Abstract
Cystic artery pseudoaneurysm (CAP) is a rare entity most often resulting from inflammatory conditions (acute cholecystitis or pancreatitis) or iatrogenic trauma (cholecystectomy). We report the case of a 73-year-old female who presented with abdominal pain and gastrointestinal bleeding after an episode of acute cholecystitis and endoscopic retrograde cholangiopancreatography for choledocolithiasis removal. Computed tomography and angiography revealed a CAP measuring 5 cm. A right hepatic artery transcatheter embolization was performed with glue, excluding the pseudoaneurysm. The next day, the patient underwent open cholecystectomy with ligation of the cystic artery. Later, ischemic hepatitis and abscess developed.
Keywords: Cystic artery pseudoaneurysm, Transarterial catheter embolization, Liquid embolics
Resumo
O pseudoaneurisma da artéria cística é uma entidade rara, que pode resultar de patologia inflamatória (colecistite aguda ou pancreatite) ou trauma iatrogénico (colecistectomia). Apresentamos o caso de uma mulher de 73 anos que se apresentou com dor abdominal e hemorragia digestiva após um episódio de colecistite aguda e CPRE para remoção de coledocolitíase. A TC e a angiografia revelaram um pseudoaneurisma da artéria cística com 5 cm. Foi realizada embolização da artéria hepática direita com cola, com exclusão do pseudoaneurisma. No dia seguinte a paciente foi submetida a colecistectomia com ligação da artéria cística. Posteriormente, desenvolveu-se hepatite isquémica e abcesso hepático.
Palavras Chave: Pseudo-aneurisma da artéria cística, Embolização transarterial por catéter, Embolizantes líquidos
Introduction
Cystic artery pseudoaneurysms (CAP) represent an uncommon complication of biliary inflammatory processes or iatrogenic trauma.
We describe the case of a patient who presented with CAP in the setting of acute cholecystitis and choledocolithiasis, followed by an endoscopic retrograde cholangiopancreatography (ERCP). This CAP was diagnosed by contrast-enhanced computed tomography (CT) and was managed with transcatheter embolization of the right hepatic artery, followed by open cholecystectomy.
Case Report and Case Presentation
A 73-year-old female was transferred to our hospital with an inaccurately described right hepatic artery pseudoaneurysm rupture. Two weeks before, she was admitted to a hospital with acute cholecystitis and choledocolithiasis and was managed conservatively with antibiotics. ERCP was successfully performed for choledocal stone extraction, with no immediate complications. One week after ERCP, the patient returned to the hospital after a syncopal episode witnessed at her local health center. She also complained of abdominal pain, hematemesis, and a 4-day history of melena. She was hemodynamically stable, but blood tests revealed a decreased level of hemoglobin (Hb) of 6.2 g/dL (normal range: 12–16) and mild leukocytosis.
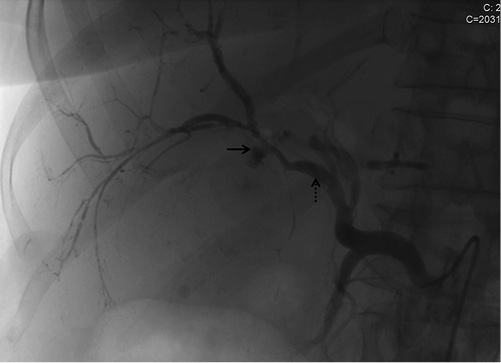
Contrast-enhanced CT revealed a pseudoaneurysm measuring 5 cm contained in the gallbladder, fed by the cystic artery (Fig. 1). There was no intraperitoneal fluid. The patient was referred to our hospital for transarterial catheter embolization. Arteriography showed a common hepatic artery arising from the superior mesenteric artery and a CAP of 5 cm (Fig. 2). Due to the high risk of intraprocedural rupture, nonselective right hepatic artery embolization was performed (backdoor and frontdoor) with cyanoacrylate (Glubran2; GEM, Via dei Campi, Italy). Control angiography demonstrated complete exclusion of the pseudoaneurysm (Fig. 3).
