Abstract
Purpose
Intensity-modulated radiotherapy (IMRT) allows for more precise treatment, reducing unwanted radiation to nearby structures. We investigated the safety and feasibility of IMRT for anaplastic ependymoma patients below 3 years of age.
Materials and Methods
A total of 9 anaplastic ependymoma patients below 3 years of age, who received IMRT between October 2011 and December 2017 were retrospectively reviewed. The median equivalent dose in 2 Gy fractions was 52.0 Gy (range, 48.0 to 60.0 Gy). Treatment outcomes and neurologic morbidities were reviewed in detail.
Results
The median patient age was 20.9 months (range, 12.1 to 31.2 months). All patients underwent surgery. The rates of 5-year overall survival, freedom from local recurrence, and progression-free survival were 40.6%, 53.3%, and 26.7%, respectively. Of the 9 patients, 5 experienced recurrences (3 had local recurrence, 1 had both local recurrence and cerebrospinal fluid [CSF] seeding, and 1 had CSF seeding alone). Five patients died because of disease progression. Assessment of neurologic morbidity revealed motor dysfunction in 3 patients, all of whom presented with hydrocephalus at initial diagnosis because of the location of the tumor and already had neurologic deficits before radiotherapy (RT).
Conclusion
Neurologic morbidity is not caused by RT alone but may result from mass effects of the tumor and surgical sequelae. Administration of IMRT to anaplastic ependymoma patients below 3 years of age yielded encouraging local control and tolerable morbidities. High-precision modern RT such as IMRT can be considered for very young patients with anaplastic ependymoma.
Keywords: Pediatrics, Ependymoma, Intensity-modulated radiotherapy, Local neoplasm recurrence, Morbidity
Introduction
Ependymoma is the third most common pediatric brain tumor [1]. Thirty percent of all pediatric ependymomas occur in children below 3 years of age [2]. The 7-year local control and event-free survival rates in pediatric ependymoma patients undergoing current treatment regimens (maximal safe resection, followed by focal adjuvant radiotherapy [RT]) were reported to be 83.7% and 69.1%, respectively [3]. In particular, both progression-free survival (PFS) and overall survival (OS) were significantly worse in patients with anaplastic ependymoma (grade III) than in patients with grade II ependymoma [4].
Although RT is indispensable for the prevention of local recurrence of anaplastic ependymoma, the exposure of normal tissue to radiation may lead to acute or late toxicity. There are many reports of long-term sequelae of central nervous system (CNS) tumors, such as neurocognitive dysfunctions, growth disorders, psychological and behavioral disorders, ototoxicity, and increased risk of secondary malignancy [5-7]. On the basis of this evidence, many physicians try and avoid RT in children below 3 years of age who are particularly vulnerable to the damaging effects of radiation.
Despite concerns regarding RT-related toxicity, there is an emerging need for adjuvant RT in patients below 3 years of age with CNS tumors. The prospective German brain tumor trials HIT-SKK 87 and 92 [8] evaluated the role of RT in anaplastic ependymoma in children below 3 years of age and showed that delaying RT increased the risk of local recurrence even after intensive chemotherapy. In addition, according to the Children’s Oncology Group trial (ACNS0121) [9], the effectiveness of chemotherapy is not yet clear and thus extensive delays in or avoidance of adjuvant RT should be avoided.
