Abstract
Purpose
Although it is a well-known disease, the occurrence of Herpes simplex encephalitis (HSE) during a hospital stay may render the diagnosis particularly challenging. The objective of this report is to alert clinicians about the diagnostic pitfalls arising from hospital-developed HSE.
Materials and methods
Clinical observation of one patient.
Case report
An 87-year-old male was admitted to the Intensive Care Unit (ICU) because of respiratory failure due to an exacerbation of myasthenia gravis. After corticoids and azathioprine treatment, his clinical condition improved, allowing weaning from mechanical ventilation. One month after admission, while still hospitalized in the ICU, the patient developed fever and confusion. In the context of confounding factors, HSE was not suspected before a convulsive status epilepticus occurred, resulting in a significant delay in treatment. Diagnosis was confirmed by PCR-analysis in the cerebrospinal fluid. Serological status confirmed reactivation of prior herpes simplex infection. The patient died one week after the onset of confusion.
Conclusions
Hospital-“acquired” HSE must be suspected in case of new neurologic symptoms associated with fever, even in ICU-hospitalized patients. The diagnosis is made even more difficult by nonspecific symptoms due to previous diseases, leading to an even more severe prognosis in those vulnerable patients.
Keywords: Electrophysiology, Infectious disease, Neurology, Neurosurgery, Intensive care medicine, Herpes simplex Encephalitis, Intensive care, Immunosuppression, ICU acquired Infection, Herpes simplex reactivation
Electrophysiology; Infectious disease; Neurology; Neurosurgery; Intensive care medicine; Herpes simplex Encephalitis; Intensive care; Immunosuppression; ICU acquired Infection; Herpes simplex reactivation
1. Introduction
Acute viral encephalitis can be caused by several types of virus, especially herpes viruses (Herpes Simplex virus 1, 2, 6, Varicella Zoster Virus, Cytomegalovirus, Epstein Barr virus etc.). Although it is a relatively rare disease, Herpes simplex Encephalitis (HSE) is the main cause of acute encephalitis [1, 2, 3]. Thanks to early diagnosis by Polymerase Chain Reaction (PCR) in the cerebrospinal fluid (CSF) and to acyclovir therapy, mortality dropped [1, 2, 3], even if neurological sequelae remain frequent. However, in immunocompromised patients atypical illness and poorer outcomes have been described [1]. Mechanisms exacerbating virulence of herpes simplex virus (HSV) in these patients are still unknown, but HSE is not yet considered as an opportunistic infection. We report the case of severe intensive care unit (ICU)-“acquired” HSE after three weeks of corticosteroids and immunosuppressive therapy.
2. Case report
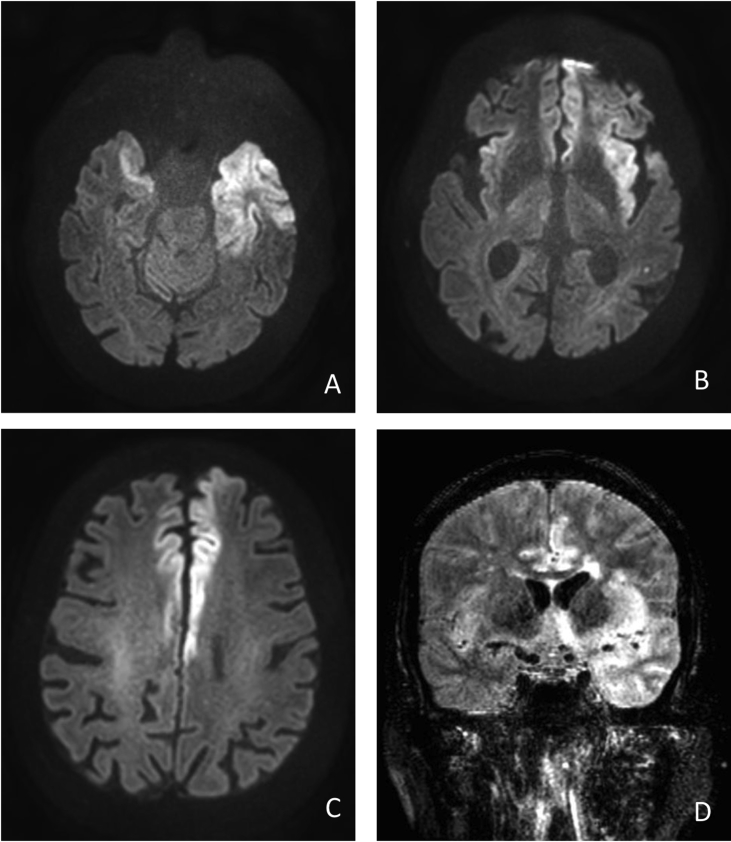
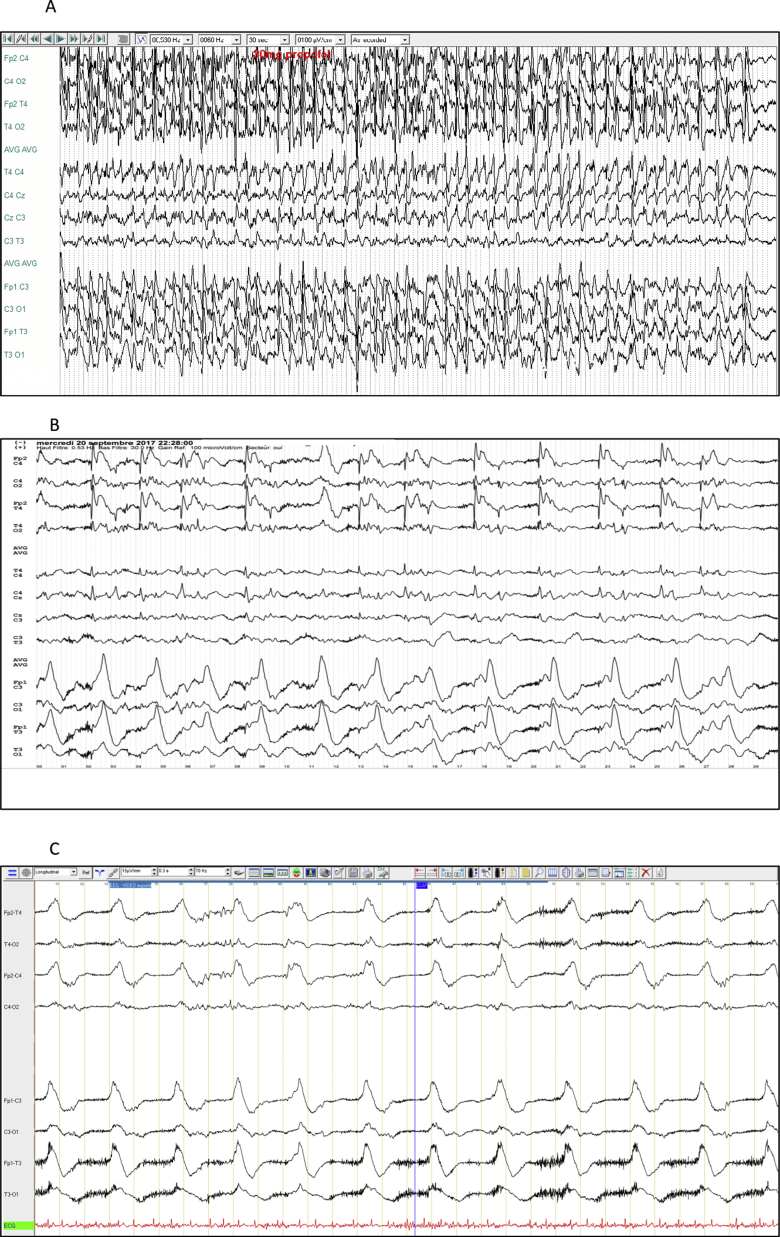
