Abstract
Collaboration between emergency medical services (EMS) and hospitals receiving stroke patients is critical to ensure prompt, effective treatment, and is a key component of the stroke systems of care (SSoC). The goal of our study was to evaluate the association between presentation by EMS and EMS prenotification with odds of receiving Tissue-type Plasminogen Activator (IV-tPA) in a state implementing SSoC while rigorously accounting for missing data. We utilized data from the Massachusetts Paul Coverdell Stroke Registry for this study, and analyzed adult patients presenting with ischemic stroke to Massachusetts Coverdell hospitals between 2016 and 2018. Patients with contraindications to IV-tPA were excluded. We used generalized estimating equations to assess associations between presentation by EMS, EMS prenotification, and receipt of IV-tPA. We also performed a sensitivity analysis using multiple imputation to assess the sensitivity of our findings to missing data. We identified 9,230 eligible patients with ischemic stroke during the study period. In multivariate complete case regressions, presentation by EMS and EMS prenotification were associated with statistically significant increased odds of receiving IV-tPA (odds ratio [OR] 1.52, 95% confidence interval [CI] 1.28–1.80, p-value<0.01; OR 1.75, 95% CI 1.36–2.24, p-value<0.01, respectively). Analysis of imputed data indicated level or stronger associations. Our analysis indicates that presentation by EMS and EMS prenotification are associated with increased odds of receiving IV-tPA in a state implementing the SSoC. Our results lend importance to the critical role of EMS in the SSoC. Future interventions should work to increase rates of prenotification by EMS and assess inequities in receipt of IV-tPA.
Keywords: emergency medical services, stroke, delivery of health care
Introduction
Prompt evaluation and treatment are critical for improving outcomes among patients experiencing a stroke. Tissue-type Plasminogen Activator (IV-tPA) is an effective treatment for patients with ischemic stroke, which must be administered within a narrow time window(1,2). However, studies suggest that not all eligible patients receive IV-tPA(3–5). Time between symptom onset to emergency department triage is a major source of delay and cause of ineligibility for IV-tPA and other reperfusion therapies(6,7).
Recognizing that the fragmentation of the United States healthcare system presents an obstacle to prompt and effective treatment, the American Stroke Association (ASA) outlined a systems approach to stroke treatment, referred to as Stroke Systems of Care (SSoC)(8). The Massachusetts Paul Coverdell National Acute Stroke Program, funded by the Centers for Disease Control and Prevention since 2004, began implementing the SSoC model in 2015 with Massachusetts hospitals participating in the program. All Massachusetts Coverdell hospitals have Primary Stroke Service (PSS) designation, which indicates that hospitals meet regulatory requirements and therefore can provide care for stroke patients.
Two critical components of the SSoC are emergency medical services (EMS) collaboration with hospitals receiving stroke patients and the implementation of protocols that standardize EMS prenotification of the destination hospital that a suspected stroke patient is in transport. Massachusetts PSS designation as well as statewide protocols require EMS personnel to communicate with hospitals during transport of patients with suspected stroke to permit the emergency department to efficiently prepare for the patient’s arrival(9). To further improve these systems, Massachusetts Coverdell hospitals are expected to establish formal partnerships with EMS agencies to enhance EMS communication and collaboration. Further, participating EMS agencies work with receiving hospitals to strengthen and consistently implement prenotification protocols. These protocols include standing orders, checklists outlining stroke prenotification criteria, and standardized clinical procedures for suspected stroke patients.
Previous studies indicate the role of EMS in prompt, appropriate stroke care. A previous study of stroke patients demonstrate an association between EMS transport and prenotification with more timely brain imaging and interpretation(10). In addition, previous studies indicate increased administration of IV-tPA among patients with EMS prenotification(11,12). However, to the best of our knowledge, no studies have assessed these associations within a state implementing the SSoC, which may impact the relationship between mode of presentation, prenotification, and IV-tPA. Further, several of these studies did not assess the impact of missing data on these conclusions or could not control for stroke severity or other key variables due to missingness.
To elucidate the relationship between presentation by EMS and IV-tPA, we conducted an analysis using 2016 to 2018 Massachusetts Stroke Registry data. We assessed whether presentation by EMS and EMS prenotification are associated with IV-tPA administration among a large population of ischemic stroke patients treated at Massachusetts Coverdell hospitals implementing the SSoC model. We also conducted a multiple imputation analysis to account for missing data.
