Abstract
Sepsis is a dysregulated systemic reaction to a common infection, that can cause life-threatening organ dysfunction. Over the last decade, the mortality rate of patients with sepsis has decreased as long as patients are treated according to the recommendations of the Surviving Sepsis Campaign, but is still unacceptably high. Patients at risk of sepsis should therefore be identified prior to the onset of organ dysfunction and this requires a rapid diagnosis and a prompt initiation of treatment. Unfortunately, there is no gold standard for the diagnosis of sepsis and traditional standard culture methods are time-consuming. Recently, in order to overcome these limitations, biomarkers which could help in predicting the diagnosis and prognosis of sepsis, as well as being useful for monitoring the response to treatments, have been identified. In addition, recent advances have led to the development of newly identified classes of biomarkers such as microRNAs, long-non-coding RNAs, and the human microbiome. This review focuses on the latest information on biomarkers that can be used to predict the diagnosis and prognosis of sepsis.
Keywords: Sepsis, Biomarkers, Diagnostic, Prognostic
Introduction
According to the third international consensus definition, sepsis is defined as a life-threatening organ dysfunction that occurs due to a dysregulated host response to infection. Septic shock is a subtype of sepsis that is clinically identified by a requirement for the administration of vasopressors to increase the mean arterial blood pressure to 65 mmHg or greater despite sufficient fluid resuscitation, or by an increase in serum lactic acid levels by 2 mmol/L or greater [1]. Sepsis is one of the most common causes of ICU hospitalization, and its frequency continues to increase. In a meta-analysis of 27 studies in high-income countries, the incidence rate of sepsis was found to be 288 cases per 100,000 person-years [2]. A multicenter cohort study in Korea reported that the incidence of sepsis in patients admitted to the emergency department was 1.5%, of which 36.5% were accompanied by septic shock [3]. Several studies have shown that mortality related to sepsis has been decreasing annually, but in low and middle-income countries there is still a high mortality rate that can be up to 80%. Sepsis treatment is the most expensive in the United States, resulting in more than 20 billion dollars each year. Patients at risk of sepsis should be identified prior to the onset of organ dysfunction and they require rapid diagnosis and onset of treatment. Unfortunately, there is no gold standard for the diagnosis of sepsis, and the sequential organ failure assessment (SOFA) score [4], recommended for assessing organ dysfunction in sepsis criteria-3 [1], runs the risk of premature recognition of the signs of a potentially fatal infection [5,6,7,8,9]. In addition, because traditional standard culture methods are time-consuming, accurate microbial diagnosis can be delayed. The development of sepsis biomarkers that can help in predicting the diagnosis and prognosis of sepsis and monitoring treatment responses is an ongoing process [10].
Sepsis begins with the activation of an innate immune response mediated by the detection of damage-associated molecular patterns (DAMPs) or pathogen-associated molecular patterns (PAMPs) by pattern-recognition receptors (PRRs) on host cells. In the activated innate immune response to sepsis, pro-inflammatory and anti-inflammatory mediators such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), interleukin-6 (IL-6) and monocyte chemoattractant protein 1 (MCP-1) are released, followed a rise in the levels of acute phase proteins such as procalcitonin, calprotectin, pro-adrenomedulin, pentraxin-3, and C-reactive protein (CRP). In addition, the serum levels of glycoproteins on cell membranes such as presepsin, soluble triggering receptor expressed on myeloid cell 1 (sTREM-1), and soluble urokinase plasminogen activator receptor (suPAR) may be increased, and the expression of CD64, an immunoglobulin receptor, may also be upregulated [11,12].
Many of these molecules have been proposed as sepsis biomarkers (Table 1). In particular, procalcitonin and CRP are already widely used as biomarkers for the prediction of diagnosis and the severity of sepsis [13,14]. MCP-1 is a soluble chemokine that is secreted by monocytes, endothelial cells, fibroblasts and other cells under pro-inflammatory conditions and initiates the inflammatory cascade allowing the recruitment of immune cells to the site of injury. The increase in the levels of MCP-1 in sepsis patients is correlated with organ dysfunction and may help to predict a poor prognosis (Table 2) [15]. sTREM-1, a soluble form of TREM-1, is expressed mainly on monocytes and neutrophils, and plays an important role in the inflammatory and cytotoxic response to sepsis including the synergic activation of Toll-like receptors and the increase of production of pro-inflammatory cytokines [16]. Several studies have demonstrated that the serum levels of sTREM-1 are a useful diagnostic biomarker for sepsis (Table 1) [17]. suPAR, a soluble form of uPAR, is expressed on immune cells such as neutrophils, lymphocytes, monocytes, and macrophages, as well as on endothelial cells, and is involved in a variety of immunological functions including cell migration, cell adhesion, angiogenesis, fibrinolysis, and cell proliferation [18]. Higher serum levels of suPAR are associated with a higher mortality (Table 2). suPAR levels are thought to have a limited diagnostic value, but a recent meta-analysis has reported that the area under the curve (AUC) of suPAR for predicting sepsis was as high as 0.83 [19]. CD64, a high-affinity Fcγ receptor I, is present at low levels on resting neutrophils, but its expression is up-regulated in the early stages of activation of the innate immune response. The CD64 index has been suggested to be a diagnostic marker of sepsis in several studies (Table 1) [20,21,22]. In addition to the biomarkers described above, various proteins, soluble receptors, cytokines, and chemokines, which are involved in the pathophysiology of sepsis, have been proposed and evaluated as novel biomarkers. Recent advances have also led to the development of newly identified classes of biomarkers such as microRNAs, long-non-coding RNAs, or the human microbiome. This review focuses on the latest information on biomarkers that can be used for predicting the diagnosis and prognosis of sepsis.
Table 1. Diagnostic markers of sepsis.
| Category | Biomarker | Ability to predict | Patients | Variables | AUC | 95% CI | Ref |
|---|---|---|---|---|---|---|---|
| Soluble receptors | Presepsin | Sepsis diagnosis | Sepsis [93] (n = 72), healthy controls or SIRS (n = 43) | Presepsin | 0.954 | 0.910 – 0.998 | [31] |
| PCT | 0.847 | 0.793 – 0.955 | |||||
| CRP | 0.859 | 0.782 – 0.936 | |||||
| Sepsis diagnosis | Sepsis [93] (n = 73), healthy controls or SIRS (n = 45) | Presepsin | 0.937 | [30] | |||
| PCT | 0.915 | ||||||
| hs-CRP | 0.853 | ||||||
| IL-6 | 0.869 | ||||||
| sTREM-1 | Differentiation between SIRS and sepsis | Sepsis [93] (n = 52), SIRS (n = 38) | sTREM-1 | 0.78 | 0.69 – 0.86 | [94] | |
| PCT | 0.65 | 0.53 – 0.76 | |||||
| APACHE II | 0.71 | 0.60 – 0.81 | |||||
| Septic shock diagnosis | Septic shock [95] (n = 60), healthy controls (n = 30) | sTREM-1 | 0.955 | [96] | |||
| PCT | 0.844 | ||||||
| CRP | 0.791 | ||||||
| IL-6 | 0.898 | ||||||
| suPAR | Sepsis diagnosis | Sepsis [95] (n = 40), healthy controls (n = 40) | suPAR | 0.99 | 0.93 – 1.00 | [18] | |
| Lactate | 0.84 | 0.74 – 0.91 | |||||
| Membrane receptors | CD64 | Sepsis diagnosis | Sepsis [1] (n = 151), healthy controls (n = 20) | CD64 | 0.879 | 0.795 – 0.962 | [20] |
| PCT | 0.868 | 0.795 – 0.962 | |||||
| CRP | 0.609 | 0.491 – 0.727 | |||||
| SOFA | 0.701 | 0.579 – 0.874 | |||||
| DAMP | Calprotectin | Sepsis diagnosis | Sepsis [1] (n = 77), non-sepsis (n = 194) | CaPT | 0.67 | [42] | |
| PCT | 0.55 | ||||||
| Sepsis diagnosis | Sepsis [1] (n = 300), healthy controls (n = 53) | CaPT | 0.901 | 0.852 – 0.942 | [44] | ||
| CC chemokine ligand 2 | MCP-1 | Septic shock diagnosis | Sepsis [1] (n = 43), healthy controls (n = 25) | MCP-1 | 0.716 | 0.564 – 0.868 | [15] |
| PTX-3 | 0.798 | 0.666 – 0.921 | |||||
| Angpt-1 | 0.501 | 0.320 – 0.683 | |||||
| Angpt-2 | 0.631 | 0.464 – 0.799 | |||||
| Acute phase protein | PTX-3 | Septic diagnosis | Sepsis [1] (n = 213), healthy controls (n = 77) | PTX-3 | 0.92 | 0.87 – 0.97 | [38] |
| PCT | 0.92 | 0.88 – 0.97 | |||||
| CRP | 0.82 | 0.72 – 0.91 | |||||
| IL-6 | 0.91 | 0.86 – 0.95 | |||||
| MR-proADM | Septic diagnosis | Sepsis [1] (n = 109), healthy controls (n = 50) | MR-proADM | 0.817 | 0.733 – 0.884 | [97] | |
| PCT | 0.884 | 0.810 – 0.937 | |||||
| SOFA | 0.774 | 0.685 – 0.847 | |||||
| qSOFA | 0.827 | 0.744 – 0.892 | |||||
| miRNA | miR-125a | Sepsis diagnosis | Sepsis [1] (n = 150), healthy controls (n = 150) | miR-125a | 0.749 | 0.695 – 0.803 | [74] |
| miR-125b | miR-125b | 0.839 | 0.795 – 0.882 | ||||
| Non-coding RNAs | Lnc-MALAT1 | Sepsis diagnosis | Sepsis [1] (n = 120), healthy (n = 60) | LncMALAT1 | 0.910 | 0.867 – 0.953 | [79] |
| PCT | 0.928 | 0.867 – 0.964 | |||||
| Septic shock diagnosis | LncMALAT1 | 0.836 | 0.757 – 0.916 | ||||
| Lactate | 0.830 | 0.758 – 0.902 | |||||
| SOFA | 0.908 | 0.856 – 0.960 | |||||
| APACHE II | 0.856 | 0.791 – 0.922 | |||||
| Lnc-MEG3 | Sepsis diagnosis | Sepsis [1] (n = 219), healthy (n = 219) | LncMEG3 | 0.887 | 0.856 – 0.917 | [84] | |
| LncMEG3/miR-21 | 0.934 | 0.909 – 0.958 | |||||
| Reduced sepsis risk | miR-21 | 0.801 | 0.758 – 0.844 |
AUC, area under the curve; CI, confidence interval; Ref, reference; SIRS, systemic inflammatory response syndrome; PCT, procalcitonin; CRP, C-reactive protein; hs-CRP, high sensitivity C-reactive protein; IL, interleukin; sTREM-1, soluble triggering receptor expressed on myeloid cell 1; APACHE II, acute physiology and chronic health evaluation II; suPAR, soluble urokinase plasminogen activator receptor; SOFA, sequential organ failure assessment; DAMP, damage-associated molecular pattern; CaPT, calprotectin; MCP-1, monocyte chemoattractant protein 1; PTX-3, pentraxin-3; Angpt, angiopoietin; MR-proADM, mid-regional fragment of pro-adrenomedullin; ADM, adrenomedullin; Lnc, long non-coding; MALAT, metastasis-associated lung adenocarcinoma transcript; MEG, maternally expressed gene.
