Abstract
Background:
Some women who enter pregnancy in a healthy state may survive with serious complications while others may die. This study sets out to determine the frequency of maternal near-miss (MNM) and maternal death. It also intended to identify common causes and determinants.
Materials and Methods:
This was a cross-sectional study from June 2012 to May 2013 that involved women who were admitted for delivery, within 42 days of delivery or termination of pregnancy and those who died from pregnancy, childbirth, or puerperal complications. Data obtained were analyzed using Epi info 2002.
Results:
There were 105 maternal near misses and deaths. Nineteen of them were mortalities, whereas 86 were MNMs. The maternal mortality ratio over the period was 806/100,000 live births and near miss was 3649/100,000 live birth. Hypertensive disorders in pregnancy were the leading cause of maternal deaths (47.36%) and MNMs (47.7%). Maternal deaths (57.9%) and near misses (43%) were the highest among those that treatment was instituted after 60 min and within 30–60 min of diagnosis, respectively. The consultants were the highest level of expertise involved in the management of 73.3% and this group recorded the least maternal death and highest MNM.
Conclusion:
Hypertensive disorder was the leading cause of MNM and mortality. Involving the highest level of expertise in patient management and reducing the time interval between diagnoses and instituting definitive treatment is essential for a better outcome. Health institutions will benefit from the evaluation of their quality of obstetric care by including near miss investigations in their maternal death enquiries.
Keywords: Maternal mortality, maternal near miss, pregnancy
INTRODUCTION
Most women will progress through pregnancy in an uncomplicated fashion and deliver healthy infants requiring little medical or midwifery intervention. Unfortunately, a significant number will have medical problems that will complicate their pregnancy or develop such serious conditions that the lives of both themselves and their unborn child will be threatened.1
Women who survived severe complications during pregnancy, childbirth, and the postpartum period could serve as surrogates to help us gain a better understanding of the set of conditions and preventable factors that together contribute to maternal death.1 This is known as the concept of maternal near-miss (MNM)2 recently defined by the World Health Organization (WHO), after some controversy,3 as the near death of a woman from a complication during pregnancy, childbirth or within 42 days after the termination of pregnancy.4
Maternal mortality (MM), on the other hand, is the death of a woman while pregnant or within 42 days of termination of pregnancy, from any cause related to, or aggravated by, the pregnancy or its management but not from accidental or incidental causes.5 The MM ratio as of February 2013 in Nigeria was 630 deaths/100,000 live births.6
Some of the causes of MNM include obstetrical hemorrhage, anemia, dystocia, severe hypertensive disorders in pregnancy, and infections.7 The direct causes resulting from obstetric complications of the pregnant state, from interventions or omission will include severe hemorrhage, eclampsia, infection, obstructed labor, and unsafe abortion. Indirect causes of MM result from the previous existing diseases or diseases that occurred during pregnancy and which was not due to direct obstetric causes, but which was aggravated by the physiologic effect of pregnancy that are due to indirect or direct maternal causes, for example, death from cardiac disease in pregnancy.7
MNM occurs more frequently than MM. In low-income countries, near misses are often considered obstetric successes because ultimately the woman's life was saved by a focused medical intervention.1,8 However, little is known about long-term outcomes following these complications.2 Studies have documented a substantial degree of physical and psychological morbidity in their aftermath3,4,5,7,9,10 and the high cost of emergency obstetric care has serious social and economic consequences.7 It has been shown that for every 7 women who survived life-threatening complications, one died.9 MNM will, therefore, generate information as the women themselves can be a source of information to enable identification of the common causes. This will, in turn, enable a reduction in the MM.
Effective interventions to reduce mortality and morbidity in maternal and newborn health already exist. Information about the quality and performance of care and the use of critical interventions are useful for shaping improvements in healthcare and strengthening the contribution of health systems. The near-miss concept and the criterion-based clinical audit are proposed as useful approaches for obtaining such information in maternal and newborn health care.10 We, therefore, sought to determine the frequency of MNM and maternal death among women managed at the Jos University Teaching Hospital, to identify the common causes of near miss/MM and to identify the determinants responsible for MNM and maternal deaths.
MATERIALS AND METHODS
This was a cross-sectional study done for 1 year from June 2012 to May 2013 as part of a nationwide MM/near miss study.11 This involved women who were admitted for delivery within 42 days of delivery or termination of pregnancy and those who died from pregnancy, childbirth or puerperal complications.