Methods
Data Sources and Population
We analyzed data from the Massachusetts Paul Coverdell Stroke Registry, which contains detailed clinical, demographic, and quality of care data on stroke patients admitted to the 50 of the 68 Massachusetts PSS hospitals participating in the Coverdell program. This analysis was approved by the MDPH institutional review board (protocol #373932).
We included all patients aged 18 years or older with a primary discharge diagnosis of ischemic stroke (ICD-10 I63*, I65*−6*) admitted to Coverdell hospitals between January 1, 2016 and December 31, 2018. We excluded patients with contraindications to IV-tPA (systolic blood pressure > 185 mm Hg or diastolic blood pressure > 110 mm Hg; recent intracranial, spinal, or head injury; prior stroke within past 3 months; history intracranial hemorrhage, neoplasm arteriovenous malformation, or aneurysm; active internal bleeding; any indication of hemorrhage on computed tomography scan; acute bleeding diathesis; multilobar infarction; arterial puncture at non-compressible site in previous 7 days; or blood glucose concentration < 50 mg/dL); patients who were comfort measures only on the day of or day after hospital admission; patients transferred from another hospital; patients with strokes occurring in acute care facilities or chronic healthcare facilities; patients not admitted; patients with resolved symptoms; and patients admitted solely for an elective carotid intervention.
We utilized 2014 Massachusetts Case Mix Hospitalization and Observation data to create a clustering variable of annual hospital stroke volume. Total case counts comprised all stroke types and included both hospital observations and admissions.
Analysis
After applying inclusion and exclusion criteria, we analyzed available population characteristics, including age, sex, race, ethnicity, and insurance type. We also assessed the proportion of patients presenting by EMS and of these how many had EMS prenotification. Finally, we assessed the proportion of patients who had documented pre-hospital and in-hospital delays, indicating delays in hospital presentation, stroke diagnosis, or other related factors which contributed to not administering IV-tPA.
Our primary outcome of interest was IV-tPA administration, treated dichotomously. Independent variables of interest were presentation by EMS and EMS prenotification. Patient arrival mode was coded as private transportation or EMS. EMS prenotification was coded as yes or no. We used generalized estimating equations (GEE) to assess associations. We ran two bivariate models-a mode of arrival regression among all patients meeting inclusion and exclusion criteria; and an EMS prenotification regression only among patients who presented by EMS.
We then repeated these regressions controlling for key covariates, including patient sex, age (18–44, 45–54, 55–64, 65+ years), race (Hispanic, white non-Hispanic, black non-Hispanic, Asian non-Hispanic, other non-Hispanic), insurance (Medicare, Medicaid, private, no insurance), calendar year of admission, National Institutes of Health Stroke Scale (NIHSS) at admission, hours between last known well and emergency department (ED) triage, and hours between ED triage and computed tomography (CT) scan. Documentation of pre-hospital or in-hospital delay was controlled for in the model. Hospital annual stroke volume was included as a clustering variable according to the following categorizations: small 1–100 cases; medium 101–200 cases; large 201–350 cases; and extra-large 351 cases or more. We analyzed the data using SAS 9.3(13).
Sensitivity Analysis
To assess the degree of missing data in our analysis, we analyzed each covariate included in the models for missingness and identified variables that were missing in greater than 5% of cases. We then used predictive mean matching to impute these variables 10 times in the full patient cohort using PROC MI in SAS and repeated the GEE analysis. We pooled the results using PROC MIANALYZE and compared to results of complete case analysis. To ensure the assumptions of the imputation models did not impact our main findings, we ran several imputation models by varying covariates and repeated the GEE models.