An 87-year-old male was admitted on August 15th to the neurological ward for an exacerbation of myasthenia gravis (swallowing disorder and dysphonia, Osserman myasthenia score at 61). His medical history included bulbar myasthenia gravis since 2015 (positive anti choline-acethyl receptor antibodies), atrial fibrillation, left middle cerebral artery infarctus of cardioembolic cause without sequelae five months prior (no visible on Figure 2), giant cell arteritis, and a prostatic adenocarcinoma considered as cured. Despite his medical history, he used to be self-sufficient at home, and he presented neither focal neurological deficits nor cognitive complaints. He had no fever. His usual treatment included pyridostigmine, apixaban, and prednisolone (10 mg/day). On August 19th, he was transferred to the ICU because of acute respiratory failure requiring endotracheal intubation with mechanical ventilation. CT scans of the chest showed parenchymal condensation of the two lung bases, with an effusion blade bilateral pleural, in favour of associated bilateral inhalation pneumonia. Due to lack of clinical improvement after intravenous (IV) polyvalent immunoglobulin, he received a second-line treatment that consisted of azathioprine and methylprednisolone 0.75 mg/kg/day. Tracheotomy was performed on September 8th, allowing meaning from mechanical ventilation on September 10th. Thus, acute respiratory failure lasted 22 days. On September 16th, although clinical state had improved (best Osserman myasthenia score 50 on the 12th), the patient became confused. On the 17th, apixaban was discontinued because of rectal bleeding. On the 18th, he developed fever (38.5 °C), and alveolar consolidation that motivated antibiotic therapy (piperacillin–tazobactam). On the 20th, four days after the onset of confusion, he developed a focal secondarily generalized tonic–clonic seizure starting on his right hemiface, evolving into a status epilepticus. The patient was treated with IV valproate 15 mg/kg as first-line treatment, and then with propofol and midazolam. The cerebral CT at 3 a.m. showed no significant changes, but the electroencephalogram (EEG), recorded at 6.30 a.m. revealed a right hemispheric status epilepticus, controlateral to his left posterior stroke sequelae (Figure 1A). Magnetic resonance imaging (MRI) on September 20th at 9 p.m. showed bilateral insular, frontal and temporal hypersignal predominant on the left hemisphere (Figure 2) and motivated immediate treatment with acyclovir (15 mg/kg every 8 h). A second EEG at 10 p.m. was markedly aggravated with the emergence of high amplitude periodic complexes predominating on the left fronto-temporal electrodes (Figure 1B). EEG was thus strongly in favor of HSV encephalitis. The lumbar puncture performed after a negative apixaban testing, showed 576 white bloods cells/mm [3], 909 red blood cells/mm3, protein 144 mg/dl, glucose 2,63 mmol/l. The positive HSV-2 PCR in the cerebrospinal fluid (CSF) confirmed the diagnosis of HSE on September 21st (HSV-1 and VZV PCR were negative). The blood serological status was in favour of a viral reactivation: IgM negative and IgG positive for HSV1 and HSV2. Anti-NMDA receptor antibodies were also negative in serum, as well as anti-Yo, anti-Hu, anti-Ri, anti-amphiphysine, anti-Ma2, anti-CV2 (september 18th). Despite the treatment, the clinical state did not improve. A third EEG, performed on 21st, was compatible with a highly advanced state of HSE, displaying a typical bi-hemispheric monomorphic, ample, periodic and areactive sub-delta activity (Figure 1C). The patient died one week after the onset of confusion.
