On March 11, 2020, a novel human coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become pandemic [1]. By March 24, 372.757 SARS-CoV-2 confirmed cases and 16.231 related deaths have been reported worldwide [2]. In Italy, 62.844 cases and 5.542 deaths have been reported, mostly in northern regions. Detailed data are updated by the Italian National Institute of Health [3].
Short abstract
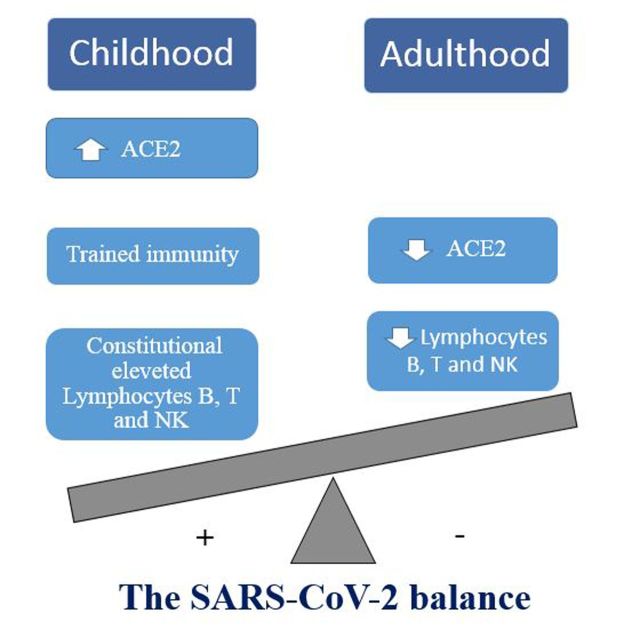
Epidemiological evidences show that SARS-CoV-2 infection in children is less frequent and severe than adults. Age-related ACE2 receptor expression, lymphocyte count and trained immunity might be the keystone to reveal children's secret.
On March 11, 2020, a novel human coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become pandemic [1]. By March 24, 372.757 SARS-CoV-2 confirmed cases and 16.231 related deaths have been reported worldwide [2]. In Italy, 62.844 cases and 5.542 deaths have been reported, mostly in northern regions. Detailed data are updated by the Italian National Institute of Health [3].
Available reports suggest that SARS-CoV-2 infection in children appears to be unusual. Among 44.672 confirmed cases, Chinese Centre of Disease Control and Prevention report showed 416 paediatric confirmed cases in 0–9 years age group (0.9%) with no fatalities and 549 cases in 10–19 years age group (1.2%) with 1 fatality (0.2%) [4]. Latest Italian report showed similar results with 318 (0.5%) confirmed cases in 0–9 years age group and 386 (0.7%) confirmed cases in 10–19 years age group. No children were recovered in the intensive care unit and no deaths were reported [5].
Since respiratory viral infection are usually more common in children under 5 years of age compared to adults, experts started to question which could be the children hidden secret [6, 7]. A recent study seems to point out that children are just as likely adults to get infected with SARS-CoV-2 [8]. A report from the town of Vo’ Euganeo (Veneto, Italy) - supposed to be one of the two starting outbreak spots in northern Italy - showed opposite results. From February 22, to March 5, 2020, 2.778 people were tested for SARS-CoV-2 out of 3.500 inhabitants. Swab tests were done also in asymptomatic inhabitants. Collected data showed that only 2 out of 316 swabs resulted positive in children under 14 years of age [9]. Data on susceptibility to SARS-CoV-2 according to children age are conflicting. Yuanyuan et al. retrospectively analysed epidemiological characteristics of 2143 children affected by SARS-CoV-2 infection in China, supporting the evidence that children are as susceptible as adults to infection. They found an elevated vulnerability to SARS-CoV-2 among infants, with a proportion of severe and critical cases of 10.6% in this age group (40 out 379 infants) [10]. However, the majority of severe and critical cases in the study were not SARS-CoV-2 confirmed, opening the debate whether other untested pathogens could have been responsible of such clinical pictures [11]. In fact, Sun et al. showed that among 8 children (age range: 2 months–15 years), who were admitted in the intensive care unit, only 2 (25%) were under the age of 12 months [12].
