Short abstract
Objective
The type of surgical treatment that should be adopted for thoracic tuberculosis (TB) remains controversial. This study was performed to compare the clinical efficacy of surgery via the single anterior and single posterior approaches for treatment of thoracic spinal TB.
Methods
Seventy-eight patients with thoracic TB undergoing surgical treatment were divided into two groups on the basis of the surgical methods employed: Group A (single anterior debridement + bone graft fusion and internal fixation) and Group B (single posterior debridement + bone graft fusion and internal fixation). Results of clinical and imaging examinations were analysed and compared between the two groups.
Results
The surgical duration and mean hospital stay were significantly longer and the perioperative bleeding volume was significantly higher in Group A than B. At the last follow-up, changes in the American Spinal Injury Association grade showed no obvious differences between the two groups. Before and after the surgery and at the last follow-up, no significant differences were detected in the Cobb angle change or correction rate between the two groups.
Conclusion
Surgery via the single anterior and single posterior approaches achieved good clinical efficacy in the treatment of thoracic spinal TB.
Keywords: Spinal tuberculosis, anterior approach, posterior approach, debridement, internal fixation, clinical efficacy
Introduction
Tuberculosis (TB) is caused by Mycobacterium tuberculosis. TB is prevalent worldwide and can occur in many parts of the human body, with pulmonary TB being the most common form. Bone TB and spinal TB, which mostly occur in the thoracolumbar spine region (≤90%), account for 50% of extrapulmonary TB.1 After the introduction of anti-TB drugs in the last century, the incidence of TB once showed a downward trend. However, the incidence of TB has again been increasing with the emergence of drug-resistant M. tuberculosis strains, and this increased incidence is closely related to economic development and the nutritional environment.2 China has a large population and unbalanced regional economic development. Statistics show that China ranks third in the incidence of TB worldwide.3
Spinal TB is one of the most common and severe forms of bone and joint TB. It mostly occurs in the thoracic spine region and always involves the anterior and middle spine. Spinal TB can occur in people of any age. Secondary infections caused by TB always lead to the development of low-grade fever, chills, kyphosis, paravertebral abscesses, or progressive neurological impairment.4 Although conservative treatment for spinal TB can effectively alleviate pain, kyphotic deformity continues to progress, with 3% to 5% of patients showing severe progression and subsequent paraplegia.4 When trauma or TB leads to the destruction of two consecutive vertebral bodies, the spine is often considered unstable. Therefore, it is particularly important to perform necessary surgical interventions to relieve clinical symptoms and achieve good long-term outcomes.5
Many surgical treatments are available for thoracic TB, such as single anterior debridement + bone graft fusion and instrumentation, single posterior debridement + bone graft fusion and instrumentation, and combined anterior and posterior approaches. However, the type of surgical treatment that should be adopted for thoracic TB remains controversial.6 Anterior surgery can completely expose the lesions, and such lesions can then be completely removed under direct vision to reduce the compression of the spinal cord. Bone grafting can be performed to correct kyphotic deformities and re-establish spinal stability; however, this method provides poor fixation and orthopaedic strength.7 Although posterior surgery can achieve satisfactory kyphosis correction and spine stability, the lesion is not completely removed; this facilitates the entry of TB bacteria into the normal posterior tissue, leading to interference of the spinal cord and an increase in postoperative intraspinal adhesion.8 Combined anterior–posterior surgery can overcome the limitations of the single anterior approach9; however, combined anterior–posterior surgery is a long procedure that is associated with substantial trauma and several complications that are not conducive to early rehabilitation. Therefore, the present study was performed to compare the clinical efficacy of surgery via the single anterior and single posterior approaches for treatment of thoracic spinal TB.