Ethical clearance obtained for the institution as part of the national survey for MNM and mortality was used for this study.
All women who received antenatal care within the hospital or from other hospitals but were admitted with complications in pregnancy during the study were included using the WHO criteria for maternal death and near miss.
The data were collected from the obstetric ward, gynecological ward, labor room, and the intensive care unit records using a data form when admitted and this was further updated from the medical records of the patients at the time of discharge or death. Data analysis was performed using Epi info 2002.
RESULTS
During the period of the study, a total number of births were 2439; live births were 2357, stillbirths 82, and 53 of them were twin birth. There were 105 maternal near misses and deaths. Nineteen of them were mortalities, while 86 were MNMs.
Majority of the study participants were aged between 20 and 34 years, had secondary education and were of low-socioeconomic class and had received antenatal care as shown in Table 1.
Table 1.
Maternal sociodemographic characteristics
| Parameter | Frequency (mortality) | Frequency (MNM) | Total |
|---|---|---|---|
| Age, n (%) | |||
| 15-19 | 1 (5.26) | 3 (3.49) | 4 (3.81) |
| 20-24 | 4 (21.05) | 11 (12.79) | 15 (14.29) |
| 25-29 | 7 (36.84) | 28 (32.56) | 35 (33.33) |
| 30-34 | 5 (26.31) | 26 (30.23) | 31 (29.52) |
| >34 | 2 (10.52) | 18 (20.93) | 20 (19.05) |
| Educational status, n (%) | |||
| None | 5 (41.7) | 7 (58.3) | 12 (100) |
| Primary | 5 (22.7) | 17 (77.3) | 22 (100) |
| Secondary | 8 (21) | 30 (79) | 38 (100) |
| Tertiary | 1 (3) | 32 (97) | 33 (100) |
| Religion, n (%) | |||
| Christian | 11 (14.3) | 66 (85.7) | 77 (100) |
| Muslim | 8 (28.6) | 20 (71.4) | 28 (100) |
| Social class, n (%) | |||
| Low | 15 (25.9) | 43 (74.1) | 58 (100) |
| Middle | 3 (7.3) | 38 (92.7) | 41 (100) |
| High | 1 (16.7) | 5 (83.3) | 6 (100) |
| Marital status, n (%) | |||
| Married | 17 (17.5) | 80 (82.5) | 97 (100) |
| Unmarried | 2 (25) | 6 (75) | 8 (100) |
| Parity, n (%) | |||
| ≤4 | 13 (21.3) | 48 (78.7) | 61 (100) |
| >4 | 6 (13.6) | 38 (86.4) | 44 (100) |
| Antenatal care, n (%) | |||
| Booked | 12 (16.2) | 62 (83.8) | 74 (100) |
| Unbooked | 7 (22.6) | 24 (77.4) | 31 (100) |
MNM – Maternal near miss
The MM ratio over the period was 806/100,000 live births. Hypertensive disorders in pregnancy were the leading cause of maternal death accounting for 47.36%. Anemia (from causes other than hemorrhage) as well as infections (chorioamnionitis, genital sepsis and systemic sepsis) accounted for 15.8% each. Embolic disease, postpartum hemorrhage, heart disease, and HIV/AIDS were responsible each for 5.26% of maternal death [Table 2].
Table 2.
Causes of maternal deaths and near misses
| Pathology | Frequency (%) |
|
|---|---|---|
| Deaths | Near miss | |
| Hypertensive diseases | 9 (47.36) | 41 (47.7) |
| Anemia | 3 (15.80) | 0 (0) |
| Infection | 3 (15.80) | 5 (5.8) |
| Embolic disease | 1 (5.26) | 0 (0) |
| Hemorrhage | 1 (5.26) | 32 (37.2) |
| Heart disease | 1 (5.26) | −0 (0) |
| Dystotic labor | −0 (0) | 4 (4.7) |
| HIV/AIDS | 1 (5.26) | 1 (1.2) |
| Others* | −0 (0) | 3 (3.4) |
| Total | 19 (100) | 86 (100) |
*Others – Severe anemia, cardiac disease, and sickle cell disease crises
The MNM rate during the study period was 3649/100,000 live birth. Hypertensive disorder of pregnancy accounted for the highest cause of MNM being 47.7%. Hemorrhage accounted for 37.2%, infection 5.8%, and dystocic labor was 4.7%. HIV/AIDS/Wasting syndrome was responsible for 1.2% [Table 2].