Table 2. Prognostic biomarkers of sepsis.
| Category | Biomarker | Ability to predict | Patients | Variables | AUC | 95% CI | Ref |
|---|---|---|---|---|---|---|---|
| Soluble receptors | suPAR | 28-day mortality | Sepsis [95] (n = 130) | suPAR | 0.77 | 0.68 – 0.86 | [98] |
| Lactate | 0.70 | 0.59 – 0.80 | |||||
| CC chemokine ligand 2 | MCP-1 | 30-day mortality | Sepsis [1] (n = 136) | MCP-1 | 0.64 | 0.55 – 0.74 | [99] |
| PCT | 0.57 | 0.47 – 0.68 | |||||
| CRP | 0.51 | 0.40 – 0.62 | |||||
| IL-6 | 0.69 | 0.59 – 0.78 | |||||
| SOFA | 0.67 | 0.57 – 0.77 | |||||
| qSOFA | 0.63 | 0.48 – 0.78 | |||||
| APACHE II | 0.74 | 0.65 – 0.83 | |||||
| Acute phase protein | PTX-3 | 28-day mortality | Sepsis [1] (n = 83) | PTX-3 | 0.82 | 0.68 – 0.96 | [100] |
| PCT | 0.64 | 0.50 – 0.77 | |||||
| CRP | 0.56 | 0.40 – 0.73 | |||||
| APACHE II | 0.77 | 0.59 – 0.94 | |||||
| SOFA | 0.59 | 0.40 – 0.79 | |||||
| MR-proADM | 28-day mortality | Sepsis [1] (n = 326) | MR-proADM | 0.79 | 0.74 – 0.84 | [59] | |
| Lactate | 0.71 | 0.64 – 0.77 | |||||
| PCT | 0.61 | 0.55 – 0.68 | |||||
| CRP | 0.54 | 0.47 – 0.61 | |||||
| SOFA | 0.75 | 0.69 – 0.80 | |||||
| ADM | 30-day mortality | Sepsis [1] (n = 215) | Bio-ADM | 0.827 | 0.770 – 0.875 | [64] | |
| SOFA | 0.830 | 0.774 – 0.878 | |||||
| Angiogenic growth factor | Angiopoietin | 28-day mortality | Sepsis [1] (n = 145) | Angpt-2/1 | 0.736 | 0.649 – 0.823 | [90] |
| SOFA | 0.745 | 0.655 – 0.836 | |||||
| 28-day mortality | Sepsis [95] (n = 333), control (n = 55) | Angpt-2/1 | 0.845 | 0.810 – 0.880 | [91] | ||
| PCT | 0.732 | 0.685 – 0.780 | |||||
| MEDS score | 0.826 | 0.785 – 0.866 | |||||
| Non-coding RNAs | miRNA | 28-day mortality | Sepsis [93] (n = 214) | miR-223 | 0.748 | P <0.001 | [71] |
| miR-15a | 0.610 | P = 0.015 | |||||
| miR-16 | 0.760 | P <0.001 | |||||
| miR-122 | 0.744 | P <0.001 | |||||
| miR-193b | 0.790 | P <0.001 | |||||
| miR-483-5p | 0.657 | P <0.001 | |||||
| Lnc-NEAT1 | 28-day mortality | Sepsis [93] (n = 82), healthy (n = 82) | Lnc-NEAT1 | 0.726 | 0.615 – 0.837 | [79] | |
| miR-124 | miR-124 | 0.784 | 0.668 – 0.900 | ||||
| Lnc-NEAT1/miR-124 axis | 0.830 | 0.738 – 0.922 | |||||
| Lnc-MALAT1 | Mortality | Sepsis [1] (n = 120), healthy controls (n = 60) | Lnc-MALAT1 | 0.886 | 0.819 – 0.954 | [83] | |
| Lactate | 0.868 | 0.800 – 0.937 | |||||
| SOFA | 0.943 | 0.905 – 0.981 | |||||
| APACHE II | 0.856 | 0.802 – 0.934 | |||||
| Lnc-MEG3 | 28-day mortality | Sepsis [1] (n = 219), healthy (n = 219) | Lnc-MEG3 | 0.704 | 0.626 – 0.783 | [84] | |
| APACHE II | 0.793 | 0.729 – 0.857 | |||||
| SOFA | 0.758 | 0.687 – 0.830 |
AUC, area under the curve; CI, confidence interval; Ref, reference; suPAR, soluble urokinase plasminogen activator receptor; MCP-1, monocyte chemoattractant protein 1; PCT, procalcitonin; CRP, C-reactive protein; IL, interleukin; SOFA, sequential organ failure assessment; APACHE II, acute physiology and chronic health evaluation II; PTX-3, pentraxin-3; MR-proADM, mid-regional fragment of pro-adrenomedullin; ADM, adrenomedullin; Angpt, angiopoietin; MEDS, mortality in emergency department sepsis; NEAT, nuclear enriched abundant transcript; MALAT, metastasis-associated lung adenocarcinoma transcript; MEG, maternally expressed gene.
Diagnostic biomarkers
1. Presepsin
CD14 is a glycoprotein that is expressed on the surface of immune cells, such as monocytes and macrophages that acts as a receptor for lipopolysaccharide (LPS). During the pro-inflammatory signaling cascade that occurs following contact with infectious agents, the N-terminus of CD14 is cleaved and is secreted into circulation as soluble CD14 subtypes, one of which has been identified as the 13 kDa glycopeptide, presepsin (PSEP). The physiological role of presepsin is thought to be related to bacterial phagocytosis and lysosomal cleavage of microorganisms, but it is not yet fully understood. In the immune response to sepsis, the serum levels of presepsin are elevated before procalcitonin or IL-6, so it has been proposed as a potential biomarker for the diagnosis of sepsis [11,23,24,25], and several meta-analysis studies have demonstrated that presepsin is useful as a diagnostic marker for sepsis [26,27,28]. Presepsin is one of the receptors for lipopolysaccharides found in the cell walls of gram-negative bacteria, and a prospective study has reported that an increase in presepsin levels is associated with the bacteremia status of SIRS patients admitted to the emergency department (Table 1) [29]. A prospective study in Korea reported that presepsin levels were significantly increased following patient infection compared to non-infected patients and AUC of presepsin for predicting a diagnosis of sepsis was higher (0.937) than procalcitonin (0.915), IL-6 (0.869), or high-sensitivity-CRP (0.853) [30]. In addition, Lu et al. reported significant differences in presepsin levels between gram-positive and gram-negative bacterial infections [31]. The diagnostic value of presepsin has been confirmed in several studies, but its prognostic value is controversial [11,25,30,32]. However, a recent prospective study has reported that both the serum levels of presepsin and the presepsin clearance ratio in patients with severe sepsis are correlated with the SOFA score. In addition, there was a significant difference in the levels of presepsin in sepsis patients between survival and non-survival groups, and that presepsin was better than procalcitonin as a biomarker to assess sepsis prognosis and therapeutic effect [33]. Presepsin is therefore considered a good biomarker for the diagnosis of sepsis and for the differential detection of bacterial infections, but further in-depth analysis of its prognostic value is required.
