Abstract
Ethnopharmacological relevance and aim of the study
Tripterygium wilfordii (lei gong teng; Thunder of God Vine), a member of the Celastraceae family, is a medicinal plant used to treat a range of illnesses. Celastrol is a quinone methide triterpene and the most abundant bioactive constituent isolated from the root extracts of T. wilfordii. Previous studies have shown that celastrol exhibits antiviral activity against HIV and SARS-CoV. To date, no investigations of the anti-DENV activity of celastrol have been reported. This work aimed to investigate the anti-DENV effect and possible mechanism of celastrol in vitro and in vivo.
Methods
A four-serotype DENV infection system was performed to determine the anti-DENV effect of celastrol by detecting DENV RNA replication and protein synthesis. The precise anti-DENV replication mechanism of celastrol was clarified using specific RNA silencing and specific inhibitor. In addition, the therapeutic efficacy of celastrol was evaluated by monitoring survival rates and clinical scores in a DENV-infected Institute of Cancer Research (ICR) suckling mouse model.
Results
Celastrol inhibited DENV-1, -2, -3, and -4 RNA replication with EC50 values of 0.19 ± 0.09, 0.12 ± 0.11, 0.16 ± 0.14, and 0.17 ± 0.08 μM, respectively. This antiviral effect of celastrol was associated with celastrol-induced interferon-α (IFN-α) expression and was attenuated by a specific inhibitor of the JAK–STAT signaling pathway downstream of IFN-α or specific shRNA. Furthermore, celastrol protected ICR suckling mice against life-threatening DENV infection.
Conclusion
Celastrol represents a potential anti-DENV agent that induces IFN-α expression and stimulates a downstream antiviral response, making the therapy a promising drug or dietary supplement for the treatment of DENV-infected patients.
Keywords: Dengue virus, Celastrol, Antiviral interferon response
1. Introduction
Dengue virus (DENV) is an enveloped virus belonging to the Flavivirus genus in the Flaviviridae family, and based on antigenic diversity, DENV can be divided into four different serotypes (Halsey et al., 2012). The virus has an 11-kb RNA genome that is translated into a polyprotein and is subsequently cleaved by both host and virus NS2B/NS3 protease into at least 10 mature viral proteins (Lee et al., 2015a). Three structural proteins (capsid, prM, and envelope) distinguish DENV serotypes and regulate DENV attachment and entry. Seven nonstructural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5) are indispensable for DENV replication and are highly conserved across DENV serotypes (Dalrymple et al., 2015). DENV is an arthropod-borne pathogen that is propagated by the mosquito Aedes aegypti (Salazar et al., 2007). DENV infection causes a spectrum of symptoms ranging from acute self-limiting febrile illness to life-threatening dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS) (Jones et al., 2005, Ubol et al., 2008). The geographic range of dengue is extensively increasing due to urbanization and global warming, particularly in tropical and subtropical areas (McMichael et al., 2006). Approximately 400 million people in over 100 countries are exposed to the threat of DENV infection (Bhatt et al., 2013, Ubol et al., 2008). Currently, the tetravalent dengue vaccine exhibits limited efficacy (Screaton et al., 2015). Hence, the discovery of alternative strategies to decrease the burden of DENV infection is urgently needed.
Innate cellular immune responses, especially interferon alpha/beta (IFN α/β)-mediated antiviral signaling, are the most important action against viral replication and pathogenesis (Jones et al., 2005, Morrison et al., 2013). In general, virus infection induces the production and secretion of type I IFN, which interacts with cell surface IFN-α receptors (IFNAR1 and IFNAR2) on virus-infected and nearby cells. IFN-α receptors receive stimulation from type I IFN, leading to the activation of Jak1 and Tyk2 kinases via tyrosine phosphorylation. Subsequently, signal transducer and activator of transcription 1 and 2 (STAT1/2) are phosphorylated, after which they form heterodimers. The STAT1/2 heterodimers translocate to the nucleus and bind to IFN-stimulated response elements (ISREs), leading to the upregulation of hundreds of cellular genes and the induction of antiviral responses (Morrison et al., 2013). Conversely, knockout mice that lack IFN α/β receptors or exhibit deficiencies in type I IFN production are susceptible to DENV infection (Johnson and Roehrig, 1999, Shresta et al., 2004). Clinically, low levels of type I IFN have been observed in patients with severe dengue-associated disease, revealing that the IFN system plays an important role in preventing DENV infection and pathogenesis (Jones et al., 2005, Ubol et al., 2008). Several reports demonstrated that IFN-stimulated genes and proteins could inhibit DENV replication, such as IFN-induced transmembrane protein 2 and 3 (IFITM2 and IFITM3), double-stranded RNA-dependent protein kinase, and 2′, 5′-oligoadenylate synthetase/RNase L (OAS) (Jiang et al., 2010, Simon-Loriere et al., 2015); thus, boosting the IFN-mediated antiviral response might represent a potent strategy against DENV infection.
Tripterygium wilfordii (lei gong teng; Thunder of God Vine), a member of the Celastraceae family, is a medicinal plant used to treat a range of illnesses including inflammation, swelling, fever, sores, and pain, and it has been used in India, Japan, China, Korea, and other Asian countries for some time (Ju et al., 2015, Lee et al., 2015b, Youn et al., 2014). Celastrol is a quinone methide triterpene and the most abundant bioactive constituent isolated from the root extracts of T. wilfordii (Ju et al., 2015). Celastrol is a meal supplement that is comprehensively used in herbal medicine because of its diverse biological activities, such as anti-inflammation, anti-cancer, hepatoprotection, and immunomodulation (Youn et al., 2014). Moreover, celastrol exhibits antiviral activity against HIV and SARS-CoV via different mechanisms (Ryu et al., 2010, Youn et al., 2014). To date, no investigations of the anti-DENV activity of celastrol have been reported. In this study, our data revealed that celastrol inhibits DENV replication by upregulating IFN-α production and activating JAK–STAT signaling in hepatoma cells. Celastrol also provided a protective effect against life-threatening DENV-2 infection in Institute of Cancer Research (ICR) suckling mice.
2. Materials and methods
2.1. Ethics statement
The experimental protocol was ratified by the Animal Research Committee of Kaohsiung Medical University of Taiwan (IACUC, 102177) under the guidance of the Public Health Service Policy on Humane Care and Use of Laboratory Animals. All mice received humane care and were fed with standard rodent chew and water ad libitum. Mice were acclimatized under a standard laboratory condition following the Animal Use Protocol of Kaohsiung Medical University for a week before experiment.
2.2. Experimental animals
Six-day-old ICR suckling mice were used in this study, and breeder mice of the ICR strain were obtained from BioLasco Taiwan Co. Ltd. All mice received humane care and ad libitum access to standard rodent chew and water. Mice were acclimatized under standard laboratory conditions following the Animal Use Protocol of Kaohsiung Medical University for a week before the experiment.
2.3. Cells and virus
Huh-7 cells were maintained in Dulbecco's modified Eagle's medium containing 10% fetal bovine serum, 1% non-essential amino acids, and 1% antibiotic–antimycotic in a 5% CO2 atmosphere at 37 °C. DENV (type 1 strain DN8700828; DENV-1, type 2 strain 16681; DENV-2, type 3 strain DN8700829A; DENV-3, and type 4 strain S9201818; DENV-4) was obtained from the Centers for Disease Control, Department of Health, Taiwan and amplified in C6/36 mosquito cells (Hsu et al., 2012, Lee et al., 2015a).