Maternal death was the highest being 57.9% among those that treatment was instituted after 60 min of diagnosis [Table 3]. MNM was also the highest among those whose treatment commenced within 30–60 min of diagnosis as shown in Table 3.
Table 3.
Outcome for time interval between diagnosis and treatment
| Time (min) | Death, n (%) | Near miss, n (%) |
|---|---|---|
| <10 | 4 (21) | 4 (4.7) |
| 10-19 | 1 (5.3) | 11 (12.8) |
| 20-29 | 1 (5.3) | 7 (8.1) |
| 30-60 | 2 (10.5) | 37 (43) |
| >60 | 11 (57.9) | 27 (31.4) |
| Total | 19 (100) | 86 (100) |
During the study period, the consultants were the highest level of expertise involved in the management of 73.3% of the patients, while the senior registrar accounted for 24.7%. The junior resident was the highest level of expertise in 2% of the cases [Figure 1]. The involvement of consultants in patient management had a better outcome as shown in Figure 1.
Figure 1.
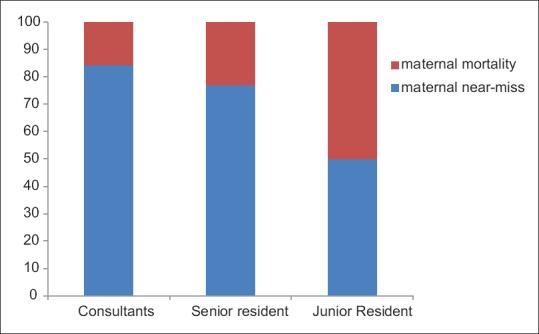
Outcome of patient management across level of expertise
DISCUSSION
In this study, the MM ratio was 806/100,000 live birth, which is very high when compared to the worldwide figure and also to that of Nigeria which is 630/100,000 live birth.6 There is a need to ensure a reduction in this value.
Hypertensive disorder of pregnancy (47.36%) was found to be the leading cause of death. This was followed by anemia (causes other than hemorrhage) and infections which both accounted equally for 15.80%. This is similar to the findings of a study from Sagamu, Nigeria done by Oladapo et al., which showed that hypertensive disorder (31.4%) and hemorrhage (29%) were the leading causes of maternal death.12 This finding may be due to poor health-seeking behavior of women in our environment;13,14 hence, hypertensive disorders are not picked up early during antenatal care and appropriately managed to prevent morbidities and mortality. There is also probably an improvement in active management of the third stage of labor and also proper use of antibiotics, especially after delivery in our center which has reduced the causes from postpartum hemorrhage and infection, respectively. However, worldwide, the leading cause of maternal death is postpartum hemorrhage which is followed by infection and hypertensive disorder in pregnancy accounting for 25%, 15%, and 12% respectively.15
A study to determine the worldwide MNM rate, showed a value of 3648/100,000 live births and hypertensive disorder was the leading cause of MNM (47.7%).10 This was followed by obstetric hemorrhage (37.2%) while infection (5.8%) was the third. This shows that hypertensive disorder of pregnancy is a common cause of near-miss in our environment as well. A study done in Damascus, Syria by Almerie et al. to investigate the frequency and nature of near miss and also to evaluate the level of care at maternal life-saving emergency services to aid appropriate distribution of fund in the health sector showed that hypertensive disorders (52%) and hemorrhage (34%) were the top causes of MNMs16 which is in keeping with the outcome of this study. The study at Sagamu in Nigeria also revealed that hypertensive disorders and hemorrhage were responsible for majority of the near-miss event which is similar to the outcome in this study.12 The overall maternal death to near-miss ratio was 1:4.5 which is comparable with the study done in Sagamu with a value of 1:4.8.12
Majority of the women (92.4%) were married and this group of women had near miss and mortality of 82.5% and 17.5%, respectively. Those that were unmarried had 75% and 25% for near miss and mortality, respectively. This may have been accounted for by inadequate social, emotional and financial support for these women in seeking medical care as opposed to the situation among the married.
