Abstract
Background Comorbidity in the metacarpophalangeal joint (MCPj) of the thumb, i.e., hyperextension or ulnar collateral instability, could affect the outcome of arthroplasty in the thumb carpometacarpal joint (CMCj).
Objective In a retrospective study, we evaluated the effect of arthrodesis of the MCPj for thumbs with unstable MCPj and simultaneous ligament reconstruction tendon interposition (LRTI) arthroplasty for the CMCj in terms of strength, function, and patient satisfaction.
Patients and Methods A total of 69 thumbs treated with a LRTI arthroplasty of the CMCj were included. In 14 of those cases, an arthrodesis of the MCPj was performed as well. In 12 thumbs, both procedures were done simultaneously; in one case MCPj arthrodesis followed LRTI arthroplasty, whereas one patient already had MCPj arthrodesis at time of LRTI arthroplasty. Those 14 thumbs were compared with the control group of 55 thumbs who had only undergone LRTI. At a mean follow-up of 4 to 5 years (mean 54 [10–124] months) postoperative assessments included range of motion (ROM) of the CMC, MCP, and interphalangeal (IP) joint of the thumb, as well as any instability of the MCPj. Pinch and grip strength were examined, also the visual analogue scale (VAS), patient satisfaction, QuickDASH, PRWE-Thumb, and the Kapandji's Opposition Score. Radiologically, proximalization of the first metacarpal bone was measured. Student's t -test was used to determine significance, p < 0.05 was considered significant.
Results Additional arthrodesis of the MCPj provided no significant difference of function in thumbs that only had a hyperextension-instability. However, in thumbs with marked ulnar instability, stronger pinch-grip was obtained with arthrodesis, compared with only LRTI.
Conclusion In patients with advanced painful thumb CMCj osteoarthritis, we recommend (simultaneous) arthrodesis of the MCPj, to allow a stable thumb grip if there is additional marked ulnar collateral ligament instability.
Level of Evidence This is a Level III, retrospective comparative study.
Keywords: MCP joint, ulnar instability, hyperextension, CMC joint osteoarthritis, LRTI Arthroplasty
The main task of the thumb is to provide a stable counter-grip against the long fingers. Instability in the metacarpophalangeal joint (MCPj) often occurs as comorbidity in thumb carpometacarpal joint (CMCj) osteoarthritis 1 ( Fig. 1 ). Hyperextension-instability was the main limiting factor for the counter-grip, but quite often there was additional ulnar collateral instability. Until now, this type of instability in the MCPj was not described as important with respect to limited function.
Fig. 1.

Hyperextension as frequent comorbidity in osteoarthritis of the CMCj, anterior–posterior ( A ) and oblique ( B ) view. CMCj, carpometacarpal joint.
Trapeziectomy with or without interposition/ligamentoplasty is considered the standard treatment for advanced painful thumb CMCj osteoarthritis. 2 But there is still little agreement on management with concomitant instability/hyperextension in the MCPj.
As early as 1986, Burton and Pellegrini described it as a failure not to treat instability of the MCPj at time of surgery for thumb CMCj osteoarthritis. 3
In 1988, Eaton and Floyd noted that hyperextension decreases pinch strength, and therefore recommended to restore mechanical efficiency by stabilization of both CMCj and MCPj. 4 They proposed temporary stabilization of the MCPj with K-wires in hyperextension below 30 degrees and volar capsulodesis over 30 degrees of hyperextension. Besides temporary K-wiring, other authors advocated tendon-transfer, volar capsulodesis, or sesamoidesis for less severe cases, and arthrodesis for cases over 40 degrees of hyperextension, 1 5 whereas others suggested arthrodesis already at more than 30 degrees. 6
Hyperextension greater than 30 degrees was also stated by de Smet et al as a “general” indication for surgical therapy, and in their investigation, no difference in outcome was seen between capsulodesis and arthrodesis. 7
So far, only Brogan et al referred to associated ulnar instability. In 2012, they described their choice of therapy depending on presence of osteoarthritis and/or ulnar instability 8 : without osteoarthritis, they perform tenodesis with APL (abductor pollicis longus tendon) and EPB (extensor pollicis brevis tendon). If there is arthritis or “marked” ulnar instability in the MCPj, they perform arthrodesis. However, this decision to change therapy due to ulnar instability in MCPj was only mentioned in a brief statement, without supporting data or further definition of “marked” ulnar instability.