2. Pentraxin-3
Pentraxins (PTX) are a type of soluble pattern recognition molecules (PRMs), which are divided into short and long pentraxins depending on the length of the N-terminal region. C-reactive protein (CRP) and serum amyloid P belong to the short pentraxins, while PTX-3, PTX-4, neuronal pentraxin 1 (NP1), and NP2 belong to the long pentraxins. Short pentraxins are secreted from hepatocytes in response to pro-inflammatory cytokines such as IL-6. CRP, one of the short pentraxins, levels are low in healthy adults (below 3 mg/L), but levels can increase by about 1000-fold within 48 hours during an inflammatory response. PTX-3, a member of the long pentraxin subfamily, is released from monocytes, dendritic cells and macrophages, epithelial cells, vascular endothelial cells, and smooth muscle cells after stimulation by toll-like receptor agonists, microbial moieties such as lipopolysaccharides, or inflammatory cytokines. Circulating PTX-3 modulates complement activity, cell extravasation, and pathogen recognition by myeloid cells, and contributes to resistance to microorganisms through the generation of an antimicrobial microenvironment, and plays a variety of roles in different conditions such as in cardiovascular disease, wound healing, and cancer [34,35]. Several studies have shown that PTX-3 has a good diagnostic value for sepsis. A recent prospective study of 101 patients compared sepsis and healthy groups by measuring plasma PTX-3, MCP-1, and angiopoietin (Angpt)-2 levels on the first day of sepsis onset. All of these biomarkers were significantly increased in the sepsis group compared to the healthy group, and PTX-3 had the highest AUC of 0.798 [95% confidence interval (CI) 0.666 – 0.921, P <0.0001] for predicting septic shock [15]. In a prospective controlled study of 213 ICU patients, PTX-3, procalcitonin, and IL-6 were measured on day 1, 3, and 8 of hospitalization in sepsis patients. On each day, the diagnostic AUCs for sepsis were similarly high for PTX-3 (AUC 0.92, 95% CI 0.87 – 0.97), IL-6 (AUC 0.91, 95% CI 0.86 – 0.95) and procalcitonin (AUC 0.92, 95% CI 0.88 – 0.97), and PTX-3 was also significantly correlated with the degree of organ dysfunctions as evaluated by SOFA, APACHE (acute physiology and chronic health evaluation) II [36], and PTX-3 was also significantly correlated with the degree of organ dysfunctions as evaluated by SOFA, APACHE (acute physiology and chronic health evaluation) II and SAPS (simplified acute physiology score) II [37,38]. PTX-3 has also been evaluated as a prognostic marker of sepsis. A recent meta-analysis showed that elevated PTX-3 levels were correlated with an increase of the risk of all-cause mortality (hazard ratio 1.91, 95% CI 1.53 – 2.46, P <0.0001). However, in this study, the cut-off values could not be shown due to the high heterogeneity among the studies [39]. A recent prospective study of 245 sepsis patients identified according to sepsis criteria-3 [1] reported that the AUC for predicting 28-day mortality for PTX-3 was 0.78 (95% CI 0.65 – 0.81), higher than for procalcitonin (AUC 0.73, 95% CI 0.65 – 0.81) or lactate (AUC 0.67, 95% CI 0.59 – 0.75), and the cut-off value for PTX-3 was found to be 49.9 ng/mL. However, the specificity of this cut-off value of PTX-3 was limited to 64.2%. This limit was improved by a new sepsis score, PPL, combining these three biomarkers (AUC 0.90, 95% CI 0.83 – 0.94) [40]. The ability of PTX-3 to predict mortality may be improved by combining with other biomarkers and further evaluation of the most appropriate model is still needed.
3. Calprotectin
Calprotectin is a heterodimeric calcium-binding protein composed of calgranulin A (S100A8) and calgranulin B (S100A9) subunits. They are expressed in a variety of cells, especially in the cytosol of myeloid cells. Calprotectin is released from activated cells, following binding to cell surface receptors such as the receptor for advanced glycation end products (RAGE), toll-like receptor 4 (TLR4), and the extracellular matrix metalloprotease inducer (EMMPRIN), it participates in inflammatory processes through signaling pathways such as the mitogen-activated protein kinase (MAPK) pathway, the NF-κB pathway, the phosphoinositide 3 kinase (PI3K) pathway, as well as Ras homologous-GTPases (Rho-GTPases). In addition, it plays an important role in various cellular processes such as cell cycle progression, proliferation, differentiation, and cell survival, and is involved in the regulation of calcium homeostasis, zinc and manganese chelation, cytoskeletal rearrangement, cell migration, and the inhibition of microbial growth [41]. Several studies have evaluated the diagnostic value of serum calprotectin levels in sepsis patients (Table 1) [42,43]. A prospective study of 125 patients demonstrated that the calprotectin AUC for predicting sepsis was as high as 0.901 (95% CI 0.852 – 0.942) and the sensitivity and specificity at the cut-off value of 3128.8 ng/mL were 83.1% and 88.5%, respectively [44]. An increase in serum calprotectin levels has also been reported to be associated with bacterial infections. A prospective observational single-center study showed a significant difference in the serum levels of calprotectin between bacterially and virally infected groups among sepsis patients, and the AUC value of calprotectin (AUC 90.97) was higher than that of procalcitonin (88.19) [45]. A cohort study of critically ill patients reported that the diagnostic accuracy of serum calprotectin for bacterial infection (AUC 0.76, 95% CI 0.65 – 0.86) was higher than procalcitonin (AUC 0.63, 95% CI 0.49 – 0.77) and CRP (AUC 0.69, 95% CI 0.60 – 0.81)[46]. Havelka et al. also demonstrated that calprotectin (AUC 0.775, 95% CI 0.667 – 0.861) was superior to procalcitonin (AUC 0.736, 95% CI 0.625 – 0.829) as a biomarker for differentiating bacterial pneumonia from viral pneumonia [47]. Therefore, in several studies, calprotectin has been identified as a specific marker for bacterial infection. Further evaluation will be needed to address the clinical use of calprotectin to guide the initiation and de-escalation of antibiotic therapies in sepsis patients.
4. Intestinal microbiota
The intestinal microflora is a complex community of microorganisms that exist along the gastrointestinal tract, and the intestine is the most densely and heterogeneously occupied with microorganisms among all body sites. The intestinal microbiota plays important roles in human energy homeostasis, regulates intestinal endocrine function, and acts as a bio-factory for the synthesis of vitamins and cofactors. The intestinal microbiota is also crucial in the development and maturation of the immune system and plays a protective role against pathogens through actions such as competition for shared nutrients, generation of anti-microbial compounds, or resistance to colonization [48]. In addition, it is involved in the pathophysiological processes of various diseases such as diabetes, liver cirrhosis, cancer, and atherosclerosis, and is considered to be a powerful biomarker for the development and progression of these diseases. Several studies have shown that the integrity in the intestinal microbiota is severely affected by sepsis, but may also affect the development and progression of sepsis and the development of organ failure [49]. Liu et al. reported that the intestinal microbiota was disrupted in sepsis patients and that the intestinal microbial metabolite profiles of sepsis patients were completely altered compared to healthy people. In addition, there was an induction of intestinal dysbiosis in mice that had been transplanted with feces from sepsis patients and an there was an exacerbation of sepsis-induced liver injury confirmed in these septic-feces recipient mice, which suggests that intestinal dysbiosis is associated with susceptibility to sepsis [50]. Several studies have shown that intestinal microbial diversity in patients with sepsis is reduced compared to healthy people, and that a decrease in intestinal microbial diversity is associated with an increase in mortality in sepsis patients [51,52]. In a recent study, it was found that the microbiota in sepsis patients is rich in microorganisms that are highly related to inflammation, such as Parabacteroides, Fusobacterium, and Bilophylloma. In particular, the abundance of enterococcus species was increased in non-survivors among sepsis patients, and the enterococcus species was proposed as a potential prognostic biomarkers of sepsis [53]. However, a recent prospective cohort study on 150 patients with septic shock demonstrated that a low microbial diversity was not correlated with an increase in the mortality rate [54]. Disruption of the intestinal microbiota can occur not only in sepsis, but also in response to a variety of other factors, such as changes in antibiotic therapy, hospitalization, and changes in diet. Therefore, the causal mechanism of sepsis-associated disturbances of the microbiota is currently not understood [49,53,55]. Furthers studies are required in order to understand sepsis-associated dysbiosis, which could lead to the development of biomarkers and microbiota-targeted therapies for the treatment of sepsis.