The reasons still remain unclear. The interaction between host immunological response and viral pathogenetic mechanisms might be the keystone.
The doorway
Angiotensin-converting enzyme 2 (ACE2) is a type I membrane protein expressed in many organs such as lungs (type II alveolar epithelial cells), heart, intestine and kidneys where is physiologically involved in maturation of angiotensin II (angII) [13, 14]. ACE2 has been proven to be the functional receptor of severe acute respiratory syndrome-associated coronavirus (SARS-CoV) and, recently, of SARS-CoV-2 [14, 15]. Xu et al. found an almost identical 3-D structure in the receptor-binding domain of SARS-CoV and SARS-CoV-2 spike proteins [16]. Full-length elucidation of ACE2 structure also suggests a stronger binding affinity of SARS-CoV-2 to ACE2 along with a more efficient receptor recognition, which may have strong human-to-human transmission implications [16, 17]. Crucially, SARS-CoV and Human Coronavirus NL63 infections were shown to downregulate ACE2 protein expression [18]. ACE2 key role is the angII conversion to its metabolite angiotensin-(1–7) (Ang1–7), especially in lung microenvironment, where ACE2 levels are intrinsically elevated. Ang1–7 has a homeostatic role in the regulation of the renin-angiotensin system (RAS), with anti-hypertensive and pro-fibrotic effects [19, 20]. As a matter of fact, elevation of ACE or low expression of ACE2 can lead to hypertension, chronic heart failure and lung injury [20]. Therefore, since ACE2 seems to act in a protective manner, SARS-CoV-2 could unbalance Ang II/Ang1–7 level and thus lead to inflammation and hypoxia [21].
However, the effect of RAS derangement is not clear. Low level of ACE2 has been detected in patients with underlying chronic conditions, which normally do not affect paediatric population [20, 21, 22]. In a study by Xudong et al., ACE2 was seen to dramatically decrease with aging in rat models [23]. Chen et al. publication encompassing ACE2 genomics, epigenomics and transcriptomics data, supports the evidence that young people seem to be less susceptible to virus detrimental effects, suggesting a negative correlation between ACE2 expression and SARS-CoV-2 severe outcomes [24]. Furthermore, according to their analysis both estrogens and androgens, which decrement is well known with aging, have shown to upregulate ACE2 expression [24, 25]. These evidences may suggest that the increase concentration of ACE2 receptors in lung pneumocytes in children may have a protective effect on severe clinical manifestations due to SARS-CoV-2 infection.
The crux
The SARS-CoV-2 viral genome has been sequenced and it is 75 to 80% identical to the SARS-CoV [26]. Genetic and clinical evidences suggest that SARS-CoV-2 has similar pathogenetic mechanisms to SARS-CoV and MERS-CoV [27, 28].
Innate immune cells recognise pathogen-associated molecular patterns (PAMPs) by pattern recognition receptors (PRRs) that include Toll-like receptors (TLRs) and other cytosolic pathogen sensors. PRRs set off the activation of the downstream signalling cascade that lead to the production of type I and III interferons (IFNs) and other proinflammatory mediators which initiate the host innate and adaptive immune response. Type I IFNs activate JAK/STAT pathway which plays a critical role in regulating immune response; IFNs can also directly activate immunity through dendritic cells stimulation and they also increase cytotoxic T and NK cells activity [29]. Moreover, NK cells migrate to the infected sites and respond to viruses producing IFN-gamma, killing virus-infected cells and boosting the adaptive immune response [29]. Cytokines and IFNs facilitate inflammation but they are also answerable for lung injury during acute viral infection. In SARS-CoV-2 severe cases, patients have high levels of innate pro-inflammatory cytokine and type I IFNs. Similarly to SARS-CoV and MERS-CoV infections, several reports show increased neutrophil and reduced lymphocyte counts in SARS-CoV-2 patients with the onset of the so called “cytokine storm”, supporting the hypothesis of the importance of innate immune response as both a protective and a destructive mechanism [27].