In summary, various suggestions of techniques were presented, but there is little evidence in the management of instability in the MCPj and still no general recommendation.
The purpose of this study was to examine whether arthrodesis of the MCPj simultaneously performed with LRTI arthroplasty result in a functional significant difference. This was based on the following hypothesis:
Does (simultaneous) arthrodesis in the MCPj with pronounced hyperextension instability change function?
Following the results, we again assessed our data and a second hypothesis arose:
Does (simultaneous) arthrodesis in the MCPj with pronounced ulnar instability change function?
And if so, which grade of concomitant ulnar instability/ hyperextension in the MCPj should be addressed?
Patients and Methods
The study was designed as a single center retrospective study. We analyzed the outcome of a combined arthrodesis in the MCPj at pronounced instability, with LRTI arthroplasty for osteoarthritis of the CMCj of the thumb.
All patients had a painful grade III or IV (Eaton–Littler) thumb CMCj osteoarthritis refractory to conservative treatment. Between January 2006 and February 2016, 161 LRTI arthroplasties were performed, 24 thumbs were operated on both sides, and four patients had one side operated at another clinic. Seven thumbs were excluded due to recent operations on the other side or other hand problems at time of follow-up. Measurements could be performed on 69 thumbs with a mean follow-up of 4.5 years postoperatively (mean FU: 54 [10–121] months). In 14 thumbs, an additional arthrodesis in the MCPj was performed. These thumbs presented with either distinct instability or a combination of instability and osteoarthritis in the MCPj. Hyperextension instability of 40 degrees existed in 7 thumbs; two thumbs had hyperextension instability of 50 degrees and one thumb of 70 degrees. In five thumbs, in addition to the hyperextension instability, the MCPj was also ulnar instable. In four thumbs, there was preexisting painful osteoarthritis.
In 12 of those 14 cases, the two procedures were performed simultaneously. One patient received arthrodesis as a secondary procedure 15 months after LRTI arthroplasty; one patient already had an arthrodesis in the MCPj because of posttraumatic osteoarthritis, followed by LRTI arthroplasty 45 months later. In these two cases, time of follow-up was counted from the second surgery.
Postoperatively, range of motion (ROM) of CMC, MCP, and interphalangeal (IP) joint of the thumb was measured on both sides. Stability of MCPj was noted for active and passive motion at two levels ( Video 1 ). Grip strength was measured with Jamar dynamometer, and key (lateral) pinch strength with Jamar pinch-meter ( Fig. 2 ), each rated in absolute values in pounds (lb) and in percentage to the opposite side. The subjective parameters were visual analogue scale (VAS) to estimate the level of pain, and a six-step scale to evaluate postoperative satisfaction (1: best; 6: worst). To assess function, the QuickDASH score (Disabilities of Arm, Shoulder, and Hand), the PRWE-Thumb score (Patient-Rated Wrist Evaluation, modified for evaluation of function of the thumb), and Kapandji's score were used.
Fig. 2.

Measurement of lateral (key) pinch strength.
Video 1
Evaluation of stability of the MCPj. MCPj, metacarpophalangeal joint.
Radiologically, proximalization of the first metacarpal bone was recorded by measurement of the mean scapho–metacarpal distance (mm). This consists of the average of three distance measurements, which were executed at the radial and ulnar margins, as well as centrally from the distal scaphoid pole and each in the axis of the first metacarpal.
At our institution, LRTI arthroplasty of the CMCj is usually performed using a distally based flexor-carpi-radialis partial tendon strip suspension, pulled through a burr-hole in the base of the first metacarpal. Only in two cases, there was either no suspension or an interposition by an APL tendon strip because the FCR tendon was too low caliber or appeared too eroded to harvest. The angle of fixation in MCP arthrodesis is usually 10 to 15 degrees of flexion. In 11 cases, fixation was done with a dorsal plate (MOH/KLS Martin or Aptus/Medartis; Fig. 3 ). In three cases, the technique of tension band wiring was used. Postoperatively, the hand including the thumb below the IP joint was protected in an orthosis for 6 weeks.
Fig. 3.