Fig. 1.
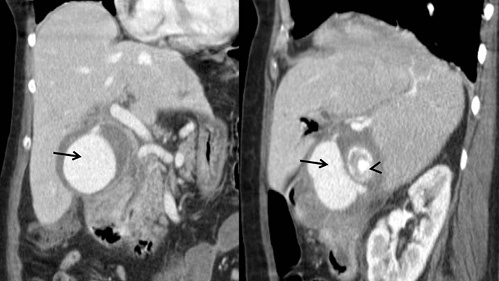
Abdominal CT with contrast showing the CAP (arrow) and a gallbladder stone (arrowhead).
Fig. 2.

Angiography showing the CAP (arrow) before embolization. Catheter's tip at the origin of the common hepatic artery (arrowhead), right hepatic artery (dotted arrow).
Fig. 3.
Angiography control showing complete exclusion of the CAP (arrow) and radiodense glue opacifying vessels distal to the dotted arrow (at the level of the right hepatic artery).
The next day she underwent open cholecystectomy, and the ischemic gallbladder was removed with ligation of the cystic artery. Intraoperatively, ischemic areas in liver segments VI and V were noticed. Aspartate transaminase (1,196 U/L) and alanine transaminase (448 U/L) were elevated (normal values: <34 and <55, respectively), and empirical therapy piperacillin-tazobactam was started.
She remained hemodynamically stable after surgery, and 1 week later she developed fever, with elevated C-reactive protein (74 mg/L, normal <5). CT revealed a hepatic fluid collection on segments V and VI, measuring 85 × 80 mm (Fig. 4), which was drained percutaneously. Citrobacter freundii and Enterococcus faecium were isolated on the abscess culture. The patient started antibiotics, and the fever ceased, with a decrease in inflammatory parameters. She remained hemodynamically stable, without evidence of blood loss, and was transferred to the hospital of origin.
Fig. 4.

Angio-CT performed 1 week after embolization showing high-density material due to glue embolization (arrows) and a non-enhanced area of hepatic parenchyma with air bubbles within, corresponding to a necrotic area due to ischemia (arrowheads).
Discussion and Conclusion
CAP is a rare entity, most often resulting from inflammatory conditions (acute cholecystitis or pancreatitis) or iatrogenic trauma (cholecystectomy) [1, 2, 3]. Visceral pseudoaneurysms following ERCP are rare complications, most frequently occurring in the gastroduodenal artery [4]. To our knowledge, there is only one case of a CAP following ERCP described in the literature, and it was also preceded by acute cholecystitis [4]. Most likely, acute cholecystitis may have been the cause of arterial wall erosion, and ERCP trauma could have precipitated rupture, leading to pseudoaneurysm formation.
Clinical symptoms of hemobilia classically include abdominal pain, jaundice, and upper gastrointestinal bleeding (Quincke triad), although only 25–30% of the patients present these symptoms [1, 2, 5, 6].
Non-contrast CT has a role in detecting recent hemorrhagic collections. Contrast-enhanced CT is an important imaging technique to demonstrate the presence of a pseudoaneurysm, its relationship with adjacent structures, and active bleeding [3]. When pseudoaneurysms are too small for angio-CT detection, angiography may be required for diagnosis [1].
Currently, there are no specific guidelines on the management of CAP due to the rarity of this condition [2, 7]. Transcatheter embolization is being successfully used as a first-approach modality or “bridging” due to diagnostic and treatment potential, reducing the probability of visceral injury and anesthetic risk [8]. Many embolization agents can be used, such as coils, Gelfoam slurry, n-butyl cyanoacrylate (glue), ethylene vinyl alcohol copolymer, and thrombin [1]. In this case, the embolic agent of choice was glue, due to the high risk of bleeding, which could require a faster control.
