sampling times were conducted continuously at the same one sampling point in each chicken house.
On arrival at the laboratory, the inlet of each sampler was rinsed with 1–5 ml of sterile phosphate buffer to collect cells trapped in the curved inlet tube. Wash buffer was added to the collection buffer, resulting in a total volume of 23–24 ml and then the air samples were stored at 4 °C overnight. All microbiological cultures were conducted within 24 h of arrival at the laboratory (Chinivasagam and Blackall, 2005). Most chickens seemed undisturbed and were breathing quietly during sample collection.
Oropharyngeal and cloacal swabs were collected at random from 15 chickens in houses A and B and 10 chickens in houses C–E. Swabs were placed in one tube and the supernatant fluids were removed after processed and stored at −70 °C until tested by RT-PCR.
2.5. Viral RNA preparation
Air collection fluids were first spun at 10,000 × g for 45 min to remove the pelleted bacteria and dust, followed by ultracentrifugation at 100,000 × g for 2 h to collect the viral pellet.
Viral RNA was isolated from the air collection pellet and swabs supernatant fluids using Trizol reagent (Invitrogen, Carlsbad, CA). The viral RNA was resuspended in diethylpyrocarbonate (DEPC)-treated water and stored at −70 °C until further use. Controls and other known viruses were handled identically to the air samples taken from chicken houses.
2.6. RT-PCR using degenerate primers
Degenerate primers for the RT-PCR amplification for the main function region of the fusion protein gene of NDV in the air samples swabs and were designed on the basis of published primers (Kant et al., 1997, Tiwari et al., 2004). Three primers [P1-5′-TTGATGGCAGGCCTCTTGC-3′ nucleotide position 141–159; P2-5′-AGCGT(C/T)TCTGTCTCCT-3′ nucleotide position 395–380; P3-5′-G(A/G)CG(A/T)CCCTGT(C/T)TCCC-3′ nucleotide position 395–380] were synthesized in Sangon Biotechnology (Shanghai, China). Both the amplicons of P1 + P2 (virulent) and P1 + P3 (avirulent) were 255 bp. RT-PCR was performed using BioRT Two Step RT-PCR Kit (BIOER Technology CO., LTD. Hangzhou, China). The RT reaction mixture was incubated at 42 °C for 45 min and 95 °C for 5 min followed by chilling on ice bath for 5 min. The PCR reaction mixture was preheated at 94 °C for 3 min and then cycled 35 times at 94 °C for 30 s, 55 °C for 30 s, 72 °C for 45 s; and finally extended at 72 °C for 5 min. The PCR products were analyzed by electrophoresis on a 1.5% agarose gel, stained with ethidium bromide (EB).
2.7. Airborne NDV isolation and plaque purification
The allantoic cavity of 9- to 11-day-old embryonated SPF chicken eggs was inoculated with 0.2 ml of the aerosol collecting medium, incubated at 37.0 °C for 4–6 days. Eggs were monitored, and dead or dying embryos were removed as they arose. Embryos dying within 24 h of inoculation were discarded. Allantoic fluids were collected from the remaining eggs upon death or at the end of the incubation period, chilled to 4 °C, and examined with haemagglutination (HA) test and haemagglutination inhibition (HI) test according to the OIE standard (OIE, 2004). Fluids that gave a negative reaction were passaged into at least one further batch of eggs.
In order to exclude interference from other pathogens, viruses were purified by using the virus plaque technique. If morphology was maintained after three successive steps of purification, then plaques were picked again and a sample was injected into 10-day-old embryonated eggs. Fluids were harvested, clarified by low-speed centrifugation and stored at −20 °C.
2.8. Pathogenicity indices of airborne Newcastle disease viruses
Pathotyping of the isolates involved virus inoculation of 10-day-old embryonated, SPF eggs to determine the mean death time (MDT) in eggs of the embryos, and further testing entailed to determine the intracerebral pathogenicity index (ICPI) values in 1-day-old SPF chicks and the intravenous pathogenicity index (IVPI) test in 6-week-old SPF chickens. All the tests were performed using standard procedure according to the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Chapntiters 2.1.12 and 2.1.15 (OIE, 2004).
