Highlights
-
•
Optimal protocol for freeze-drying that allows safe and effective preservation of HCoV-NL63 infectious material was developed.
-
•
Lyophilized virus preparations can be stored either at ambient temperature or at +4 °C. In the latter case samples may be stored for at least two months.
-
•
HCoV-NL63 virions are exquisitely stable in liquid media and can be stored also without preservatives at ambient temperature for up to 14 days.
Keywords: Coronaviridae, Coronavirus, NL63, Lyophilization, Stability, HCoV-NL63
Abbreviations: CoVs, coronaviruses; HBS, HEPES Buffered Saline; HCoV, human coronavirus; IBV, Infectious Bronchitis Virus; MERS-CoV, Middle East respiratory syndrome coronavirus; PBS, phosphate buffered saline; RT, room temperature; SARS-CoV, Severe Acute Respiratory Syndrome coronavirus
Abstract
The human coronavirus NL63 was identified in 2004 and subsequent studies showed its worldwide distribution. Infection with this pathogen is associated with upper and lower respiratory tract diseases of mild to moderate severity. Furthermore, HCoV-NL63 is the main cause of croup in children. Within this study an optimal protocol for freeze-drying that allows safe and effective preservation of HCoV-NL63 infectious material was developed. Lyophilized virus preparations can be stored either at ambient temperature or at +4 °C. In the latter case samples may be stored for at least two months. Surprisingly, conducted analysis showed that HCoV-NL63 virions are exquisitely stable in liquid media and can be stored also without preservatives at ambient temperature for up to 14 days.
Coronaviruses (CoVs) belong to the family Coronaviridae, order Nidovirales. This subfamily is currently divided into 4 groups based on phylogenic relationship (International Committee on Taxonomy of Viruses and King, 2012). Groups alpha and beta consist of mammalian CoVs, whereas gamma and delta viruses infect birds and marine mammals (Woo et al., 2010). Human CoVs for years were considered relatively harmless common cold viruses outside on the mainstream research on viral pathogens. That has changed after the outbreak of the SARS-CoV (Drosten et al., 2003, Ksiazek et al., 2003, Peiris et al., 2003) which brought CoVs to the limelight. An intense of CoVs research resulted better understanding of their pathogenesis and biology. Furthermore, two novel human CoVs were discovered: human coronavirus NL63 (van der Hoek et al., 2004) and human coronavirus HKU1 (Pyrc et al., 2010, Woo et al., 2005). Their detailed investigations revealed great variability of coronaviral species infecting animals and the potential threat of zoonotic transmission to human community. Very recently this viral family again drew attention, as another animal coronavirus – Middle East respiratory syndrome coronavirus (MERS-CoV) – crossed the species border, proving that the emergence of SARS-CoV was not an isolated case (Centers for Disease and Prevention, 2013, Zaki et al., 2012).
Intensified research on coronaviruses and development of a novel research tool based on a coronaviral backbone (e.g., vectors, vaccines) requires a method for safe storage and shipment of infectious material. Coronavirus particles are relatively stable, but previous reports show that this stability is insufficient for storage and transport of coronavirus-based vaccines, vectors and for the material exchange between laboratories (Lamarre and Talbot, 1989, Muller et al., 2008). Lyophilization is the method of choice for cost-effective stabilization of infectious material. It is a process, where a sample is frozen and subsequently the solvent is removed by sublimation (primary drying) and then by desorption (secondary drying) to the level that inhibits biological growth and chemical reactions (Jennings, 1999). To improve the stability of a sample during lyophilization and storage stabilizing substances, including lyoprotectants (Townsend and DeLuca, 1988) and bulking agents (Jennings, 1999), are added. There are numerous reports describing the freeze-drying of viruses, mainly for vaccine production (Amorij et al., 2008, Audouy et al., 2011, Bieganski et al., 1998, Burger et al., 2008, Croyle et al., 1998, de Jonge et al., 2007, Furuya et al., 2010, Geeraedts et al., 2010, Gupta et al., 2010, Kang et al., 2010, Lang et al., 2009, Levy and Fieldsteel, 1982, Yannarell et al., 2002). These methods differ in terms of process parameters and buffer content and stability of preparations ranging from 12 weeks at +4 °C (de Jonge et al., 2007) to one year at ambient temperature (Geeraedts et al., 2010, Levy and Fieldsteel, 1982). Precausta et al. developed a protocol that allowed storage of the Infectious Bronchitis Virus (IBV) for 12 months at +6 °C using 40 mg/ml mannitol as the lyoprotectant (Precausta et al., 1980). Roseto et al. lyophilized Bovine Enteric Coronavirus without addition of any stabilizing formulation for structural studies using electron microscopy (Roseto et al., 1982). Virus stability during storage was not tested. No studies on freeze-drying preservation of other coronaviruses, including human coronaviruses were previously reported.