Results
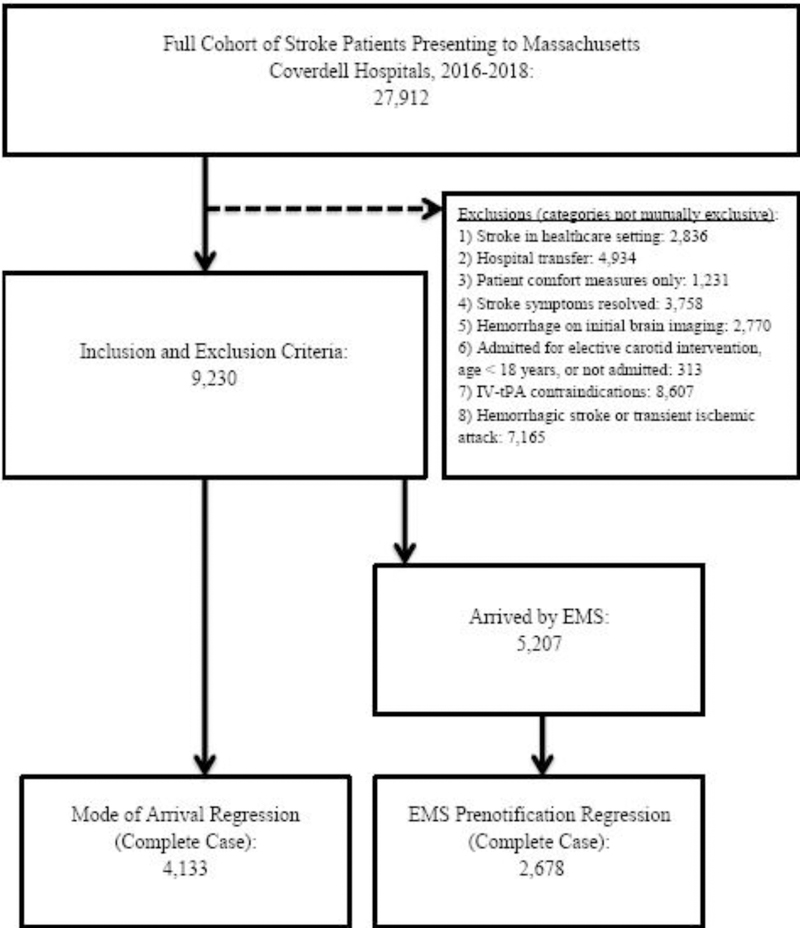
During the study period, 27,912 stroke patients were admitted to the Coverdell hospitals. After applying inclusion and exclusion criteria, 9,230 patients were eligible for our analysis, of whom 5,207 (56.4%) presented by EMS. See Figure 1 for consort flow diagram.
Figure 1.
Consort Flow Diagram
The full demographics of the patient population are summarized in Table 1. The overall population had the following characteristics: 49.3% (4,556) were female; 76.3% (7,046) were white, non-Hispanic; 50.5% (4,664) had private insurance; and 70.2% (6,483) were aged 65 or more years. Among patients arriving by EMS, 44.6% (2,324) had EMS prenotification. Of the 9,230 patients in our study, 11.6% (1,076) received IV-tPA. In restricting our analysis to patients arriving within 4.5 hours of last known well, the percent of patients receiving IV-tPA was 73.4% (1,059 of 1,442 patients).
Table 1.
Demographics of Ischemic Stroke Patients Meeting Inclusion and Exclusion Criteria Admitted to Coverdell Hospitals, 2016–2018.
| Characteristic | Total Population (n=9,230) |
Presented by EMS (n=5,207) |
Did not Present by EMS (n=3,858) |
|---|---|---|---|
| Age Group | |||
| 18–44 Years | 3.3% (309) | 2.4% (125) | 4.5% (175) |
| 45–54 Years | 8.8% (817) | 6.4% (338) | 12.1% (467) |
| 55–64 Years | 17.5% (1,621) | 14.3% (749) | 22.1% (854) |
| 65+ Years | 70.2% (6,483) | 76.7% (3,995) | 61.2% (2,362) |
| Sex (Female) | 49.3% (4,556) | 52.2% (2,723) | 44.9% (1,734) |
| Insurance | |||
| Medicare | 27.1% (2,502) | 30.0% (1,567) | 23.9% (924) |
| Medicaid | 15.8% (1,467) | 15.4% (805) | 16.9% (654) |
| Private | 50.5% (4,664) | 49.7% (2,591) | 52.8% (2,040) |
| No Insurance | 5.1% (477) | 4.4% (232) | 6.1% (238) |
| Race and Ethnicity | |||
| White, non-Hispanic | 76.3% (7,046) | 78.9% (4,109) | 72.8% (2,812) |
| Black, non-Hispanic | 10.4% (967) | 9.5% (496) | 11.8% (456) |
| Asian, non-Hispanic | 4.5% (415) | 3.6% (191) | 5.5% (215) |
| Other, non-Hispanic | 3.8% (352) | 3.7% (193) | 3.9% (151) |
| Hispanic | 4.8% (450) | 4.1% (218) | 5.8% (224) |
| Received IV-tPA | 11.6% (1,076) | 16.7% (873) | 5.0% (193) |
| EMS Prenotification | 25.1% (2,324) | 44.6% (2,324) | - |
| Delay in Care | 43.0% (3,974) | 41.1% (2,141) | 46.9% (1,812) |
Counts and percentages may not sum due to missing data or rounding.