2.4. Reagents
Celastrol (PubChemCID:122724) were purchased from Fusol-Material Co., LTD (Tainan, Taiwan), the batch number is 14092610 and the HPLC quality control data was shown in Fig. S1. The JAK inhibitor were obtained from Sigma (St. Louis, MO, USA). T-Pro™ transfection reagent was obtained from Ji-Feng Biotechnology Co., Ltd. (Taipei, Taiwan).
2.5. Cell cytotoxicity assay
Huh-7 cells were seeded in 96-well plates at a density of 5 × 103 cells per well and treated with celastrol at the indicated concentrations. Cell viability was determined by the CellTiter 96 AQueous One Solution Cell Proliferation Assay (Promega, Madison, WI, USA) according to the manufacturer's instructions. Color intensity was detected at 490 nm using a 550 BioRad plate-reader (Bio-Rad, Hertfordshire, UK).
2.6. DENV and cellular mRNA quantification
Total cell RNA was extracted using an RNA extraction kit (ALLBio Co, Ltd, Taiwan) according to the manufacturer's instructions. DENV RNA and cellular mRNA levels were analyzed by quantitative real-time reverse-transcription polymerase chain reaction (qRT-PCR) as previously described (Lee et al., 2015a). Relative DENV RNA levels were normalized against cellular glyceraldehyde-3-phosphate dehydrogenase (gapdh) mRNA expression. The primers used in the study are listed in Table 1 .
Table 1.
Oligonucleotide sequences for real-time RT-PCR.
| Oligonucleotide name | Sequence 5′–3′ |
|---|---|
| DENV gene oligonucleotide sequences | |
| 5′ NS5 | 5′-GGA AACCAAGCTGCCCATCA |
| 3′ NS5 | 5′—CCTCCACGGATAGAAGTTTA |
| Human gene oligonucleotide sequences | |
| 5′ GAPDH | 5′-GTCTTCACCACCATGGAGAA |
| 3′ GAPDH | 5′-ATGGCATGGACTGTGGTCAT |
| 5′ OAS1 | 5′- CAAGCTTAAGAGCCTCATCC |
| 3′ OAS1 | 5′- TGGGCTGTGTTGAAATGTGT |
| 5′ OAS2 | 5′- ACAGCTGAAAGCCTTTTGGA |
| 3′ OAS2 | 5′- GCATTAAAGGCAGGA AGCAC |
| 5′ OAS3 | 5′- CACTGACATCCCAGACGATG |
| 3′ OAS3 | 5′- GATCAGGCTCTTCAGCTTGG |
| 5′ IFN-alpha 2 | 5′-GCA AGT CAA GCT GCT CTG TG |
| 3′ IFN-alpha 2 | 5′-GAT GGT TTC AGC CTT TTG GA |
| 5′ IFN-alpha 5 | 5′- AGTTTGATGGCAACCAGTTC |
| 3′ IFN-alpha 5 | 5′- TCAGAGGAGTGTCTTCCACT |
| 5′ IFN-alpha 17 | 5′-AGG AGT TTG ATG GCA ACC AG |
| 3′ IFN-alpha 17 | 5′-CAT CAG GGG AGT CTC TTC CA |
2.7. Western blotting
Western blotting was performed as described previously (Lee et al., 2014). In brief, 20 μg of cell lysates were analyzed by SDS-PAGE, followed by transfer to a PVDF membrane. Membrane samples were probed with anti-DENV NS2B (1:3000; GeneTex), anti-GAPDH (1:10,000; GeneTex), anti-STAT1 (1:5000, Cell Signaling), anti-phosphorylated STAT1 (1:2000, Cell Signaling), anti-STAT2 (1:3000, Cell Signaling), and anti-phosphorylated STAT2 antibodies (1:1000, Cell Signaling).
2.8. Plaque assay
BHK-21 cells were plated in 12-well plates at 1 × 105 cells per well. The virus collected from culture medium was serially diluted and was incubated with BHK-21 cells in a volume of 400 μl at 30 °C. After 2 h incubation, the 3 ml DMEM containing 2% FBS and 0.8% methyl cellulose (Sigma-Aldrich) were added into each well. At 5 days post-infection, cells were fixed and stained with the plaque assay solution (1% crystal violet, 0.64% NaCl, and 2% formalin) at 25 °C for 2 h. Finally, the viral titer was calculated by observation of plaque formation.
2.9. Plasmid and shRNA
pISRE-Luc, a reporter vector containing firefly luciferase under the control of an ISRE, was used to measure IFN response-dependent transcriptional activity (Stratagene, Agilent Technologies, CA). STAT1, STAT2, Tyk2, and enhanced green fluorescent protein (EGFP) shRNAs were purchased from the National RNAi Core Facility, Institute of Molecular Biology/Genomic Research Center, Academia Sinica, Taiwan. All cloned DNA fragments were verified by DNA sequencing.
2.10. Transfection and luciferase activity assay
To evaluate transcriptional regulation of the IFN response by celastrol, Huh-7 cells were plated in 24-well plates at a density of 5 × 104 cells per well and transfected with pISRE-Luc plasmids using T-Pro™ transfection reagent according to the manufacturer's instructions. The transfected cells were treated with the indicated concentrations of celastrol for 3 days. Luciferase activity was analyzed using the Steady-Glo Luciferase Assay System (Promega) as previously described.
2.11. In vivo anti-DENV activity assay
Six-day-old ICR suckling mice weighing 3.5–4 g were randomly divided into three groups (n = 10/group) as follows: Group 1, intracerebrally injected with 2.5 × 105 pfu of 60 °C heat-inactive DENV type 2 strain PL046 (iDENV); Group 2, intracerebrally injected with 2.5 × 105 pfu of DENV type 2 strain PL046 + 20 μl of saline (DENV); and Group 3, intracerebrally injected with 2.5 × 105 pfu of DENV type 2 strain PL046 + 0.1 mg/kg celastrol (DENV + celastrol). Mice were given saline or 0.1 mg/kg celastrol via intracerebral injection at 1, 3, and 5 days post-infection (dpi). Survival rates, body weight, and clinical scores were measured every day after DENV injection. Illness symptoms were scored as follow: 0 for no symptoms; 1 for slight weight loss and ruffled hair; 2 for slowing of activity; 3 for asthenia and anorexia; 4 for paralysis and mortally ill; and 5 for death. At 6 dpi, the mice were sacrificed by CO2 asphyxiation, after which 0.1 g of brain tissue was harvested using TRIzol for RNA collection.
2.12. Statistical analysis
Data were presented as mean ± standard deviation for at least three independent experiments. Statistical significance was analyzed using Student's t-test.