Milder disease presentation in children might be linked to “trained immunity”. “Trained immunity” represents an innate immune memory and it is formed by innate immunity cells that became “memory cells” after antigen exposure [30]. Mitroulis et al. demonstrated that systemic antigens determine transcriptomic, metabolomic, and functional changes in haemopoietic progenitor leading to the generation of myeloid cells with a faster responsiveness to infections [31]. These modifications not only occur in bone marrow but also in NK cells and innate lymphoid cells group 2 (ILC2). Lung ILC2 were shown to be able to remember their activation status if stimulated by inhaled allergens [32]. Cytomegalovirus and Influenza A can trigger a stronger NK mediated secondary innate immune response if exposed to reinfections [33]. It is demonstrated that common epigenetic mechanisms determine memory cells development both in the adaptive and in innate immune system [34]. Trained immunity memory is mediated by epigenetic modifications in haemopoietic progenitor and in cells of the innate immunity; it represents a cross protection against various pathogens and it can be activated also by vaccines [30]. After pathogen exposure, antigen-presenting cells increased activation leads to a nonspecific resistance of the host to reinfection providing cross-protection to other infections. It is also assumed that vaccines could induce cross-reactivity, training the innate immune system. A growing body of evidence suggests that measles-vaccinated children have a reduction in mortality rates that cannot be explained only by the prevention of measles-related deaths [35]. Several papers have examined the immunomodulating effect of influenza vaccination through the elicitation of NK cytotoxic response. Mysliwska et al. investigated the relationship between NK activity in the vaccinated population and specific immune protection against influenza virus and non-specific immune protection against other infections. Monitoring NK activity before and after immunisation, they found it was still significantly elevated 1 month apart. They concluded that NK cells activation may confers protection against influenza and other respiratory viral infections [29]. Both frequent viral infections and vaccines in children could induce an innate immune system enhanced state of activation, which would result in more effective defence against different pathogens [35]. A relatively low benefit from trained immunity (partial immunisation status and underexposure to viral infections) may justify the epidemiological evidences of more severe clinical presentation among SARS-CoV-2 infected infants compared to older children [10]. Moreover, human neonatal antigen-presenting cells and plasmacytoid dendritic cells have impaired production of type I IFNs and present a bias against the production of Th1-cytokines [36]. Such polarisation, that allows beneficial microbial colonisation, leaves newborns more susceptible to pathogenic infections. The age-dependent maturation of the immune response occurs with repeated stimuli and results in an enhanced innate function (trained immunity), that may protect older children as discussed above.
Adaptive immune response plays also a crucial role in SARS-CoV-2 infection; proinflammatory mediators activate Th1 type immune response (CD4+ and CD8+ T cells) and B lymphocytes that cause an effective virus-specific antibody response [37]. Adults infected by SARS-CoV-2, especially those with a severe disease, usually have decreased lymphocyte count and lymphocytopenia [27, 38, 39]. In children with SARS-CoV-2, peripheral blood lymphocytes remain mostly in normal range, suggesting less immune dysfunction [30, 40]. In healthy children, this could be related to the fact that lymphocytes, especially NK cells, are constitutionally in greater amount than healthy adults. Lymphocyte count is very high in the first months of life and decreases in later childhood and in adolescence [41]. Moreover, lymphocytes could be higher in children even due to frequently experienced viral infections in childhood, as the result of an everlasting immune system activation in the first years of life.
Conclusion
We can speculate that high ACE2 receptor concentrations, trained immunity and a constitutional high lymphocyte count in children may partially explain the mild disease observed in this group of patients (fig. 1). Real reasons will probably remain a mystery fortunately because the number of infected children is too low to allow good-sized immunological studies.
FIGURE 1.
The figure illustrates the theoretical constructs and putative immunological and pathogenetic differences between children and adults relative to SARS-CoV-2 infection Legend: unlike adults, children show constitutionally elevated ACE2 expression and lymphocyte count. Moreover, they undergo several viral infections and scheduled immunizations, which may boost their innate and adaptive immunity.
Footnotes
Conflict of interest: Dr. Cristiani has nothing to disclose.
Conflict of interest: Dr. Mancino has nothing to disclose.
Conflict of interest: Dr. Matera has nothing to disclose.