Prognostic biomarkers
1. Adrenomedullin and the mid-regional fragment of pro-adrenomedullin
Adrenomedullin (ADM) is a 52-amino acid peptide that is produced mainly in endothelial cells and vascular smooth muscle cells and is secreted by various organs and tissues. It is one of the important mediators of vasodilation and is involved in the regulation of systemic circulation as an autocrine/paracrine vasoactivator. It is also known to play an important role in the progression of the inflammatory response, sepsis, and septic shock. Circulating ADM is quickly degraded and cleared from circulation and is difficult to detect by a standard immunoassay due to the masking effect of its binding protein (complement factor H). The mid-regional fragment of pro-adrenomedullin (MR-proADM), comprised of amino acids 45–92, is more stable than the ADM peptide, and its levels directly reflect the levels of the active ADM peptide [56,57]. MR-proADM has been identified in several studies as a prognostic marker for the prediction of mortality in sepsis and septic shock patients (Table 2) [57,58,59]. A prospective observational study has been conducted to evaluate the relationship between MR-proADM and severity scores, such as the SOFA score, the Pitt [60] score, and the Clinical Pulmonary Infection Score (CPIS) [61], using linear-mixed effects models. As a result, MR-proADM levels were able to predict sepsis-related organ dysfunction 24 hours before onset. This predictive role can be considered as being equivalent to a diagnostic marker for sepsis [56]. Recently, a double monoclonal sandwich immunoassay has been developed that is able to measure C-terminally amidated biologically active ADM (bio-ADM) [62,63]. A prospective study at a single center in Korea measured bio-ADM levels in 215 patients diagnosed with sepsis and septic shock. The levels of bio-ADM in the septic shock group were significantly higher than in the sepsis group (110.3 vs. 45.3 pg/mL, P <0.0001), and there was a significant difference between the levels of bio-ADM in the non-survivor and survival groups (137.8 vs. 55.3 pg/mL, P <0.0001). The levels of bio-ADM also predicted 30-day mortality similar to the SOFA score (AUC 0.827 vs. 0.830) [64]. The AdrenOSS-1 study has also demonstrated that the level of bio-ADM was higher in septic shock patients than in sepsis patients. In addition, the rapid recovery of bio-ADM levels to normal values (<70 pg/mL), measured at 48 hours after admission, was correlated with a decrease in 28-day mortality and an improvement in cardiovascular function [65]. MR-proADM has been used as a surrogate for ADM due to methodological difficulties in measuring ADM levels, such as the requirement for large sample volumes, but there is a gap between the two in terms of their functionality and clearance kinetics. Since the recent development of the double monoclonal sandwich immunoassay enabling bio-ADM measurements, further evaluation, including validation of the optimal cut off, will be required for the clinical use of bio-ADM as a sepsis biomarker.
2. Non-coding RNAs
1) MicroRNA
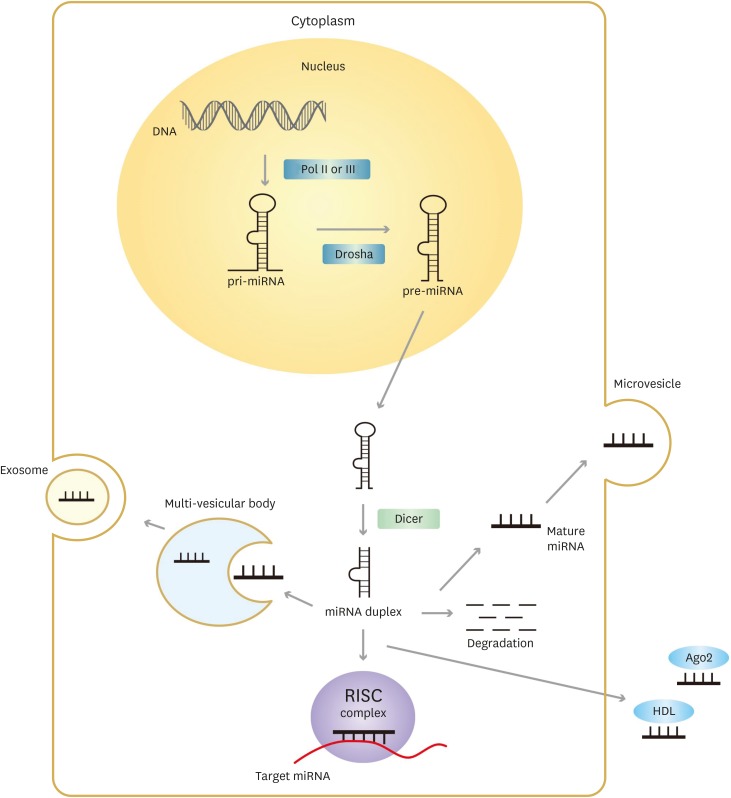
MicroRNAs (miRNAs) are one of a number of small non-coding RNAs. They are comprised of 20 to 24 nucleotides, accounting for about 1% of the human genome, but regulate up to 50% of all human protein-coding genes. The biogenesis of miRNAs begins with the synthesis of primary (pri)-miRNA transcripts by RNA polymerase II or III in the nucleus. The pri-miRNA is processed by Drosha into a pre-miRNA, a hairpin-like structure of approximately 70 nucleotides, and then transported to the cytoplasm. The pre-miRNA in turn is matured into miRNA double strands through processing by Dicer, a ribonuclease (RNAse) III, present in the cytoplasm. One of the strands, usually known as the guide strand, is integrated into the RNA-induced silencing complex (RISC) to regulate the expression of target mRNAs. The other one, known as the passenger strand, is degraded in the cell or released from the parent cell through tissue damage, apoptosis, and necrosis, through binding to proteins such as Ago2 protein or high-density lipoprotein, or through microvesicles and exosomes (Fig.1) [66,67]. Most mRNAs are unstable due to the excessive pH and temperature conditions in circulation, but miRNAs can be protected against degradation by lipoproteins and RNA-binding protein complexes or by being transported within exosomes and microvesicles. miRNAs are stable in a variety of body fluids and are specific to tissues orcell types, and can be readily measured in a variety of ways, including by polymerase chain reaction (PCR) and microarray. miRNAs are therefore being investigated for their potential as biomarkers in many different diseases, including cancer, neurologic disorders, cardiovascular diseases, and inflammatory diseases [68]. miRNAs are known to regulate a variety of pathways involved in the pathophysiology of sepsis, such as TLR4-mediated or pro-inflammatory cytokines-mediated pathways [69]. Vasilescu et al. have demonstrated that the expression level of miR-150 correlates with the expression levels of major immune response genes such as TNF-alpha, IL-10, and IL-18, and has suggested the potential of miR-150 as a prognostic marker in sepsis patients (Table 2) [70]. In a prospective observational study, six miRNAs, namely miR-193b, miR-223, miR-15a, miR-16, miR-122, and miR-483-5p, were identified as prognostic markers in patients with sepsis. In particular, the AUC and multivariate odds ratio of miR-193b for the 28-day mortality rate of sepsis patients were high, being 0.790 (P <0.001) and 9.07 (95% CI 1.32 – 62.42), respectively, suggesting the possibility of it being a prognostic marker for sepsis [71]. In addition, several recent studies have demonstrated the potential of the miR-125 family as a sepsis biomarker, which has previously been reported to be associated with inflammatory responses and organ injuries [72,73]. The AUCs of miR-125a and miR-125b for predicting sepsis were 0.749 (95% CI 0.695 – 0.803) and 0.839 (95% CI 0.795 – 0.882), respectively, and the AUC of miR-125b for predicting 28-day mortality was 0.699 (95% CI 0.603 – 0.795), similar to the SOFA score (AUC 0.739, 95% CI 0.655 – 0.823) or the APACHE II score (AUC 0.755, 95% CI 0.675 – 0.836) [74].
Figure 1. The biogenesis of microRNA.
Pol, polymerase; miRNA, MicroRNAs; HDL, high-density lipoprotein; Ago2, argonaute 2; RISC, RNA-induced silencing complex.