IV-tPA = intravenous tissue-type plasminogen activator; EMS = emergency medical services.
The bivariate arrival mode regression and EMS prenotification regression demonstrated a significant association with IV-tPA (odds ratio (OR) 3.82, 95% confidence interval [CI] 3.44–4.24, p-value<0.01; OR 3.39, 95% CI 2.93–3.92, p-value<0.01, respectively). In complete case regressions accounting for covariates, these associations remained significant (OR 1.52, 95% CI 1.28–1.80, p-value<0.01; OR 1.75, 95% CI 1.36–2.24, p-value<0.01, respectively). Further, in both regressions, patients aged 65 or more years were less likely to receive IV-tPA, while Asian, non-Hispanic and Hispanic patients were more likely to receive IV-tPA. Finally, female patients and patients on Medicaid were less likely to receive IV-tPA in the arrival mode regression. See Tables 2 and 3 for complete model information.
Table 2.
Factors associated with IV-tPA receipt among all patients in multivariate model (n=4,133).
| Covariate | Estimate (95% Confidence Interval) |
p-value |
|---|---|---|
| Arrival by EMS | 1.52 (1.28,1.80) |
<0.01 |
| National Institutes of Health Stroke Scale | 1.08 (1.04,1.11) |
<0.01 |
| Calendar Year of Admission | 1.00 (0.72,1.41) |
<0.95 |
| Last Known Well to ED Arrival | 0.23 (0.18,0.30) |
|
| ED Arrival to CT Imaging | 0.65 (0.54,0.78) |
<0.01 |
| Health Insurance (reference=Private) | ||
| Medicare | 1.07 (0.57,1.98) |
<0.82 |
| Medicaid | 0.49 (0.34,0.70) |
<0.01 |
| No Insurance | 0.75 (0.47,1.20) |
<0.23 |
| Age Group (reference=18–44 Years) |
||
| 45–54 Years | V (0.85,1,85) | <0.24 |
| 55–64 Years | 103 (0.94,1.13) |
<0.47 |
| 65+ Years | 0.49 (0.42,0.58) |
<0.01 |
| Race/ Ethnicity (reference=White, Non-Hispanic) |
||
| Black, Non-Hispanic | 1.15 (0.83,1,60) |
<0.37 |
| Asian, Non-Hispanic | 1.60 (1.16,2.21) |
<0.01 |
| Hispanic | 2.87 (1.84,4.47) |
<0.01 |
| Other, Non-Hispanic | 1.20 (0.97,1.48) |
<0.08 |
| Sex (Female) | 0.69 (0.57,0.84) |
<0.01 |
| Pre or In-Hospital Delay | 0.15 (0.10,0.22) |
<0.01 |
EMS = emergency medical services; ED = emergency department; CT = computed tomography.
Table 3.
Factors associated with IV-tPA receipt among patients arriving by EMS in multivariate model (n=2,678).
| Covariate | Estimate (95% Confidence Interval) |
p-value |
|---|---|---|
| EMS Prenotification | 1.75 (1.36,2.24) |
<0.01 |
| National Institutes of Health Stroke Scale | 1.07 (1.02,1.11) |
<0.01 |
| Calendar Year of Admission | 1.06 (0.84,1.33) |
<0.61 |
| Last Known Well to ED Arrival | 0.24 (0.18,0.34) |
<0.01 |
| ED Arrival to CT Imaging | 0.75 (0.65,0.86) |
<0.01 |
| Health Insurance (ref=Private) | ||
| Medicare | 1.07 (0.56,2.05) |
<0.82 |
| Medicaid | 0.60 (0.32,1.12) |
<0.11 |
| No Insurance | 0.96 (0.51,1.82) |
<0.91 |
| Age Group (ref=18–44 Years) | ||
| 45–54 Years | 0.84 (0.52,1.36) |
<0.49 |
| 55–64 Years | 0.60 (0.45,0.78) |
<0.01 |
| 65+ Years | 0.30 (0.25,0.36) |
<0.01 |
| Race/ Ethnicity (ref=White, Non-Hispanic) | ||
| Black, Non-Hispanic | 1.06 (0.71,1.61) |
<0.74 |
| Asian, Non-Hispanic | 1.79 (1.36,2.37) |
<0.01 |
| Hispanic | 2.02 (1.51,2.71) |
<0.01 |
| Other, Non-Hispanic | 1.36 (0.96,1.92) |
<0.08 |
| Sex (Female) | 0.78 (0.59,1.03) |
<0.08 |
| Pre or In-Hospital Delay | 0.16 (0.11,0.24) |
<0.01 |
EMS = emergency medical services; ED = emergency department; CT = computed tomography.