Conflict of interest: Dr. Nenna has nothing to disclose.
Conflict of interest: Dr. Pierangeli has nothing to disclose.
Conflict of interest: Dr. Scagnolari has nothing to disclose.
Conflict of interest: Dr. Midulla has nothing to disclose.
References
- 1. www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 WHO Director-General's opening remarks at the media briefing on COVID-19–11 March 2020.
- 2.WHO www.who.int/docs/default-source/coronaviruse/situation-reports/20200324-sitrep-64-covid-19.pdf?sfvrsn=703b2c40_2 Coronavirus disease 2019 (COVID-19) Situation Report – 64. Date last updated: March 24, 2020.
- 3.Istituto Superiore di Sanità Sorveglianza Integrata COVID-19 in Italia www.epicentro.iss.it/coronavirus/bollettino/Infografica_24marzo%20ITA.pdf. Date last updated: March 24, 2020
- 4.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi, 41: 145, 2020. [Google Scholar]
- 5.Istituto Superiore di Sanità www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_23-marzo%202020.pdf Epidemia COVID-19 Aggiornamento Nazionale. . Date last updated March 23, 2020.
- 6.Lee P, Hu YL, Chen PY, et al. Are children less susceptible to COVID-19?. J Microbiol Immunol Infec 2020: S1684-1182(20)30039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monto AS, Ullman BM. Acute respiratory illness in an American community. The Tecumseh Study. JAMA 1974; 227: 164–169. doi: 10.1001/jama.1974.03230150016004 [DOI] [PubMed] [Google Scholar]
- 8.Qifang B, Yongsheng W, Shujiang M, et al. Epidemiology and Transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1286 of their close contacts. MedRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Regione Veneto Azienda Zero. Esito dei tamponi eseguiti nella popolazione di Vo’ (PD) www.it.scribd.com/document/450608044/Coronavirus-Regione-Veneto-Azienda-Zero pdf#from_embed
- 10.Dong Y, Mo X, Hu Y, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics 2020: e20200702.32179660 [Google Scholar]
- 11.Ludvigsson JF. Systematic review of COVID-19 in children show milder cases and a better prognosis than adults. Acta Paediatr 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun D, Li H, Lu XX, et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center's observational study. World J Pediatr 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu Z, Zixian Z, Yujia W, et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv 2020. doi: 10.1101/2020.01.26.919985 [DOI] [Google Scholar]
- 14.Yan R, Zhang Y, Li Y, et al. Structural basis for the recognition of the SARS-CoV-2 by full-length human ACE2. Science 2020; 367: 1444–1448. doi: 10.1126/science.abb2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li W, Moore MJ, Vasilieva N, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 2003; 426: 450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu X, Chen P, Wang J, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modelling of its Spike protein for risk of human transmission. Sci China Life 2020; 63: 457–460. doi: 10.1007/s11427-020-1637-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li F, Li W, Farzan M, et al. Structure of SARS coronavirus Spike receptor-binding domain complexed with receptor. Science 2005; 309: 1864–1868. doi: 10.1126/science.1116480 [DOI] [PubMed] [Google Scholar]
- 18.Glowacka I, Bertram S, Herzog P, et al. Differential Downregulation of ACE2 by the Spike Proteins of Severe Acute Respiratory Syndrome Coronavirus and Human Coronavirus NL63. J Virol 2010; 84: 1198–1205. doi: 10.1128/JVI.01248-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrario CM, Chappell MC, Tallant EA, et al. Counterregulatory actions of angiotensin- (1-7). Hypertension 1997; 30: 535–541. [DOI] [PubMed] [Google Scholar]
- 20.Tikellis C, Thomas MC. Angiotensin-Converting Enzyme 2 (ACE2) Is a Key Modulator of the Renin Angiotensin System in Health and Disease. Int J Pept 2012; 2012: 256294. doi:1155/2012/256294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sodhi CP, Wohlford-Lenane C, Yamaguchi Y, et al. Attenuation of pulmonary ACE2 activity impairs inactivation of des-Arg9 bradykinin/BKB1R axis and facilitates LPS-induced neutrophil infiltration. Am J Physiol Lung Cell Mol Physiol 2018; 314: L17–L31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watkins J. Preventing a covid-19 pandemic. BMJ 2020; 368: m810. doi: 10.1136/bmj.m810 [DOI] [PubMed] [Google Scholar]