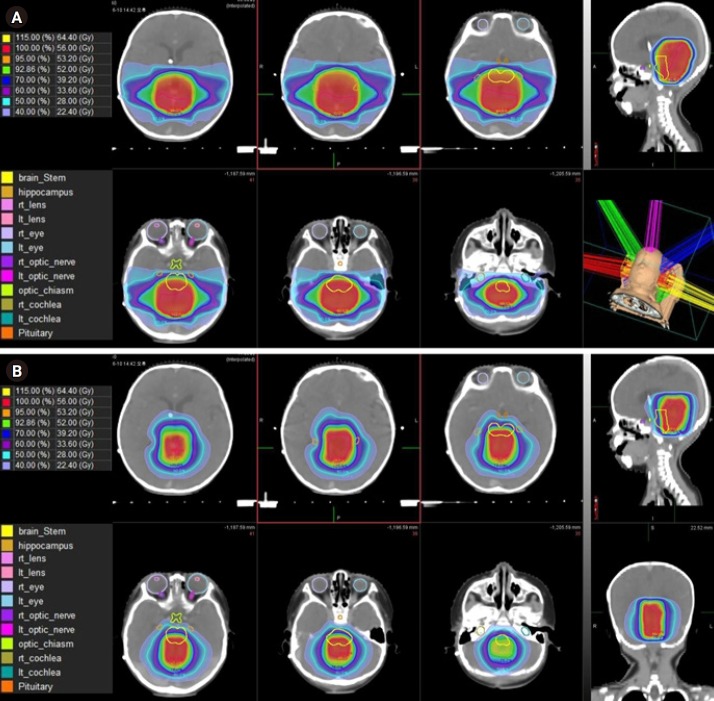
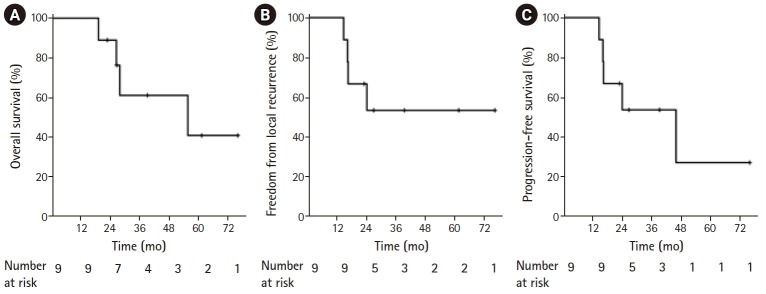
Recent developments in RT technology, such as intensity-modulated radiotherapy (IMRT), have led to more accurate and precise treatments than the three-dimensional conformal radiotherapy (3D-CRT) plans (Fig. 1), thereby reducing unnecessary radiation exposure of surrounding normal tissues. As shown on the dose volume histogram, there was a sharp reduction in the planning target volume (PTV) in the IMRT plan, representing the superior PTV dose homogeneity (Fig. 2). Moreover, dose-volume histograms showed a lower dose to the optic chiasm, brainstem, and both cochleae on IMRT, demonstrating that RT-related neurologic toxicity can be significantly reduced.
Fig. 1.
Comparison of three-dimensional conformal radiotherapy (A) versus intensity-modulated radiotherapy (B) in the treatment of brain tumor. The difference between preservation of optic chiasm, brainstem, and both cochlear among treatment plans can be compared visually to some extent.
Fig. 2.
Comparison of dose volume histograms between three-dimensional conformal radiotherapy (dotted line) and intensity-modulated radiotherapy (solid line). The planning target volume (PTV) in blue, optic chiasm in pink, brainstem in yellow, right cochlear in light green and left cochlea in orange.
The aim of this study was to evaluate the safety and feasibility of IMRT in children under 3 years of age who received IMRT for anaplastic ependymoma.
Materials and Methods
1. Patient selection
Patients below 3 years of age with anaplastic ependymoma who underwent postoperative IMRT at our institution between October 2011 and December 2017 were included in this study. All patients were diagnosed on the basis of histological confirmation and underwent magnetic resonance imaging (MRI) for disease evaluation and follow-up. Pathology was confirmed by surgical resection. A total of 9 patients were included in our study. This study was approved by the Institutional Review Board of the Yonsei University Health System (No. 4-2019-0939). The informed consent was waived by Institutional Review Board.
2. Follow-up and assessment of neurologic morbidity
During the RT period, patients were followed up clinically once a week. After RT, patients were followed up clinically within 1 month, then every 3 months for the first 2 years, every 6 months for 1 year, and once a year thereafter. MRI examination was also performed 1 month after RT, followed by every 3 months for the first year, every 6 months for next 2 years, and once a year thereafter. Recurrence was determined by comprehensive evaluation of MRI images and clinical findings.
Three categories related to neurologic morbidity (neurocognitive dysfunction, motor dysfunction, and hearing impairment) were retrospectively evaluated through medical records maintained by physiatrists, pediatric neurosurgeons, pediatric medical oncologists, and pediatric radiation oncologists as well as using the Denver Developmental Screening Test II (DDST-II) and the Bayley Scales of Infant and Toddler Development. The DDST-II is a revised version of the Denver Developmental Screening Test designed to identify developmental problems in children aged 0–6 years; it is divided into four areas: personal-social, fine motor-adaptive, language, and gross motor [10]. The Bayley Scales of Infant and Toddler Development (Bayley-III is the current version) are a standard series of measurements primarily used to assess the development of infants and toddlers aged 1–42 months [11]. Neurocognitive dysfunction was defined as the occurrence of declining intellectual function or of problems with attention, processing speed, or working memory [12]. Because treatment and clinical features were different for each patient, each patient’s record was reviewed in detail by radiation oncologists (JL, HIY, and COS) and a neurosurgeon (DSK) to analyze the exact causes of neurologic morbidity.