2) Long non-coding RNAs
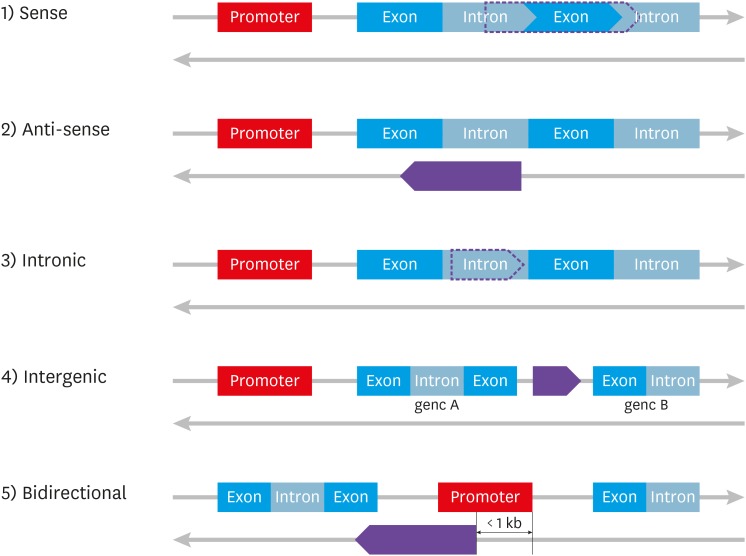
Long non-coding RNAs (lncRNAs) are a class of non-coding RNAs with transcripts of more than 200 nucleotides that lack an open reading frame. Most lncRNAs, like mRNAs, are usually transcribed by RNA polymerase II, 5'-capped, 3'-polyadenylated, and spliced. They can be classified into five different types namely, sense, antisense, intronic, intergenic, bidirectional, antisense, according to their relative position with protein coding genes (Fig. 2), and serve as decoys, scaffolds, guides, and enhancers to regulate gene expression [75]. Several studies have reported that various lncRNAs are involved in the innate and adaptive immune responses [76]. LncRNA nuclear enriched abundant transcript 1 (NEAT1) is an important component of the paraspeckle structure in nuclear bodies [77]. It is known to regulate the expression of genes involved in antiviral responses, such as IL-8, and to play an important role in the innate immune response [78]. Several studies have shown that the increase of lnc-NEAT1 levels in sepsis patients was positively correlated with APACHE II and SOFA scores (Table 1) and associated with an unfavorable prognosis (Table 2) [79,80]. LncRNA metastasis-associated lung adenocarcinoma transcript 1 (MALAT1), also known as lnc-NEAT2, is a prognostic marker for non-small cell lung cancer. It is also known to play an important role in regulating neural development, skeletal myogenesis, and vascular growth [81]. Zhao et. al. demonstrated that lnc-MALAT1 regulates the LPS-stimulated expression of the pro-inflammatory cytokines, TNFα and IL-6, through inhibition of NF-κB activity [82]. A prospective cohort study of 120 sepsis patients showed that lnc-MALAT1 had diagnostic value, with an AUC of 0.910 for sepsis, and also had a higher prognostic value (AUC 0.886) than the APACHE II score (AUC 0.868) and lactate levels (AUC 0.868) when comparing non-survival and survival groups [83]. As another lncRNA, long non-coding RNA maternally expressed gene 3 (lnc-MEG3) levels have been reported to be positively correlated with inflammatory responses and organ damage. It acts as a molecular sponge for several microRNAs such as miR-21, miR-181a, and miR-7-5p [84,85]. Among its target miRNAs, miR-21 is known to act as an important contributor to inflammatory responses and organ dysfunction in organs such as the liver, kidney, and lung in sepsis [84,85,86]. In a recent study of 219 sepsis patients and 219 healthy controls, lnc-MEG3 and miR-21 levels in plasma samples obtained within 24 hours after admission showed good predictive values for sepsis diagnosis (Table 1) and prognosis (Table 2) [84]. Although many non-coding RNAs associated with inflammatory diseases, including sepsis, have been identified, their functions and mechanisms are not well known and are controversial. Therefore, a further evaluation, including the roles of non-coding RNAs in the pathogenesis of sepsis and the development of an optimal normalization strategy for the analysis of the levels non-coding RNAs will be needed in the future.
Figure 2. LncRNA classification by genomic location relative to protein coding genes.
3. Angiopoietin
Angiopoietins (Angpts) represent one member of the family of angiogenic growth factors that are secreted by vascular endothelial cells under stress conditions such as in inflammation. Angpt-1 and Angpt-2 are ligands for the endothelial cell-specific Tie2 receptor, with both having a similar affinity for the Tie2 receptor and likely have the same binding site since they can compete with each other for binding. Activation of the Tie2 receptor by its ligands is involved in vessel stability and endothelial barrier function acting through activation of PI3K/Akt signaling cascade, and in anti-adhesive and anti-inflammatory effects acting through the inhibition of NF-κB. However, Angpt-2 can antagonize Angpt-1 during an inflammatory response such as sepsis [87,88]. The increase in the levels of Angpt-2 and the Angpt-2/1 ratio in sepsis patients have been reported to be associated with a poor prognosis. In a retrospective cohort study of 145 ICU patients in Korea, the 28-day mortality of sepsis patients was positively associated with Angpt-2 levels and negatively associated with Angpt-1 levels. The Angpt-2/1 ratio in non-survivors was significantly higher than that in survivors and the AUC of the Angpt-2/1 levels for predicting 28-day mortality was 0.736 (95% CI 0.649 – 0.823), which was not significantly different from the SOFA score of 0.745 (95% CI 0.655 – 0.836) [89,90]. Fang et al. have reported that the Angpt-2/1 ratio was also valuable for predicting the prognosis of patients with sepsis in the emergency department [91]. Several studies have reported that the Angpt/Tie2 pathway is also modulated by microRNAs. Zhang et al. demonstrated that microRNA-204/211 in the EA.hy926 endothelial cell line binds to the Angpt-1 3'-untranslated region (UTR) to regulate the expression of Angpt-1 [92]. In a preclinical study, treatment with Angpt-2 neutralizing antibodies or an Angpt-2 targeted short interfering RNA in mouse models of sepsis or acute lung injury decreased mortality rate and the incidence of multiple-organ dysfunction syndrome through Angpt-2 inhibition or stimulation of anpgt-1/Tie2 axis [88]. In the future, we expect the development of angiopoietin as a biomarker for predicting the diagnosis and prognosis of sepsis, but also the development of therapies for sepsis that target angiopoietin.
Conclusion
Sepsis is a life-threatening disease and is one of the most common causes of ICU inpatients. Early diagnosis and proper management are necessary to reduce the mortality of sepsis. However, the individual difference in the physiological response to infection is large, and the signs and symptoms of sepsis are non-specific, making early diagnosis difficult. Therefore, a number of potential biomarkers for the diagnosis of sepsis have been developed. These molecules are mainly involved in the initial pathogenesis of the innate immune response to infection, and in many cases, they show prognostic value as well as diagnostic value. The prognostic markers of sepsis are often involved in the organ dysfunction caused by sepsis and the development of therapeutic agents for sepsis targeting these prognostic biomarkers is being attempted. In addition, recent advances in technology have led to the development of new types of biomarkers such as the microbiome and non-coding RNAs. The intestinal microbiome is known to play an important role in the development and maturation of the immune system and protection against pathogens. Therefore, gut dysbiosis is considered to be a powerful biomarker for the development and progression of sepsis. Non-coding RNAs including miRNAs and long non-coding RNAs regulate gene expression in various ways, but their function and mechanisms in the pathogenesis of sepsis are not completely understood. Further evaluation, including the roles of these new biomarkers in the pathogenesis of sepsis and the development of an optimal normalization strategy for the analysis of these new biomarkers will be needed for their future clinical use.
Footnotes
Conflict of Interest: No conflicts of interest.
- Conceptualization: MHK, JHC.
- Data curation: MHK, JHC.
- Formal analysis: MHK, JHC.
- Funding acquisition: JHC.
- Investigation: MHK, JHC.
- Methodology: MHK, JHC.
- Project administration: MHK, JHC.
- Resources: MHK, JHC.
- Software: MHK, JHC.
- Supervision: JHC.
- Validation: MHK, JHC.
- Visualization: MHK, JHC.
- Writing - original draft: MHK, JHC.
- Writing - review & editing: MHK, JHC.
References
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K International Forum of Acute Care Trialists. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193:259–272. doi: 10.1164/rccm.201504-0781OC. [DOI] [PubMed] [Google Scholar]
- 3.Jeon K, Na SJ, Oh DK, Park S, Choi EY, Kim SC, Seong GM, Heo J, Chang Y, Kwack WG, Kang BJ, Choi WI, Kim KC, Park SY, Kwak SH, Shin YM, Lee HB, Park SH, Cho JH, Kim B, Lim CM Korean Sepsis Alliance (KSA) study group. Characteristics, management and clinical outcomes of patients with sepsis: a multicenter cohort study in Korea. Acute Crit Care. 2019;34:179–191. doi: 10.4266/acc.2019.00514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 5.Arefian H, Heublein S, Scherag A, Brunkhorst FM, Younis MZ, Moerer O, Fischer D, Hartmann M. Hospital-related cost of sepsis: a systematic review. J Infect. 2017;74:107–117. doi: 10.1016/j.jinf.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, Kadri SS, Angus DC, Danner RL, Fiore AE, Jernigan JA, Martin GS, Septimus E, Warren DK, Karcz A, Chan C, Menchaca JT, Wang R, Gruber S, Klompas M CDC Prevention Epicenter Program. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009-2014. JAMA. 2017;318:1241–1249. doi: 10.1001/jama.2017.13836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esposito S, De Simone G, Boccia G, De Caro F, Pagliano P. Sepsis and septic shock: New definitions, new diagnostic and therapeutic approaches. J Glob Antimicrob Resist. 2017;10:204–212. doi: 10.1016/j.jgar.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO) WHO recommended surveillance standards. 2nd ed. 2004. [Accessed July 21, 2013]. pp. 123–124. Available at: http://www.who.int/csr/resources/publications/surveillance/whocdscsrisr992.pdf.