Methods
Patient population
The clinical data of patients with thoracic spinal TB treated with two surgical approaches at the Department of Spinal Surgery of Xi'an Honghui Hospital from January 2013 to December 2017 were retrospectively analysed. All patients were followed up. Active spinal TB was diagnosed on the basis of clinical manifestations and the results of laboratory [erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level], imaging [X-ray, computed tomography (CT), and magnetic resonance imaging (MRI)], and pathological examinations. Active pulmonary TB was excluded based on the findings of sputum smears and lung radiography. The inclusion criteria were (1) active thoracic spinal TB with a definite clinical, imaging, or pathological diagnosis; (2) treatment with anterior or posterior debridement + bone graft fusion or internal fixation in our hospital; (3) severe kyphosis; and (4) progressive nerve injury. The exclusion criteria were (1) lesions involving more than two vertebral bodies, (2) obvious gravitation abscess or sinus tract formation, (3) active pulmonary TB or no obvious alleviation of toxicity symptoms following 2-week routine chemotherapy, (4) recurrent thoracic spinal TB, (5) cardiopulmonary dysfunction or intolerance to surgery, and (6) complications with chronic debilitating diseases, such as malignant tumours. The study protocol was approved by the ethics review committee of our hospital, and all patients provided written informed consent to participate in the study as well as to the use and publication of data for research purposes.
Preoperative preparation
Preoperative routine anti-TB treatment was administered for ≥2 weeks via quadruple chemotherapy, including isoniazid (300 mg/day), rifampicin (450 mg/day), ethambutol (750 mg/day), and pyrazinamide (750 mg/day). Surgical treatment was performed after an ESR of <40 mm/hour and a haemoglobin level of >100 g/L had been achieved.
Surgical technique
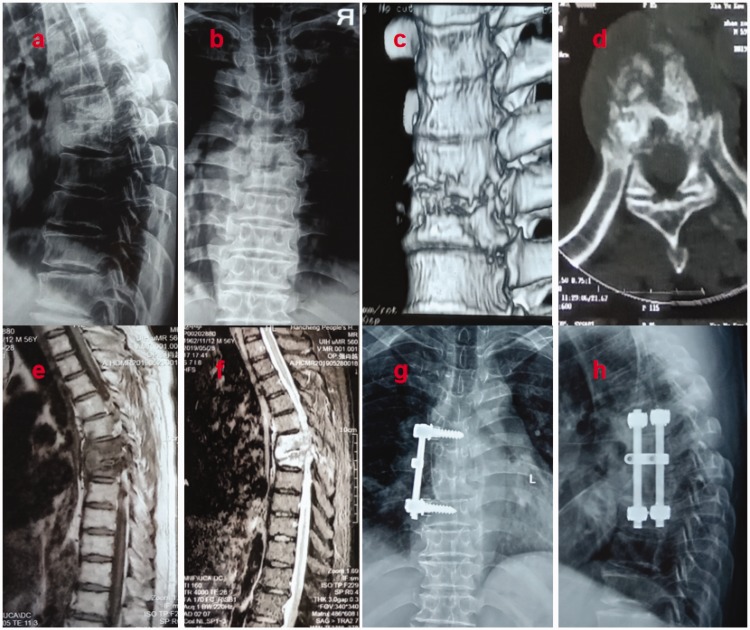
Patients in Group A were placed in the lateral decubitus position after undergoing general anaesthesia, with the more severe lesions on the upper side. Thoracic TB was treated with thorough debridement and decompression of the TB and abscess via a thoracic incision. Autologous iliac bone or an autologous trihedral cortical bone graft was used, followed by the placement of a vertebral screw, instalment of a connecting rod, and appropriate compression or distraction (Figure 1). The incision was washed and closed layer by layer. A closed thoracic drainage tube was placed for approximately 1 week following thoracotomy.
Figure 1.
Imaging findings of a 59-year-old patient with thoracic spinal tuberculosis who underwent single anterior debridement, bone grafting, and instrumentation. (a–f) Preoperative radiography, computed tomography, and magnetic resonance images showing T6–7 destruction. (g, h) Postoperative radiograph showing T5–8 fixation and vertebral height recovery.