3. Radiotherapy
All patients underwent simulation computed tomography (CT) for RT planning. During simulation CT, the patient’s head and neck were immobilized with a thermoplastic mask in the supine position. Simulation CT images were imported into MIM software (MIM Software Inc., Cleveland, OH, USA) for target delineation. Gross tumor volume 1 (GTV1) consisted of any residual or recurrent lesions. GTV2 was defined as GTV1 plus the surgical cavity. Clinical target volume (CTV) was defined as GTV2 plus 0.5–1.0 cm margins. PTV was defined as the CTV plus 0.3 cm margins. The TomoTherapy (Accuray, Sunnyvale, CA, USA) or RayStation (RaySearch Laboratories, Stockholm, Sweden) software was used for IMRT plans. In an IMRT plan, higher doses were prescribed in the order of GTV1, GTV2, and CTV using a simultaneous-integrated boost technique. The median total dose of GTV1, GTV2, and CTV was equivalent to a dose of 2 Gy fractions (EQD2) 57.0 Gy (range, 56.0 to 60.0 Gy, α/β = 3), 52.0 Gy (range, 48.0 to 60.0 Gy, α/β = 3), and 40.0 Gy (range, 38.0 to 52.0 Gy, α/β = 3), respectively (Table 1).
Table 1.
Patient and treatment characteristics
| Characteristic | Value |
|---|---|
| Age (mo) | 20.9 (12.1–31.2) |
| Sex | |
| Male | 5 (55.6) |
| Female | 4 (44.4) |
| Tumor size (cm) | 5.1 (2.4–7.0) |
| Tumor site | |
| Supratentorial | 2 (22.2) |
| Infratentorial | 7 (77.8) |
| Surgery | |
| Gross total resection | 5 (55.6) |
| Near total resection | 2 (22.2) |
| Subtotal resection | 2 (22.2) |
| Total RT dose (Gy) (EQD2, α/β = 3) | |
| GTV1 | 57.0 (56.0–60.0) |
| GTV2 | 52.0 (48.0–60.0) |
| CTV | 40.0 (38.0–52.0) |
| Fractional RT dose (Gy) | |
| GTV1 | 2.0 (2.0–2.1) |
| GTV2 | 1.8 (1.8–2.0) |
| CTV | 1.5 (1.5–1.8) |
Values are presented as median (range) or number of patients (%).
RT, radiotherapy; EQD2, equivalent dose in 2 Gy fractions; GTV, gross tumor volume; CTV, clinical target volume.
If the patient was unable to fall asleep during RT, we attempted conscious sedation by administering 25–100 mg/kg chloral hydrate orally. In cases wherein chloral hydrate failed, we administered 0.05–0.1 mg/kg midazolam intravenously. If the second option also failed, we attempted general anesthesia by administrating propofol. Of our 9 patients, 2 went to sleep before RT, 3 were under conscious sedation with chloral hydrate, 1 was sedated with midazolam because of failure of chloral hydrate, and the other 3 were treated under general anesthesia with propofol.
4. Statistical analysis
OS is calculated from the date of RT to the date of death, regardless of the cause of death. Local recurrence is defined as recurrence within the RT field. Freedom from local recurrence (FFLR) is defined as the time from the date of RT to local recurrence. PFS is defined as the time from the date of RT to any recurrence or death. Survival outcomes were analyzed using the Kaplan-Meier method and log-rank test. Statistical analyses were performed using IBM SPSS version 23.0 software (IBM Corp., Armonk, NY, USA).
Results
1. Patient and treatment characteristics
The baseline and treatment characteristics of all 9 patients are listed in Table 1. The median patient age was 20.9 months (range, 12.1 to 31.2 months). Five patients were male and 4 were female. The median tumor size was 5.1 cm (range, 2.4 to 7.0 cm). The most common tumor location was the 4th ventricle (6 patients, 66.7%), and the remaining tumors were located in the cerebellopontine angle cistern, temporo-parieto-occipital lobe, or frontal lobe. When the location of the tumor was divided by the tentorium cerebelli, the tumors were in the infratentorial area in 7 patients.