- 9.Jeon JH, Park DW. Controversies regarding the new definition of sepsis. Korean J Med. 2017;92:342–348. [Google Scholar]
- 10.Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- 11.Larsen FF, Petersen JA. Novel biomarkers for sepsis: A narrative review. Eur J Intern Med. 2017;45:46–50. doi: 10.1016/j.ejim.2017.09.030. [DOI] [PubMed] [Google Scholar]
- 12.Faix JD. Biomarkers of sepsis. Crit Rev Clin Lab Sci. 2013;50:23–36. doi: 10.3109/10408363.2013.764490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cho SY, Choi JH. Biomarkers of sepsis. Infect Chemother. 2014;46:1–12. doi: 10.3947/ic.2014.46.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.So-Ngern A, Leelasupasri S, Chulavatnatol S, Pummangura C, Bunupuradah P, Montakantikul P. Prognostic value of Serum Procalcitonin level for the diagnosis of bacterial infections in critically-ill patients. Infect Chemother. 2019;51:263–273. doi: 10.3947/ic.2019.51.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian R, Wang X, Pan T, Li R, Wang J, Liu Z, Chen E, Mao E, Tan R, Chen Y, Liu J, Qu H. Plasma PTX3, MCP1 and Ang2 are early biomarkers to evaluate the severity of sepsis and septic shock. Scand J Immunol. 2019;90:e12823. doi: 10.1111/sji.12823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bleharski JR, Kiessler V, Buonsanti C, Sieling PA, Stenger S, Colonna M, Modlin RL. A role for triggering receptor expressed on myeloid cells-1 in host defense during the early-induced and adaptive phases of the immune response. J Immunol. 2003;170:3812–3818. doi: 10.4049/jimmunol.170.7.3812. [DOI] [PubMed] [Google Scholar]
- 17.Gómez-Piña V, Soares-Schanoski A, Rodríguez-Rojas A, Del Fresno C, García F, Vallejo-Cremades MT, Fernández-Ruiz I, Arnalich F, Fuentes-Prior P, López-Collazo E. Metalloproteinases shed TREM-1 ectodomain from lipopolysaccharide-stimulated human monocytes. J Immunol. 2007;179:4065–4073. doi: 10.4049/jimmunol.179.6.4065. [DOI] [PubMed] [Google Scholar]
- 18.Khater WS, Salah-Eldeen NN, Khater MS, Saleh AN. Role of suPAR and lactic acid in diagnosing sepsis and predicting mortality in elderly patients. Eur J Microbiol Immunol (Bp) 2016;6:178–185. doi: 10.1556/1886.2016.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang Q, Xiong H, Yan P, Shuai T, Liu J, Zhu L, Lu J, Yang K, Liu J. The diagnostic and prognostic value of supar in patients with sepsis: a systematic review and meta-analysis. Shock. 2020;53:416–425. doi: 10.1097/SHK.0000000000001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yin WP, Li JB, Zheng XF, An L, Shao H, Li CS. Effect of neutrophil CD64 for diagnosing sepsis in emergency department. World J Emerg Med. 2020;11:79–86. doi: 10.5847/wjem.j.1920-8642.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ye Z, Zou H, Liu S, Mei C, Chang X, Hu Z, Yang H, Wu Y. Diagnostic performance of neutrophil CD64 index in patients with sepsis in the intensive care unit. J Int Med Res. 2019;47:4304–4311. doi: 10.1177/0300060519860677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yeh CF, Wu CC, Liu SH, Chen KF. Comparison of the accuracy of neutrophil CD64, procalcitonin, and C-reactive protein for sepsis identification: a systematic review and meta-analysis. Ann Intensive Care. 2019;9:5. doi: 10.1186/s13613-018-0479-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandquist M, Wong HR. Biomarkers of sepsis and their potential value in diagnosis, prognosis and treatment. Expert Rev Clin Immunol. 2014;10:1349–1356. doi: 10.1586/1744666X.2014.949675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang HS, Hur M, Yi A, Kim H, Lee S, Kim SN. Prognostic value of presepsin in adult patients with sepsis: Systematic review and meta-analysis. PLoS One. 2018;13:e0191486. doi: 10.1371/journal.pone.0191486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ulla M, Pizzolato E, Lucchiari M, Loiacono M, Soardo F, Forno D, Morello F, Lupia E, Moiraghi C, Mengozzi G, Battista S. Diagnostic and prognostic value of presepsin in the management of sepsis in the emergency department: a multicenter prospective study. Crit Care. 2013;17:R168. doi: 10.1186/cc12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu J, Hu L, Zhang G, Wu F, He T. Accuracy of presepsin in sepsis diagnosis: a systematic review and meta-analysis. PLoS One. 2015;10:e0133057. doi: 10.1371/journal.pone.0133057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang J, Hu ZD, Song J, Shao J. Diagnostic value of presepsin for sepsis: a systematic review and meta-analysis. Medicine (Baltimore) 2015;94:e2158. doi: 10.1097/MD.0000000000002158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X, Liu D, Liu YN, Wang R, Xie LX. The accuracy of presepsin (sCD14-ST) for the diagnosis of sepsis in adults: a meta-analysis. Crit Care. 2015;19:323. doi: 10.1186/s13054-015-1032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Romualdo LG, Torrella PE, González MV, Sánchez RJ, Holgado AH, Freire AO, Acebes SR, Otón MD. Diagnostic accuracy of presepsin (soluble CD14 subtype) for prediction of bacteremia in patients with systemic inflammatory response syndrome in the Emergency Department. Clin Biochem. 2014;47:505–508. doi: 10.1016/j.clinbiochem.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 30.Kweon OJ, Choi JH, Park SK, Park AJ. Usefulness of presepsin (sCD14 subtype) measurements as a new marker for the diagnosis and prediction of disease severity of sepsis in the Korean population. J Crit Care. 2014;29:965–970. doi: 10.1016/j.jcrc.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 31.Lu B, Zhang Y, Li C, Liu C, Yao Y, Su M, Shou S. The utility of presepsin in diagnosis and risk stratification for the emergency patients with sepsis. Am J Emerg Med. 2018;36:1341–1345. doi: 10.1016/j.ajem.2017.12.038. [DOI] [PubMed] [Google Scholar]
- 32.Godnic M, Stubljar D, Skvarc M, Jukic T. Diagnostic and prognostic value of sCD14-ST--presepsin for patients admitted to hospital intensive care unit (ICU) Wien Klin Wochenschr. 2015;127:521–527. doi: 10.1007/s00508-015-0719-5. [DOI] [PubMed] [Google Scholar]
- 33.Yu H, Qi Z, Hang C, Fang Y, Shao R, Li C. Evaluating the value of dynamic procalcitonin and presepsin measurements for patients with severe sepsis. Am J Emerg Med. 2017;35:835–841. doi: 10.1016/j.ajem.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 34.Porte R, Davoudian S, Asgari F, Parente R, Mantovani A, Garlanda C, Bottazzi B. The long pentraxin PTX3 as a humoral innate immunity functional player and biomarker of infections and sepsis. Front Immunol. 2019;10:794. doi: 10.3389/fimmu.2019.00794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bottazzi B, Doni A, Garlanda C, Mantovani A. An integrated view of humoral innate immunity: pentraxins as a paradigm. Annu Rev Immunol. 2010;28:157–183. doi: 10.1146/annurev-immunol-030409-101305. [DOI] [PubMed] [Google Scholar]
- 36.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 37.Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–2963. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- 38.Hamed S, Behnes M, Pauly D, Lepiorz D, Barre M, Becher T, Lang S, Akin I, Borggrefe M, Bertsch T, Hoffmann U. Diagnostic value of Pentraxin-3 in patients with sepsis and septic shock in accordance with latest sepsis-3 definitions. BMC Infect Dis. 2017;17:554. doi: 10.1186/s12879-017-2606-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee YT, Gong M, Chau A, Wong WT, Bazoukis G, Wong SH, Lampropoulos K, Xia Y, Li G, Wong MCS, Liu T, Wu WKK, Tse G International Heath Informatics Study (IHIS) Network. Pentraxin-3 as a marker of sepsis severity and predictor of mortality outcomes: a systematic review and meta-analysis. J Infect. 2018;76:1–10. doi: 10.1016/j.jinf.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 40.Hu C, Zhou Y, Liu C, Kang Y. Pentraxin-3, procalcitonin and lactate as prognostic markers in patients with sepsis and septic shock. Oncotarget. 2018;9:5125–5136. doi: 10.18632/oncotarget.23701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shabani F, Farasat A, Mahdavi M, Gheibi N. Calprotectin (S100A8/S100A9): a key protein between inflammation and cancer. Inflamm Res. 2018;67:801–812. doi: 10.1007/s00011-018-1173-4. [DOI] [PubMed] [Google Scholar]