Sensitivity Analysis
In complete case regressions accounting for covariates, there was a significant loss of observations due to missing values: 4,133 of 9,230 eligible patients were analyzed in the complete case arrival mode regression and 2,678 of 5,207 eligible patients were analyzed in the complete case EMS prenotification regression. Variables missing in greater than 5% of cases in the eligible patient cohort include NIHSS (16.1%), last known well to ED triage (50.2%), and ED triage to CT imaging (5.3%).
To assess whether missing data impacted our results, NIHSS, last known well to ED triage, and ED triage to CT imaging were imputed 10 times using several different imputation models, the multivariate regressions repeated, and the results pooled. Compared to complete case regressions, the associations between arrival by EMS and EMS prenotification with IV-tPA were approximately level or strengthened, regardless of the imputation model used. Further, many of the covariates in both regressions maintained statistical significance and directionality of association, although there were some exceptions (see supplement for select regression results).
Discussion
In our analysis of data from a statewide stroke quality improvement registry, we found increased odds of receiving IV-tPA among patients presenting by EMS and with EMS prenotification in a state implementing the SSoC, a conclusion that was confirmed after accounting for missing data. Our results reinforce the critical role of EMS in the SSoC.
Our results extend previous findings to an SSoC setting. A 2011 North Carolina stroke registry study found that EMS transport and prenotification was associated with reduced delays in brain imaging and interpretation, and increased administration of IV-tPA, while a study conducted in 2011 of patients arriving by EMS found prenotification to be associated with shorter door to imaging time, shorter door to needle time, and higher rates of IV-tPA(10,12). However, these studies either could not control for stroke severity or excluded large numbers of patients with missing data. Using multiple imputation, were able to replicate these findings while accounting for past methodological limitations. Finally, a small study of stroke patients admitted to a Massachusetts hospital between 2004 and 2005 found EMS prenotification was associated with reduced door to CT time and increased thrombolysis(11). Our study confirms these associations in a large population of stroke patients. The association between EMS transport and prenotification with increased administration of IV-tPA may be engendered by faster transport, documentation of stroke onset (a key factor in determining eligibility for IV-tPA and other reperfusion therapies), and enabling mobilization of hospital care teams for timely intervention(8,10–12,14).
Our observed rate of prenotification (44.6% among patients presenting by EMS) was low, although a previous nationwide study noted significant variation in rates of prenotification as well as low rates in Massachusetts(15). There are several potential causes of this. First, although prenotification is required by statewide protocol when a stroke is suspected, there is likely great variation among the over 300 licensed EMS agencies operating in Massachusetts. Second, it is possible that EMS agencies do not recognize less severe strokes. Indeed, analysis of NIH stroke scale at admission indicates that among patients arriving by EMS, those with prenotification had a slightly higher NIHSS than those without prenotification (7.9, 95% CI 7.6–8.2; 5.5, 95% CI 5.2–5.7, respectively). These findings present an opportunity to increase rates of prenotification by providing additional education on stroke signs and symptoms to EMS agencies, especially milder strokes. Finally, there is potential data entry error by data abstractors when completing the prenotification variable in the Coverdell stroke registry. Although annual audits of select cases from the Coverdell stroke registry in 2016, 2017, and 2018 suggest low error rates in this variable, these audits compare registry data to the hospital medical record. Thus, it is still possible that the hospital incorrectly documented in the patient’s medical record whether EMS prenotification actually occurred.
The association between EMS prenotification and receipt of IV-tPA underscores the critical nature of a strong SSoC. To this end, the Massachusetts Coverdell program encourages formal partnerships between participating hospitals and EMS agencies, and engages with participating entities to enhance key processes, such as provision of feedback from hospital to EMS, improved data sharing procedures, and establishing standardized protocols for identifying and treating stroke patients. Further, participating hospitals and EMS agencies attend joint learning sessions that provide education on SSoC implementation. Recruitment of EMS agencies in the Massachusetts Coverdell program is ongoing, and as of 2019 includes 34 EMS agencies. The results of this analysis signify the importance of continuing this work.