3. Results
3.1. Degenerate primers based RT-PCR for detection and differentiation of NDV in the air samples and swabs
As expected, using the mixed primers of P1 + P2 the RT-PCR generated a fragment of 255 bp only with RNA isolated from NDV F48E9 strain, SGM01 strain and WHZ03 strain which were already known as velogenic (Fig. 1, Fig. 2 ). Using the mixed primers of P1 + P3 the RT-PCR also resulted in a 255 bp fragment only with RNA of vaccine strain La sota and B1 which were known as lentogenic strains (Fig. 1, Fig. 2).
Fig. 1.
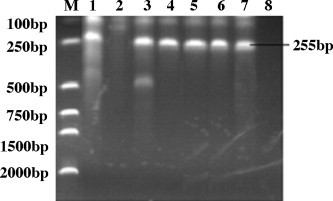
The amplification generated by degenerate primers based RT-PCR of airborne Newcastle disease viruses of representative air samples and controls. Lane M: DL2000 DNA Maker; lane 1: NDV F48E9 strain amplified by primer combination P1 + P2; lane 2: NDV F48E9 strain amplified by primer combination P1 + P3; lanes 3 and 4: representative air samples amplified by primer combination P1 + P2; lanes 5 and 6: representative air samples amplified by primer combination P1 + P3; lane 7: NDV La sota strain amplified by primer combination P1 + P3; lane 8: NDV La sota strain amplified by primer combination P1 + P2.
Fig. 2.
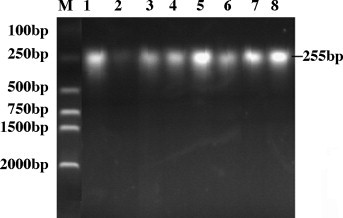
The amplification generated by degenerate primers based RT-PCR of NDV originated from representative swabs and other known NDV. Lane M: DL2000 DNA Maker; Lane 1: NDV B1 strain amplified by primer combination P1 + P3; lane 2: NDV B1 amplified by primer combination P1 + P2; lanes 3 and 4: representative swabs samples amplified by primer combination P1 + P2; lanes 5 and 6: representative swab samples amplified by primer combination P1 + P3; lane 7: NDV SGM01 strain amplified by primer combination P1 + P2; lane 8: NDV WHZ03 strain amplified by primer combination P1 + P2.
Avirulent ND viruses were detected in four out of five houses (houses A, B, C and E), virulent ND viruses were detected in two out of five houses (houses B and C) and no virus was detected in house D (Table 2 ).
Table 2.
Results of detection and isolation of airborne Newcastle disease viruses.
| House | P1 + P2a |
P1 + P3b |
Double positivec |
|||
|---|---|---|---|---|---|---|
| Air samples | Swabs | Air samples | Swabs | Air samples | Swabs | |
| A | 0/15 | 0/15 | 2/15 | 4/15 | 0/15 | 0/15 |
| B | 5/15 | 0/15 | 7/15 | 5/15 | 3/15 | 0/15 |
| C | 2/15 | 0/10 | 6/15 | 5/10 | 1/15 | 0/10 |
| D | 0/15 | 0/10 | 0/15 | 0/10 | 0/15 | 0/10 |
| E | 0/15 | 0/10 | 7/15 | 1/10 | 0/15 | 0/10 |
| Total | 7/75 | 0/60 | 22/75 | 15/60 | 4/75 | 0/60 |
NDV positive samples out of 15 samples of detected by the mixed primers of P1 + P2.
NDV positive samples out of 15 samples of detected by the mixed primers of P1 + P3.
NDV positive samples out of 15 samples of detected by the mixed primers of P1 + P2 and P1 + P3 simultaneously (double positive).
Only avirulent viruses were detected in two air samples and four swab samples in house A. Avirulent viruses were detected in seven air samples and five swab samples and virulent viruses were detected only in five air samples in house B. Avirulent viruses were detected in six air samples and five swab samples and virulent viruses were detected only in two air samples in house C. Avirulent viruses were detected in seven air samples and one swab samples in house E (Table 2).