Human coronavirus NL63 belongs to the genus alphacoronavirus (International Committee on Taxonomy of Viruses and King, 2012, Pyrc et al., 2006, Pyrc et al., 2007, van der Hoek et al., 2004). This pathogen is spread worldwide and is responsible for 1–10% of cases of viral respiratory tracts diseases (Bastien et al., 2005, Cabeca et al., 2012, Gaunt et al., 2010, Kon et al., 2012, Moes et al., 2005). Symptoms of HCoV-NL63 upper respiratory tract infection include rhinitis, cough, fever and sore throat, while infection of the lower respiratory tract manifests in bronchitis, bronchiolitis and pneumonia (Pyrc et al., 2007). Furthermore, HCoV-NL63 was proved to be the main cause of croup in children (Sung et al., 2010, van der Hoek et al., 2005).
The aim of this study was the development of a safe method for freeze-drying preservation of infectious HCoV-NL63. To this end LLC-MK2 cells (ATCC: CCL-7; Macaca mulatta kidney epithelial cell line) were used for in vitro culture of HCoV-NL63 (Schildgen et al., 2006). The cells were cultured on T25 flasks (TPP, Germany) at +37 °C with 5% CO2 in minimal essential medium (MEM), containing 2 parts of Hank's MEM and 1 part of Earle's MEM (Life Technologies, Poland) supplemented with 3% heat-inactivated fetal bovine serum (Life Technologies, Poland), penicillin (100 U/ml), and streptomycin (100 μg/ml) (H/E medium). HCoV-NL63 (Amsterdam I strain) stock was generated by infecting LLC-MK2 cells. Infected cells were lysed 6 days post-infection by two freeze–thaw cycles. The virus-containing fluid was cleared by centrifugation, aliquoted and stored at −80 °C. A control from mock infected cells was prepared in the same manner as the virus stocks. Virus yield was assessed by virus titration on fully confluent LLC-MK2 cells, according to Reed and Muench formula (Reed and Muench, 1938). All formulations used during lyophilization are presented in Table 1 and were prepared as 2× concentrated solutions in distilled water. Five times concentrated HBS buffer was prepared in distilled water. All samples were sterilized by filtration. Samples were prepared as follows: formulations 1–7: 80 μl 5× HBS, 20 μl sterile water, 200 μl 2× concentrated stabilizing formulation, 100 μl HCoV-NL63 stock (TCID50 = 1.4 million) in medium H/E 3% P/S; formulations 8–13: 100 μl sterile water, 200 μl of 2× concentrated stabilizing formulation, 100 μl HCoV-NL63 stock (TCID50 = 1.4 million) in medium H/E 3% P/S; HBS control: 80 μl 5× HBS, 220 μl sterile water, 100 μl HCoV-NL63 stock (TCID50 = 1.4 million) in medium H/E 3% P/S; PBS control: 300 μl 1× PBS (NaCl 8.0 g/l, KCl 0.2 g/l, Na2HPO4 1.44 g/l, KH2PO4 0.24 g/l, pH 7.4), 100 μl HCoV-NL63 stock (TCID50 = 1,4 million) in medium H/E 3% P/S:-H/E 3% P/S. The solutions were prepared in 2 ml tubes (Sarstdedt, Germany), snap frozen in liquid nitrogen and positioned within the sterile, pre-cooled lyophilization container with open caps.
