Abstract
We performed a point seroprevalence survey of measles among healthcare workers (HCWs) at two Korean teaching hospitals in 2019. A total of 2,830 HCWs underwent an antibody test. The overall seropositivity of measles was 93.1%. The seroprevalence of measles was lowest in HCWs aged 20 - 24 years (81.2%), followed by those aged 25 - 29 years (90.1%). The rates of anti-measles IgG positivity were significantly different between the two hospitals (97.0% vs. 89.4%, P <0.001). These results suggest that the seropositivity of measles in HCWs may differ depending on the hospital's vaccination policy.
Keywords: Measles, Measles-Mumps-Rubella vaccine, Healthcare workers, Seroprevalence
Measles was declared to have been eliminated in the Korea in 2014, after a nationwide outbreak in 2000 - 2001 [1]. However, measles outbreaks have been occurring thereafter in the community and in healthcare settings because of cases imported from other countries [2,3,4]. In a recent outbreak involving 16 patients (8 children and 8 adults) in Daegu, Korea, between December 2018 and January 2019, five of the adult patients were healthcare workers (HCWs) [3]. To prevent nosocomial spread of measles, high levels of seropositivity should be maintained in HCWs. Therefore, it is essential to determine the rate of anti-measles antibody positivity of HCWs in the Korea. This study aimed to determine and compare the seroprevalence of anti-measles immunoglobulin G (IgG) in HCWs at two Korean teaching hospitals in 2019. We also investigated the vaccination records of seronegative HCWs.
After outbreaks of measles occurred in Korea in 2018 - 2019, a point-prevalence survey of measles antibodies in HCWs was planned at two university-affiliated teaching hospitals with 600 - 650 beds in Seoul and Goyang. Serologic testing of HCWs for anti-measles IgG was performed in September 2019 at hospital A and in May 2019 at hospital B. Anti-measles IgG was detected using a chemiluminescence immunoassay (LIAISON® Measles IgG, DiaSorin, Saluggia, Italy) on a LIAISON® analyzer according to the manufacturer's instructions. Borderline or equivocal anti-measles IgG values were considered negative.
The measles vaccination histories of seronegative HCWs were retrieved from the web-based immunization registry system operated by the Korea Centers for Disease Control and Prevention (KCDC) [5].
Since 2014, hospital A has recommended two doses of the measles, mumps, and rubella (MMR) vaccination to newly employed HCWs unless they have documentation showing that they have received two doses of measles vaccine or evidence of immunity. At hospital B, since 2018 new HCWs have been required to submit documentation proving that they have received two doses of measles vaccination. If documentation cannot be provided, mandatory measles antibody screening and subsequent MMR vaccination is performed. At both study hospitals, neither mandatory measles antibody screening nor MMR vaccination program has been implemented to their current HCWs before 2019. This study was approved by the institutional review board of hospital A, with a waiver of consent.
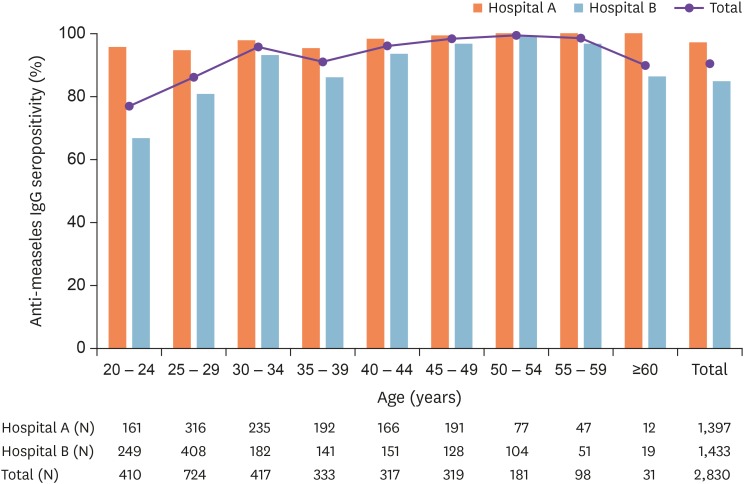
The measles antibody screening was performed in 1,397 (98.4%) of the 1,419 HCWs at hospital A and 1,433 (99.5%) of the 1,440 HCWs at hospital B. The age distribution of the 2,830 total HCWs was 20 - 87 (median 33) years, and 2,072 (73.2%) were female. The overall seropositivity for measles was 93.1% (Fig. 1). The rate of anti-measles IgG positivity was significantly higher at hospital A than at hospital B (97.0% vs. 89.4%, P <0.001). The seroprevalence of anti-measles antibodies in HCWs according to the hospital and age group is shown in Table 1. The seropositivity was lowest in HCWs aged 20 – 24 years (81.2%), followed by those aged 25 - 29 years (90.1%) (P <0.001). In HCWs aged ≥50 years, the anti-measles antibody positivity rate was 100% at both hospitals. The seropositivity of measles was significantly higher at hospital A than hospital B in both the 20 – 24 year (95.7% vs. 71.9%, respectively, P <0.001) and 25 – 29 year (94.6% vs. 86.5%, respectively, P <0.001) age groups.