3.2. Airborne NDV isolation and pathogenicity indices test
Seven NDV strains were obtained. Three were virulent strains and four were avirulent strains (Table 3 ). One strain avirulent (NDV01) was isolated in house A; one virulent strain (NDV02) and one avirulent strain (NDV03) were isolated in house B; two virulent strains (NDV04, NDV05) and one avirulent strain (NDV06) were isolated in house C; one avirulent strain (NDV07) was isolated in house E (Table 2, Table 3).
Table 3.
Pathogenicity of airborne NDV isolates.
| NDV strain | Chicken house | DAa | MDTb | ICPIc | IVPId | Virulence |
|---|---|---|---|---|---|---|
| NDV01 | A | 0.5–0.7 | 100 | 0.0 | 0.00 | Avirulent |
| NDV02 | B | 1.9–2.1 | 54.4 | 1.70 | 2.70 | Virulent |
| NDV03 | B | 0.5–0.7 | 101 | 0.20 | 0.00 | Avirulent |
| NDV04 | C | 2.1–2.3 | 46 | 1.91 | 2.56 | Virulent |
| NDV05 | C | 1.9–2.2 | 58.5 | 1.75 | 2.73 | Virulent |
| NDV06 | C | 0.5–0.7 | 100 | 0.46 | 0.00 | Avirulent |
| NDV07 | E | 0.5–0.6 | 101 | 0.52 | 0.16 | Avirulent |
Diameter of Plaque (mm).
Mean death time (MDT).
Intracerebral pathogenicity index (ICPI).
Intravenous pathogenicity index (IVPI).
The overt clinical signs observed in chickens following intravenous inoculation were tremors and paralysis, typical of a neurotropic virus infection. Those with severe paralysis were euthanized and recorded as dead.
4. Discussion
In the present study, RT-PCR was applied on NDV in air samples using degenerate primers designed from F gene encoding for cleavage site. Using both primer combinations P1 + P2 and P1 + P3, a specific product of 255 bp could be amplified from the air samples, swab samples, control NDV strains and other known viruses (Fig. 1, Fig. 2). A total of 75 air samples and 60 swab samples were collected from the five chicken houses. Both virulent and avirulent viruses were detected by RT-PCR and were also isolated from air samples in the vaccinated chicken flocks (Table 1, Table 2). However, only avirulent viruses were detected by RT-PCR in the swab samples (Table 2). It indicated that only a small proportion of bird samples could not represent all the chickens and bird samples were collected from all the chickens was impractical at the same time. Environmental sampling has several advantages for flock surveillance, including minimizing direct human contact with flocks, eliminating individual bird handling, and providing a time- and cost-efficient sampling technique (Hietala et al., 2005). Air sampling of poultry environments to detect NDV, is not a new concept. Delay et al. (1948) documented originally the recovery of Newcastle disease virus from poultry environment air samples in 1948, and Hietala et al. (2005) collected successfully air of poultry environments to detect airborne NDV by real-time reverse transcriptase PCR. The evaluation of environmental air sampling to detect an aerosolized virus indicated that the technique has potential application as an effective sampling tool.
Since the 1980s, strict vaccination programs have been practised in both large-scale poultry operations and small poultry farms. The prevalence of ND has been both mild and sporadic. However, NDV still induces a high mortality rate in some regions in the world, which is caused mainly by virulent NDV. In the current study, virulent NDV were detected in seven air samples of two chicken houses, though there was no prevailing of ND. Virulent NDV may have been present in the chicken house and the surrounding environment constantly. Airborne NDV was a major threat to chickens. Once some of the failed immunized chickens were challenged by virulent NDV, the spread of ND will probably occur (Toyoda et al., 1989, Seal et al., 1995). It is important to develop rapid and accurate methods to monitor and differentiate NDV aerosols in chicken houses. The specificity, sensitivity, and reduced processing time of PCR are suitable for applications for aerobiological monitoring for the detection of small numbers of targeted microorganisms (Saiki et al., 1988, Alvarez et al., 1995). Agranovski et al. (2004) had proven that the PCR method could be utilized in detection the Vaccinia virus and considered that even in case of some decay, collected fluid could be tested by RT-PCR to detect qualitatively the existence of the Severe Acute Respiratory Syndrome (SARS) virus in the ambient air.