3. Results
3.1. Celastrol inhibits DENV RNA replication and protein synthesis
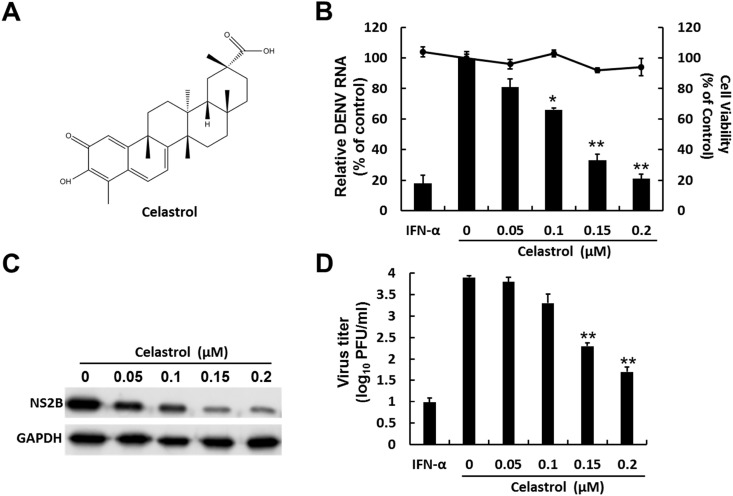
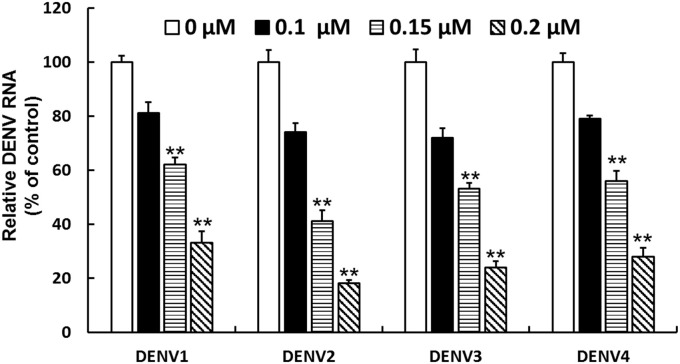
Celastrol is a quinone methide triterpene (Fig. 1 A) possessing diverse biological activities (Ju et al., 2015, Lee et al., 2015b). To investigate whether celastrol exhibits anti-DENV activity, we treated DENV-2–infected Huh-7 cells with the drug at various concentrations for 3 days. qRT-PCR analysis was performed to evaluate the inhibitory effect of celastrol on DENV RNA replication. In the meantime, the cytotoxic effect of DENV-infected cells (Fig. 1B) and naïve Huh-7 cells (Fig. S2) were tested using the MTS assay. As shown in Fig. 1B, celastrol proportionally reduced DENV RNA replication with a 50% effective concentration (EC50) of 0.12 ± 0.011 μM, and it was not cytotoxic at effective antiviral concentrations. Western blotting was then performed to evaluate the inhibitory effect of celastrol on DENV protein synthesis, and similar to the result for DENV RNA replication, celastrol concentration-dependently reduced DENV NS2B protein level (Fig. 1C). In addition, celastrol concentration-dependently decreased the viral titer compared with the celastrol-untreated cells (Fig. 1D). To further examine the inhibitory effect of celastrol on RNA replication in different DENV serotypes, Huh-7 cells were infected with DENV-1, -2, -3, and -4. The DENV-infected Huh-7 cells were treated with celastrol at various concentrations for 3 days, and DENV RNA replication was analyzed by qRT-PCR analysis. As shown in Fig. 2 , celastrol inhibited DENV-1, -2, -3, and -4 RNA replication with EC50 values of 0.19 ± 0.009, 0.12 ± 0.011, 0.16 ± 0.014, and 0.17 ± 0.008 μM, respectively.
Fig. 1.
Celastrol inhibits DENV RNA replication and protein synthesis. (A) Structure of celastrol. Celastrol inhibits DENV (B) RNA replication, (C) protein synthesis, and (D) DENV propagation. Huh-7 cells were seeded in 24-well plates and infected with DENV-2 at an MOI of 0.1 for 2 h. The DENV-2–infected Huh-7 cells were treated with 0.05, 0.1, 0.15, and 0.2 μM celastrol for 3 days. DENV RNA replication was normalized against the cellular gapdh mRNA level and is presented as the percentage change relative to the celastrol-untreated control. The IFN-α (300UI) was severed as positive control. Protein synthesis was evaluated by Western blotting using anti-DENV NS2B antibody. Equal loading of cell lysates was confirmed by probing the same blot with anti-GAPDH antibody. DENV titer was determined by performing plague assay. The IFN-α (300UI) was severed as positive control. Results are expressed as the mean ± SD (error bar) of 3 independent experiments; *P < 0.05, **P < 0.01.
Fig. 2.
Celastrol inhibits DENV-1–4 RNA replication. Huh-7 cells were seeded in 24-well plates at a density of 4 × 104 cells/well and separately infected with four different DENV serotypes at an MOI of 0.1 for 2 h (DENV-1: DN8700828; DENV-2: 16681; DENV-3: DN8700829A; DENV-4: S9201818). The DENV-infected Huh-7 cells were treated with 0.1, 0.15, and 0.2 μM celastrol for 3 days. DENV RNA replication was normalized against the cellular gapdh mRNA level and is presented as the percentage change relative to the celastrol-untreated control. Results are expressed as the mean ± SD (error bar) of 3 independent experiments; **P < 0.01.
3.2. Celastrol protects ICR suckling mice against life-threatening DENV infection
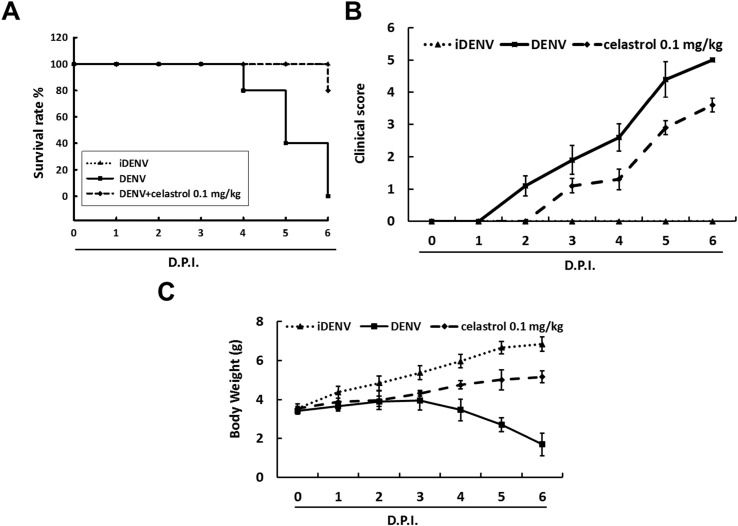
To further investigate whether celastrol also exhibits anti-DENV activity in vivo, we employed DENV-infected ICR suckling mice to examine the protective effect of celastrol on life-threatening DENV infection. Six-day-old ICR suckling mice weighing 3.5–4 g were randomly divided into three groups, and the survival rates, clinical scores, and body weights of DENV-injected mice treated with or without celastrol were measured daily for 6 days. Relative to the iDENV group, severe illness leading to death within 4–6 days dpi was noted in the DENV group. By contrast, celastrol at a concentration of 0.1 mg/kg protected 80% of the mice against life-threatening DENV-2 infection compared with the non-celastrol–treated mice (Fig. 3 A). After 6 days of observation, the animals in the DENV group exhibited severe asthenia, paralysis, and 60% body weight loss compared with the iDENV group (Fig. 3B and C). Conversely, the celastrol-treated group displayed slight asthenia, paralysis, and 15% body weight loss compared with the iDENV group at 6 dpi (Fig. 3B and C). These results revealed that celastrol exerted a protective effect against DENV-2–induced lethality and related illness.