Figure 1. Seroprevalence of anti-measles IgG antibodies and the number of healthcare workers based on the hospital and age distribution.
IgG, immunoglobulin G.
Table 1. Numbers (%) of healthcare workers positive for anti-measles IgG antibodies by age group.
| Age, years (birth year) | 20 – 24a (1994 – 1998) | 25 – 29a (1989 – 1993) | 30 – 34 (1984 – 1988) | 35 – 39 (1979 – 1983) | 40 – 44 (1974 – 1978) | 45 – 49 (1969 – 1973) | 50 – 54 (1964 – 1968) | 55 – 59 (1959 – 1963) | ≥60 (≤1958) | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| Hospital A | 154 (95.7) | 299 (94.6) | 230 (97.9) | 183 (95.3) | 163 (98.2) | 190 (99.5) | 77 (100) | 47 (100) | 12 (100) | 1,355 (97.0) |
| Hospital B | 179 (71.9) | 353 (86.5) | 175 (96.2) | 131 (92.9) | 145 (96.0) | 124 (96.9) | 104 (100) | 51 (100) | 19 (100) | 1,281 (89.4) |
| Total | 333 (81.2) | 652 (90.1) | 405 (97.1) | 314 (94.3) | 308 (97.2) | 314 (98.4) | 181 (100) | 98 (100) | 31 (100) | 2,636 (93.1) |
aP <0.001 between hospital A and B.
IgG, immunoglobulin G.
Of the 2,830 HCWs tested, 194 (6.9%) were measles-antibody negative, and they were 20 - 47 (median 25.5) years old. Of these, 154 (79.4%) had immunization records of receiving more than one dose of measles-containing vaccine (MCV) in either childhood or adulthood (Table 2). Of these 154 HCWs, 75 (38.7%) were presumed to have received the catch-up MCV as a child during the 2000 – 2001 nationwide measles outbreak. Among the seronegative HCWs, 41 (21.1%) had received up to three doses of the MMR vaccination after the age of 18 years, most often at the start of employment at the hospital. Notably, we found one HCW who did not have measles antibodies despite multiple documented doses of MCV administration, including one dose of MCV in the 2001 catch-up as a child and three doses of the MMR vaccine as an adult.
Table 2. Documented administration of measles-containing vaccines in seronegative healthcare workers in the study hospitalsa .