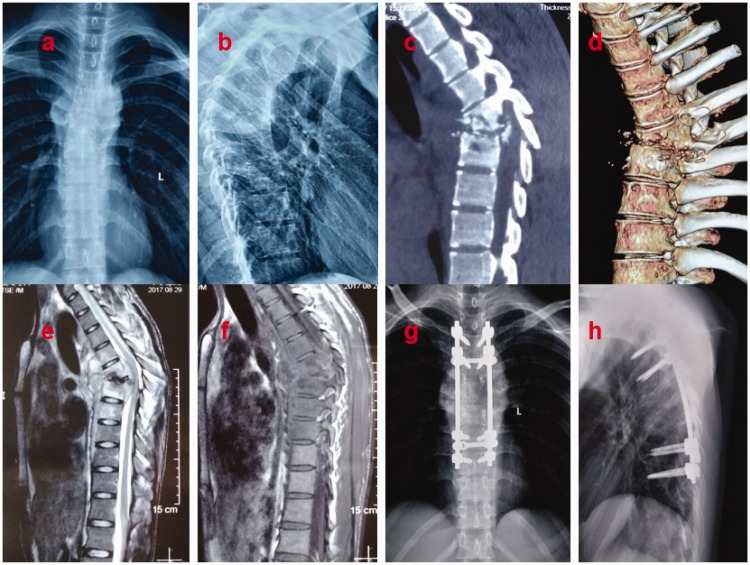
Patients in Group B were placed in the prone position after undergoing general anaesthesia. A posterior median incision was made with the affected vertebra at the centre. The paravertebral muscles were dissected along the subperiosteum of the spinous process to the outer edge of the articular process. The vertebral arch of the corresponding vertebral bodies was exposed, and a screw was inserted. Thoracic TB was treated by excision of the unilateral or bilateral costal transverse processes and facet joints. Abscesses, necrotic tissues, sequestra, and cheese-like tissues were removed completely. The deep abscess cavity was repeatedly washed with normal saline. An allogeneic bone graft or autologous iliac bone graft of the corresponding size was implanted at the bone defect, followed by placement of a pre-bent titanium rod and compression and tightening of the screw cap for fixation (Figure 2). The incision was washed and closed layer by layer, and an indwelling negative-pressure drainage tube was placed.
Figure 2.
Imaging findings of a 21-year-old patient with thoracic spinal tuberculosis who underwent single-stage posterior debridement, bone grafting, and instrumentation. (a–f) Preoperative radiography, computed tomography, and magnetic resonance images showing T5–6 destruction and a paravertebral abscess. (g, h) Postoperative anteroposterior and lateral radiographs showing T3–9 fixation.
Postoperative care
Antibiotic therapy was administered for 3 days postoperatively. When the drainage volume in the surgical area was <30 mL/day and the colour of the drainage fluid became clear, the drainage tube was removed. Doppler ultrasonography was then performed, and the drainage tube was removed after no obvious pleural effusion was observed. At postoperative days 5 to 7, all patients were examined by radiography to evaluate the position of the internal fixator and stability of the bone graft. One week after surgery, the patients were asked to stand or walk with braces. After confirmation of interbody fusion, normal activities were allowed without braces.
After 6 months of postoperative routine quadruple anti-TB chemotherapy, pyrazinamide was withdrawn but isoniazid, rifampicin, and ethambutol were continued for 12 to 18 months. The ESR, CRP level, and liver and kidney function were evaluated at monthly postoperative follow-ups. At 1, 3, 6, and 12 months after discharge, radiographs of the whole spine were re-examined and CT or MRI was performed if necessary.
Evaluation standard
The surgical duration, intraoperative bleeding volume, and mean hospital stay of all patients were recorded. The change in the angle of kyphotic deformity (Cobb angle) was used to evaluate the efficacy of the surgical correction of deformity. Recovery of spinal cord or nerve injuries was evaluated using the American Spinal Injury Association (ASIA) grading system. The visual analogue scale (VAS) score was used to assess preoperative and postoperative pain relief. The clinical curative effect of the treatment on spinal TB was evaluated based on changes in the ESR and CRP level before and after surgery. Radiographic examination was performed regularly to evaluate the duration of bone graft fusion, the correction effect of kyphosis, and the stability of the spine. The criteria for bone graft fusion included the growth of callus around the bone graft in the fusion area, the appearance of continuous trabecular bones, and the formation of obvious bone bridges around the fused vertebral bodies.10
Statistical analysis
IBM SPSS 19.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Measurement data are expressed as mean and standard deviation. The chi-square test was used to compare non-continuous variables such as age, sex, and TB onset time between the two groups. Preoperative and postoperative changes in the ASIA grade were compared between the two groups using the Wilcoxon signed-ranks test. A paired t-test was used to compare the degree of kyphotic deformity and the ESR and CRP level before and after the operation. An independent-sample t-test was used to compare changes in various laboratory and physical parameters between the two groups. Any discrepancy in a normal distribution was analysed using the rank sum test, with a significance level of 0.05.