Fig. 3.
Celastrol protects ICR suckling mice against life-threatening DENV infection. Six-day-old ICR suckling mice weighing 3.5–4 g were randomly divided into three groups: Group 1, intracerebrally injected with 2.5 × 105 pfu of 60 °C heat-inactive DENV and 20 μl of saline at 1, 3, and 5 days post-infection (dpi) as a negative control (iDENV); Group 2, intracerebrally injected with 2.5 × 105 pfu of DENV and 20 μl of saline at 1, 3, and 5 dpi as a positive control (DENV); Group 3, intracerebrally injected with 2.5 × 105 pfu of DENV and celastrol 0.1 mg/kg at 1, 3, and 5 dpi. (A) Survival rates, (B) clinical scores, and (C) body weight were measured every day after DENV injection. Symptoms were scored as follows: 0 for no symptoms; 1 for slight weight loss and ruffled hair; 2 for slowing of activity; 3 for asthenia and anorexia; 4 for paralysis and mortally ill; and 5 for death. Mice in the control group were treated with 60 °C heat-inactive DENV for 30 min. Each group included 6–8 mice.
3.3. Celastrol induces antiviral IFN-α gene expression and protein secretion
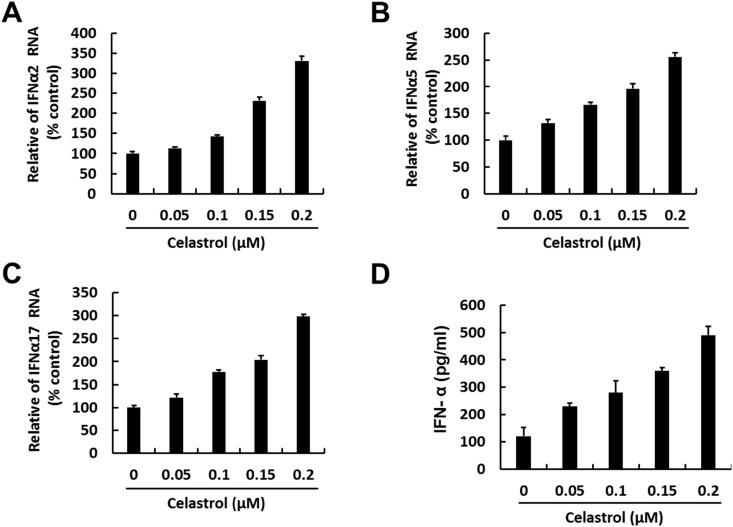
Numerous reporters demonstrated that celastrol exerts an immunomodulatory effect (Ryu et al., 2010, Seo et al., 2010). To determine whether celastrol could induce IFN-α expression via this effect, we measured IFN-α-2, IFN-α-5, and IFN-α-17 RNA expression and IFN-α protein secretion. The DENV-2 infected-Huh-7 cells were treated with celastrol at increased concentrations for 3 days. The qRT-PCR analysis was then performed to evaluate the IFN-α-2, IFN-α-5, and IFN-α-17 gene expression. As shown in Fig. 4 A–C, celastrol concentration-dependently induced IFN-α-2, IFN-α-5, and IFN-α-17 RNA expression compared with the findings in non-celastrol-treated cells. The inductive effects of IFN-α-2, IFN-α-5, and IFN-α-17 RNA expression by celastrol were also observed in naïve Huh-7 cells (Fig. S3). In addition, the IFN-α protein level in the supernatant was measured by ELISA under the same experimental conditions. As expected, celastrol induced IFN-α protein secretion into the supernatant in a concentration-dependent manner (Fig. 4D).
Fig. 4.
Celastrol induces antiviral IFN-α gene expression and protein secretion. Celastrol induces RNA transcription of (A) IFN-α-2, (B) IFN-α-5, and (C) IFN-α-17 in DENV-infected Huh-7 cells. Huh-7 cells were seeded in 24-well plates and infected with DENV-2 at an MOI of 0.1 for 2 h. The DENV-2-infected Huh-7 cells were treated with 0.05, 0.1, 0.15, and 0.2 μM celastrol for 3 days. Total RNA was harvested for RT-qPCR with specific primers against IFN-α-2, IFN-α-5, and IFN-α-17. The RNA levels of IFN-α-2, IFN-α-5, and IFN-α-17 were normalized against the cellular gapdh mRNA level and are presented as the percentage change relative to the celastrol-untreated control. (D) Celastrol induces IFN protein secretion. Huh-7 cells were seeded in 24-well plates and infected with DENV-2 at an MOI of 0.1 for 2 h. The DENV-2-infected Huh-7 cells were treated with 0.05, 0.1, 0.15, and 0.2 μM celastrol for 3 days. The culture fluid was subjected to ELISA to determine IFN-α protein levels. Results are expressed as the mean ± SD (error bar) of 3 independent experiments; *P < 0.05, **P < 0.01.
3.4. Celastrol induces antiviral IFN responses through the JAK–STAT pathway
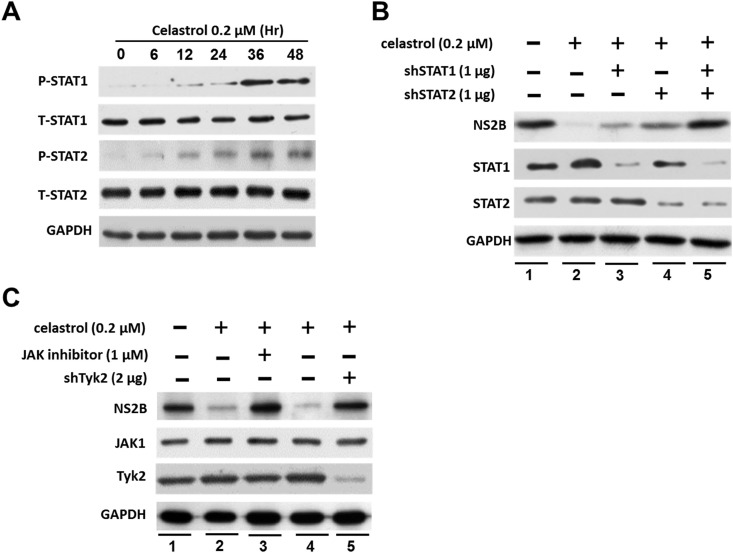
IFN-α interacts with cell surface IFN-α receptors and activates Jak1 and Tyk2 kinases (Fink and Grandvaux, 2013, Katze et al., 2002), leading to the phosphorylation and translocation of STAT1/2 (Darnell, 1997, Schindler and Strehlow, 2000). To further confirm whether celastrol stimulated JAK–STAT pathways, we first treated DENV-infected Huh-7 cells with celastrol at 0.2 μM for different time periods, and STAT1/2 phosphorylation levels were analyzed by Western blotting. As shown in Fig. 5 A, Celastrol treatment increases the levels of STAT1/2 phosphorylation in a time dependent manner. To further confirm the role of STAT1/2 in celastrol anti-DENV activity, shRNA against STAT1/2 was employed to silence STAT1/2 expression. As shown in Fig. 5B, celastrol effectively reduced DENV protein replication (lanes 1 and 2), and the STAT1-and STAT2-specific shRNA (lanes 3 and 4) partially restored the anti-DENV effect of celastrol. Relative to the depletion of STAT1 or STAT2 alone, depletion of both STAT1 and STAT2 exerted a restorative effect on DENV protein replication (lane 5). To further clarify the contribution of celastrol-induced IFN-α expression to STAT1/2 phosphorylation, the STAT1/2 upstream kinases Jak1 and Tyk2 were inhibited using a Jak1-specific inhibitor and Tyk2-specific shRNA. As shown in Fig. 5C, the Jak1-specific inhibitor effectively attenuated the anti-DENV effect of celastrol compared with the findings in celastrol-treated and untreated cells (lanes 1–3), and Tyk2-specific shRNA exerted a restoration effect on DENV protein replication (lanes 1, 4, and 5). These data indicated that the anti-DENV activity of celastrol was mediated by IFN-α.