- 23.Xie X, Xudong X, Chen J, et al. Age- and gender-related difference of ACE2 expression in rat lung. Life Sci 2006; 78: 2166–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen J, Jiang Q, Xia X, et al. Individual Variation of the SARS-CoV2 Receptor ACE2 Gene Expression and Regulation. Preprints 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horstman A, Dillon M, Urban EL, et al. The role of androgens and estrogens on healthy aging and longevity. J Gerontol A Biol Sci Med Sci 2012; 67: 1140–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou P, Yang X-L, Wang X-G, et al. Discovery of a novel coronavirus associated with the recent pneumonia outbreak in 2 humans and its potential bat origin. BioRxiv 2020. [Google Scholar]
- 27.Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol 2020; 38: 1–9. doi: 10.12932/AP-200220-0772 [DOI] [PubMed] [Google Scholar]
- 28.Newton AH, Cardani A, Braciale TJ. The host immune response in respiratory virus infection: balancing virus clearance and immunopathology. Semin Immunopathol 2016; 38: 471–482. doi: 10.1007/s00281-016-0558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myśliwska J, Trzonkowski P, Szmit E, et al. Immunomodulating effect of influenza vaccination in the elderly differing in health status. Exp Gerontol 2004; 39: 1447–1458. doi: 10.1016/j.exger.2004.08.005 [DOI] [PubMed] [Google Scholar]
- 30.Cao Q, Chen Y-C. SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. J Formos Med Assoc 2020; 119: 670–673. doi: 10.1016/j.jfma.2020.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mitroulis I, Ruppova K, Wang B, et al. Modulation of Myelopoiesis progenitors is an integral component of trained immunity. Cell 2018; 172: 147–161, e112. doi: 10.1016/j.cell.2017.11.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Halim TY, Steer CA, Matha L, et al. Group 2 innate lymphoid cells are critical for the initiation of adaptive T helper 2 cell-mediated allergic lung inflammation. Immunity 2014; 40: 425–435. doi: 10.1016/j.immuni.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mehta D, Petes C, Gee K, et al. The role of virus infection in deregulating the cytokine response to secondary bacterial infection. J Interferon Cytokine Res 2015; 35: 925–934. doi: 10.1089/jir.2015.0072 [DOI] [PubMed] [Google Scholar]
- 34.Lau CM, Adams NM, Geary CD, et al. Epigenetic control of innate and adaptive immune memory. Nat Immunol 2018; 19: 963–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Christine SB, Mihai GN. A small jab – a big effect: nonspecific immunomodulation by vaccines. Trends Immunol 2013; 34: 431–439. doi: 10.1016/j.it.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 36.Levy O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat Rev Immunol 2007; 7: 379–390. doi: 10.1038/nri2075 [DOI] [PubMed] [Google Scholar]
- 37.Medzhitov R, Janeway C Jr. Innate immunity: impact on the adaptive immune response. Curr Opin Immunol 1997; 9: 4–9. doi: 10.1016/S0952-7915(97)80152-5 [DOI] [PubMed] [Google Scholar]
- 38.Nicholls JM, Poon LL, Lee KC, et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet 2003; 361: 1773–1778. doi: 10.1016/S0140-6736(03)13413-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mahallawi WH, Khabour OF, Zhang Q, et al. MERS-CoV infection in humans is associated with a pro-inflammatory Th1 and Th17 cytokine profile. Cytokine 2018; 104: 8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang YH, Lin DJ, Xiao MF, et al. 2019 novel coronavirus infection in a three-month-old baby. Zhonghua Er Ke Za Zh 2020; 58: E006. [DOI] [PubMed] [Google Scholar]
- 41.Tosato F, Bucciol G, Pantano G, et al. Lymphocytes Subsets Reference Values in Childhood. Cytometry A 2014. [DOI] [PubMed] [Google Scholar]