Multivariate regressions suggests that female patients, patients aged 65 years or more, and patients on Medicaid were significantly less likely to receive IV-tPA, while Hispanic and Asian, non-Hispanic patients were more likely to receive IV-tPA. However, in regressions of multiply imputated data, some associations changed directionality or significance, suggesting that these results are sensitive to missing data. The literature on whether certain subgroups are more or less likely to receive IV-tPA is mixed, with some studies noting variations by race, ethnicity, age, and sex, while others finding no variation(4,5,16). The National Academies of Science report, Crossing the Quality Chasm: A New Health System for the 21st Century, calls for equity in healthcare, however the literature suggests that inequities in access, treatment, and outcomes remain pervasive(17–19). The variations observed here should be explored in future analyses.
This study has important limitations to note. This analysis utilized data from hospitals participating in the Massachusetts Coverdell program and may not be generalizable to hospitals not participating in the Coverdell program or to hospitals in other states. Our analysis of EMS prenotification was limited to yes or no, and we could not complete a more detailed analysis of quality of information transmitted to hospitals. Such an analysis is a critical next step in assessing and improving quality of EMS stroke care. In addition, registries are subject to bias and data entry error by abstractors. Finally, there were significant amounts of data missing on key variables, which raises concerns about validity of complete case analysis. However, sensitivity analyses did not suggest bias in the primary findings.
This study indicates a significant association between presentation by EMS and EMS prenotification with odds of receiving IV-tPA among ischemic stroke patients in a state implementing the SSoC. Our findings lend importance to strong EMS integration in the SSoC, continued public education on stroke symptom recognition and utilization of EMS, and continued engagement with EMS agencies regarding importance of prenotification from the field. These efforts will be important to continue to improve rates of IV-tPA delivery among acute ischemic stroke patients.
Supplementary Material
Acknowledgements
We thank hospitals and emergency medical service agencies participating in the Coverdell program. We thank Nora McElroy, MPH for providing information on Primary Stroke Service hospitals in Massachusetts.
Sources of Funding
This work was funded by the Centers for Disease Control and Prevention (CDC) under the Paul Coverdell National Acute Stroke Prevention Program (NU58DP006072).
Footnotes
Disclosure of Interest
The authors report no conflict of interest.
References
- 1.Marler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, Broderick JP, Levine SR, Frankel MP, Horowitz SH, Haley ECJ, Lewandowski CA, Kwiatkowski TPMarler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, Broderick JP, Levine SR, Frankel MP, Horowitz SH, Haley ECJ, Lewandowski CA, Kwiatkowski TP. Early stroke treatment associated with better outcome: The NINDS rt-PA Stroke Study. Neurology. 2012;55(11): 1649–55. [DOI] [PubMed] [Google Scholar]
- 2.Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EFMAdams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EFM. Guidelines for the Early Management of Adults With Ischemic Stroke: A Guideline From the American Heart Association/ American Stroke Association Stroke Council. Circulation. 2007;115:e478–534. [DOI] [PubMed] [Google Scholar]
- 3.Messé SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, Grau-Sepulveda MV, Cox M, Peterson ED, Fonarow GC, Schwamm LHMessé SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, Grau-Sepulveda MV.,Cox M, Peterson ED, Fonarow GC, Schwamm LH. Why are acute ischemic stroke patients not receiving IV tPA? Neurology. 2016;87(15): 1565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reed SD, Cramer SC, Blough DK, Meyer K, Jarvik JGReed SD, Cramer SC, Blough DK, Meyer K, Jarvik JG. Treatment With Tissue Plasminogen Activator and Inpatient Mortality Rates for Patients With Ischemic Stroke Treated in Community Hospitals. Stroke. 2001;32:1832–40. [DOI] [PubMed] [Google Scholar]