Following endovascular intervention, open or laparoscopic cholecystectomy and cystic artery ligation can be performed as an elective procedure, as gallbladder ischemia is a possible complication of cystic artery embolization [1, 2, 5]. In the absence of portal vein thrombosis, arterial hepatic embolization is usually well tolerated [1]. Nevertheless, postembolization ischemic hepatitis is a possible complication, and subsequent liver abscess formation may occur, which may be treated by percutaneous hepatic drainage and antibiotic therapy [9].
In conclusion, CAP is a rare, life-threatening entity with high potential of growth and rupture that requires immediate intervention [4]. A two-step approach using transcatheter embolization for diagnosis and stabilization of the patient, followed by elective cholecystectomy, is a successful multidisciplinary management of this entity, although no guidelines are established in the literature. Close monitoring of these patients is required to assure hemodynamic stability and to treat possible complications such as ischemic hepatitis and abscess formation.
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was not supported by any funding.
Author Contributions
A.L. Proença drafted the article. F. Veloso Gomes, N. Costa, T. Bilhim, J.H. Luz, and E. Coimbra participated in the embolization procedure and critically reviewed the article for intellectual content.
References
- 1.Tapnio RH, Kolber MK, Shukla PA, Berkowitz E. Transcatheter Embolization of Cystic Artery Pseudoaneurysms Secondary to Acute Cholecystitis. Vasc Endovascular Surg. 2017 Oct;51((7)):498–500. doi: 10.1177/1538574417720363. [DOI] [PubMed] [Google Scholar]
- 2.Loizides S, Ali A, Newton R, Singh KK. Laparoscopic management of a cystic artery pseudoaneurysm in a patient with calculus cholecystitis. Int J Surg Case Rep. 2015;14:182–5. doi: 10.1016/j.ijscr.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Praveen Kumar Sunkara PR, Shah PK, Rakshit K, Choudhary SR, Bohidar NP, Dubey SK. Rupture of Cystic Artery Pseudoaneurysm: a Rare Complication of Acute Cholecystitis. Indian J Surg. 2018 Feb;80((1)):87–9. doi: 10.1007/s12262-017-1667-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaduputi V, Tariq H, Dev A. Visceral Arterial Aneurysms Complicating ERCP. Hindawi Publishing Corporation. Case Rep Gastrointest Med. 2013;2013:515201. doi: 10.1155/2013/515201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trombatore C, Scilletta R, Bellavia N, Trombatore P, Magnano S Lio V, Petrillo G, et al. Acute hemobilia from a pseudoaneurysm of the cystic artery arising from the left hepatic artery: case report and literature review. Int J Surg Case Rep. 2017;37:60–4. doi: 10.1016/j.ijscr.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berry R, Han J, Kardashian HA, LaRusso NF, Tabibian JH. Hemobilia: Etiology, diagnosis, and treatment. Liver Res. 2018 Dec;2((4)):200–8. doi: 10.1016/j.livres.2018.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuzman MS, Adiamah A, Higashi Y, Gomez D. Rare case of cystic artery pseudoaneurysm. BMJ Case Rep. 2018 Mar;2018:bcr-2017–223789. doi: 10.1136/bcr-2017-223789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mokrane FZ, Alba CG, Lebbadi M, Mejdoubi M, Moulabbi M, Lombard F, et al. Pseudoaneurism of the cystic artery treated with hyperselective embolisation alone. Diagn Interv Imaging. 2013 Jun;94((6)):641–3. doi: 10.1016/j.diii.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Mezhir JJ, Fong Y, Fleischer D, Seo SK, D'Amico F, Petre E. Pyogenic abscess after hepatic artery embolization: a rare but potentially lethal complication. J Vasc Interv Radio. 2011 Feb;22((2)):177–182. doi: 10.1016/j.jvir.2010.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