- 42.Larsson A, Tydén J, Johansson J, Lipcsey M, Bergquist M, Kultima K, Mandic-Havelka A. Calprotectin is superior to procalcitonin as a sepsis marker and predictor of 30-day mortality in intensive care patients. Scand J Clin Lab Invest. 2019:1–6. doi: 10.1080/00365513.2019.1703216. [DOI] [PubMed] [Google Scholar]
- 43.Huang L, Li J, Han Y, Zhao S, Zheng Y, Sui F, Xin X, Ma W, Jiang Y, Yao Y, Li W. Serum calprotectin expression as a diagnostic marker for sepsis in postoperative intensive care unit patients. J Interferon Cytokine Res. 2016;36:607–616. doi: 10.1089/jir.2016.0037. [DOI] [PubMed] [Google Scholar]
- 44.Gao S, Yang Y, Fu Y, Guo W, Liu G. Diagnostic and prognostic value of myeloid-related protein complex 8/14 for sepsis. Am J Emerg Med. 2015;33:1278–1282. doi: 10.1016/j.ajem.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 45.Bartáková E, Štefan M, Stráníková A, Pospíšilová L, Arientová S, Beran O, Blahutová M, Máca J, Holub M. Calprotectin and calgranulin C serum levels in bacterial sepsis. Diagn Microbiol Infect Dis. 2019;93:219–226. doi: 10.1016/j.diagmicrobio.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 46.Jonsson N, Nilsen T, Gille-Johnson P, Bell M, Martling CR, Larsson A, Mårtensson J. Calprotectin as an early biomarker of bacterial infections in critically ill patients: an exploratory cohort assessment. Crit Care Resusc. 2017;19:205–213. [PubMed] [Google Scholar]
- 47.Havelka A, Sejersen K, Venge P, Pauksens K, Larsson A. Calprotectin, a new biomarker for diagnosis of acute respiratory infections. Sci Rep. 2020;10:4208. doi: 10.1038/s41598-020-61094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gerritsen J, Smidt H, Rijkers GT, de Vos WM. Intestinal microbiota in human health and disease: the impact of probiotics. Genes Nutr. 2011;6:209–240. doi: 10.1007/s12263-011-0229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Haak BW, Wiersinga WJ. The role of the gut microbiota in sepsis. Lancet Gastroenterol Hepatol. 2017;2:135–143. doi: 10.1016/S2468-1253(16)30119-4. [DOI] [PubMed] [Google Scholar]
- 50.Liu Z, Li N, Fang H, Chen X, Guo Y, Gong S, Niu M, Zhou H, Jiang Y, Chang P, Chen P. Enteric dysbiosis is associated with sepsis in patients. FASEB J. 2019;33:12299–12310. doi: 10.1096/fj.201900398RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wan YD, Zhu RX, Wu ZQ, Lyu SY, Zhao LX, Du ZJ, Pan XT. Gut microbiota disruption in septic shock patients: a pilot study. Med Sci Monit. 2018;24:8639–8646. doi: 10.12659/MSM.911768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lankelma JM, van Vught LA, Belzer C, Schultz MJ, van der Poll T, de Vos WM, Wiersinga WJ. Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Intensive Care Med. 2017;43:59–68. doi: 10.1007/s00134-016-4613-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Agudelo-Ochoa GM, Valdés-Duque BE, Giraldo-Giraldo NA, Jaillier-Ramírez AM, Giraldo-Villa A, Acevedo-Castaño I, Yepes-Molina MA, Barbosa-Barbosa J, Benítez-Paéz A. Gut microbiota profiles in critically ill patients, potential biomarkers and risk variables for sepsis. Gut Microbes. 2020:1–16. doi: 10.1080/19490976.2019.1707610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yin L, Wan YD, Pan XT, Zhou CY, Lin N, Ma CT, Yao J, Su Z, Wan C, Yu YW, Zhu RX. Association between gut bacterial diversity and mortality in septic shock patients: a cohort study. Med Sci Monit. 2019;25:7376–7382. doi: 10.12659/MSM.916808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17:407–420. doi: 10.1038/nri.2017.36. [DOI] [PubMed] [Google Scholar]
- 56.Viaggi B, Poole D, Tujjar O, Marchiani S, Ognibene A, Finazzi S. Mid regional pro-adrenomedullin for the prediction of organ failure in infection. Results from a single centre study. PLoS One. 2018;13:e0201491. doi: 10.1371/journal.pone.0201491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Önal U, Valenzuela-Sánchez F, Vandana KE, Rello J. Mid-regional pro-adrenomedullin (MR-proADM) as a biomarker for sepsis and septic shock: narrative review. Healthcare (Basel) 2018;6:E110. doi: 10.3390/healthcare6030110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Christ-Crain M, Morgenthaler NG, Struck J, Harbarth S, Bergmann A, Müller B. Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care. 2005;9:R816–R824. doi: 10.1186/cc3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Andaluz-Ojeda D, Nguyen HB, Meunier-Beillard N, Cicuéndez R, Quenot JP, Calvo D, Dargent A, Zarca E, Andrés C, Nogales L, Eiros JM, Tamayo E, Gandía F, Bermejo-Martín JF, Charles PE. Superior accuracy of mid-regional proadrenomedullin for mortality prediction in sepsis with varying levels of illness severity. Ann Intensive Care. 2017;7:15. doi: 10.1186/s13613-017-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chow JW, Fine MJ, Shlaes DM, Quinn JP, Hooper DC, Johnson MP, Ramphal R, Wagener MM, Miyashiro DK, Yu VL. Enterobacter bacteremia: clinical features and emergence of antibiotic resistance during therapy. Ann Intern Med. 1991;115:585–90. doi: 10.7326/0003-4819-115-8-585. [DOI] [PubMed] [Google Scholar]
- 61.Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991;143:1121–1129. doi: 10.1164/ajrccm/143.5_Pt_1.1121. [DOI] [PubMed] [Google Scholar]
- 62.Weber J, Sachse J, Bergmann S, Sparwaßer A, Struck J, Bergmann A. Sandwich immunoassay for bioactive plasma adrenomedullin. J Appl Lab Med. 2017;2:222–233. doi: 10.1373/jalm.2017.023655. [DOI] [PubMed] [Google Scholar]
- 63.Marino R, Struck J, Maisel AS, Magrini L, Bergmann A, Di Somma S. Plasma adrenomedullin is associated with short-term mortality and vasopressor requirement in patients admitted with sepsis. Crit Care. 2014;18:R34. doi: 10.1186/cc13731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim H, Hur M, Struck J, Bergmann A, Di Somma S. Circulating biologically active adrenomedullin predicts organ failure and mortality in sepsis. Ann Lab Med. 2019;39:454–463. doi: 10.3343/alm.2019.39.5.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mebazaa A, Geven C, Hollinger A, Wittebole X, Chousterman BG, Blet A, Gayat E, Hartmann O, Scigalla P, Struck J, Bergmann A, Antonelli M, Beishuizen A, Constantin JM, Damoisel C, Deye N, Di Somma S, Dugernier T, François B, Gaudry S, Huberlant V, Lascarrou JB, Marx G, Mercier E, Oueslati H, Pickkers P, Sonneville R, Legrand M, Laterre PF AdrenOSS-1 study investigators. Circulating adrenomedullin estimates survival and reversibility of organ failure in sepsis: the prospective observational multinational Adrenomedullin and Outcome in Sepsis and Septic Shock-1 (AdrenOSS-1) study. Crit Care. 2018;22:354. doi: 10.1186/s13054-018-2243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Winter J, Jung S, Keller S, Gregory RI, Diederichs S. Many roads to maturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol. 2009;11:228–234. doi: 10.1038/ncb0309-228. [DOI] [PubMed] [Google Scholar]
- 67.Krol J, Loedige I, Filipowicz W. The widespread regulation of microRNA biogenesis, function and decay. Nat Rev Genet. 2010;11:597–610. doi: 10.1038/nrg2843. [DOI] [PubMed] [Google Scholar]
- 68.Condrat CE, Thompson DC, Barbu MG, Bugnar OL, Boboc A, Cretoiu D, Voinea SC. miRNAs as biomarkers in disease: latest findings regarding their role in diagnosis and prognosis. Cells. 2020;9:E276. doi: 10.3390/cells9020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Szilágyi B, Fejes Z, Pócsi M, Kappelmayer J, Nagy B., Jr Role of sepsis modulated circulating microRNAs. EJIFCC. 2019;30:128–145. [PMC free article] [PubMed] [Google Scholar]
- 70.Vasilescu C, Rossi S, Shimizu M, Tudor S, Veronese A, Ferracin M, Nicoloso MS, Barbarotto E, Popa M, Stanciulea O, Fernandez MH, Tulbure D, Bueso-Ramos CE, Negrini M, Calin GA. MicroRNA fingerprints identify miR-150 as a plasma prognostic marker in patients with sepsis. PLoS One. 2009;4:e7405. doi: 10.1371/journal.pone.0007405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang H, Zhang P, Chen W, Feng D, Jia Y, Xie L. Serum microRNA signatures identified by Solexa sequencing predict sepsis patients' mortality: a prospective observational study. PLoS One. 2012;7:e38885. doi: 10.1371/journal.pone.0038885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li H, Ding G. Elevated serum inflammatory cytokines in lupus nephritis patients, in association with promoted hsa-miR-125a. Clin Lab. 2016;62:631–638. doi: 10.7754/clin.lab.2015.150812. [DOI] [PubMed] [Google Scholar]