Fig. 5.
Celastrol activates Jak-STAT signaling and increases STAT1/2 phosphorylation. (A) Celastrol increases STAT1/2 phosphorylation in a time-dependent manner. DENV-infected Huh-7 cells were treated with 0.2 μM celastrol at the indicated times (0–48 h), and total protein was assayed by Western blotting using anti-phospho-STAT1, anti-STAT1, anti-phospho-STAT2, anti-STAT2, and anti-GAPDH (loading control) antibodies. Band intensity was quantified by densitometric scanning and presented as the fold value relative to the 0 h measurement (defined as 1) following normalization against the GAPDH protein level. (B) STAT1/2-specific shRNA restored the anti-DENV effect of celastrol. Huh-7 cells were transfected with shRNA against STAT1 and STAT2 (1 μg) or EGFP (1 μg) followed by DENV infection and celastrol treatment for 3 days. Protein synthesis was evaluated by Western blotting using anti-DENV NS2B antibody, anti-STAT1 antibody, and anti-STAT2 antibody. Equal loading of cell lysates was confirmed by probing the same blot with anti-GAPDH antibody. (C) A Jak inhibitor and Tyk2-specific shRNA restored the anti-DENV effect of celastrol. Huh-7 cells were transfected with shRNA against Tyk2 (2 μg) or treated with a Jak inhibitor (1 μM). The cells were infected with DENV and treated with 0.2 μM celastrol 3 days. Protein synthesis was evaluated by Western blotting using anti-DENV NS2B antibody anti-JAK1 antibody, and anti-Tyk2 antibody. Equal loading of cell lysates was confirmed by probing the same blot with anti-GAPDH antibody.
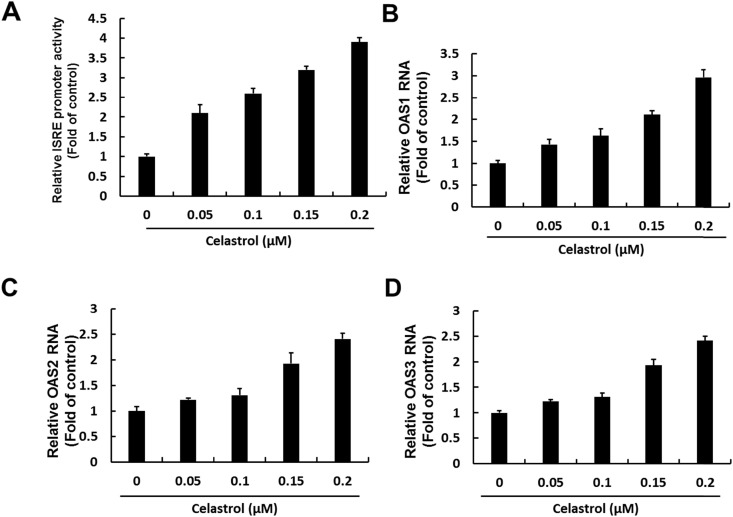
Upon phosphorylation and translocation, STAT1 and STAT2 bind to ISREs, leading to the upregulation of downstream antiviral genes (McComb et al., 2014, Perry et al., 2011). To determine whether celastrol-induced IFN-α could activate downstream antiviral genes, ISRE activity and OAS1–3 gene expression were measured. The DENV-infected cells were transfected with ISRE-driven firefly luciferase reporter plasmid followed by treatment of celastrol for 3 days. As shown in Fig. 6 A, celastrol increased ISRE promoter activity approximately 2.1–3.9-fold, as determined by luciferase activity. Furthermore, as critical IFN-stimulated genes against viral infection, OAS1–3 gene expression was examined. As shown in Fig. 6B–D, OAS1–3 was significantly upregulated by celastrol in a concentration-dependent manner.
Fig. 6.
Celastrol induces anti-viral IFN responses in DENV infected Huh-7 cells. (A) Celastrol induces ISRE promoter activity in DENV-infected Huh-7 cells. Huh-7 cells were transfected with pISRE-Luc. After 6 h, the transfected cells were infected with DENV-2 strain 16681 at an MOI of 0.2 for 2 h at 37 °C and treated with 0.05, 0.1, 0.15, and 0.2 μM celastrol for 3 days. Luciferase activity was measured to determine ISRE promoter activity and presented as fold activation relative to celastrol-untreated cells (defined as 1). Celastrol induces RNA transcription of (B) OAS1, (C) OAS2, and (D) OAS3 in DENV-infected Huh-7 cells. Huh-7 cells were seeded in 24-well plates and infected with DENV-2 at an MOI of 0.1 for 2 h. The DENV-2-infected Huh-7 cells were treated with 0.05, 0.1, 0.15, and 0.2 μM celastrol for 3 days. Total RNA was harvested for qRT-PCR with specific primers against OAS1, OAS2, and OAS3. The RNA levels of OAS1, OAS2, and OAS3 were normalized against the cellular gapdh mRNA level and are presented as the percentage change relative to the celastrol-untreated control. Results are expressed as the mean ± SD (error bar) of 3 independent experiments; *P < 0.05, **P < 0.01.
