Abstract
Obstetric brachial plexus injury is reported in 0.42 per 1000 births in UK and Ireland and are associated with a reduction in quality of life for the patient and their carers. In this report we describe the first use of a patient specific, anatomically accurate 3D model as a communication tool in the treatment of a complex case of posterior shoulder subluxation secondary to glenohumeral deformity resulting from obstetric brachial plexus injury.
The use of 3D models for surgical planning is associated with decreased operating time and reduction of intra-operative blood loss, whilst their use in patient education increases patient understanding. In this case all surgeons surveyed agreed that it was useful and will use 3D modelling to improve consent processes and to conceptualise novel techniques for complex cases in future. This highly reproducible, low cost technique may be adapted to a variety of upper limb reconstructive surgeries, and as the resolution of image acquisition and additive manufacturing capabilities increase so too do the potential applications of this precise 3D printed surgical adjunct.
Keywords: Obstetric brachial plexus injury (OBPI), 3D modelling, 3D printing, Surgical planning
Introduction
Obstetric brachial plexus injury (OBPI) is reported in 0.42 per 1000 births in UK and Ireland.1 Adults with OBPI, and parents with children who have OBPI, report lower EQ-5D-5 L scores, indicating significantly poorer quality of life (p < 0.001).2 Risk factors for OBPI include shoulder dystocia, difficult or instrumented vaginal delivery, and high foetal birth weight. Symptoms depend upon the level and severity of injury, ranging from limited mobility to complete paralysis of the upper limb.3,4 Spontaneous improvement of the initial palsy may occur within 2 months for the majority of patients, but a significant minority develop glenohumeral deformity and progress to surgery to improve function.
Recent developments in 3D modelling and printing technology are being increasingly employed in other conditions, and can enhance surgical planning and simulation ahead of difficult surgeries whilst avoiding the use of cadavers or animal models.5,6 In this case we describe the first use of a patient specific, anatomically accurate 3D model to illustrate the relationship between scapula, glenoid, and head of humerus in a posterior shoulder subluxation, secondary to obstetric brachial plexus injury, who proceeded to open reduction and glenoplasty.
Case report
This is the case of a child with right sided Narakas II obstetric brachial plexus palsy (OBPI) involving C5, C6 and C7 nerve roots. Biceps recovery was demonstrated at 3 months, and by 21 months she regained 90° of shoulder elevation but developed persistent internal rotation contracture at the right shoulder and passive external rotation did not reach neutral. Radiographs revealed posterior subluxation of the humeral head and therefore it was decided to proceed to anterior subscapularis release and tendon lengthening, derotation osteotomy of the humerus, and latissimus dorsi and trees major tendon transfer. She achieved 90° active right shoulder elevation, −10° of active external rotation in adduction and internal rotation to reach the buttock, with 160° of passive elevation, 10° external rotation in adduction and internal rotation to reach T12 passively. Her brachial plexus outcome measure score postoperatively was 37/55.7
The patient did not then return for follow up, before representing aged 10 with instability in external rotation and difficulty bringing her right hand to her mouth and when holding a book. Clinical examination, CT, and MRI confirmed static posterior subluxation of the humeral head, and a severely deficient and retroverted glenoid.
Being potentially suitable for a glenoplasty procedure under development at the Royal National Orthopaedic Hospital, the patient's CT images were used to build interactive 3D virtual images and 3D print an anatomically accurate model to facilitate discussion, management planning, and patient counselling. Postoperatively the patient could bring her right hand to her mouth and comfortably put her hands behind her head. She achieved 170° active right shoulder elevation, −20° of active external rotation in adduction and internal rotation to reach L1, with 180° passive elevation −10° external rotation in adduction and internal rotation to reach the sacroiliac junction passively. There was a marked reduction in forearm pronation but she managed to compensate by internally rotating the shoulder. Clinically her shoulder remained subluxed posteriorly but overall she showed a clinical and functional improvement following surgery, with a meaningful increase in BPOM score (45/55).
Discussion
This patient with right sided Narakas II OBPI had spontaneous biceps recovery by 3 months, but incomplete recovery of C5/C6 shoulder innervation resulted in contracture and unopposed action of the rotator cuff muscles that generate internal rotation, innervated by the lower plexus nerves. An internal rotation, adduction deformity then arose that was compounded by growth deformity of the glenoid (hypoplastic, flattend, posteriorly rotated) and humeral head (hypoplastic, ovoid). Posterior shoulder subluxation resulted, with eventual posterior dislocation of the humeral head. This required surgical intervention to reduce the subluxation by a novel procedure designed to also augment the posterior glenoid.