Both avirulent and virulent viruses could be detected in the same air samples in the present study (Table 2). Therefore, differentiation of virulent and avirulent strains in the air is an important aspect of diagnosis of virus aerosol. Kant et al. (1997) have developed an RT-PCR which detected and differentiated two pathotypes, virulent (velogenic) and non-virulent (lentogenic), of NDV strains directly in tissue homogenate. Tiwari et al. (2004) also demonstrated that degenerate primers based RT-PCR was a simple and rapid for the detection and differentiation of virulent and avirulent NDV, which is important for the control of the disease in the event of the outbreaks.
Airborne viruses in the air samples were also isolated and differentiated by in vivo tests (Table 3). Viruses could be isolated from all RT-PCR positive samples and seven viruses were obtained by purified assay (Table 3). As demonstrated in the present study, the use of an available air sampler, paired with virus detection using degenerate primers RT-PCR, allows environmental air sampling to be a more accessible, time-efficient, and a practical surveillance tool than described previously, which was also demonstrated by Hietala et al. (2005). The current study opens new possibilities of moving to a next development stage related to the replacement of the standard RT-PCR with the available multichannel real time RT-PCR capable of providing quantitative results within even shorter time periods for a number of microorganisms simultaneously.
Acknowledgments
This work was supported by a grant from University Science Foundation for Young Scholars (2008ZRQNZ029), the Ph.D. Programs Foundation of Ministry of Education of China (no. 20060434007) and the Shandong province Natural Science Foundation of China (no. Y2006d14). We are indebted to National Reference Laboratory for Newcastle Diseases, Animal Quarantine Institute, Ministry of Agriculture, People's Republic of China and Animal Disease Prevention Technology of and Research center of Shandong Province, People's Republic of China for assistance in the trial.
References
- Agranovski I., Safatov A., Pyankov O., Sergeev A.N., Agafonov A., Ignatiev G., Ryabchikova E., Borodulin A., Sergeev A.A., Doerr H., Rabenau H., Agranovski V. Monitoring of viable airborne SARS virus in ambient air. Atmos. Environ. 2004;38:3879–3884. doi: 10.1016/j.atmosenv.2004.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander D.J. Newcastle disease: methods of spread. In: Saif Y.M., Barnes H.J., Glisson J.R., Fadly A.M., McDougald D.J., Swayne D.E., editors. Diseases of Poultry. 11th ed. Iowa State Press; Ames: 1988. pp. 63–100. [Google Scholar]
- Alexander D.J. The epidemiology and control of avian influenza and Newcastle disease. J. Comp. Pathol. 1995;112(2):105–126. doi: 10.1016/s0021-9975(05)80054-4. [DOI] [PubMed] [Google Scholar]
- Alexander D.J. Newcastle disease, other paramyxoviruses and pneumovirus infections. In: Saif Y.M., Barnes H.J., Glisson J.R., Fadly A.M., McDougald D.J., Swayne D.E., editors. Diseases of Poultry. 11th ed. Iowa State Press; Ames, IA: 2003. pp. 63–100. [Google Scholar]
- Alvarez A.J., Buttner M.P., Stetzenbach L.D. PCR for bioaerosol monitoring: sensitivity and environmental interference. Appl. Environ. Microb. 1995;61(10):3639–3644. doi: 10.1128/aem.61.10.3639-3644.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang P.W. Newcastle disease. In: Beran G.W., editor. vol. II. CRC Press; Baton Raton: 1981. pp. 261–274. (CRC Handbook Series in Zoonose. Section B: viral Zoonoses). [Google Scholar]