| Vaccination time and frequency | Hospital A (N = 42) | Hospital B (N = 152) | Total (N = 194) | |
|---|---|---|---|---|
| Childhood | 23 (54.8%) | 117 (77.0%) | 140 (72.2%) | |
| Before 2001 | 4 (9.5%) | 41 (27.0%) | 45 (23.2%) | |
| 2001 | 15 (35.7%) | 60 (39.5%) | 75 (38.7%) | |
| After 2001 | 4 (9.5%) | 16 (10.5%) | 20 (10.3%) | |
| Adulthood (≥18 years old ) | 23 (54.8%) | 18 (11.8%) | 41 (21.1%) | |
| 1 dose | 19 (45.2%) | 15 (9.9%) | 34 (17.5%) | |
| 2 doses | 3 (7.1%) | 3 (2.0%) | 6 (3.1%) | |
| 3 doses | 1 (2.4%) | 0 | 1 (0.5%) | |
| Overall | 33 (78.6%) | 121 (79.6%) | 154 (79.4%) | |
| 1 dose | 19 (45.2%) | 102 (67.1%) | 121 (62.4%) | |
| 2 doses | 10 (23.8%) | 15 (9.9%) | 25 (12.9%) | |
| ≥3 doses | 4 (9.5%) | 4 (2.6%) | 8 (4.1%) | |
aThe measles vaccination history was retrieved from the web-based immunization registry system operated by the Korea Centers for Disease Control and Prevention (https://nip.cdc.go.kr/irgd/index.html))
In this study, the overall measles seropositivity of HCWs was 93.1%, which is comparable with, or higher than, the seropositivity rates reported in other Korean hospitals in 2019 [3,6]. A recent study [3] observed that rates of measles seropositivity among HCWs differed significantly among six hospitals (59.9 – 93.1%), despite all being university-affiliated and/or teaching hospitals located in the same metropolitan city. The differences in measles seropositivity among the hospitals' HCWs was presumed to be due to differences in the MMR vaccination policies of the hospitals or nursing colleges [3]. In fact, nurses at both study hospitals, comprising most of newly employed HCWs, were graduates from about 70 different nursing colleges. Because of such heterogeneity, we do not think that the MMR vaccination policies of nursing colleges affected the measles seropositivity in our study. We hypothesize that the difference in the seroprevalence of measles antibodies at the study hospitals may have been due to the hospitals' vaccination policies for HCWs, since the seropositivity rate was higher among the younger HCWs of hospital A, where the MMR vaccination is recommended to newly employed seronegative HCWs. The results of this study, together with those of other studies [3,6], support the recommendation of the Korean Society of Infectious Diseases that HCWs without evidence of immunity or documentation showing that they have received two doses of the MMR vaccination should receive two doses of the MMR vaccine [7].
In this study, the lowest seropositivity rate found was in HCWs aged 20 – 24 years, which is consistent with previous reports [3,6,8,9]. Individuals in this age group were not included in the MMR catch-up vaccination program in 2001, which targeted children aged 8 – 16 years, but instead were required to show proof of MCV vaccination before entry into elementary school [9]. In addition, HCWs aged 25 – 29 years also had a low seropositivity rate at study hospital B, although most of the HCWs in this age group were presumed to have received the measles catch-up vaccination in 2001. The reason for the low seropositivity rate in younger HCWs is unknown [6,8,9].
Of note, 79.4% (154/194) of measles-antibody-negative HCWs had received at least one dose of MCV during childhood and/or adulthood. Of these HCWs, 33 (17.0%) had immunization records of more than two doses of MCV but nevertheless were found to be seronegative. Recently, a case of measles was reported in a Korean HCW who had documentation of having received two doses of MCV [10]. Until now, documentation of two doses of MMR vaccination has generally been considered confirmation of immunity [7,11]. However, as in our cases, there have been reports that documentation of two doses of MMR vaccination does not guarantee immunity [9,10]. Based on these findings, documentation of receiving two doses of MCV, especially in young Korean HCWs, may not be sufficient for preventing the spread of measles in hospitals. We may need a more conservative strategy, including measles antibody testing and additional doses of MMR if the newly employed HCWs are negative for measles antibodies.
This study had several limitations. We did not investigate the measles vaccination records of seropositive HCWs; thus, measles vaccination status could not be compared between the seronegative and seropositive HCWs in this study. Furthermore, the measles vaccination histories of the seronegative HCWs were not complete, since not all immunization records were registered in the KCDC immunization registry system, which is based on a website that was created in 2002 to store and manage immunization records [12,13]. Not all past vaccinations were registered at the initial implementation stage, and this immunization registry relied on the voluntary registration of immunization providers until 2009. Moreover, registration of non-National Immunization Program vaccinations, especially in adults, is not mandatory [14]. Therefore, the measles vaccination rate among our HCWs might have been underestimated.
In summary, the results of this study show that measles antibody seroprevalence among HCWs can differ between hospitals depending on their vaccination policies for HCWs. We found that among HCWs working at Korean hospitals in 2019, those in their early 20s were the most vulnerable to measles. Therefore, additional measures are necessary for HCWs in this age group to prevent nosocomial transmission of measles in the hospital setting. Further immunological studies to determine the cause of measles seronegativity are needed in a small number of HCWs who were administered multiple doses of MCV but failed to form anti-measles IgG antibodies.
ACKNOWLEDGMENT
We thank the staff of the Infection Control Offices of both study hospitals for their assistance.
Footnotes
Funding: None.
Conflicts of Interest: BNK is an associate editor of the journal Infect Chemother. However, he did not involve in the reviewer selection, evaluation, and decision making of this article. Otherwise, no conflicts of interest were reported.