Postoperative after MCPj arthrodesis and LRTI arthroplasty, X-ray in anterior–posterior ( A ) and lateral ( B ) view of the thumb. MCPj, metacarpophalangeal joint; LRTI, ligament reconstruction tendon interposition.
For further evaluation and comparison based on these parameters, subgroups were formed. Group A (arthrodesis) includes thumbs that received arthrodesis in addition to LRTI arthroplasty. Thumbs in Group NA (nonarthrodesis) only got LRTI arthroplasty.
Group NA was subdivided in three groups according to the degree of hyperextension in the MCPj ( NA H) . Group 1 (NA H 1) includes hyperextension up to 10 degrees, Group 2 (NA H 2) major 10 to 40 degrees, and Group 3 (NA H 3) major to 40 degrees ( Fig. 4 ).
Fig. 4.

For comparison, the nonarthrodesis group (NA) was subdivided in three groups according to the degree of hyperextension in the MCPj (NA H). MCPj, metacarpophalangeal joint; NA H, nonarthrodesis group.
When the first results were available, a second hypothesis emerged. To answer this, the NA H groups were again subdivided in three subgroups of ulnar instability (NA HU) . Each subgroup one up to 10 degrees ulnar instability (NA HU x.1), subgroup two major 10 degrees up to 30 degrees (NA HU x.2), and subgroup three major of 30 degrees of ulnar instability (NA HU x.3; Fig. 5 ).
Fig. 5.
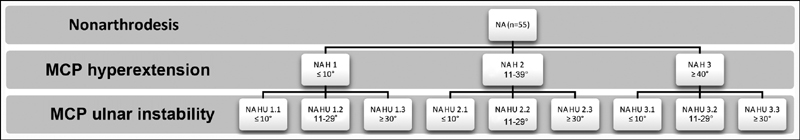
The NA H groups were again subdivided in three subgroups according to ulnar instability (NA HU). NA H, nonarthrodesis group.
As hyperextension does not play a role in our data, but ulnar instability does; the following subgroups allowed looking for further detail ( NA U ). The boundaries of the subdivision were defined as before. Subgroup one up to 10 degrees ulnar instability (NA U 1), subgroup two major 10 degrees up to 30 degrees (NA U 2), and subgroup three more than 30 degrees of ulnar instability (NA U 3; Fig. 6 ).
Fig. 6.

The initial nonarthrodesis group (NA) was then subdivided in three groups according to the degree of ulnar instability in the MCPj (NA U). MCPj, metacarpophalangeal joint.
Baseline characteristics were comparable in the groups and subgroups for mean age at operation, Eaton's classification, sex, left/right distribution, as well as dominant and powerful hands operated on, respectively ( Tables 1 , 2 , 3 ).
Table 1. Characteristics of the three nonarthrodesis subgroups (NA H), divided according the degree of hyperextension in the MCPj, faced to the characteristics of the arthrodesis group (A).
| Mean (min–max) value |
A (
n
= 14)
arthrodesis |
NA (
n
= 55)
nonarthrodesis subdivided according to MCP hyperextension |
||
|---|---|---|---|---|
| NA H 1 ≤ 10° |
NA H 2 11–39° |
NA H 3 ≥ 40° |
||
| n (thumbs) | 14 | 19 | 23 | 13 |
| Age (y) | 68 (54–86) | 66 (48–78) | 69 (50–84) | 63 (53–74) |
| Sex (f:m) | 12:2 | 19:4 | 22:1 | 12:1 |
| Dominant hand operated | 5 | 10 | 12 | 6 |
| Powerful hand operated | 3 | 11 | 14 | 6 |
| FU (mo) | 56 (19–121) | 51 (17–100) | 58 (10–101) | 52 (14–116) |
Abbreviations: FU, follow-up; MCP, metacarpophalangeal.