All patients underwent surgery. Five patients underwent gross total resection (no residual tumor), 2 underwent near total resection (>90% of tumor removed), and 2 underwent subtotal resection (50%–90% of tumor removed) [13]. The time interval from surgery to RT was 20–140 days (median: 28 days). No patient received chemotherapy or peripheral blood stem cell transplantation. All patients except one received IMRT postoperatively at initial diagnosis. The remaining patient received salvage RT because of recurrence after the initial surgery.
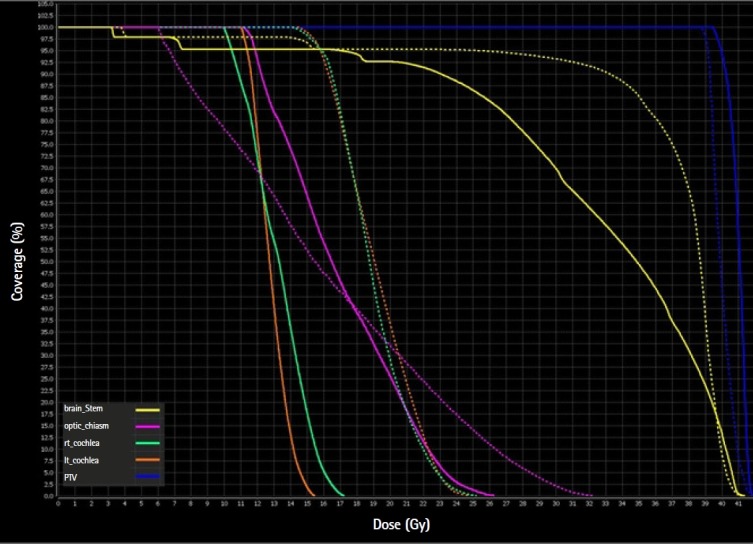
2. Survival outcomes
The median follow-up duration was 28.0 months (range, 19.3 to 76.0 months). The 5-year OS, FFLR, and PFS rates for all patients were 40.6%, 53.3%, and 26.7%, respectively (Fig. 3A–3C).
Fig. 3.
Kaplan-Meier curves of overall survival (A), freedom from local recurrence (B) and progression-free survival (C) in patients with anaplastic ependymoma.
Recurrence occurred in 5 patients: 3 had local recurrence, 1 had both local recurrence and cerebrospinal fluid (CSF) seeding, and 1 had CSF seeding alone. Four patients without recurrence had undergone gross total resection and received EQD2 52–60 Gy to the tumor bed. None of these 4 patients underwent additional surgery or chemotherapy after RT.
Of the 3 patients who underwent local recurrence, 1 received surgery and adjuvant chemotherapy as salvage treatment; however, residual tumor progression was observed. The patient subsequently underwent surgery but died because of disease progression. The second patient underwent gamma knife surgery as salvage treatment but developed CSF seeding thereafter. Despite subsequently undergoing palliative re-irradiation targeting the whole ventricle, the patient died because of disease progression. The third patient underwent surgery and gamma knife surgery for residual lesions, followed by adjuvant chemotherapy as salvage treatment. However, 1 year after the end of chemotherapy, a recurrent tumor was observed. Gamma knife surgery was repeated, but the patient died because of disease progression.
One patient with local recurrence and CSF seeding underwent surgery as salvage treatment and was expected to receive adjuvant chemotherapy; however, the treatment was delayed because of the patient’s poor physical condition, and the patient died because of progression of leptomeningeal seeding.
One patient who experienced CSF seeding at the age of 6 years 2 months was treated with tumor removal for recurrent lesions at the L2-L5 vertebrae of the spinal cord, followed by 36 Gy craniospinal irradiation and boost RT of 18 Gy to the tumor bed. Approximately 10 months after the end of RT, the patient showed no evidence of disease.
Of the 4 patients without recurrence, 2 received EQD2 52 Gy to the tumor bed after gross total resection of the 4th ventricle tumor and 40 Gy to the tumor bed plus margins. They showed no evidence of disease for approximately 2 years after RT completion. Another patient received EQD2 56 Gy to the tumor bed after gross total resection of the left temporal-parietal-occipital lobe tumor and 52 Gy to the tumor bed plus margins. This patient showed no evidence of disease for 6 years after RT completion. The last patient received EQD2 60 Gy to the tumor bed after gross total resection of the right frontal lobe tumor and 52 Gy to the tumor bed plus margins. The patient showed no evidence of disease for 2 years and 6 months after the RT completion.