Results
Seventy-eight patients were included in this study. Of these patients, 35 (16 men and 19 women; mean age, 44.25 ± 4.82 years) were included in Group A (treated with single anterior debridement + bone graft fusion and instrumentation) and 43 (20 men and 23 women; mean age, 43.81 ± 5.64 years) were included in Group B (treated with single posterior debridement + bone graft fusion and instrumentation). There was no significant difference in age, sex, or TB onset time between the two groups. All patients underwent radiographic examinations and some underwent CT examinations, and all showed bone graft fusion. All patients were diagnosed with TB based on the results of bacterial culture and pathological examination. Forty-five patients showed a positive M. tuberculosis culture. MRI showed accompanying cold abscesses of varying degrees in 48 patients. The surgical duration and hospital stay were significantly shorter and the intraoperative bleeding volume was significantly lower in Group B than in Group A (P < 0.05). The patients’ general information, surgical details, and postoperative characteristics are detailed in Table 1. No complications related to spinal or nerve injury occurred during surgery. All patients were followed up for a mean of 18 ± 5.4 months. No sinus tract formation or TB recurrence was observed after surgery. In Group A, two patients developed functional intestinal obstruction, which was resolved by gastrointestinal decompression. In Group B, one patient developed a fever and elevated ESR and CRP level after removal of the drainage tube 5 days after surgery, but the patient recovered with antibiotic therapy.
Table 1.
Patients’ general information, surgical details, and postoperative characteristics.
| Group | A (n = 35) | B (n = 43) |
|---|---|---|
| Sex (male/female) | 16/19 | 20/23 |
| Age (years) | 44.25 ± 4.82 | 43.81 ± 5.64 |
| TB onset time (months) | 5.68 ± 1.04 | 6.09 ± 1.10 |
| Intraoperative bleeding volume (mL) | 530.19 ± 158.91 | 295.28 ± 158.31△ |
| Surgical duration (minutes) | 136.34 ± 31.87 | 109.67 ± 49.37△ |
| Hospital stay (days) | 19.54 ± 6.29 | 14.61 ± 6.08△ |
| Duration of bone graft fusion (months) | 6.6 ± 1.3 | 6.7 ± 1.4 |
| Follow-up duration (months) | 19.36 ± 3.55 | 17.28 ± 4.21 |
TB, tuberculosis.
Data are presented as n or mean ± standard deviation.
△Comparison between Groups B and A, P < 0.05; there was no significant difference in age, sex, or TB onset time between the two groups (P > 0.05).
A single vertebral body was affected in 41 patients, and two vertebral bodies were affected in 37 patients. The lesion distribution is presented in Table 2.
Table 2.
Lesion distribution.
| T4 | T5 | T5–6 | T6 | T6–7 | T7 | T7–8 | T9 | T9–10 | |
|---|---|---|---|---|---|---|---|---|---|
| Group A (n = 35) | 0 | 1 | 2 | 4 | 7 | 6 | 5 | 7 | 3 |
| Group B (n = 43) | 1 | 1 | 3 | 5 | 6 | 7 | 6 | 9 | 5 |
In both groups, the VAS score, ESR, and CRP level were significantly lower 6 weeks after surgery than before surgery (P < 0.05). However, there were no statistically significant differences in the VAS score, ESR, or CRP level between the last follow-up and 6 weeks after surgery. Moreover, there were no statistically significant differences in the VAS, ESR, or CRP level between the two groups at the same time point before and after surgery (Table 3).
Table 3.
Comparison of VAS score, ESR, and CRP level between the two groups before and after surgery.
| Group |
VAS score |
ESR (mm/h) |
CRP (mg/L) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Before surgery | 6 weeks after surgery | Last follow-up | Before surgery | 6 weeks after surgery | Last follow-up | Before surgery | 6 weeks after surgery | Last follow-up | |
| Group A | 6.1 ± 0.6 | 3.4 ± 0.2△ | 2.2 ± 0.2* | 56.7 ± 7.6 | 16.7 ± 3.5△ | 10.2 ± 1.1* | 19.6 ± 4.3 | 9.4 ± 0.6△ | 3.1 ± 0.1* |
| Group B | 5.8 ± 0.7 | 3.1 ± 0.3△ | 2.3 ± 0.1* | 51.23 ± 8.1 | 15.8 ± 3.8△ | 9.7 ± 0.6* | 19.1 ± 5.4 | 9.1 ± 0.4△ | 4.2 ± 0.2* |
VAS, visual analogue scale; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.