Table 2. Characteristics of the nine nonarthrodesis subgroups (NA HU), divided according the degree of hyperextension and ulnar instability in the MCPj, and faced to the characteristics of the arthrodesis group (A).
| Mean (min–max) value |
A (
n
= 14)
Arthrodesis |
NA (
n
= 55)
nonarthrodesis subdivided according to MCP hyperextension |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NA H 1 hyperextension ≤ 10° + ulnar instability |
NA H 2 hyperextension 11–39° + ulnar instability |
NA H 3 hyperextension ≥ 40° + ulnar instability |
||||||||
| NA HU 1.1 ≤ 10° |
NA HU 1.2 11–29° |
NA HU 1.3 ≥ 30° |
NA HU 2.1 ≤ 10° |
NA HU 2.2 11–29° |
NA HU 2.3 ≥ 30° |
NA HU 3.1 ≤ 10° |
NA HU 3.2 11–29° |
NA HU 3.3 ≥ 30° |
||
| n (thumbs) | 14 | 4 | 8 | 7 | 6 | 9 | 8 | 2 | 8 | 3 |
| Age (y) | 68 (54–86) | 72 (67–76) | 66 (55–78) | 63 (48–77) | 64 (50–77) | 75 (60–84) | 68 (57–77) | 65 (58–72) | 63 (53–74) | 59 (57–62) |
| Sex (f:m) | 12:2 | 3:1 | 6:2 | 6:1 | 6:0 | 9:0 | 7:1 | 2:0 | 8:0 | 2:1 |
| Dominant hand operated | 5 | 2 | 4 | 4 | 3 | 4 | 5 | 2 | 4 | 0 |
| Powerful hand operated | 3 | 3 | 4 | 4 | 4 | 5 | 5 | 2 | 3 | 1 |
| FU (mo) | 56 (19–121) | 56 (46–66) | 60 (27–100) | 37 (17–73) | 62 (10–92) | 48 (16–93) | 65 (14–110) | 69 (63–75) | 43 (14–116) | 63 (14–124) |
Abbreviations: FU, follow-up; MCPj, metacarpophalangeal joint.
Table 3. Characteristics of the three nonarthrodesis subgroups (NA U), divided according the degree of ulnar instability in the MCPj, faced to the characteristics of the arthrodesis group (A).
| Mean (min–max) value |
A (
n
= 14)
arthrodesis |
NA (
n
= 55)
nonarthrodesis subdivided according to ulnar instability |
||
|---|---|---|---|---|
| NA U 1 ≤ 10° |
NA U 2 11–29° |
NA U 3 ≥ 30° |
||
| n (thumbs) | 14 | 12 | 25 | 18 |
| Age (y) | 68 (54–86) | 67 (50–77) | 68 (53–84) | 64 (48–77) |
| Sex (f:m) | 12:2 | 11:1 | 23:2 | 15:3 |
| Dominant hand operated | 5 | 7 | 12 | 8 |
| Powerful hand operated | 3 | 9 | 12 | 9 |
| FU (mo) | 56 (19–121) | 61 (10–92) | 50 (14–116) | 52 (14–124) |
Abbreviation: FU, follow-up.
A two tailed t -test was used to determine significance in comparison of mean values, p < 0.05 was considered as significant (s**). A p -value of <0.01 or <0.10 is separately marked (s*** or s*, respectively).
Results
Does (simultaneous) arthrodesis in the MCPj with pronounced hyperextension instability change function?
Only in comparison to the subgroup NA H 2, defined as major 10 degrees to 40 degrees hyperextension in MCPj, the arthrodesis group (A) showed a significantly better pinch strength ( A vs. NA H 2 [>10°– < 40°] 101 [67–200] vs. 93 [50–100]; p -value = 0.0167), measured in percentage of the opposite side. Although the mean value of pinch strength (% of opposite side) of the subgroup NA H 1 was similar to that of NA H 2, there were no statistically significant differences in comparison of group A to the other subgroups, concerning grip strength or pinch strength. Also, no differences in pain intensity or satisfaction after surgery were shown. With regard to functional scores (Quick-DASH and PRWE-Thumb), all the NA-groups without arthrodesis scored slightly better, but only showed significance with a lower Quick-DASH-score in the NA H 3 subgroup ( A vs. NA H 3 [≥40°] 31 [0–64] vs. 16 [5–34]; p -value = 0.0306). Concerning the Kapandji's opposition score, a lower mean value was seen in group A with arthrodesis, but also only with significance in comparison to subgroup NA H 3 ( A vs. NA H 3 [≥40°] 7 [4–10] vs. 9 [9–10]; p -value = 0.0002). No differences between the groups were observed in proximalization of the first metacarpal bone ( Table 4 ).