3. Neurologic morbidity
Neurologic morbidity after treatment was evaluated in all patients, 3 (33.3%) of whom showed neurologic morbidity; all had motor dysfunction alone (Table 2). The first patient had a 5-cm-sized tumor located in the 4th ventricle, causing hydrocephalus. Before diagnosis, the patient was able to stand with support, but at the time of disease diagnosis and after surgery, the patient’s motor function had declined, and the patient was only able to sit with support for 1 minute. There was no difference in motor dysfunction before and after RT. The Denver Developmental Screening Test at 18 months of age showed that the development levels were those of an 11-month-old, characterized by difficulty standing alone because of a decline in overall muscle strength.
Table 2.
Summary for cases of neurologic morbidity
| Patient no. | Sex | Age at RT (mo) | Tumor size (cm) | Tumor site | Surgery extent | Hydrocephalus at diagnosis | Neurologic morbidity classification | Sx related to neurologic morbidity | Denver developmental screening test | Interval between onset of neurologic Sx and RT |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 12.1 | 5 | 4th ventricle | STR | Yes | MD | Sitting with arm support for only 1 minute | Gross motor: 11-month-old level (at 18 months of age) | 1 month before RT |
| 2 | M | 18.4 | 5 | 4th ventricle | NTR | Yes | MD | Delayed gross muscle development | Gross motor: 14-month-old level (at 18 months of age) | 1 month before RT |
| 3 | M | 31.2 | 5.9 | Left CPA cistern | STR | Yes | MD | Left hand weakness, overall postural tone deterioration | Gross motor: 9-month-old level (at 43 months of age) | 1 month before RT |
RT, radiotherapy; Sx, symptoms; F, female; M, male; CPA, cerebellopontine angle; STR, subtotal resection; NTR, near total resection; MD, motor dysfunction.
The second patient had a 5.0-cm-sized tumor located in the 4th ventricle, causing hydrocephalus. Hydrocephalus improved after surgery but was still observed. The patient showed delayed gross muscle development after surgery, and the Denver Developmental Screening Test at 18 months of age showed gross motor development levels equivalent to those of a 14-month-old. The motor dysfunction seen before RT was maintained after RT, and the patient subsequently underwent rehabilitation therapy.
The third patient had a 5.9-cm-sized tumor located in the left cerebellopontine angle cistern, causing hydrocephalus. There was no deterioration in motor function after the first surgery. However, left-hand weakness and overall postural tone deterioration developed with progression of the residual lesion. RT was performed on these residual lesions. Motor dysfunction present before RT persisted after RT. The patient underwent rehabilitation therapy, but persistent motor function deterioration was observed.
Discussion and Conclusion
In pediatric patients, the immature CNS is vulnerable to RT; therefore, the adverse effects of RT can be more severe than those in adults, which in turn may lead to problems such as delayed development [5,14]. Some studies have suggested that RT therapy should be delayed or excluded as a treatment option in pediatric patients, instead utilizing intensive chemotherapy until the age of 3 years, when CNS cell division is nearly complete [15,16]. However, delays in RT can compromise oncologic outcomes [8,17]. With advances in RT techniques, IMRT enables a more targeted delivery, sparing the normal tissue and markedly reducing toxicity compared to that with 3D-CRT. In our hospital, IMRT has been performed in patients below 3 years of age, resulting in an improvement in neurologic morbidity and treatment outcome.
The most important issue in the treatment of ependymoma is that it often occurs in children below 3 years of age who are more vulnerable to the damaging effects of RT [18]. Some studies have shown a poor outcome if RT was deferred for more than 1 year after surgery and therefore recommended immediate RT, even in children below 3 years of age [19]. In the analysis of the HIT-SKK 87 and 92 trials that exclusively enrolled patients below 3 years of age with anaplastic ependymoma, the 3-year OS was 66.7% when RT was administered immediately after chemotherapy, compared to 38.5% when RT was delayed [8]. As availability of IMRT has increased, recent studies analyzing pediatric ependymoma patients have shown that despite a reduction in treatment volumes treatment with IMRT results in favorable local control rates that do not increase the risk of marginal failure or neurologic toxicity compared to those published historically [20,21]. Together with the results presented here, these findings reveal that the use of IMRT can reduce toxicity while maximizing therapeutic outcomes for ependymoma patients below 3 years of age.