Advances in three dimensional virtual modelling and printing provide the opportunity to produce accurate anatomical replicas using patient specific images that enable visualisation, simulation and planning in complex cases. Regulatory standards for the evolving 3D printed surgical device landscape is being developed by the medical health and regulations agency, and will consider qualification of the processing, software, data processing, input material and printer used. Current Data Protection regulations allow for 3D modelling to proceed once patient identifiable data is removed. The use of 3D models for surgical planning is associated with decreased operating time and reduction of intraoperative blood loss, whilst their use as a patient education tool indicated an increase in patient understanding, thereby improving clinical governance.8 An awareness of the available processing platforms and how to use them allows the surgical team to rapidly obtain a pre-operative surgical prototype, which additionally enhances the development of novel techniques in a safe, simulated, setting. Appropriate printing materials may be used to allow for sterilisation and use intraoperatively where required.8
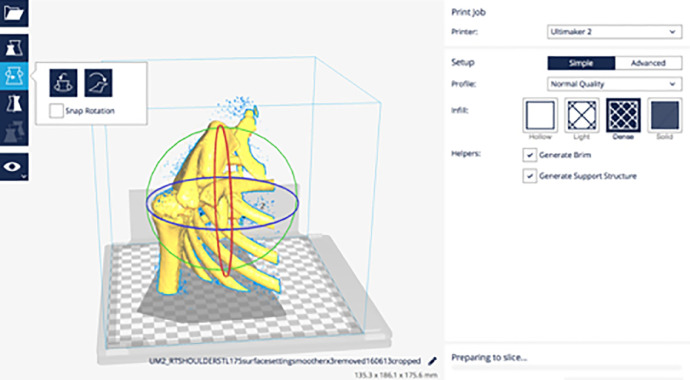
In this case, the patient's computerised tomography digital image (DICOM) files were acquired and 3D surface rendered (OsiriX, Pixmeo, Switzerland) (Figure 1) before being exported as an .stl file. Meshlab and CURA 2.6.2 open source software was used to programme the 3D print (Figure 2) in ABS plastic on an Ultimaker Original tabletop printer (Ultimaker, B.V, Netherlands), which was scaled as required. The anatomical print (Figure 3) was used to facilitate discussion between responsible teams and with the patient's family during the counselling and consent processes.
Figure 2.
3D virtual modelling of the 3D surface rendered patient's images (Meshlab, Visual Computing Laboratory, Italy).
Figure 3.
3D printed, anatomically accurate model (Ultimaker, B.V, Netherlands).
Figure 1.
3D surface rendering of the patient's CT images (OsiriX, Pixmeo, Switzerland).
All parties surveyed deemed its use in this case to have been beneficial, reporting enthusiasm for using 3D modelling to achieve increased precision and to safely gain the greater depth of understanding required to conceptualise novel techniques for treating complex cases.
The highly reproducible, low cost technique used in this complex OBPI case could be adapted to a variety of upper limb reconstructive surgeries. As the resolution of image acquisition and additive manufacturing capabilities increase so too do the potential applications of this precise anatomically accurate surgical tool.
Declaration of Competing Interest
None.
Footnotes
Presented at BAPRAS Scottish Plastic Surgery Meeting, Dunkeld 2017.
References
- 1.Evans-Jones G., Kay S.P.J., Weindling A.M., Cranny G., Ward A., Bradshaw A. Congenital brachial palsy: incidence, causes, and outcome in the United Kingdom and Republic of Ireland. Arch Dis Child Fetal Neonatal Ed. 2003;88:185–189. doi: 10.1136/fn.88.3.F185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yau C.W.H., Pizzo E., Prajapati C., Draycott T., Lenguerrand E. Obstetric brachial plexus injuries (OBPIs): health-related quality of life in affected adults and parents. Health Qual Life Outcomes. 2018;16:212. doi: 10.1186/s12955-018-1039-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coroneos C.J., Voineskos S.H., Coroneos M.K. Obstetrical brachial plexus injury: burden in a publicly funded, universal healthcare system. J Neurosurg Pediatr. 2016;17:222–229. doi: 10.3171/2015.6.PEDS14703. [DOI] [PubMed] [Google Scholar]
- 4.Yau C.W.H., Pizzo E., Prajapati C., Draycott T., Lenguerrand E. Obstetric brachial plexus injuries (OBPIs): health-related quality of life in affected adults and parents. Health Qual Life Outcomes. 2018;16:212. doi: 10.1186/s12955-018-1039-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abzug J.M., Mehlman C.T., Ying J. Assessment of current epidemiology and risk factors surrounding brachial plexus birth palsy. J Hand Surg Am. 2019;44:515. doi: 10.1016/j.jhsa.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Ganguli A., Pagan-Diaz G.J., Grant L. 3D printing for preoperative planning and surgical training: a review. Biomed Microdevices. 2018;20:65. doi: 10.1007/s10544-018-0301-9. [DOI] [PubMed] [Google Scholar]
- 7.Ho E.S., Curtis C.G., Clarke H.M. The brachial plexus outcome measure: development, internal consistency, and construct validity. J Hand Ther. 2012;25(4):406–417. doi: 10.1016/j.jht.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Jiang M., Chen G., Coles-Black J., Chuen J., Hardidge A. Three- dimensional printing in orthopaedic preoperative planning improves intraoperative metrics: a systematic review. ANZ J Surg. 2019 doi: 10.1111/ans.15549. 7. [DOI] [PubMed] [Google Scholar]