Table 4. Results of the comparison of the arthrodesis group (A) to the NA H subgroups.
| Mean (min–max) value |
A (
n
= 14)
arthrodesis |
NA (
n
= 55)
nonarthrodesis subdivided according to MCP hyperextension |
||
|---|---|---|---|---|
| NA H 1 ≤ 10° |
NA H 2 11–29° |
NA H 3 ≥ 40° |
||
| n (thumbs) | 14 | 19 | 23 | 13 |
| Grip (lb) | 39 (20–80) | 46 (0–110) | 36 (10–100) | 44 (30–60) |
| Grip (% of opposite side) | 99 (50–200) | 103 (50–200) | 103 (75–150) | 101 (67–150) |
| Pinch (lb) | 11 (10–20) | 11 (0–20) | 11 (5–25) | 12 (5–20) |
| Pinch (% of opposite side) | 101 (67–200) | 92 (0–200) | 93 (50–100) s** ( p -value 0.0167) |
100 (50–200) |
| VAS at rest (0–10) | 1 (0–3) | 1 (0–4) | 1 (0–4) | 1 (0–3) |
| VAS at stress (0–10) | 3 (0–7) | 2 (0–6) | 2 (0–6) | 2 (0–4) |
| Quick-DASH (0–100) | 31 (0–64) | 29 (0–68) | 21 (0–61) | 16 (5–34) s** ( p -value 0.0306) |
| PRWE-Thumb (0–100) | 27 (0–50) | 21 (0–67) | 19 (0–73) | 17 (4–45) |
| Satisfaction (1–6) | 2.21 (1–5) | 2 (1–6) | 2 (1–4) | 2 (1–4) |
| Do surgery again (y:n) | 12:2 | 18:1 | 22:1 | 13:0 |
| Kapandji's score (1–10) | 7 (4–10) | 8 (6–10) | 9 (7–10) | 9 (9–10) s*** ( p -value 0.0002) |
| Proximalization X-ray (mm) | 2 (0–4) | 2 (0–3) | 2 (0–4) | 2 (0–5) |
Abbreviations: PRWE-Thumb, patient-rated wrist evaluation, modified for evaluation of function of the thumb; Quick-DASH, the Disabilities of the Arm, Shoulder, and Hand Score; VAS, Visual Analogue Scale.
Our first hypothesis that a (simultaneous) arthrodesis of the MCP joint with pronounced hyperextension leads to significant difference in functional outcome was not confirmed or at best partially confirmed.
Does (simultaneous) arthrodesis in the MCPj with pronounced ulnar instability change function?
The investigation whether an arthrodesis of the MCPj with additional ulnar instability leads to better function, showed no superiority in terms of grip strength. Also, no statistical significance could be observed with regard to pinch strength values. However, the subgroups with more than 30 degrees ulnar instability (NA HU x.3), regardless to the grade of hyperextension, showed lower mean values of pinch force compared with group A, which is supplementary to the LRTI arthroplasty received arthrodesis in the MCPj ( A vs. NA HU 2.3, 11 vs. 11 (lb), and 101 vs. 81 [%]). Even in the subgroup with mild or no hyperextension (≤10°), this effect was apparent ( A vs. NA HU 1.3 , 11 vs. 8 (lb), and 101 vs. 67 [%]). No benefit in terms of pinch strength was observed in comparison to the subgroup with the highest degree of hyperextension (≥40°) and ulnar instability (≥30°) ( A vs. NA HU 3.3 , 11 vs. 13 (lb), and 101 vs. 133 [%]). However, this subgroup contained only two thumbs, so conclusion is limited. The relatively small case number in the other subgroups could also explain the lack of statistical significance in this comparison ( Table 5 ).
Table 5. Results of the comparison of the arthrodesis group (A) to the NA HU subgroups.