Table 1.
Composition of stabilizing formulations used during freeze-drying of HCoV NL63 samples. Composition of different formulations including lyoprotectants, bulking agents, additional excipients and references to original works are included in the table. All formulas are presented for 1× concentrated solutions. Formulation names are used throughout the manuscript.
| Lp. | Name | Lyoprotectant | Bulking agent | Reference |
|---|---|---|---|---|
| 1. | In25 | Inulin 25 g/l | – | Audouy et al. (2011), de Jonge et al. (2007), Geeraedts et al. (2010), Amorij et al. (2008) |
| 2. | In40 | Inulin 40 g/l | – | |
| 3. | Treh100 | Trehalose 100 g/l | – | Croyle et al. (1998), Bieganski et al. (1998), Amorij et al. (2008) |
| 4. | Sucr0.5 | Sucrose 0.5 M (171 g/l) | – | Croyle et al. (1998) |
| 5. | Sucr74.6 | Sucrose 74.6 g/l | Gelatin 2% | Levy and Fieldsteel (1982) |
| 6. | Sor10 | Sorbitol 10% | Gelatin 0.4% | Croyle et al. (1998) |
| 7. | Sor2 | Sorbitol 2% | Gelatin 0.5% | Kang et al. (2010) |
| 8. | 50Mia | Myo-inositol 50 g/l | – | Burger et al. (2008) |
| 9. | 35Mi15Manna | Myo-inositol 35 g/l | 15 g/l Mannitol | |
| 10. | 25Mi25Manna | Myo-inositol 25 g/l | 25 g/l Mannitol | |
| 11. | 35Mi15Sora | Myo-inositol 35 g/l | 15 g/l Sorbitol | |
| 12. | 50Mi2Leua | Myo-inositol 50 g/l | 2 g/l Leucine | |
| 13. | 30Mi15Gela | Myo-inositol 30 g/l | 15 g/L Gelatin |
Samples supplemented with gelatin (25 g/l; with the exception of formulation 13), L–arginine (16 g/l), alanine (1 g/l), and histidine (2.1 g/l).
The drying process was carried out in the shelf lyophilizer – TMFreeZone Triad 7400030 (Labconco) with attached vacuum pump 195 (Labconco). To ensure safety, the sealed box was prepared from poly(methyl methacrylate) with a rubber seal. The container was designed for a standard probe stand. For sterilization, the box was disinfected with 70% ethanol and exposed to ultraviolet radiation. The gas exchange between the container and the lyophilizer was possible via the vent protected with a 0.1 μm air filter (Sartorius stedim, Germany). Before the lyophilization the container was pre-cooled at −20 °C. Process parameters were chosen based on literature data. In order to maintain stable temperature, the apparatus was stabilized for 3–4 h before the process (shelf temperature −30 °C, collector temperature −80 °C, vacuum off). The first drying step was carried out for 40 h at −30 °C and the pressure of 0.22 mBar. After this time the temperature was increased to −10 °C and the process was carried out for another 24 h. Subsequently, samples in the container were transferred to the laminar flow hood and capped. All samples were stored at −20 °C, +4 °C or at room temperature for stability testing.