Until the 2000s, it was not possible to determine the optimal radiation dose for ependymoma because of small cohort sizes or heterogeneity between studies. Although some retrospective studies have recommended RT of 45 Gy or higher at the tumor site [22,23], the European Association of Neuro-Oncology (EANO) guidelines recently recommended a postoperative RT dose of 59.4 Gy for patients older than 18 months with World Health Organization (WHO) grade II or III ependymoma, whereas a dose of 54 Gy was recommended for patients younger than 18 months because of neurological vulnerability [24]. Given that the studies that were the basis for the EANO guidelines mainly used 3D-CRT, in the modern era, IMRT can be safely used to administer this radiation dose with lower toxicity. In the current study, the median total doses for residual lesions were EQD2 57.0 Gy (range, 56.0 to 60.0 Gy) and those for the tumor cavity were EQD2 52.0 Gy (range, 48.0 to 60.0 Gy). Although the statistical comparison was difficult because of the small the number of patients, the median total dose of tumor cavity in patients with in-field recurrence was EQD2 48.0 Gy (range, 48.0 to 52.0 Gy), whereas in patients without in-field recurrence, the median total dose was EQD2 54.0 Gy (range, 52.0 to 60.0 Gy). Thus, a sufficient radiation dose may be critical to achieve local control, and IMRT can be used for the administration of high radiation doses.
Regarding RT field, the German HIT-SKK 87 and 92 trials included neuraxis in the RT field [8], but more recent studies defined the RT field as the tumor bed plus margins [3,4]. The recently revised the EANO guideline also recommended setting the CTV to tumor bed plus margins [24]. In line with previous reports, our institution’s practice also defined RT field as tumor bed plus margins.
Radiation to critical tissues is known to be associated with the development of neurologic morbidity [5,14]. Previous studies that applied IMRT or proton therapy to brain tumors concluded that the use of advanced RT technique for brain tumors allows for improved target conformity and better critical tissue sparing, resulting in lower neurologic toxicity [25-27]. Therefore, on the basis of multiple studies, the application of a modern RT technique is important in pediatric patients.
In our study on very young children treated with IMRT, neurologic morbidity was observed in 3 patients (Table 2), all of whom had tumors located around the 4th ventricle. At the time of initial diagnosis, these 3 patients suffered from hydrocephalus due to the location of the tumor. Following RT, hydrocephalus worsened in only 1 patient. Considering the relationship between time of onset and RT, we can conclude that RT was not a direct cause of the hydrocephalus. This patient also exhibited motor dysfunction before RT, which did not worsen after RT. Issues arising from pediatric hydrocephalus, including surgical complications, academic achievement, and neurologic sequelae, have been the focus of numerous studies. Motor handicap in pediatric patients with hydrocephalus was reported in 30%–60% of cases [28-30], and low IQ was reported in 12.5%–54.7% of cases [31,32]. Our findings suggest that most toxicities are caused by mass effects from the tumor itself combined with sequelae from surgery.
One of the limitations of this study was the small sample size, making statistical analysis difficult. In addition, because we did not conduct longitudinal studies that prospectively measured neurologic deficits, it was difficult to analyze the changing patterns of neurologic deficiencies. Thus, although neurologic morbidity was thought to be caused by a combination of mass effects from the tumor and sequelae from surgery, it was difficult to determine how RT affected neurologic morbidity exactly. Despite these limitations, our results are still meaningful. Few previous studies have collected data from this many anaplastic ependymoma patients below 3 years of age who received IMRT from one institution. As well, we tried to analyze each case in detail and compared related factors to the greatest extent possible.