| Mean (min–max) value |
A (
n
= 14)
arthrodesis |
NA (
n
= 55)
nonarthrodesis subdivided according to MCP hyperextension |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NA H 1 hyperextension ≤ 10° + ulnar instability |
NA H 2 hyperextension 11–39° + ulnar instability |
NA H 3 hyperextension ≥ 40° + ulnar instability |
||||||||
| NA HU 1.1 ≤ 10° |
NA HU 1.2 11–29° |
NA HU 1.3 ≥ 30° |
NA HU 2.1 ≤ 10° |
NA HU 2.2 11–29° |
NA HU 2.3 ≥ 30° |
NA HU 3.1 ≤ 10° |
NA HU 3.2 11–29° |
NA HU 3.3 ≥ 30° |
||
| n (thumbs) | 14 | 4 | 8 | 7 | 6 | 9 | 8 | 2 | 8 | 3 |
| Grip (lb) | 39 (20–80) | 45 (40–60) | 53 (35–110) | 44 (5–110) | 38 (30–50) | 34 (20–50) | 36 (10–100) | 50 (40–60) | 43 (30–60) | 43 (30–60) |
| Grip (% of opposite side) | 99 (50–200) | 92 (66–100) | 118 (100–200) | 88 (50–100) | 110 (75–150) | 100 (100–100) | 100 (75–125) | 100 (100–100) | 95 (66–118) | 117 (100–100) |
| Pinch (lb) | 11 (10–20) | 11 (10–15) | 13 (10–20) | 8 (0–20) | 12 (10–15) | 12 (10–15) | 11 (5–25) | 13 (10–15) | 11 (10–15) | 13 (10–20) |
| Pinch (% of opposite side) | 101 (67–200) | 104 (66–150) | 109 (75–200) | 67 (50–100) | 100 (100–100) | 100 (100–100) | 81 (50–100) | 100 (50–100) | 88 (50–114) | 133 (100–200) |
In our data, despite the lack of statistical difference, not the hyperextension, but the ulnar instability seemed to play a role. Therefore, we compared subgroups of varying extent of ulnar instability ( NA U 1–3 ).
As before, comparable grip strength values were obtained. However, higher pinch strength could be measured in the group with additional arthrodesis, compared with the two subgroups of thumbs with moderate ( A vs. NA U 2 [>10– < 30°], 101 [67–200] vs. 99 [50–200;%], p -value 0,7445) or pronounced ulnar instability ( A vs. NA U 3 [≥30°], 11 [10–20] vs. 10 [0–25; lb], and 101 [67–200] vs. 82 [0–200];%]), which received only LRTI arthroplasty. There were no differences in terms of VAS, satisfaction, and functional scores (Quick-DASH and PRWE-Thumb). Once more, group A with arthrodesis showed a lower Kapandji's score in comparison to all three subgroups. No differences in proximalization were seen ( Table 6 ).
Table 6. Results of the comparison of the arthrodesis group (A) to the NA U subgroups.
| Mean (min–max) value |
A (
n
= 14)
arthrodesis |
NA (
n
= 55)
nonarthrodesis subdivided according to ulnar instability |
||
|---|---|---|---|---|
| NA U 1 ≤ 10° |
NA U 2 11–29° |
NA U 3 ≥ 30° |
||
| n (thumbs) | 14 | 12 | 25 | 18 |
| Grip (lb) | 39 (20–80) | 43 (30–60) | 43 (20–110) | 40 (5–110) |
| Grip (% of opposite side) | 99 (50–133) | 102 (67–150) | 104 (67–200) | 100 (50–150) |
| Pinch (lb) | 11 (10–20) | 12 (10–15) | 12 (5–20) | 10 (0–25) |
| Pinch (% of opposite side) | 101 (67–200) | 101 (67–150) |
99
(50–200) s*
( p -value 0.0744) |
82 (0–200) |
| VAS at rest (0–10) | 1 (0–3) | 1 (0–3) | 1 (0–4) | 1 (0–2) |
| VAS at stress (0–10) | 3 (0–7) | 2 (0–6) | 2 (0–6) | 2 (0–6) |
| Quick-DASH (0–100) | 31 (0–64) | 19 (0–68) | 24 (0–61) | 24 (0–57) |
| PRWE-Thumb (0–100) | 27 (0–50) | 16 (0–67) | 23 (0–73) | 17 (0–59) |
| Satisfaction (1–6) | 2 (1–5) | 2 (1–6) | 2 (1–3) | 2 (1–4) |
| Do surgery again (y:n) | 12:2 | 11:1 | 25:0 | 17:1 |
| Kapandji's Score (1–10) | 7 (4–10) |
9
(8–10) s***
( p -value 0.0039) |
9
(8–10) s***
( p -value 0.0002) |
9
(6–10) s**
( p -value 0.0417) |
| Proximalization X-ray (mm) | 2 (0–4) | 2 (0–5) | 2 (0–3) | 2 (0–4) |
Abbreviations: PRWE-Thumb, Patient-Rated Wrist Evaluation, modified for evaluation of function of the thumb; Quick-DASH, The Disabilities of the Arm, Shoulder, and Hand Score; VAS, Visual Analogue Scale.