- 5.Katzan IL, Hammer MD, Hixson ED, Furlan AJ, Abou-Chebl A, Nadzam DMKatzan IL, Hammer MD, Hixson ED, Furlan AJ, Abou-Chebl A, Nadzam DM. Utilization of Intravenous Tissue Plasminogen Activator for Acute Ischemic Stroke. Arch Neurol. 2004;61(3):346. [DOI] [PubMed] [Google Scholar]
- 6.Morris D, Rosamond W, Madden K, Schultz C, Hamilton SMorris D, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke. 2000;31(11):2585–90. [DOI] [PubMed] [Google Scholar]
- 7.Prehospital and hospital delays after stroke onset--United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2007;56(19):474–8. [PubMed] [Google Scholar]
- 8.Schwamm LH, Pancioli A, Acker JE, Goldstein LB, Zorowitz RD, Shephard TJ, Moyer P, Gorman M, Johnston SC, Duncan PW, Gorelick P, Frank J, Stranne SK, Smith R, Federspiel W, Horton KB, Magnis E, Adams RJSchwamm LH, Pancioli A, Acker JE, Goldstein LB, Zorowitz RD, Shephard TJ, Moyer P, Gorman M, Johnston SC, Duncan PW, Gorelick P, Frank J, Stranne SK, Smith R, Federspiel W, Horton KB, Magnis E, Adams RJ. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Circulation. 2005;111(8): 1078–91 [DOI] [PubMed] [Google Scholar]
- 9.Massachusetts Department of Public Health Massachusetts Department of Public Health. Primary Stroke Services guidelines and information [Internet]. 2019. [cited 2019 Aug 8]. Available from: https://www.mass.gov/info-details/primary-stroke-services-guidelines-and-information
- 10.Patel MD, Rose KM, Obrien EC, Rosamond WDPatel MD, Rose KM, Obrien EC, Rosamond WD. Prehospital notification by emergency medical services reduces delays in stroke evaluation: Findings from the North Carolina stroke care collaborative. Stroke. 2011;42(8):2263–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LHAbdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance Hospital Notification by EMS in Acute Stroke Is Associated with Shorter Door-to-Computed Tomography Time andlncreased Likelihood of Administration of Tissue-Plasminogen Activator. Prehospital Emerg Care. 2008;12(4):426–31. [DOI] [PubMed] [Google Scholar]
- 12.Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, Olson DM, Shah BR, Hernandez AF, Schwamm LH, Fonarow GCLin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, Olson DM, Shah BR, Hernandez AF, Schwamm LH, Fonarow GC. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5(4):514–22. [DOI] [PubMed] [Google Scholar]
- 13.SAS (Version 9.3). Cary, NC, USA: SAS Institute Inc.; 2010. [Google Scholar]
- 14.Kim SK, Lee SY, Bae HJ, Lee YS, Kim SY, Kang MJ, Cha JKKim SK, Lee SY, Bae HJ, Lee YS, Kim SY, Kang MJ, Cha JK. Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. Eur J Neurol. 2009; 16(12): 1331–5. [DOI] [PubMed] [Google Scholar]
- 15.Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, Olson DM, Shah BR, Hernandez AF, Schwamm LH, Fonarow GCLin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, Olson DM, Shah BR, Hernandez AF, Schwamm LH, Fonarow GC. Patterns, Predictors, Variations, and Temporal Trends in Emergency Medical Service Hospital Prenotification for Acute Ischemic Stroke. J Am Heart Assoc. 2012;1(111):e002345x-e002345x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hsia AW, Edwards DF, Morgenstern LB, Wing JJ, Brown NC, Coles R, Loftin S, Wein A, Koslosky SS, Fatima S, Sánchez BN, Fokar A, Gibbons MC, Jayam-Trouth A, Kidwell CSHsia AW, Edwards DF, Morgenstern LB, Wing JJ, Brown NC, Coles R, Loftin S, Wein A, Koslosky SS, Fatima S, Sánchez BN, Fokar A, Gibbons MC, Jayam-Trouth A, Kidwell CS. Racial disparities in tpa treatment rate for stroke: a population-based study. Stroke. 2011;42(8):2217–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corrigan J, Donaldson M, Kohn L, Maguire S, Pike KCorrigan J, Donaldson M, Kohn L, Maguire S, Pike K. Crossing the Quality Chasm A New Health System for the 21st Century. Washington DC: Institute of Medicine, National Academy of Sciences, National Academies Press; 2001. [Google Scholar]
- 18.Mayberry RM, Nicewander DA, Qin H, Ballard DJMayberry RM, Nicewander DA, Qin H, Ballard DJ. Improv ing quality and reducing inequities: a challenge in achieving best care. Proc (Bayl Univ Med Cent). 2006;19(2):103–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Department of Health US and Human Services Agency for Healthcare Research and Quality. National Quality and Disparities Report. Rockville, MD; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.