The freeze-dried virus was dissolved in 400 μl of sterile water and incubated at +37 °C with mixing for 15 min to facilitate the dissolving of the cake. Obtained solution was diluted 5 times in H/E medium. LLC-MK2 cells were seeded on the 96-well culture plate and incubated for 48 h at +37 °C with 5% CO2 to obtain fully confluent cell monolayer. Medium was removed from the cells and fresh medium containing serially diluted virus or control samples reconstituted from lyophilized material were added. Two hours post-inoculation medium was removed and fresh H/E medium was applied. Six days post infection the cytopathic effect on the LLC-MK2 cells was assessed. Obtained data were re-calculated to TCID50 according to Reed and Muench formula (Reed and Muench, 1938).
The primary screening of different buffer composition revealed that already during the freeze-drying process some formulations do not provide sufficient protection. First, 1× HBS buffer was selected over the 1× PBS buffer, as PBS exhibits significant pH instability during the freezing process (Amorij et al., 2008). Second, the requirement for a bulking agent was confirmed, in line with observations made by Jennings (1999). Lack of a bulking agent (e.g., in sample Sucr0.5) resulted in excessive foaming during freeze-drying process, what rendered the storage of the sample impossible. Conversely, samples buffered with Sucr74.6, containing similar concentration of sucrose as samples buffered with Sucr0.5, produce during the freeze-drying a cake of good structural properties. This can be explained by the presence of gelatin.
Formulations that contained high concentration of sugars (Treh100, Sucr0.5, and Sucr74.6); sorbitol (35Mi15Sor, Sor10) or inulin (In25, In40) turned out to be toxic for the cells during the incubation with the virus. To prevent the cytotoxic effect of these formulations, the virus/mock medium was applied on cells for 2 h; following this time cells were washed and fresh medium was applied. Samples lyophilized with Sor2, Sor10 and Treh100 (Table 1) buffers showed lower TCID50 values, compared to reference samples, i.e., 1× PBS and 1× HBS (Fig. 1 ). The conducted experiments proved that mannitol is a preferable bulking agent compared to sorbitol, as cell toxicity was observed with the latter carbohydrate but not the former one. This analysis showed also that myo-inositol is optimal as a lyoprotectant for HCoV-NL63 virions.
Fig. 1.
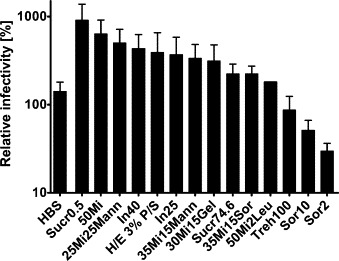
Infectivity of freeze-dried HCoV-NL63. TCID50 as a measure of infectivity of the lyophilized virus was assessed 6 days post infection. All assays were performed in triplicate in at least three independent experiments and average values with standard errors (error bars) are presented. Presented data is shown as % of TCID50 in the relation to PBS control. All formulation names are described in Table 1.
Based on obtained results three formulations yielding most promising results were selected. Selected samples contained myo-inositol as lyoprotectant and mannitol as bulking agent (25Mi25Mann, 35Mi15Mann and 50Mi). All these buffers were supplemented with gelatin, l-arginine (Merck, Germany), alanine and histidine (Sigma–Aldrich, Poland).
To test the stability of freeze-dried virus in different conditions, lyophilized samples were stored at −20 °C, +4 °C or at room temperature (RT). Preparations of the lyophilized virus were solubilized at days 0, 7, 14, 28 and 56 post-lyophilization and titrated. A set of original, not lyophilized samples was stored in identical conditions as lyophilized samples in H/E 3% P/S medium and used as a control (Fig. 2 ).
Fig. 2.