Figure 2.
MRI (September 20th at 9 p.m.). High signal intensity lesions in Diffusion (A,B,C) and in T2 fluid-attenuated inversion recovery (FLAIR) (D) sequences in the bilateral temporal, frontal lobes and cingular gyri.
Figure 1.
EEG recordings of epileptic and periodic discharges. 1A. September 20th at 6.30 a.m.: Status epilepticus: Continuous rhythmic spike-wave activity prevailing on the right hemisphere with left hemispheric propagation and a minor attenuation by propofol. 1B. September 20th at 10 p.m.: Within 16h, substantial changes were visible on EEG, which now showed unreactive right paroxysmal fronto-central spikes waves of short periodicity and left fronto-temporal monomorphic periodic delta activity in favor of HSE. Midazolam had no effect on the periodic pattern. 1C. September 21st: Slow monomorphic bi-hemispheric periodic subdelta complexes, unreactive to external stimuli, indicating very advanced stages of HSE.
The patient's wife gave her consent for the publication of this case report and the two associated images (EEG and MRI).
3. Discussion
The present case study demonstrates the pitfalls of HSE-diagnosis in the context of the ICU. In our patient, HSE occurred one month after admission for acute respiratory failure related to myasthenia gravis. It is very unlikely that HSE was already present at admission, since the patient had no fever or confusion signs. Moreover, outcome was initially favourable without antiviral treatment. Due to the nonspecific nature of the early symptoms of HSE, which mimicked a bacterial ICU acquired-infection, diagnosis and antiviral treatment were delayed. This has certainly contributed to the fatal outcome, as did the patient's general vulnerability after immunosuppressive treatment and one month of hospitalization in the ICU. Since our patient received IV polyvalent immunoglobulins, one might speculate on a false positive HSV serology. In fact, both HSV 1 and 2 serologies were positive, but only HSV-2 was confirmed by PCR. HSV-2 encephalitis are less common than HSV-1, but can occur [2, 3].
An autoimmune encephalitis could have been suggested at the time of the secondary neurological worsening. However, the brutal clinical pattern, with general signs of sepsis (fever, mottling, chills) mainly evoke a septic complication. Moreover, although Anti-neuronal receptor antibodies have not been searched in CSF, they were negative in serum. Finally the MRI pictures and the evolution EEG towards bitemporal necrosis in 24 h are quasi-pathognomonic of an HSE. The immunosuppressive treatment received by the patient for more than one month is yet another argument in favour of HSE.