- Chinivasagam H.N., Blackall P.J. Investigation and application of methods for enumerating heterotrophs and Escherichia coli in the air within piggery sheds. J. Appl. Microbiol. 2005;98:1137–1145. doi: 10.1111/j.1365-2672.2005.02560.x. [DOI] [PubMed] [Google Scholar]
- Delay P.D., DeOme K.B., Bankowski R.A. Recovery of pneumoencephalitis (Newcastle) virus from the air of poultry houses containing infected birds. Science. 1948;107:474–475. doi: 10.1126/science.107.2784.474-a. [DOI] [PubMed] [Google Scholar]
- de Leeuw O., Peeters B. Complete nucleotide sequence of Newcastle disease virus: evidence for the existence of a new genus within the subfamily Paramyxovirinae. Gen. Virol. 1999;80(Pt. 1):131–136. doi: 10.1099/0022-1317-80-1-131. [DOI] [PubMed] [Google Scholar]
- Hietala S.K., Hullinger P.J., Crossley B.M., Kinde H., Ardans A.A. Environmental air sampling to detect exotic Newcastle disease virus in two California commercial poultry flocks. J. Vet. Diagn. Invest. 2005;17(2):198–200. doi: 10.1177/104063870501700219. [DOI] [PubMed] [Google Scholar]
- Hugh-Jones M., Allan W.H., Dark F.A., Harper G.J. The evidence for the airborne spread of Newcastle disease. J. Hyg. Camb. 1973;71:325–339. doi: 10.1017/s0022172400022786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant A., Koch G., van Roozelaar F., Balk F., Huurne A.T. Differentiation of virulent and non-virulent strains of Newcastle disease virus with in 24 hours by polymerase chain reaction. Avian Dis. 1997;26:837–840. doi: 10.1080/03079459708419257. [DOI] [PubMed] [Google Scholar]
- Lin X., Willeke K., Ulevicius V., Grinshpun S.A. Effect of sampling time on the collection efficiency of all-glass impinge. AIHA J. 1997;58:480–488. [Google Scholar]
- Mayo M.A. Virus taxonomy—Houston 2002. Arch. Virol. 2002;147:1071–1076. doi: 10.1007/s007050200036. [DOI] [PubMed] [Google Scholar]
- McFerran, J.B., 1989. Control of Newcastle disease in Northern Ireland. Proceedings of the Avian Exotic Disease Control Seminar. Animal Health Report 2, NSW Agriculture and Fisheries, Glenfield, NSW, Australia, pp. 16–21.
- OIE . Office International Des Epizooties—Manual of Standards for Diagnostic Tests and Vaccines. 5th ed. OIE; Paris: 2004. Newcastle disease. [Google Scholar]
- Pedersen J.C., Senne D.A., Woolcock P.R., Kinde H., King D.J., Wise M.G., Panigrahy B., Seal B.S. Phylogenetic relationships among virulent Newcastle disease virus isolates from the 2002–2003 outbreak in California and other recent outbreaks in North America. J. Clin. Microbiol. 2004;42(5):2329–2334. doi: 10.1128/JCM.42.5.2329-2334.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saiki R.K., Gelfand D.H., Stoffel S., Scharf S.J., Higuchi R., Horn G.T., Mullis K.B., Erlich H.A. Primer-directed enzymatic amplification of DNA with a thermostable DNA polymerase. Science. 1988;239:487–494. doi: 10.1126/science.2448875. [DOI] [PubMed] [Google Scholar]
- Seal B.S., King D.J., Bennet J.D. Characterization of Newcastle disease virus isolates by reverse transcription PCR coupled to direct nucleotide sequencing a development of sequence database for pathotype prediction and molecular epidemiological analysis. J. Clin. Microbiol. 1995;33:2624–2630. doi: 10.1128/jcm.33.10.2624-2630.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari A.K., Kataria R.S., Nanthakumar T., Dash B.B., Desai G. Differential detection of Newcastle disease virus strains by degenerate primers based RT-PCR. Comp. Immunol. Microb. 2004;27:163–169. doi: 10.1016/j.cimid.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Toyoda T., Sakaguchi T., Hirota H., Gotoh B., Kuma K., Miyata T., Nagai Y. Newcastle disease virus evolution. II: Lack of gene recombination in generating virulent and avirulent strains. Virology. 1989;169:273–282. doi: 10.1016/0042-6822(89)90152-9. [DOI] [PubMed] [Google Scholar]