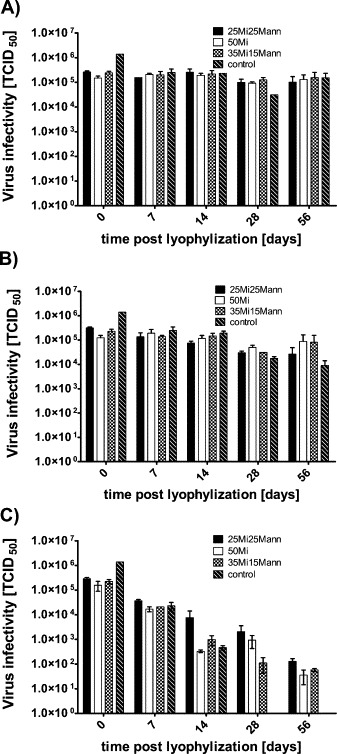
Effect of stabilizing formulations on stability of freeze-dried HCoV-NL63. TCID50 as a measure of infectivity of the lyophilized virus was assessed 6 days post infection. All assays were performed in duplicate in at least three independent experiments and average values with standard errors (error bars) are presented. Time point 0 represents samples titrated immediately after lyophilization. All formulations are described in Table 1. Graphs represent samples stored at −20 °C (A), +4 °C (B) or at ambient temperature (C).
Conducted analysis revealed that two formulations containing myo-inositol (50 g/l and 35 g/l with 15 g/l mannitol) supplemented with gelatin (25 g/l), l-arginine (16 g/l), alanine (1 g/l) and histidine (2.1 g/l) in 20 mM HEPES provided optimal stability of HCoV-NL63 virions. Sample storage at −20 °C or +4 °C for 56 days did not affect virion infectivity. When the preparation was stored at ambient temperature, the considerable virus titer decrease was observed during first weeks. These most likely resulted from hydrolysis reactions caused by residual water present in samples (Jennings, 1999). Further, a slight increase in the virus titer after 56 days of storage at +4 °C for both storage buffers was observed. Similar phenomenon was previously observed and it was suggested that virions aggregate during freeze-drying process what lowers their infectivity. Prolonged storage results in aggregate dissociation and restoration of the infectivity (Cowdery et al., 1976).
Coronavirus stability in suspension was researched by several groups. Muller et al. showed that HCoV-NL63 was still infective after 7 days of incubation at ambient temperature in PBS medium (Muller et al., 2008). Suspension of 229E infectivity was lost after 14 days of incubation at 22, 33 or 37 degrees (Lamarre and Talbot, 1989). Here we showed that HCoV-NL63 virions were still detectable after 14 days of storage in cell culture medium at room temperature. Further, virions retained infectivity at +4 °C for 56 days, showing similar decrease in virus TCID50 as freeze dried samples.
Summarizing, the optimal protocol for freeze-drying that allows safe and effective preservation of HCoV-NL63 infectious material was developed. Safety of the process is provided by usage of the inner container, sealed with the air filtration unit. Considering the need for distribution of known and novel coronaviral pathogens to different laboratories and as a reference material, the developed method may facilitate the shipment process and significantly lower the transport cost. Surprisingly, it appeared that HCoV-NL63 virions are highly stable and can be stored at ambient temperature for up to 14 days. Obtained preparations can be shipped either at ambient temperature or at +4 °C. In the latter case samples may be stored for at least two months.
Acknowledgements
This work was in supported by the LIDER grant from the National Centre for Research and Development (Lider/27/55/L-2/10/2011) (KP). The Faculty of Biochemistry, Biophysics and Biotechnology of the Jagiellonian University is a beneficiary of the structural funds from the European Union (grant no: POIG.02.01.00-12-064/08 – “Molecular Biotechnology for Health”).