△Comparison between 6 weeks after surgery and before surgery, P < 0.05.
*Comparison between the last follow-up after surgery and before surgery, P < 0.05.
Data regarding kyphosis correction and loss are presented in Table 4. There were no significant differences in the kyphosis angle before surgery and after surgery or at the last follow-up between the two groups. The correction rate of the Cobb angle was comparable between the two groups. However, the kyphosis loss rate was higher in Group A than B at the latest follow-up (P < 0.05).
Table 4.
Kyphosis correction and kyphosis loss in two groups.
| Group | Preoperative kyphosis angle (°)* |
Postoperative |
Final follow-up |
||||
|---|---|---|---|---|---|---|---|
| Kyphosis angle (°)Δ | Angle correction (°)† | Correction rate (%)▲ | Kyphosis angle (°)◇ | Angle loss (°)□ | Loss rate (%)# | ||
| A | 21.29 ± 3.72 | 4.69 ± 1.10 | 15.1 ± 3.9 | 71.5 ± 11.0 | 7.45 ± 1.09 | 2.9 ± 0.7 | 14.1 ± 4.3 |
| B | 20.68 ± 4.13 | 5.11 ± 1.05 | 15.4 ± 4.7 | 72.6 ± 10.2 | 5.92 ± 0.76 | 1.0 ± 0.6 | 5.0 ± 3.9 |
*One-way analysis of variance for comparison of preoperative kyphosis angle between the two groups, P > 0.05.
ΔOne-way analysis of variance for comparison of postoperative kyphosis angle with preoperative kyphosis angle in the two groups, PA < 0.05, PB < 0.05.
†One-way analysis of variance for comparison of angle correction between the two groups, P > 0.05.
▲One-way analysis of variance for comparison of correction rate between the two groups, P > 0.05.
□One-way analysis of variance for comparison of angle loss between the two groups, P> 0.05.
#One-way analysis of variance for comparison of angle loss rate between the two groups, P > 0.05.
The neurological recovery findings at the last follow-up are shown in Table 5. In both study groups, patients with preoperative ASIA grades C and D recovered to grade E. Until the most recent follow-up, no significant between-group difference was observed in improvement in the ASIA grade.
Table 5.
Frankel grading of neurological recovery.
| Time point |
Group A |
Group B |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | A | B | C | D | E | |
| Before surgery | 8 | 20 | 7 | 9 | 22 | 12 | ||||
| Final follow-up* | 35 | 43 | ||||||||
*P < 0.05 vs. preoperative.
Data are presented as numbers of patients.
Discussion
Following the onset of thoracic TB, the causative bacteria destroy the vertebral body to render the thoracic vertebra unstable. This results in the formation of cold abscesses, which compress the surrounding organs and nerves and result in serious functional disorders. Therefore, thoracic spinal TB treatment is aimed at removing the lesion, stabilising the spine, and relieving the nerve compression using precise anti-TB therapy, thereby creating appropriate conditions for the recovery of normal physiological functions.11 Anterior spinal surgery is the conventional intervention for thoracolumbar TB treatment.12 Anterior spinal surgery can directly reach and thoroughly remove TB lesions and can enable reconstruction to provide stability of the spine with subsequent bone graft fusion and internal fixation.13 Single-stage anterior debridement with bone graft fusion and instrumentation has become one of the most widely used method for thoracolumbar TB treatment. The anterior approach can significantly improve the kyphosis angle and VAS score in patients with thoracic vertebral TB.14 In this retrospective study, 35 patients with thoracic TB undergoing anterior surgery showed a significantly decreased postoperative VAS score as well as a decreased ESR and CRP level with standard anti-TB treatment before and after surgery. Additionally, based on the characteristics of anterior surgery (namely the complete removal of lesions under direct vision and reconstruction of the mechanical structure of the anterior and middle columns of the spine15), we analysed the clinical data of these 35 patients and found that anterior surgery was suitable for patients with three or more involved vertebral bodies, collapse of vertebral bodies mainly in the anterior and middle columns, and spinal nerve-related symptoms mainly caused by anterior compression. Despite the advantages of anterior surgery, we also noted loss of the kyphosis correction angle following anterior surgery, which is consistent with a report by Jin et al.16 Therefore, we believe that loss of the kyphosis angle following surgery should be cautiously considered in single anterior surgery on the basis of collapse of the anterior and middle columns. If the preoperative evaluation indicates a potential risk of loss of the kyphosis angle following surgery, combined anterior–posterior surgery should be adopted.
