Editor,
Cutaneous leishmaniasis (CL) is an ulcerative skin parasitic disease common in people living in tropical regions and travelers1. Lesions characteristics (e.g., self-healing and treatment response) are extremely variable. Diagnosis can be challenging when the lesion is in an advanced stage and can be confused with other pathologies. On histology, epidermal and dermal abnormalities have been described2. Panniculitis has been reported as an important feature to distinguish CL from other dermatological lesions3. High-frequency ultrasound is a non-invasive imaging tool that depicts tissues with high definition4. We aim to describe the ultrasound morphology of confirmed cases of CL and correlation with the reported histopathological characteristics.
Nineteenth patients (≥ 18-year-old) with 20 cutaneous clinically and laboratory-confirmed leishmaniasis lesions underwent a high-frequency ultrasound examination with a 21 MHz probe before starting their treatment. The duration of the disease varied from 32 to 126 days (average of 67.4±28.6 days). From the 19 patients, 15 were males (78.9%), and four were females (21.1%) in the age range of 27 to 66 years (42.4 ± 13.7). The most frequently affected anatomical regions were: legs (30 %; n=6 /20), arms (25 %; n=5 / 20) and fingers (20 %; n=4 /20). All lesions presented involvement of the dermis and hypodermis ( mostly lobular or mostly septal panniculitis), and most of them reached the bone margin or the fascial plane (Figure 1). The whole group displayed subclinical ultrasonographic signs of panniculitis. Most of the lesions shared common features such as thickening, hypoechogenicity, and irregularity on dermis as well as thickening, hyperechogenicity, and slight heterogeneity of the hypodermis (Table 1). No signs of calcifications were detected within the lesional sites in all lesions.
Figure 1.
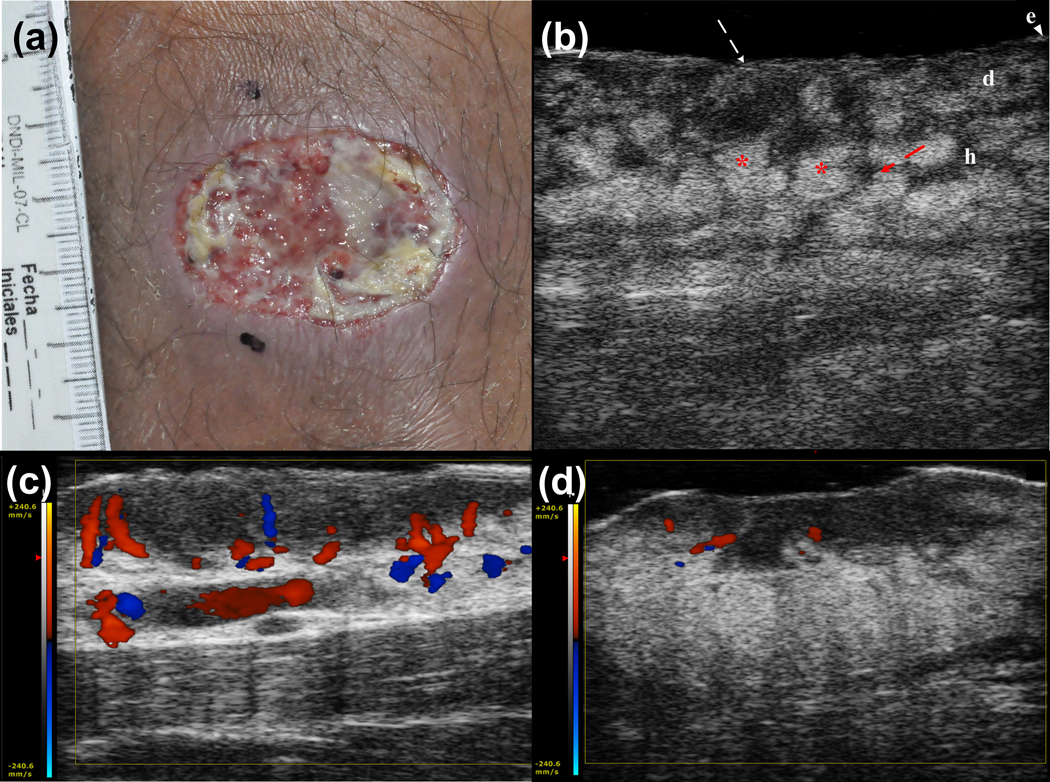
(a) Clinical photograph of a cutaneous leishmaniasis in a 50-year-old male with a lesion in the leg. (b) Greyscale ultrasound image (longitudinal view). Disruption of the epidermis (white arrow) and a mostly septal inflammatory involvement of the hypodermis (i.e., increased echogenicity of the fatty lobules (*) and thickening and decreased echogenicity of the septa (red arrow) are observed. Abbreviations: e epidermis, d dermis, h hypodermis. (c) Vascularity grading of cutaneous leishmaniasis (color Doppler) in the leg shows increased vascularity at the periphery of the lesion. (d) Color Doppler of a lesion in the dorsal aspect of the middle finger demonstrates slightly increased blood flow (poor) in the periphery of the lesion.