References
- Amorij J.P., Huckriede A., Wilschut J., Frijlink H.W., Hinrichs W.L. Development of stable influenza vaccine powder formulations: challenges and possibilities. Pharm. Res. 2008;25:1256–1273. doi: 10.1007/s11095-008-9559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audouy S.A., van der Schaaf G., Hinrichs W.L., Frijlink H.W., Wilschut J., Huckriede A. Development of a dried influenza whole inactivated virus vaccine for pulmonary immunization. Vaccine. 2011;29:4345–4352. doi: 10.1016/j.vaccine.2011.04.029. [DOI] [PubMed] [Google Scholar]
- Bastien N., Anderson K., Hart L., Van Caeseele P., Brandt K., Milley D., Hatchette T., Weiss E.C., Li Y. Human coronavirus NL63 infection in Canada. J. Infect. Dis. 2005;191:503–506. doi: 10.1086/426869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieganski R.M., Fowler A., Morgan J.R., Toner M. Stabilization of active recombinant retroviruses in an amorphous dry state with trehalose. Biotechnol. Progr. 1998;14:615–620. doi: 10.1021/bp980057d. [DOI] [PubMed] [Google Scholar]
- Burger J.L., Cape S.P., Braun C.S., McAdams D.H., Best J.A., Bhagwat P., Pathak P., Rebits L.G., Sievers R.E. Stabilizing formulations for inhalable powders of live-attenuated measles virus vaccine. J. Aerosol. Med. Pulm. Drug Deliv. 2008;21:25–34. doi: 10.1089/jamp.2007.0658. [DOI] [PubMed] [Google Scholar]
- Cabeca T.K., Carraro E., Watanabe A., Granato C., Bellei N. Infections with human coronaviruses NL63 and OC43 among hospitalised and outpatient individuals in Sao Paulo, Brazil. Mem. Inst. Oswaldo Cruz. 2012;107:693–694. doi: 10.1590/s0074-02762012000500020. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Updated information on the epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) infection and guidance for the public, clinicians, and public health authorities, 2012–2013. Morb. Mortal. Wkly. Rep. 2013;62:793–796. [PMC free article] [PubMed] [Google Scholar]
- Cowdery S., Frey M., Orlowski S., Gray A. Stability characteristics of freeze-dried human live virus vaccines. Dev. Biol. Stand. 1976;36:297–303. [PubMed] [Google Scholar]
- Croyle M.A., Roessler B.J., Davidson B.L., Hilfinger J.M., Amidon G.L. Factors that influence stability of recombinant adenoviral preparations for human gene therapy. Pharm. Dev. Technol. 1998;3:373–383. doi: 10.3109/10837459809009865. [DOI] [PubMed] [Google Scholar]
- de Jonge J., Amorij J.P., Hinrichs W.L., Wilschut J., Huckriede A., Frijlink H.W. Inulin sugar glasses preserve the structural integrity and biological activity of influenza virosomes during freeze-drying and storage. Eur. J. Pharm. Sci. 2007;32:33–44. doi: 10.1016/j.ejps.2007.05.112. [DOI] [PubMed] [Google Scholar]
- Drosten C., Gunther S., Preiser W., van der Werf S., Brodt H.R., Becker S., Rabenau H., Panning M., Kolesnikova L., Fouchier R.A., Berger A., Burguiere A.M., Cinatl J., Eickmann M., Escriou N., Grywna K., Kramme S., Manuguerra J.C., Muller S., Rickerts V., Sturmer M., Vieth S., Klenk H.D., Osterhaus A.D., Schmitz H., Doerr H.W. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Furuya Y., Regner M., Lobigs M., Koskinen A., Mullbacher A., Alsharifi M. Effect of inactivation method on the cross-protective immunity induced by whole ‘killed’ influenza A viruses and commercial vaccine preparations. J. Gen. Virol. 2010;91:1450–1460. doi: 10.1099/vir.0.018168-0. [DOI] [PubMed] [Google Scholar]