In conclusion, pediatric anaplastic ependymoma patients below the age of 3 years who received IMRT showed an encouraging local control rate and tolerable toxicity. These outcomes were comparable to those of other studies. Although neurologic morbidities were observed in 3 patients, these appear to be caused by the tumor itself and/or sequelae from surgery. On the basis of these results, when performing RT for anaplastic ependymoma in very young patients, a high-precision modern RT approach such as IMRT should be actively considered.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Halperin EC, Brady LW, Perez CA, Wazer DE. Perez & Brady's principles and practice of radiation oncology. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 2.White L, Kellie S, Gray E, et al. Postoperative chemotherapy in children less than 4 years of age with malignant brain tumors: promising initial response to a VETOPEC-based regimen. A Study of the Australian and New Zealand Children's Cancer Study Group (ANZCCSG) J Pediatr Hematol Oncol. 1998;20:125–30. doi: 10.1097/00043426-199803000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Merchant TE, Li C, Xiong X, Kun LE, Boop FA, Sanford RA. Conformal radiotherapy after surgery for paediatric ependymoma: a prospective study. Lancet Oncol. 2009;10:258–66. doi: 10.1016/S1470-2045(08)70342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massimino M, Miceli R, Giangaspero F, et al. Final results of the second prospective AIEOP protocol for pediatric intracranial ependymoma. Neuro Oncol. 2016;18:1451–60. doi: 10.1093/neuonc/now108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE. Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol. 2004;5:399–408. doi: 10.1016/S1470-2045(04)01507-4. [DOI] [PubMed] [Google Scholar]
- 6.Kiehna EN, Mulhern RK, Li C, Xiong X, Merchant TE. Changes in attentional performance of children and young adults with localized primary brain tumors after conformal radiation therapy. J Clin Oncol. 2006;24:5283–90. doi: 10.1200/JCO.2005.03.8547. [DOI] [PubMed] [Google Scholar]
- 7.Morris EB, Gajjar A, Okuma JO, et al. Survival and late mortality in long-term survivors of pediatric CNS tumors. J Clin Oncol. 2007;25:1532–8. doi: 10.1200/JCO.2006.09.8194. [DOI] [PubMed] [Google Scholar]
- 8.Timmermann B, Kortmann RD, Kuhl J, et al. Role of radiotherapy in anaplastic ependymoma in children under age of 3 years: results of the prospective German brain tumor trials HIT-SKK 87 and 92. Radiother Oncol. 2005;77:278–85. doi: 10.1016/j.radonc.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 9.Merchant TE, Mulhern RK, Krasin MJ, et al. Preliminary results from a phase II trial of conformal radiation therapy and evaluation of radiation-related CNS effects for pediatric patients with localized ependymoma. J Clin Oncol. 2004;22:3156–62. doi: 10.1200/JCO.2004.11.142. [DOI] [PubMed] [Google Scholar]
- 10.Frankenburg WK, Dodds J, Archer P, Shapiro H, Bresnick B. The Denver II: a major revision and restandardization of the Denver Developmental Screening Test. Pediatrics. 1992;89:91–7. [PubMed] [Google Scholar]
- 11.Bayley N. Bayley Scales of Infant and Toddler Development third edition (Bayley-III) San Antonio, TX: Pearson; 2006. [Google Scholar]
- 12.Stavinoha PL, Askins MA, Powell SK, Pillay Smiley N, Robert RS. Neurocognitive and psychosocial outcomes in pediatric brain tumor survivors. Bioengineering (Basel) 2018;5:73. doi: 10.3390/bioengineering5030073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wisoff JH, Boyett JM, Berger MS, et al. Current neurosurgical management and the impact of the extent of resection in the treatment of malignant gliomas of childhood: a report of the Children's Cancer Group trial no. CCG-945. J Neurosurg. 1998;89:52–9. doi: 10.3171/jns.1998.89.1.0052. [DOI] [PubMed] [Google Scholar]
- 14.Duffner PK, Cohen ME, Thomas PR, Lansky SB. The long-term effects of cranial irradiation on the central nervous system. Cancer. 1985;56(7 Suppl):1841–6. doi: 10.1002/1097-0142(19851001)56:7+<1841::aid-cncr2820561325>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 15.Horowitz ME, Mulhern RK, Kun LE, et al. Brain tumors in the very young child: postoperative chemotherapy in combined-modality treatment. Cancer. 1988;61:428–34. doi: 10.1002/1097-0142(19880201)61:3<428::aid-cncr2820610304>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 16.Duffner PK, Horowitz ME, Krischer JP, et al. Postoperative chemotherapy and delayed radiation in children less than three years of age with malignant brain tumors. N Engl J Med. 1993;328:1725–31. doi: 10.1056/NEJM199306173282401. [DOI] [PubMed] [Google Scholar]