- 73.Hu HL, Nie ZQ, Lu Y, Yang X, Song C, Chen H, Zhu S, Chen BB, Huang J, Geng S, Zhao S. Circulating miR-125b but not miR-125a correlates with acute exacerbations of chronic obstructive pulmonary disease and the expressions of inflammatory cytokines. Medicine (Baltimore) 2017;96:e9059. doi: 10.1097/MD.0000000000009059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhao D, Li S, Cui J, Wang L, Ma X, Li Y. Plasma miR-125a and miR-125b in sepsis: Correlation with disease risk, inflammation, severity, and prognosis. J Clin Lab Anal. 2020;34:e23036. doi: 10.1002/jcla.23036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hermans-Beijnsberger S, van Bilsen M, Schroen B. Long non-coding RNAs in the failing heart and vasculature. Noncoding RNA Res. 2018;3:118–130. doi: 10.1016/j.ncrna.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Heward JA, Lindsay MA. Long non-coding RNAs in the regulation of the immune response. Trends Immunol. 2014;35:408–419. doi: 10.1016/j.it.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yamazaki T, Souquere S, Chujo T, Kobelke S, Chong YS, Fox AH, Bond CS, Nakagawa S, Pierron G, Hirose T. Functional domains of NEAT1 architectural lncRNA induce paraspeckle assembly through phase separation. Mol Cell. 2018;70:1038–1053.e7. doi: 10.1016/j.molcel.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 78.Imamura K, Imamachi N, Akizuki G, Kumakura M, Kawaguchi A, Nagata K, Kato A, Kawaguchi Y, Sato H, Yoneda M, Kai C, Yada T, Suzuki Y, Yamada T, Ozawa T, Kaneki K, Inoue T, Kobayashi M, Kodama T, Wada Y, Sekimizu K, Akimitsu N. Long noncoding RNA NEAT1-dependent SFPQ relocation from promoter region to paraspeckle mediates IL8 expression upon immune stimuli. Mol Cell. 2014;53:393–406. doi: 10.1016/j.molcel.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 79.He F, Zhang C, Huang Q. Long noncoding RNA nuclear enriched abundant transcript 1/miRNA-124 axis correlates with increased disease risk, elevated inflammation, deteriorative disease condition, and predicts decreased survival of sepsis. Medicine (Baltimore) 2019;98:e16470. doi: 10.1097/MD.0000000000016470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Huang Q, Huang C, Luo Y, He F, Zhang R. Circulating lncRNA NEAT1 correlates with increased risk, elevated severity and unfavorable prognosis in sepsis patients. Am J Emerg Med. 2018;36:1659–1663. doi: 10.1016/j.ajem.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 81.Zhang X, Hamblin MH, Yin KJ. The long noncoding RNA Malat1: Its physiological and pathophysiological functions. RNA Biol. 2017;14:1705–1714. doi: 10.1080/15476286.2017.1358347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhao G, Su Z, Song D, Mao Y, Mao X. The long noncoding RNA MALAT1 regulates the lipopolysaccharide-induced inflammatory response through its interaction with NF-κB. FEBS Lett. 2016;590:2884–2895. doi: 10.1002/1873-3468.12315. [DOI] [PubMed] [Google Scholar]
- 83.Chen J, He Y, Zhou L, Deng Y, Si L. Long non-coding RNA MALAT1 serves as an independent predictive biomarker for the diagnosis, severity and prognosis of patients with sepsis. Mol Med Rep. 2020;21:1365–1373. doi: 10.3892/mmr.2020.10923. [DOI] [PubMed] [Google Scholar]
- 84.Na L, Ding H, Xing E, Gao J, Liu B, Wang H, Yu J, Yu C. Lnc-MEG3 acts as a potential biomarker for predicting increased disease risk, systemic inflammation, disease severity, and poor prognosis of sepsis via interacting with miR-21. J Clin Lab Anal. 2020:e23123. doi: 10.1002/jcla.23123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zha F, Qu X, Tang B, Li J, Wang Y, Zheng P, Ji T, Zhu C, Bai S. Long non-coding RNA MEG3 promotes fibrosis and inflammatory response in diabetic nephropathy via miR-181a/Egr-1/TLR4 axis. Aging (Albany NY) 2019;11:3716–3730. doi: 10.18632/aging.102011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhu M, Wang X, Gu Y, Wang F, Li L, Qiu X. MEG3 overexpression inhibits the tumorigenesis of breast cancer by downregulating miR-21 through the PI3K/Akt pathway. Arch Biochem Biophys. 2019;661:22–30. doi: 10.1016/j.abb.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 87.Parikh SM. The Angiopoietin-Tie2 Signaling Axis in Systemic Inflammation. J Am Soc Nephrol. 2017;28:1973–1982. doi: 10.1681/ASN.2017010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Leligdowicz A, Richard-Greenblatt M, Wright J, Crowley VM, Kain KC. Endothelial activation: The Ang/Tie axis in sepsis. Front Immunol. 2018;9:838. doi: 10.3389/fimmu.2018.00838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Saharinen P, Eklund L, Alitalo K. Therapeutic targeting of the angiopoietin-TIE pathway. Nat Rev Drug Discov. 2017;16:635–661. doi: 10.1038/nrd.2016.278. [DOI] [PubMed] [Google Scholar]
- 90.Seol CH, Yong SH, Shin JH, Lee SH, Leem AY, Park SM, Kim YS, Chung KS. The ratio of plasma angiopoietin-2 to angiopoietin-1 as a prognostic biomarker in patients with sepsis. Cytokine. 2020;129:155029. doi: 10.1016/j.cyto.2020.155029. [DOI] [PubMed] [Google Scholar]
- 91.Fang Y, Li C, Shao R, Yu H, Zhang Q, Zhao L. Prognostic significance of the angiopoietin-2/angiopoietin-1 and angiopoietin-1/Tie-2 ratios for early sepsis in an emergency department. Crit Care. 2015;19:367. doi: 10.1186/s13054-015-1075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang Y, Gan C, Zhang J, Chen D. LPS-induced downregulation of microRNA-204/211 upregulates and stabilizes Angiopoietin-1 mRNA in EA.hy926 endothelial cells. Mol Med Rep. 2017;16:6081–6087. doi: 10.3892/mmr.2017.7400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–874. [PubMed] [Google Scholar]
- 94.Aksaray S, Alagoz P, Inan A, Cevan S, Ozgultekin A. Diagnostic value of sTREM-1 and procalcitonin levels in the early diagnosis of sepsis. North Clin Istanb. 2016;3:175–182. doi: 10.14744/nci.2016.26023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G SCCM/ESICM/ACCP/ATS/SIS. SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31:1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 96.Brenner T, Uhle F, Fleming T, Wieland M, Schmoch T, Schmitt F, Schmidt K, Zivkovic AR, Bruckner T, Weigand MA, Hofer S. Soluble TREM-1 as a diagnostic and prognostic biomarker in patients with septic shock: an observational clinical study. Biomarkers. 2017;22:63–69. doi: 10.1080/1354750X.2016.1204005. [DOI] [PubMed] [Google Scholar]
- 97.Spoto S, Cella E, de Cesaris M, Locorriere L, Mazzaroppi S, Nobile E, Lanotte AM, Pedicino L, Fogolari M, Costantino S, Dicuonzo G, Ciccozzi M, Angeletti S. Procalcitonin and MR-proadrenomedullin combination with SOFA and qSOFA scores for sepsis diagnosis and prognosis: a diagnostic algorithm. Shock. 2018;50:44–52. doi: 10.1097/SHK.0000000000001023. [DOI] [PubMed] [Google Scholar]
- 98.Casagranda I, Vendramin C, Callegari T, Vidali M, Calabresi A, Ferrandu G, Cervellin G, Cavazza M, Lippi G, Zanotti I, Negro S, Rocchetti A, Arfini C. Usefulness of suPAR in the risk stratification of patients with sepsis admitted to the emergency department. Intern Emerg Med. 2015;10:725–730. doi: 10.1007/s11739-015-1268-7. [DOI] [PubMed] [Google Scholar]
- 99.Barre M, Behnes M, Hamed S, Pauly D, Lepiorz D, Lang S, Akin I, Borggrefe M, Bertsch T, Hoffmann U. Revisiting the prognostic value of monocyte chemotactic protein 1 and interleukin-6 in the sepsis-3 era. J Crit Care. 2018;43:21–28. doi: 10.1016/j.jcrc.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 100.Kim SB, Lee KH, Lee JU, Ann HW, Ahn JY, Jeon YD, Kim JH, Ku NS, Han SH, Choi JY, Song YG, Kim JM. Long pentraxin 3 as a predictive marker of mortality in severe septic patients who received successful early goal-directed therapy. Yonsei Med J. 2017;58:370–379. doi: 10.3349/ymj.2017.58.2.370. [DOI] [PMC free article] [PubMed] [Google Scholar]