- Conceptualization: YGK, BNK.
- Data curation: GBO, IHJ, HMY, GMY.
- Formal analysis: YGK, BNK.
- Investigation: YGK, BNK.
- Supervision: YGK, BNK.
- Writing - original draft: YGK, BNK.
- Writing - review & editing: YGK, GBO, IHJ, CRC, NK, JES, HMY, GMY, MJL, BNK.
References
- 1.Choe YJ, Jee Y, Oh MD, Lee JK. Measles elimination activities in the western pacific region: experience from the Republic of Korea. J Korean Med Sci. 2015;30(Suppl 2):S115–S121. doi: 10.3346/jkms.2015.30.S2.S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi WS, Sniadack DH, Jee Y, Go UY, So JS, Cho H, Bae GR, Lee DH, Kim K, Yoon HS, Chung YS, Kang C, Park H, Park O, Lee JK. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J Infect Dis. 2011;204(Suppl 1):S483–S490. doi: 10.1093/infdis/jir087. [DOI] [PubMed] [Google Scholar]
- 3.Chang HH, Kim SW, Kwon KT, Kim HI, Kim MJ, Ryu SY, Kim HA, Hur J, Kwon HH, Hong HL. Preliminary Report of Seroprevalence of Anti-Measles Immunoglobulin G among Healthcare Workers of 6 Teaching Hospitals of Daegu, Korea in 2019. Infect Chemother. 2019;51:54–57. doi: 10.3947/ic.2019.51.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang TU, Kim JW, Eom HE, Oh HK, Kim ES, Kang HJ, Nam JG, Kim KS, Kim SS, Lee CK, Park YJ, Park O. Resurgence of measles in a country of elimination: interim assessment and current control measures in the Republic of Korea in early 2014. Int J Infect Dis. 2015;33:12–14. doi: 10.1016/j.ijid.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Korea Centers Diseases Control and Prevention (KCDC) National Immunization Program. [Accessed Date October 30 2019]. Available at: https://nip.cdc.go.kr/irgd/index.html.
- 6.Jung J, Kim SK, Kwak SH, Hong MJ, Kim SH. Seroprevalence of Measles in Healthcare Workers in South Korea. Infect Chemother. 2019;51:58–61. doi: 10.3947/ic.2019.51.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korean Society of Infectious Diseases (KSID) The adult immunization schedule recommendation 2012 and 2017. [Accessed Date October 30 2019]. Available at: http://www.ksid.or.kr/data/sub07.html.
- 8.Kang HJ, Han YW, Kim SJ, Kim YJ, Kim AR, Kim JA, Jung HD, Eom HE, Park O, Kim SS. An increasing, potentially measles-susceptible population over time after vaccination in Korea. Vaccine. 2017;35:4126–4132. doi: 10.1016/j.vaccine.2017.06.058. [DOI] [PubMed] [Google Scholar]
- 9.Kim SK, Park HY, Kim SH. A third dose of measles vaccine is needed in young Korean health care workers. Vaccine. 2018;36:3888–3889. doi: 10.1016/j.vaccine.2017.11.077. [DOI] [PubMed] [Google Scholar]
- 10.Park JW, Yu SN, Park E, Lee Y, Park SM, Jeon MH. Modified measles in an anti-measles immunoglobulin G-negative healthcare worker who had received two doses of measles-containing vaccine. Infect Chemother. 2019;51:305–309. doi: 10.3947/ic.2019.51.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Advisory Committee on Immunization Practices; Centers for Disease Control and Prevention (CDC) Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–45. [PubMed] [Google Scholar]
- 12.Park B, Choi EJ, Park B, Han H, Cho SJ, Choi HJ, Lee S, Park H. Factors influencing vaccination in Korea: Findings from focus group interviews. J Prev Med Public Health. 2018;51:173–180. doi: 10.3961/jpmph.18.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eom H, Park Y, Kim J, Yang JS, Kang H, Kim K, Chun BC, Park O, Hong JI. Occurrence of measles in a country with elimination status: Amplifying measles infection in hospitalized children due to imported virus. PLoS One. 2018;13:e0188957. doi: 10.1371/journal.pone.0188957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang JH, Yoo JH. The Measles Strikes Back. J Korean Med Sci. 2019;34:e59. doi: 10.3346/jkms.2019.34.e59. [DOI] [PMC free article] [PubMed] [Google Scholar]