- 17.Buscariollo DL, Park HS, Roberts KB, Yu JB. Survival outcomes in atypical teratoid rhabdoid tumor for patients undergoing radiotherapy in a Surveillance, Epidemiology, and End Results analysis. Cancer. 2012;118:4212–9. doi: 10.1002/cncr.27373. [DOI] [PubMed] [Google Scholar]
- 18.Goldwein JW, Leahy JM, Packer RJ, et al. Intracranial ependymomas in children. Int J Radiat Oncol Biol Phys. 1990;19:1497–502. doi: 10.1016/0360-3016(90)90362-n. [DOI] [PubMed] [Google Scholar]
- 19.Grundy RG, Wilne SA, Weston CL, et al. Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: the UKCCSG/SIOP prospective study. Lancet Oncol. 2007;8:696–705. doi: 10.1016/S1470-2045(07)70208-5. [DOI] [PubMed] [Google Scholar]
- 20.Beltran C, Naik M, Merchant TE. Dosimetric effect of setup motion and target volume margin reduction in pediatric ependymoma. Radiother Oncol. 2010;96:216–22. doi: 10.1016/j.radonc.2010.02.031. [DOI] [PubMed] [Google Scholar]
- 21.Weber DC, Zilli T, Do HP, Nouet P, Gumy Pause F, Pica A. Intensity modulated radiation therapy or stereotactic fractionated radiotherapy for infratentorial ependymoma in children: a multicentric study. J Neurooncol. 2011;102:295–300. doi: 10.1007/s11060-010-0318-2. [DOI] [PubMed] [Google Scholar]
- 22.Goldwein JW, Corn BW, Finlay JL, Packer RJ, Rorke LB, Schut L. Is craniospinal irradiation required to cure children with malignant (anaplastic) intracranial ependymomas? Cancer. 1991;67:2766–71. doi: 10.1002/1097-0142(19910601)67:11<2766::aid-cncr2820671109>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 23.Wallner KE, Wara WM, Sheline GE, Davis RL. Intracranial ependymomas: results of treatment with partial or whole brain irradiation without spinal irradiation. Int J Radiat Oncol Biol Phys. 1986;12:1937–41. doi: 10.1016/0360-3016(86)90128-8. [DOI] [PubMed] [Google Scholar]
- 24.Ruda R, Reifenberger G, Frappaz D, et al. EANO guidelines for the diagnosis and treatment of ependymal tumors. Neuro Oncol. 2018;20:445–56. doi: 10.1093/neuonc/nox166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blomstrand M, Brodin NP, Munck Af Rosenschold P, et al. Estimated clinical benefit of protecting neurogenesis in the developing brain during radiation therapy for pediatric medulloblastoma. Neuro Oncol. 2012;14:882–9. doi: 10.1093/neuonc/nos120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gross JP, Powell S, Zelko F, et al. Improved neuropsychological outcomes following proton therapy relative to X-ray therapy for pediatric brain tumor patients. Neuro Oncol. 2019;21:934–43. doi: 10.1093/neuonc/noz070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kahalley LS, Ris MD, Grosshans DR, et al. Comparing intelligence quotient change after treatment with proton versus photon radiation therapy for pediatric brain tumors. J Clin Oncol. 2016;34:1043–9. doi: 10.1200/JCO.2015.62.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Platenkamp M, Hanlo PW, Fischer K, Gooskens RH. Outcome in pediatric hydrocephalus: a comparison between previously used outcome measures and the hydrocephalus outcome questionnaire. J Neurosurg. 2007;107(1 Suppl):26–31. doi: 10.3171/PED-07/07/026. [DOI] [PubMed] [Google Scholar]
- 29.Kao CL, Yang TF, Wong TT, et al. The outcome of shunted hydrocephalic children. Zhonghua Yi Xue Za Zhi (Taipei) 2001;64:47–53. [PubMed] [Google Scholar]
- 30.Hoppe-Hirsch E, Laroussinie F, Brunet L, et al. Late outcome of the surgical treatment of hydrocephalus. Childs Nerv Syst. 1998;14:97–9. doi: 10.1007/s003810050186. [DOI] [PubMed] [Google Scholar]
- 31.Lindquist B, Persson EK, Fernell E, Uvebrant P. Very long-term follow-up of cognitive function in adults treated in infancy for hydrocephalus. Childs Nerv Syst. 2011;27:597–601. doi: 10.1007/s00381-010-1311-y. [DOI] [PubMed] [Google Scholar]
- 32.Kokkonen J, Serlo W, Saukkonen AL, Juolasmaa A. Long-term prognosis for children with shunted hydrocephalus. Childs Nerv Syst. 1994;10:384–7. doi: 10.1007/BF00335127. [DOI] [PubMed] [Google Scholar]