With the widespread application of pedicle screws and the advancement of surgical techniques, single posterior surgery has gradually become the primary surgical treatment for spinal TB.17 Liu et al.18 performed posterior debridement, autologous iliac bone grafting, and pedicle screw internal fixation in 37 patients with single-segment thoracic TB. Bone graft fusion was achieved in all patients at an average of 5.6 months following surgery. The kyphosis angle improved from 28.30° ± 11.95° preoperatively to 5.50° ± 11.84° postoperatively. At the last follow-up, the kyphosis angle was 7.20° ± 11.56°. The Frankel classification of nerve function showed no changes in three patients with grade A spinal cord damage. All other patients showed improvements by 1 to 3 grades following surgery. The posterior anatomical approach is simple and less traumatic, avoiding thoracotomy and combined thoracoabdominal surgery; moreover, it can effectively correct kyphotic deformity using a three-column fixation with pedicle screw system.19 We retrospectively analysed the data of 43 patients who underwent single-stage posterior debridement with bone graft fusion and internal fixation and found that single posterior surgery had a shorter surgical duration and lower intraoperative bleeding volume than single anterior surgery (P < 0.05); these data are in line with a report by Zhou et al.20 We believe that this finding may be related to the greater experience in performing pedicle screw implantation and short-segment fixation of posterior pedicle screws in patients with a lower rate of loss of the kyphosis correction angle by posterior than anterior surgery (P < 0.05), which is consistent with previous reports.21,22
In this retrospective analysis, the anterior surgical approach for thoracic TB allowed us to directly reach and thoroughly remove the lesion, enabled bone grafting and internal fixation within a larger field of vision, and achieved the goal of reconstructing the mechanical structure of the spine. Anterior surgery is more anatomically complex than posterior surgery, and several important vessels, nerves, and organs are present in front of the spine. For upper thoracic spinal TB (T4 and above), the important organs, blood vessels, and other anatomical structures are even more complex. When exposure of the diseased vertebra and performance of internal fixation are difficult, posterior internal fixation is recommended.
The limitations of this study include its retrospective nature and small sample size. Evidence of long-term efficacy needs to be verified in a large-sample, multi-centre, randomised, prospective comparative study.
Conclusion
Both single anterior and single posterior surgical approaches for the treatment of thoracic TB can achieve good clinical efficacy. However, the single posterior approach is associated with significantly less bleeding and a shorter surgical duration and mean hospital stay.
Abbreviations
TB, tuberculosis; VAS, visual analogue scale; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; CT, computed tomography; MRI, magnetic resonance imaging; ASIA, American Spinal Injury Association
Authors’ contributions
HL, JL, XW, XD, and DH participated in the patient recruitment and the data collection and analysis. All authors contributed to the study design and drafting of the manuscript. All authors read and approved the final manuscript.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article. The raw data can be requested from the corresponding author on reasonable request.