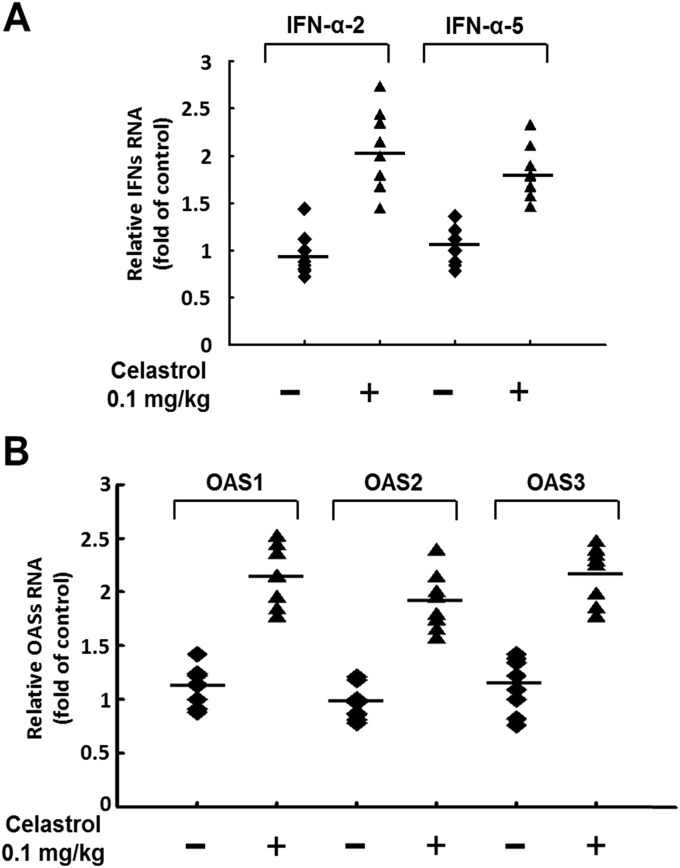
3.5. Celastrol induces antiviral IFN responses in DENV-infected ICR suckling mice in vivo
To confirm that celastrol exhibits IFN-modulating activity in vivo, brain tissue was collected to analyze IFN and OAS gene expression. As shown in Fig. 7 A and B, IFN-α-2, IFN-α-5, OAS1, OAS2, and OAS3 gene expression levels were significantly increased in celastrol-treated mice compared with levels in untreated DENV-infected mice at 6 dpi. These data suggested that celastrol preferentially induced anti-viral interferon gene expression in DENV-infected ICR suckling mice.
Fig. 7.
Celastrol induces antiviral IFN responses in DENV-infected ICR suckling mice in vivo. Six-day-old ICR suckling mice were inoculated with 2.5 × 105 pfu of DENV-2 by intracerebral injection and administered celastrol (0.1 mg/kg) at 1, 3, and 5 dpi. Then, 0.1 g of brain tissue was harvested by TRIzol for RNA collection. (A) IFN-α and (B) OAS family gene expression levels were measured by qRT-PCR with specific primers against IFN-α-2, IFN-α-5, OAS1, OAS2, and OAS3. The RNA levels of IFN-α-2, IFN-α-5, OAS1, OAS2, and OAS3 were normalized against the cellular gapdh mRNA level and are presented as the fold change relative to the celastrol-untreated control (defined as 1). The iDENV group was subjected to 60 °C heat-inactivated DENV for 30 min. The numbers of mice in each group ranged from 6 to 8.
4. Discussion
In the present study, our data clearly demonstrate that celastrol strongly suppressed DENV serotype 1–4 replication (Fig. 1, Fig. 2). In addition, celastrol effectively reduced clinical scores and protected ICR suckling mice against life-threatening DENV infection (Fig. 3). In this study, the comprehensive anti-DENV mechanisms of celastrol were demonstrated, and the antiviral IFN response was thoroughly investigated. The data indicate that the antiviral activity of celastrol in DENV-infected cells occurred together with the upregulation of IFN-α expression (Fig. 4), which echoes the findings of Diamond et al. on IFN modulation in DENV-infected human cells (Diamond et al., 2000). The retinoic acid inducible gene I signaling pathway and its downstream molecules, such as mitochondrial antiviral signaling, IPS-1, IFN regulatory factor 3 (IRF3), and IRF7, are critical for IFN production (Chen et al., 2013, Nasirudeen et al., 2011). Future studies should be performed to determine which IFN-activated pathway contributes to the anti-DENV effect of celastrol to obtain additional information for designing anti-DENV agents.
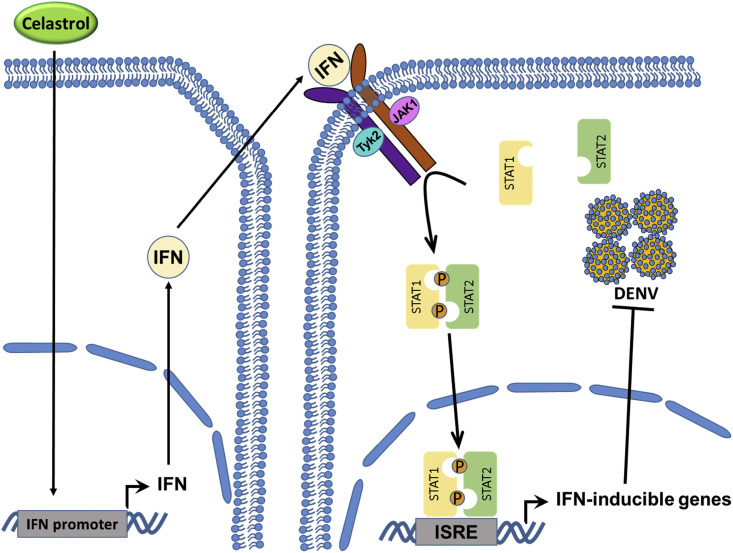
Our results reveal that Jak1/Tyk2-mediated STAT1 and STAT2 activation contributed to the anti-DENV activity of celastrol (Fig. 5). Moreover, we found that the OAS gene family, which is downstream of STAT1 and STAT2, was stimulated by celastrol (Fig. 6). Similar results were observed in DENV-infected ICR suckling mouse brain tissue (Fig. 7). On the basis of the findings presented in this study, we propose a model to demonstrate the action of celastrol against DENV infection (Fig. 8 ). Simon-Loriere et al. demonstrated that the OAS gene family exhibits high anti-DENV activity, and these data supported our findings (Simon-Loriere et al., 2015). However, DENV infection results in the inhibition of antiviral IFN signaling, which is attributable to DENV NS2B/NS3 protease-mediated cleavage of human mediator of IRF3 activation (MITA) (Yu et al., 2012), NS4A-mediated inhibition of TBK1/IRF3 phosphorylation (Dalrymple et al., 2015), and NS5 replicase-mediated inhibition of STAT2 expression (Morrison et al., 2013). The inhibitory effect of celastrol on DENV NS2B/NS3 protease, NS4A, or NS5 replicase might in part contribute to its anti-DENV activity. This hypothesis should be investigated in the future.
Fig. 8.
A model illustrating celastrol inhibits DENV replication. Celastrol inhibited DENV replication by upregulating IFN expression and activating downstream Jak-STAT signaling, resulting in the expression of IFN-stimulated antiviral genes.
In the decades, numerous groups intend to develop direct-acting antivirals (DAAs) for treating DENV infection. However, the high replication rate of DENV and low fidelity of NS5 RNA polymerase may lead to DAA-resistant variants, representing a major challenge in anti-DENV DAA development (Lim et al., 2013). In addition, the efficacy of DAAs against different serotypes of DENV may be different (Lim et al., 2013). Therefore, enhancing host innate immunity exerts protective effects against DENV progression, such as IFN activation, representing a potential tactic to avoid drug resistance and the effects of genetic variability in the viral genome (Lim et al., 2013, Morrison et al., 2013). Numerous studies illustrated that type I IFN is involved in the pathogenesis of DENV infection and the progression from undifferentiated febrile illness (DF) to life-threatening infection (DHF/DSS) (Jones et al., 2005, Ubol et al., 2008). Viral loads and the circulating levels of DENV NS1 antigen are the most important differences between DF and DHF in patients (Chuang et al., 2016, Halstead, 2015b). The high circulating levels of DENV NS1 antigen result in the enhancement of DENV infection via virus-antibody complexes. Furthermore, the intracellular innate responses against DENV are suppressed by interactions between virus-antibody complexes and Fc receptors (Chareonsirisuthigul et al., 2007, Huang et al., 2006), resulting in increased DENV replication and progression to DHF and DSS (Halstead, 2015a). Therefore, celastrol-induced IFN may function as a potential anti-DENV factor and exert cytoprotective effects against DENV-associated cell damage and the life-threatening symptoms associated with DHF and DSS. Further study is necessary to elucidate the effects of celastrol against the pathogenesis of DENV infection and progression to DHF and DSS.