- Gaunt E.R., Hardie A., Claas E.C., Simmonds P., Templeton K.E. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J. Clin. Microbiol. 2010;48:2940–2947. doi: 10.1128/JCM.00636-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geeraedts F., Saluja V., ter Veer W., Amorij J.P., Frijlink H.W., Wilschut J., Hinrichs W.L., Huckriede A. Preservation of the immunogenicity of dry-powder influenza H5N1 whole inactivated virus vaccine at elevated storage temperatures. AAPS J. 2010;12:215–222. doi: 10.1208/s12248-010-9179-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P.N., Pattani A., Malcolm R.K., Curran R.M., Andrews G. Development of liposome-based freeze-dried rods for vaginal vaccine delivery against HIV-1. J. Control. Release. 2010;148:e108–e110. doi: 10.1016/j.jconrel.2010.07.081. [DOI] [PubMed] [Google Scholar]
- International Committee on Taxonomy of Viruses, King A.M.Q. Academic Press; London/Waltham, MA: 2012. Virus Taxonomy: Classification and Nomenclature of Viruses: Ninth Report of the International Committee on Taxonomy of Viruses. http://www.sciencedirect.com/science/book/9780123846846. [Google Scholar]
- Jennings T.A. Interpharm Press; Englewood, CO: 1999. Lyophilization: Introduction and Basic Principles. [Google Scholar]
- Kang M.S., Jang H., Kim M.C., Kim M.J., Joh S.J., Kwon J.H., Kwon Y.K. Development of a stabilizer for lyophilization of an attenuated duck viral hepatitis vaccine. Poult. Sci. 2010;89:1167–1170. doi: 10.3382/ps.2009-00620. [DOI] [PubMed] [Google Scholar]
- Kon M., Watanabe K., Tazawa T., Watanabe K., Tamura T., Tsukagoshi H., Noda M., Kimura H., Mizuta K. Detection of human coronavirus NL63 and OC43 in children with acute respiratory infections in Niigata, Japan, between 2010 and 2011. Jpn. J. Infect. Dis. 2012;65:270–272. doi: 10.7883/yoken.65.270. [DOI] [PubMed] [Google Scholar]
- Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S., Tong S., Urbani C., Comer J.A., Lim W., Rollin P.E., Dowell S.F., Ling A.E., Humphrey C.D., Shieh W.J., Guarner J., Paddock C.D., Rota P., Fields B., DeRisi J., Yang J.Y., Cox N., Hughes J.M., LeDuc J.W., Bellini W.J., Anderson L.J., Group S.W. A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- Lamarre A., Talbot P.J. Effect of pH and temperature on the infectivity of human coronavirus 229E. Can. J. Microbiol. 1989;35:972–974. doi: 10.1139/m89-160. [DOI] [PubMed] [Google Scholar]
- Lang R., Winter G., Vogt L., Zurcher A., Dorigo B., Schimmele B. Rational design of a stable, freeze-dried virus-like particle-based vaccine formulation. Drug Dev. Ind. Pharm. 2009;35:83–97. doi: 10.1080/03639040802192806. [DOI] [PubMed] [Google Scholar]
- Levy J.A., Fieldsteel A.H. Freeze-drying is an effective method for preserving infectious type C retroviruses. J. Virol. Methods. 1982;5:165–171. doi: 10.1016/0166-0934(82)90006-4. [DOI] [PubMed] [Google Scholar]
- Moes E., Vijgen L., Keyaerts E., Zlateva K., Li S., Maes P., Pyrc K., Berkhout B., van der Hoek L., Van Ranst M. A novel pancoronavirus RT-PCR assay: frequent detection of human coronavirus NL63 in children hospitalized with respiratory tract infections in Belgium. BMC Infect. Dis. 2005;5:6. doi: 10.1186/1471-2334-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller A., Tillmann R.L., Muller A., Simon A., Schildgen O. Stability of human metapneumovirus and human coronavirus NL63 on medical instruments and in the patient environment. J. Hosp. Infect. 2008;69:406–408. doi: 10.1016/j.jhin.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris J.S., Lai S.T., Poon L.L., Guan Y., Yam L.Y., Lim W., Nicholls J., Yee W.K., Yan W.W., Cheung M.T., Cheng V.C., Chan K.H., Tsang D.N., Yung R.W., Ng T.K., Yuen K.Y., SARS study group Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Precausta P.M., Simatos D., Le Pemp M., Devaux B., Kato F. Influence of residual moisture and sealing atmosphere on viability of two freeze-dried viral vaccines. J. Clin. Microbiol. 