Consent for publication
All patients provided written informed consent to publish their personal details in this article.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics approval and consent to participate
Ethical approval from the Ethics Committee of Honghui Hospital, Xi'an Jiaotong University College of Medicine, was obtained for this study. Each author certifies that all investigations were conducted in conformity with ethical principles. Written informed consent was obtained from all patients included in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Glaziou P, Floyd K, Raviglione MC. Global epidemiology of tuberculosis. Semin Respir Crit Care Med 2018; 39: 271–285. [DOI] [PubMed] [Google Scholar]
- 2.El Hamdouni M, Bourkadi JE, Benamor Jet al. Treatment outcomes of drug resistant tuberculosis patients in Morocco: multi-centric prospective study. BMC Infect Dis 2019; 19: 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao Q, Zeng C, Zheng Det al. Analysis on spatial-temporal distribution characteristics of smear positive pulmonary tuberculosis in China, 2004-2015. Int J Infect Dis 2019; 80S: S36–S44. [DOI] [PubMed] [Google Scholar]
- 4.Rajasekaran S, Soundararajan DCR, Shetty APet al. Spinal tuberculosis: current concepts. Global Spine J 2018; 8: 96S–108S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn RN, Ben Husien M. Spinal tuberculosis: review of current management. Bone Joint J 2018; 100-B: 425–431. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Y, Song Z, Luo Jet al. The efficacy of local continuous chemotherapy and postural drainage in combination with one-stage posterior surgery for the treatment of lumbar spinal tuberculosis. BMC Musculoskelet Disord 2016; 17: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li ZW, Li ZQ, Tang BMet al. Efficacy of one-stage posterior debridement and bone grafting with internal fixation in the treatment of monosegmental thoracolumbar tuberculosis. World Neurosurg 2019; 121: e843–e851. [DOI] [PubMed] [Google Scholar]
- 8.Jain A, Jain RK, Kiyawat V. Evaluation of outcome of transpedicular decompression and instrumented fusion in thoracic and thoracolumbar tuberculosis. Asian Spine J 2017; 11: 31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang P, Zang Q, Kang Jet al. Comparison of clinical efficacy and safety among three surgical approaches for the treatment of spinal tuberculosis: a meta-analysis. Eur Spine J 2016, 25: 3862–3874. [DOI] [PubMed] [Google Scholar]
- 10.Moon MS, Woo YK, Lee KSet al. Posterior instrumentation and anterior interbody fusion for tuberculosis kyphosis of dorsal and lumbar spines. Spine 1995; 20: 1910–1916. [DOI] [PubMed] [Google Scholar]
- 11.Alam MS, Phan K, Karim Ret al. Surgery for spinal tuberculosis: a multi-center experience of 582 cases. J Spine Surg 2015; 1: 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mak KC, Cheung KM. Surgical treatment of acute TB spondylitis: indications and outcomes. Eur Spine J 2013; 22: 603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benli IT, Acaroğlu E, Akalin Set al. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J 2003; 12: 224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jain AK, Dhammi IK, Prashad Bet al. Simultaneous anterior decompression and posterior instrumentation of the tuberculous spine using an anterolateral extrapleural approach. J Bone Joint Surg Br 2008; 90: 1477–1481. [DOI] [PubMed] [Google Scholar]
- 15.Oga M, Arizono T, Takasita Met al. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine (Phila Pa 1976) 1993; 18: 1890–1894. [DOI] [PubMed] [Google Scholar]
- 16.Jin D, Qu D, Chen Jet al. One-stage anterior interbody autografting and instrumentation in primary surgical management of thoracolumbar spinal tuberculosis. Eur Spine J 2004; 13: 114–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang K, Wang N, Wang Yet al. Anterior versus posterior instrumentation for treatment of thoracolumbar tuberculosis: a meta-analysis. Orthopade 2019; 48: 207–212. [DOI] [PubMed] [Google Scholar]
- 18.Liu P, Sun M, Li Set al. A retrospective controlled study of three different operative approaches for the treatment of thoracic and lumbar spinal tuberculosis: three years of follow-up. Clin Neurol Neurosurg 2015; 128: 25–34. [DOI] [PubMed] [Google Scholar]
- 19.Zhang HQ, Li JS, Zhao SSet al. Surgical management for thoracic spinal tuberculosis in the elderly: posterior only versus combined posterior and anterior approaches. Arch Orthop Trauma Surg 2012; 132: 1717–1723. [DOI] [PubMed] [Google Scholar]
- 20.Zhou Y, Li W, Liu Jet al. Comparison of single posterior debridement, bone grafting and instrumentation with single-stage anterior debridement, bone grafting and posterior instrumentation in the treatment of thoracic and thoracolumbar spinal tuberculosis. BMC Surg 2018; 18: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hassan K, Elmorshidy E. Anterior versus posterior approach in surgical treatment of tuberculous spondylodiscitis of thoracic and lumbar spine. Eur Spine J 2016; 25: 1056–1063. [DOI] [PubMed] [Google Scholar]
- 22.Huang Z, Liu J, Ma K. Posterior versus anterior approach surgery for thoracolumbar spinal tuberculosis. J Coll Physicians Surg Pak 2019; 29: 187–188. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article. The raw data can be requested from the corresponding author on reasonable request.