5. Conclusions
In summary, celastrol markedly inhibited DENV replication by upregulating IFN expression and activating downstream Jak-STAT signaling, resulting in the expression of IFN-stimulated OAS genes. This may represent a therapeutic tactic against DENV infection, and celastrol can be considered a promising drug or dietary supplement for the treatment of DENV-infected patients.
Acknowledgments
We gratefully acknowledge Dr. Charles Rice (Rockefeller University and Aapth, LCC, USA) for kindly supporting human hepatoma cell; Huh-7 and Centers for Disease Control, Department of Health, Taiwan, for kindly supporting 4 serotypes of dengue virus (DENV-1: DN8700828; DENV-2: DN454009A; DENV-3: DN8700829A; DENV-4: S9201818) This work was supported by a grant from the Ministry Science and Technology of Taiwan, (MOST104-2320-B-037-025-MY3), Kaohsiung Medical University (KMU-TP104H03), the National Sun Yat-Sen University-KMU Joint Research Project (NSYSU-KMU 105-I003), and ChiMei Medical Center, Taiwan (103CM-KMU-11 and 104CM-KMU-05).
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.antiviral.2016.11.010.
Contributor Information
Ching-Liang Hsieh, Email: clhsieh@mail.cmuh.org.tw.
Jin-Ching Lee, Email: jclee@kmu.edu.tw.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Bhatt S., Gething P.W., Brady O.J., Messina J.P., Farlow A.W., Moyes C.L., Drake J.M., Brownstein J.S., Hoen A.G., Sankoh O., Myers M.F., George D.B., Jaenisch T., Wint G.R., Simmons C.P., Scott T.W., Farrar J.J., Hay S.I. The global distribution and burden of dengue. Nature. 2013;496(7446):504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chareonsirisuthigul T., Kalayanarooj S., Ubol S. Dengue virus (DENV) antibody-dependent enhancement of infection upregulates the production of anti-inflammatory cytokines, but suppresses anti-DENV free radical and pro-inflammatory cytokine production, in THP-1 cells. J. General Virol. 2007;88(Pt 2):365–375. doi: 10.1099/vir.0.82537-0. [DOI] [PubMed] [Google Scholar]
- Chen H.W., King K., Tu J., Sanchez M., Luster A.D., Shresta S. The roles of IRF-3 and IRF-7 in innate antiviral immunity against dengue virus. J. Immunol. 2013;191(8):4194–4201. doi: 10.4049/jimmunol.1300799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang Y.C., Lin J., Lin Y.S., Wang S., Yeh T.M. Dengue virus nonstructural protein 1-Induced antibodies cross-react with human plasminogen and enhance its activation. J. Immunol. 2016;196(3):1218–1226. doi: 10.4049/jimmunol.1500057. [DOI] [PubMed] [Google Scholar]
- Dalrymple N.A., Cimica V., Mackow E.R. Dengue virus NS proteins inhibit RIG-I/MAVS signaling by blocking TBK1/IRF3 phosphorylation: Dengue virus serotype 1 NS4A is a unique interferon-regulating virulence determinant. mBio. 2015;6(3) doi: 10.1128/mBio.00553-15. e00553–00515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell J.E., Jr. STATs and gene regulation. Science. 1997;277(5332):1630–1635. doi: 10.1126/science.277.5332.1630. [DOI] [PubMed] [Google Scholar]
- Diamond M.S., Roberts T.G., Edgil D., Lu B., Ernst J., Harris E. Modulation of Dengue virus infection in human cells by alpha, beta, and gamma interferons. J. Virol. 2000;74(11):4957–4966. doi: 10.1128/jvi.74.11.4957-4966.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink K., Grandvaux N. STAT2 and IRF9: beyond ISGF3. Jak-Stat. 2013;2(4):e27521. doi: 10.4161/jkst.27521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halsey E.S., Marks M.A., Gotuzzo E., Fiestas V., Suarez L., Vargas J., Aguayo N., Madrid C., Vimos C., Kochel T.J., Laguna-Torres V.A. Correlation of serotype-specific dengue virus infection with clinical manifestations. PLoS Negl. Trop. Dis. 2012;6(5):e1638. doi: 10.1371/journal.pntd.0001638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halstead S.B. Comment on “Dengue virus NS1 protein activates cells via Toll-like receptor 4 and disrupts endothelial cell monolayer integrity” and “Dengue virus NS1 triggers endothelial permeability and vascular leak that is prevented by NS1 vaccination. Sci. Transl. Med. 2015;7(318) doi: 10.1126/scitranslmed.aad4863. 318le314. [DOI] [PubMed] [Google Scholar]
- Halstead S.B. 2015. Pathogenesis of Dengue: Dawn of a New Era. F1000Research 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu Y.C., Chen N.C., Chen P.C., Wang C.C., Cheng W.C., Wu H.N. Identification of a small-molecule inhibitor of dengue virus using a replicon system. Arch. Virol. 2012;157(4):681–688. doi: 10.1007/s00705-012-1224-z. [DOI] [PubMed] [Google Scholar]
- Huang K.J., Yang Y.C., Lin Y.S., Huang J.H., Liu H.S., Yeh T.M., Chen S.H., Liu C.C., Lei H.Y. The dual-specific binding of dengue virus and target cells for the antibody-dependent enhancement of dengue virus infection. J. Immunol. 2006;176(5):2825–2832. doi: 10.4049/jimmunol.176.5.2825. [DOI] [PubMed] [Google Scholar]
- Jiang D., Weidner J.M., Qing M., Pan X.B., Guo H., Xu C., Zhang X., Birk A., Chang J., Shi P.Y., Block T.M., Guo J.T. Identification of five interferon-induced cellular proteins that inhibit west nile virus and dengue virus infections. J. Virol. 2010;84(16):8332–8341. doi: 10.1128/JVI.02199-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson A.J., Roehrig J.T. New mouse model for dengue virus vaccine testing. J. Virol. 1999;73(1):783–786. doi: 10.1128/jvi.73.1.783-786.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M., Davidson A., Hibbert L., Gruenwald P., Schlaak J., Ball S., Foster G.R., Jacobs M. Dengue virus inhibits alpha interferon signaling by reducing STAT2 expression. J. Virol. 2005;79(9):5414–5420. doi: 10.1128/JVI.79.9.5414-5420.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju S.M., Youn G.S., Cho Y.S., Choi S.Y., Park J. Celastrol ameliorates cytokine toxicity and pro-inflammatory immune responses by suppressing NF-kappaB activation in RINm5F beta cells. BMB Rep. 2015;48(3):172–177. doi: 10.5483/BMBRep.2015.48.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katze M.G., He Y., Gale M., Jr. Viruses and interferon: a fight for supremacy. Nature reviews. Immunology. 2002;2(9):675–687. doi: 10.1038/nri888. [DOI] [PubMed] [Google Scholar]