In the arthrodesis group (A), one patient presented with distinct adhesions, which did not improve much after revision and removal of the plate. In one case, arthrodesis was performed in the 0 degrees position, which does not correspond to the fixation angle of 10–15 degrees, we normally aim for. This did not give a good functional result due to impaired opposition.
Removal of arthrodesis hardware was executed in 6 of 14 thumbs. In group NA, there was one case of complex regional pain syndrome (CRPS). One patient with persistent complaints after LRTI arthroplasty, presented with pronounced ossification in the area of resected trapezium, which was progressive. The patient did not ask for revision until now. Two patients in each group (A and NA) presented with dysesthesia in the area of the superficial branch of the radial nerve, in two cases persisting after revision.
Conclusions
Hypothesis one that patients with thumb CMCj osteoarthritis and pronounced hyperextension (≥40°) in the MCPj would benefit from arthrodesis in LRTI arthroplasty could not be proven.
However, hypothesis two that arthrodesis could have an advantage in cases with (additional) ulnar instability (≥30°), and therefore could have a positive influence on the pinching force, was confirmed. The benefit seems to be unrelated to the amount of hyperextension.
Hypothesis three, if this is true, which grade of concomitant ulnar instability/hyperextension in the MCPj should be addressed?
Our results suggest that ulnar instability of the MCPj seems to be more important, especially in the group with low hyperextension. In thumbs with moderate ulnar instability, a significant lower mean in comparison of pinch strength could be observed, but with severe ulnar instability, despite the lack of statistical significance, the lowest mean of pinch strength was measured. Therefore, we recommend arthrodesis in cases with ulnar instability of more than 30 degrees.
Discussion
Based on our data, it has been confirmed that for patients with thumb CMCj osteoarthritis, who show ulnar collateral instability in the MCPj (>30°) in addition to or without hyperextension arthrodesis has a beneficial effect on pinch strength, if done in combination with LRTI arthroplasty.
One possible explanation is that in powerful pinch grip hyperextension is more easily compensated than ulnar instability. Therefore, even pronounced hyperextension does not matter so much.
These findings regarding hyperextension in the MCPj meet with those Brogan et al published recently. 9 In 2017, they evaluated the outcome of LRTI arthroplasty and included patients with either mild (<30°) or no preoperative hyperextension in the MCPj. There were no statistically significant differences between those two groups in improvement of function of the CMCj after surgery. They concluded not to treat mild hyperextension in the MCPj. This study is not entirely comparable to our results, because ulnar instability was not evaluated, only mild cases of hyperextension in the MCPj were included and patients did not receive any treatment of the MCPj.
Poulter and Davis examined the outcome of three different procedures for the hyperextended MCPj done together with LRTI arthroplasty of the CMCj. 10 They found, if hyperextension in the MCP less than 30 degrees is left untreated, clinical outcome after surgery is not affected. Moreover, they discovered no difference in strength and function with correction of the MCPj at hyperextension of more than 30 degrees, but they drew no conclusion due to the small number of patients.
The small number of cases, especially after subdivision of groups is also a limitation in our investigation, as well as the lack of complete preoperative evaluation. CMCj osteoarthritis is a very common diagnosis, as well as trigger finger, carpal tunnel, polyarthrosis, and others—all these coexisting diseases could also influence the results.
In our view, a direct comparison to other techniques for stabilization of ulnar instability, for instance ligamentoplasty or anchor fixation, 11 is not applicable: ulnar instability in thumb CMCj osteoarthritis is not an acute, traumatic lesion but a chronic instability and probably due to overuse in protecting CMCj or resulting from pathomechanisms of associated comorbidities in thumb CMCj osteoarthritis. It is not an isolated (traumatic) ulnar instability, rather an ulnar instability which occurs in addition to hyperextension instability.
Ulnar instability in the MCPj should be included in the classification of the thumb CMCj osteoarthritis stages. Thus, comparability of treatment and follow-up could be improved. But there certainly is need for further studies. At least it should be considered in treatment options.