In the literature, there is a wide spectrum of medical conditions that could theoretically promote HSE: both systemic immunocompromised status (radiation, chemotherapy, corticosteroids, human immunodeficiency virus, etc.) [1, 2], and local brain injury (cranial trauma, brain surgery) have been suggested as possible risk factors for HSE, in single case reports, but higher level evidence is lacking. Especially, corticosteroids have been recently described as a risk factor of HSE, either in monotherapy or in combination with chemotherapy. To our knowledge, except new-born cases, only three cases of “nosocomial HSE” have been reported [4, 5]. Prognosis was poor in these patients, although there were not deeply immunosuppressed.
As a matter of fact, pathophysiology of HSE remains elusive. It is generally accepted that it comes from the resurgence of the quiescent virus, and some authors claim that it would imply rather excessive inflammation than immunosuppression [1, 6]. It is of note that those articles do not report the HSV serologies that would have allowed to distinguish viral reactivation from actual nosocomial infection. In our case, the serological status was in favour of a recent viral reactivation. Moreover, since HSV-2 is most often sexually transmitted, it is very unlikely that the patient contracted it while in ICU. However, we called it "acquired-ICU HSE" because of the analogy with bacterial infections authentically acquired in ICU.
HSE diagnosis in immunocompromised patients is made difficult by the atypical symptoms and low leucocytes count in the CSF [1]. Furthermore, assessment of ICU-developed HSE is difficult because of nonspecific symptoms like confusion and moderate fever that could emanate from a multitude of other pathologies, e.g. hyponatremia, sedatives, pneumonia or other nosocomial infections, etc. Individual circumstances may add up to hinder rapid diagnosis. In our case, the CSF examination was delayed because of long acting anticoagulant. EEG and MRI helped crucially in therapeutic decision making, but their specificity was all the more pronounced as HSE had already been evolving for four days. In fact, access to early cerebral MRI is mandatory to shorten the diagnostic delay [2, 4].
Very little is known about hospital-developed HSE, but according to the sparse existing literature, the diagnosis of HSE is probably underestimated [6], and the outcome appears to be dramatic. Delayed diagnosis and treatment on one hand, and patient vulnerability on the other contribute to the poor prognosis.
4. Conclusion
Physicians should be aware of the possibility of HSE during hospitalization, probably by virus reactivation due to immunosuppression or local inflammation. The diagnosis of HSE is probably underestimated, and must be evoked in the presence of fever associated with any new onset neurological symptom (confusion, alteration of consciousness, meningeal signs, seizures…). In this situation, neurological investigations are urgent. Early MRI and EEG are sensitive and specific, and are even more useful when the lumbar puncture has to be delayed. A systemic antiviral treatment must be initiated before definitive virologic confirmation.
HSE: Herpes simplex encephalitis, ICU: Intensive Care Unit, CSF: cerebrospinal fluid, EEG: electroencephalogram, MRI: Magnetic resonance imaging, PCR: Polymerase Chain Reaction, IV: Intravenous, CT: Computed Tomography.
Declarations
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Tan I.L., McArthur J.C., Venkatesan A., Nath A. Atypical manifestations and poor outcome of herpes simplex encephalitis in the immunocompromised. Neurology. 2012;79:2125–2132. doi: 10.1212/WNL.0b013e3182752ceb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaquet P., de Montmollin E., Dupuis C., Sazio C., Conrad M., Susset V. Functional outcomes in adult patients with herpes simplex encephalitis admitted to the ICU: a multicenter cohort study. Intensive Care Med. 2019;45:1103–1111. doi: 10.1007/s00134-019-05684-0. [DOI] [PubMed] [Google Scholar]
- 3.Dhull D., Sharma V., Sharma Y., Kaushik S. Applicability of molecular assays for detection and typing of herpes simplex viruses in encephalitis cases. Virusdisease. 2019;30:504–510. doi: 10.1007/s13337-019-00558-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doshi P., Donovan Post M.J., Saigal G., Podda A., Quencer R. Nosocomial Herpes Encephalitis: rare but treatable with early MR diagnosis. NeuroRadiol. J. 2013;26:168–174. doi: 10.1177/197140091302600206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Algahtani H., Shirah B., Hmoud M., Subahi A. Nosocomial herpes simplex encephalitis: a challenging diagnosis. J Infect Publ. Health. 2017;10:343–347. doi: 10.1016/j.jiph.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Jouan Y., Grammatico-Guillon L., Guillon A. Nosocomial herpes simplex encephalitis: does it really exist? J Infect Publ. Health. 2018;11:142. doi: 10.1016/j.jiph.2016.11.001. [DOI] [PubMed] [Google Scholar]