- Lee J.C., Tseng C.K., Wu Y.H., Kaushik-Basu N., Lin C.K., Chen W.C., Wu H.N. Characterization of the activity of 2'-C-methylcytidine against dengue virus replication. Antivir. Res. 2015;116:1–9. doi: 10.1016/j.antiviral.2015.01.002. [DOI] [PubMed] [Google Scholar]
- Lee J.C., Tseng C.K., Young K.C., Sun H.Y., Wang S.W., Chen W.C., Lin C.K., Wu Y.H. Andrographolide exerts anti-hepatitis C virus activity by up-regulating haeme oxygenase-1 via the p38 MAPK/Nrf2 pathway in human hepatoma cells. Br. J. Pharmacol. 2014;171(1):237–252. doi: 10.1111/bph.12440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.Y., Lee B.H., Kim N.D., Lee J.Y. Celastrol blocks binding of lipopolysaccharides to a Toll-like receptor4/myeloid differentiation factor2 complex in a thiol-dependent manner. J. Ethnopharmacol. 2015;172:254–260. doi: 10.1016/j.jep.2015.06.028. [DOI] [PubMed] [Google Scholar]
- Lim S.P., Wang Q.Y., Noble C.G., Chen Y.L., Dong H., Zou B., Yokokawa F., Nilar S., Smith P., Beer D., Lescar J., Shi P.Y. Ten years of dengue drug discovery: progress and prospects. Antivir. Res. 2013;100(2):500–519. doi: 10.1016/j.antiviral.2013.09.013. [DOI] [PubMed] [Google Scholar]
- McComb S., Cessford E., Alturki N.A., Joseph J., Shutinoski B., Startek J.B., Gamero A.M., Mossman K.L., Sad S. Type-I interferon signaling through ISGF3 complex is required for sustained Rip3 activation and necroptosis in macrophages. Proc. Natl. Acad. Sci. U. S. A. 2014;111(31):E3206–E3213. doi: 10.1073/pnas.1407068111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael A.J., Woodruff R.E., Hales S. Climate change and human health: present and future risks. Lancet. 2006;367(9513):859–869. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- Morrison J., Laurent-Rolle M., Maestre A.M., Rajsbaum R., Pisanelli G., Simon V., Mulder L.C., Fernandez-Sesma A., Garcia-Sastre A. Dengue virus co-opts UBR4 to degrade STAT2 and antagonize type I interferon signaling. PLoS Pathog. 2013;9(3):e1003265. doi: 10.1371/journal.ppat.1003265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasirudeen A.M., Wong H.H., Thien P., Xu S., Lam K.P., Liu D.X. RIG-I, MDA5 and TLR3 synergistically play an important role in restriction of dengue virus infection. PLoS Negl. Trop. Dis. 2011;5(1):e926. doi: 10.1371/journal.pntd.0000926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry S.T., Buck M.D., Lada S.M., Schindler C., Shresta S. STAT2 mediates innate immunity to Dengue virus in the absence of STAT1 via the type I interferon receptor. PLoS Pathog. 2011;7(2):e1001297. doi: 10.1371/journal.ppat.1001297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu Y.B., Park S.J., Kim Y.M., Lee J.Y., Seo W.D., Chang J.S., Park K.H., Rho M.C., Lee W.S. SARS-CoV 3CLpro inhibitory effects of quinone-methide triterpenes from Tripterygium regelii. Bioorg. Med. Chem. Lett. 2010;20(6):1873–1876. doi: 10.1016/j.bmcl.2010.01.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar M.I., Richardson J.H., Sanchez-Vargas I., Olson K.E., Beaty B.J. Dengue virus type 2: replication and tropisms in orally infected Aedes aegypti mosquitoes. BMC Microbiol. 2007;7:9. doi: 10.1186/1471-2180-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schindler C., Strehlow I. Cytokines and STAT signaling. Adv. Pharmacol. 2000;47:113–174. doi: 10.1016/s1054-3589(08)60111-8. [DOI] [PubMed] [Google Scholar]
- Screaton G., Mongkolsapaya J., Yacoub S., Roberts C. New insights into the immunopathology and control of dengue virus infection. Nature reviews. Immunology. 2015;15(12):745–759. doi: 10.1038/nri3916. [DOI] [PubMed] [Google Scholar]
- Seo W.Y., Ju S.M., Song H.Y., Goh A.R., Jun J.G., Kang Y.H., Choi S.Y., Park J. Celastrol suppresses IFN-gamma-induced ICAM-1 expression and subsequent monocyte adhesiveness via the induction of heme oxygenase-1 in the HaCaT cells. Biochem. Biophys. Res. Commun. 2010;398(1):140–145. doi: 10.1016/j.bbrc.2010.06.053. [DOI] [PubMed] [Google Scholar]
- Shresta S., Kyle J.L., Snider H.M., Basavapatna M., Beatty P.R., Harris E. Interferon-dependent immunity is essential for resistance to primary dengue virus infection in mice, whereas T- and B-cell-dependent immunity are less critical. J. Virol. 2004;78(6):2701–2710. doi: 10.1128/JVI.78.6.2701-2710.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon-Loriere E., Lin R.J., Kalayanarooj S.M., Chuansumrit A., Casademont I., Lin S.Y., Yu H.P., Lert-Itthiporn W., Chaiyaratana W., Tangthawornchaikul N., Tangnararatchakit K., Vasanawathana S., Chang B.L., Suriyaphol P., Yoksan S., Malasit P., Despres P., Paul R., Lin Y.L., Sakuntabhai A. High anti-Dengue virus activity of the OAS gene family is associated with increased severity of Dengue. J. Infect. Dis. 2015;212(12):2011–2020. doi: 10.1093/infdis/jiv321. [DOI] [PubMed] [Google Scholar]
- Ubol S., Masrinoul P., Chaijaruwanich J., Kalayanarooj S., Charoensirisuthikul T., Kasisith J. Differences in global gene expression in peripheral blood mononuclear cells indicate a significant role of the innate responses in progression of dengue fever but not dengue hemorrhagic fever. J. Infect. Dis. 2008;197(10):1459–1467. doi: 10.1086/587699. [DOI] [PubMed] [Google Scholar]
- Youn G.S., Kwon D.J., Ju S.M., Rhim H., Bae Y.S., Choi S.Y., Park J. Celastrol ameliorates HIV-1 Tat-induced inflammatory responses via NF-kappaB and AP-1 inhibition and heme oxygenase-1 induction in astrocytes. Toxicol. Appl. Pharmacol. 2014;280(1):42–52. doi: 10.1016/j.taap.2014.07.010. [DOI] [PubMed] [Google Scholar]
- Yu C.Y., Chang T.H., Liang J.J., Chiang R.L., Lee Y.L., Liao C.L., Lin Y.L. Dengue virus targets the adaptor protein MITA to subvert host innate immunity. PLoS Pathog. 2012;8(6):e1002780. doi: 10.1371/journal.ppat.1002780. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.