Table1.
Sonographic features of Cutaneous Leishmaniasis.
| Sonographic features | |
|---|---|
| Diameter [mm] | 9.5 ± 5.6 [1.96, 22.6] |
| Under skin thickness [mm] | 7.88 ± 3.25 [2.77, 14.63] |
| Depth ulcer [mm] | 0.65 ± 0.38 [0.2, 1.54] |
| Type of predominant involvement of the hypodermis | |
| Septal | 55% |
| Lobular | 45% |
| Echogenicity dermis | |
| Isoechoic | 5% |
| Hypoechoic | 90% [18 of 20] |
| Hyperechoic | 5% |
| Type of alteration of the dermis | |
| Irregular | 95% |
| Band-like | 5% |
| Echogenicity hypodermis | |
| Isoechoic | - |
| Hypoechoic | 10% |
| Hyperechoic | 90% |
To our knowledge, this is the first attempt to describe the ultrasound features of the cutaneous form of leishmaniasis. Currently, the clinical management of the disease is based on a supposedly only epidermal and dermal disruption. Nevertheless, the common presence of panniculitis may explain some of the difficulties for clinical management. Therapeutic alternatives are scarce, and the affection of deeper layers might contribute to the high rate of treatment failure, which potentially may require a change of the management. For example, topical treatments in these cases may not be indicated due to their low penetration and effectiveness in the deeper layers. Due to the increasing evidence and recommendation of topical therapies, ultrasound can also become a more objective way to evaluate the development and effect of new or current medications.
The abnormal hypodermis presented in all the lesions coincides with some histological studies which reported panniculitis signs in CL lesions as useful clues to distinguish them from other cutaneous lesions2,5,6. In that sense, ultrasonography could aid to understand the pathobiological and reparative processes that take place inside the cutaneous ulcer and neighboring layers. The common ultrasound features may serve as a starting point to perform the differential diagnosis with other dermatologic diseases that also generate ulcerations such as pyoderma gangrenosum. The only case reported in the medical literature shows hypodermal involvement7. However, the authors described the presence of a fistulous tract which was not observed in our CL cases.
This imaging modality has the potential to monitor the treatment non-invasively and testing the outcomes of leishmaniasis treatments in research and trials.
Acknowledgments
Funding sources: This work was supported by InnovatePerú/FINCYT (PIAP-3-P-872-14), Premio a la Investigación Inter-Universitaria y Multidisciplinaria 2014 and NIH/Fogarty International Center 5R25TW009340-04 (5037874).
Footnotes
Conflict of Interest: None declared
References
- 1.Alvar J, Velez ID, Bern C, Herrero M, Desjeux P, Cano J et al. Leishmaniasis worldwide and global estimates of its incidence. PloS one. 2012;7(5): e35671. Available from: doi.org/10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharquie K, Hameed A, Noaimi A. Panniculitis is a common unrecognized histopathological feature of cutaneous leishmaniasis. Indian Journal of Pathology and Microbiology. 2016;59(1): 16–19. Available from: http://www.ijpmonline.org/text.asp?2016/59/1/16/178216 [DOI] [PubMed] [Google Scholar]
- 3.Aronson N, Herwaldt BL, Libman M, Pearson R, Lopez-Velez R, Weina P, et al. Diagnosis and Treatment of Leishmaniasis: Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Am J Trop Med Hyg. 2016;63(12):e202–e264. Available from: doi: 10.1093/cid/ciw670. [DOI] [PubMed] [Google Scholar]
- 4.Harland CC, Bamber JC, Gusterson BA, Mortimer PS. High frequency, high resolution B‐scan ultrasound in the assessment of skin tumours. British Journal of Dermatology. 1993;128(5): 525–532. Available from: doi.org/10.1148/radiol.2511080912. [DOI] [PubMed] [Google Scholar]
- 5.Sharquie KE, Noaimi AA, Saleh BA. Cutaneous Leishmaniasis as Imitator of Skin Diseases and a Diagnostic Challenge. Journal of Cosmetics, Dermatological Sciences and Applications. 2018;8(03): 158 Available from: 10.4236/jcdsa.2018.83018. [DOI] [Google Scholar]
- 6.Sharquie KE, Hameed AF. Panniculitis is an important feature of cutaneous leishmaniasis pathology. Case reports in dermatological medicine, 2012. Available from: dx.doi.org/10.1155/2012/612434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pousa-Martínez M, Sánchez-Aguilar D, Aliste C, Vázquez-Veiga H. Usefulness of ultrasound in the diagnosis and follow-up of pyoderma gangrenosum. Actas dermo-sifiliograficas. 2017;108(10):962–964. Available from: 10.1016/j.ad.2017.02.025. [DOI] [PubMed] [Google Scholar]