1980;12:483–489. doi: 10.1128/jcm.12.4.483-489.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyrc K., Dijkman R., Deng L., Jebbink M.F., Ross H.A., Berkhout B., van der Hoek L. Mosaic structure of human coronavirus NL63, one thousand years of evolution. J. Mol. Biol. 2006;364:964–973. doi: 10.1016/j.jmb.2006.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyrc K., Berkhout B., van der Hoek L. The novel human coronaviruses NL63 and HKU1. J. Virol. 2007;81:3051–3057. doi: 10.1128/JVI.01466-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyrc K., Sims A.C., Dijkman R., Jebbink M., Long C., Deming D., Donaldson E., Vabret A., Baric R., van der Hoek L., Pickles R. Culturing the unculturable: human coronavirus HKU1 infects, replicates, and produces progeny virions in human ciliated airway epithelial cell cultures. J. Virol. 2010;84:11255–11263. doi: 10.1128/JVI.00947-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed L.J., Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938;27:493–497. [Google Scholar]
- Roseto A., Bobulesco P., Laporte J., Escaig J., Gaches D., Peries J. Bovine enteric coronavirus structure as studied by a freeze-drying technique. J. Gen. Virol. 1982;63(Pt 1):241–245. doi: 10.1099/0022-1317-63-1-241. [DOI] [PubMed] [Google Scholar]
- Schildgen O., Jebbink M.F., de Vries M., Pyrc K., Dijkman R., Simon A., Muller A., Kupfer B., van der Hoek L. Identification of cell lines permissive for human coronavirus NL63. J. Virol. Methods. 2006;138:207–210. doi: 10.1016/j.jviromet.2006.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung J.Y., Lee H.J., Eun B.W., Kim S.H., Lee S.Y., Lee J.Y., Park K.U., Choi E.H. Role of human coronavirus NL63 in hospitalized children with croup. Pediatr. Infect. Dis. J. 2010;29:822–826. doi: 10.1097/INF.0b013e3181e7c18d. [DOI] [PubMed] [Google Scholar]
- Townsend M.W., DeLuca P.P. Use of lyoprotectants in the freeze-drying of a model protein, ribonuclease A. J. Parenter. Sci. Technol. 1988;42:190–199. [PubMed] [Google Scholar]
- van der Hoek L., Pyrc K., Jebbink M.F., Vermeulen-Oost W., Berkhout R.J., Wolthers K.C., Wertheim-van Dillen P.M., Kaandorp J., Spaargaren J., Berkhout B. Identification of a new human coronavirus. Nat. Med. 2004;10:368–373. doi: 10.1038/nm1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Hoek L., Sure K., Ihorst G., Stang A., Pyrc K., Jebbink M.F., Petersen G., Forster J., Berkhout B., Uberla K. Croup is associated with the novel coronavirus NL63. PLoS Med. 2005;2:e240. doi: 10.1371/journal.pmed.0020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo P.C., Lau S.K., Chu C.M., Chan K.H., Tsoi H.W., Huang Y., Wong B.H., Poon R.W., Cai J.J., Luk W.K., Poon L.L., Wong S.S., Guan Y., Peiris J.S., Yuen K.Y. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J. Virol. 2005;79:884–895. doi: 10.1128/JVI.79.2.884-895.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo P.C., Huang Y., Lau S.K., Yuen K.Y. Coronavirus genomics and bioinformatics analysis. Viruses. 2010;2:1804–1820. doi: 10.3390/v2081803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yannarell D.A., Goldberg K.M., Hjorth R.N. Stabilizing cold-adapted influenza virus vaccine under various storage conditions. J. Virol. Methods. 2002;102:15–25. doi: 10.1016/s0166-0934(01)00432-3. [DOI] [PubMed] [Google Scholar]
- Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]