Our indication for surgery has changed: we no longer see hyperextension, but ulnar instability as the primary indication for discussing the option of (simultaneous) arthrodesis of the MCPj in LRTI arthroplasty.
However, some factors are still unclear and remain an individual decision with the patient. If there is painful instability of MCPj or osteoarthritis in the MCPj, the decision for arthrodesis is certainly easier. But we should keep in mind, that there often is a discrepancy between a bland radiological finding and already marked cartilage changes in the intraoperative setting. And if a joint is severely unstable over several years, there is at least a great potential to develop osteoarthritis.
Since thumb CMCj osteoarthritis often affects patients in professional life, one factor is certainly how often a patient can afford absence from work. Provided there is an indication, it may thus be advantageous to carry out the arthrodesis in the MCPj simultaneous to resection arthroplasty.
The extent of preoperative ROM in the MCPj is also of great importance in the decision-making process. If the ROM in flexion of the MCPj is low, the functional result of arthrodesis is better, because the patient only loses “unfunctional ROM” due to instability in hyperextension and/or ulnar deviation. In asymptomatic individuals, the first MCPj is well known for its high individuality in ROM.
All these factors must be discussed with the patient. It is very important for the patient to understand the effect of arthrodesis on his daily activities. The advantage of potentially better strength and sturdier grip despite less mobility can be simulated by using an orthosis preoperatively.
Acknowledgments
The authors would like to thank Gaby Fromberg for providing feedback and language editing of the manuscript and the whole team of the practice.
Conflict of Interest None declared.
Note
The work was performed at the Practice for Plastic and Hand Surgery, Murnau, Germany.
References
- 1.Lourie G M. The role and implementation of metacarpophalangeal joint fusion and capsulodesis: indications and treatment alternatives. Hand Clin. 2001;17(02):255–260. [PubMed] [Google Scholar]
- 2.Wajon A, Vinycomb T, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2015;(02):CD004631. doi: 10.1002/14651858.CD004631.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burton R I, Pellegrini V D., Jr Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11(03):324–332. doi: 10.1016/s0363-5023(86)80137-x. [DOI] [PubMed] [Google Scholar]
- 4.Eaton R G, Floyd W E., III Thumb metacarpophalangeal capsulodesis: an adjunct procedure to basal joint arthroplasty for collapse deformity of the first ray. J Hand Surg Am. 1988;13(03):449–453. doi: 10.1016/s0363-5023(88)80029-7. [DOI] [PubMed] [Google Scholar]
- 5.Armbruster E J, Tan V.Carpometacarpal joint disease: addressing the metacarpophalangeal joint deformity Hand Clin 20082403295–299., vii [DOI] [PubMed] [Google Scholar]
- 6.Tomaino M, King J, Leit M. Philadelphia: Elsevier; 2005. Thumb basal joint arthritis; pp. 461–485. [Google Scholar]
- 7.De Smet L, Vandenberghe L, Didden K, Degreef I. Outcome of simultaneous surgical treatment of hyperextension of metacarpophalangeal and basal joint osteoarthritis of the thumb. Acta Orthop Belg. 2013;79(05):514–516. [PubMed] [Google Scholar]
- 8.Brogan D M, Kakar S. Metacarpophalangeal joint hyperextension and the treatment of thumb basilar joint arthritis. J Hand Surg Am. 2012;37(04):837–838. doi: 10.1016/j.jhsa.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Brogan D M, van Hogezand R M, Babovic N, Carlsen B, Kakar S. The effect of metacarpophalangeal joint hyperextension on outcomes in the surgical treatment of carpometacarpal joint arthritis. J Wrist Surg. 2017;6(03):188–193. doi: 10.1055/s-0036-1597836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poulter R J, Davis T RC. Management of hyperextension of the metacarpophalangeal joint in association with trapeziometacarpal joint osteoarthritis. J Hand Surg Eur Vol. 2011;36(04):280–284. doi: 10.1177/1753193411400359. [DOI] [PubMed] [Google Scholar]
- 11.Patel S, Potty A, Taylor E J, Sorene E D. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm. Strateg Trauma Limb Reconstr. 2010;5(01):1–10. doi: 10.1007/s11751-010-0079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