More than half of the women (55.2%) in the study were of low social class, while 39% were in the middle class. The least distribution of 5.8% was in the high social class. In those belonging to the low social class, MM was the highest being 25.9%. Those in the middle class had the highest MNM of 92.7% as well as the least mortality (7.3%). The high social class had a MNM and mortality of 83.3% and 16.7%, respectively. These findings may have been accounted for by the lack of financial support to access healthcare among those in the low social class. The high social class had a distribution that may have been skewed as those in this class accounted for just 5.8% of the women in the study.
Women with parity <4 accounted for 58.1%, while those with parity of >4 accounted for 41.9% of the total women. Women with parity of <4 had higher MM (21.6%) compared with those with parity of >4 (13.6%). The near misses distribution was the reverse being 78.7% among those with parity of <4 and 86.4% among those with parity of >4. Hypertensive disorder of pregnancy is common among women with low parity and being the leading cause of mortality in the study, it is no wonder that the mortality is higher among those with parity of <4. A study in Bauchi showed high MM among primigravida and adolescents with eclampsia (31.9%), hemorrhage (19.2%), and sepsis (10.4%) being the leading direct causes of maternal death further supporting the findings from this study.17
Women who booked for antenatal care accounted for 70.5% of the total, while 29.5% were unbooked. Among the unbooked, the mortality was higher (22.6%) compared to the booked women. Near misses were more among those who booked being 83.8% as majority of them survived complications following better antenatal care compared to the unbooked that had a lower MNM of 77.4%. The importance of good antenatal care cannot be overemphasized as this will help in detecting these leading causes of MNM and mortality as well as aid appropriate management for better outcomes.
Among the women with tertiary education, the MM was the least being 3% while the MNM was the highest being 97%. Those in the group with no form of formal education had the highest MM of 41.7% and the least MNM of 58.3%. The more enlightened the women are, the better the health-seeking behavior to avert complications as shown in the study.
The interval between diagnosis and institution of management analyzed showed that the highest mortality being 57.9% occurred among those that management was instituted after 60 min. The same thing was noticed among the near-miss group as 43% being the highest occurred in those whose definitive management was instituted between 30 and 60 min. A need to improve approach, improving attitude to work as well as the development of protocols for management will go a long way in averting some of these delays. Unfortunately, the exact reason for this delay was not documented in the notes of the patients hence a need for emphasis.
Various level of expertise was involved in the management of women during the study. Of all the women managed during the study, 73.3% of them had consultants as the highest form of expertise. The highest form of expertise in 24.7% of the women was by senior residents, while only 2% was by junior residents. The highest mortality of 50% was recorded among those manage by the junior resident while the least of 15.6% was among those managed by the consultants. The highest MNMs of 84.4% was recorded among those managed by the consultants, while the least of 50% among those with the junior residents as the highest level of expertise. The knowledge and experience of the consultant in reducing MM as well as improving outcomes cannot be overemphasized as shown in the study.
The multi-center study on near miss and MM has been recently published,11 and the findings are in tandem with that obtained in this study. Hypertensive disorders and obstetric hemorrhage were found to be the leading cause of MNM and MM. Outcomes of the hospital in terms of women surviving specific complications were better for obstetric hemorrhage than hypertensive disorder making hypertensive disorder the leading cause of maternal death.
Limitation of the study
It was a single hospital study may also not be representative of maternal health in the community, hence a need for caution when interpreting the data. Reasons for the delay from diagnosis to instituting care were not objectively documented in the notes of the patients hence a need for proper documentation cannot be overemphasized for all patients.
CONCLUSION
The hypertensive disorder was the leading cause of MNM and mortality. Involving the highest level of expertise in patient management and reducing the time interval between diagnoses and instituting definitive treatment is essential for a better outcome. Necessary facilities for managing these life-threatening conditions should be made available. Furthermore, emergency drills should be conducted frequently to heighten index of suspicion and also combat deficiencies in the management of these life-threatening conditions.
Health education to improve health-seeking behavior using the media, social and religious gathering, as well as community outreaches will go a long way in encouraging women to book their pregnancy, thereby improving outcome. Health institutions will benefit from the evaluation of their quality of obstetric care by including near-miss investigations in their maternal death inquiries.
Recommendation
There is a need to evaluate the circumstances surrounding near misses and maternal death as this would give an insight into modifiable factors, especially for hypertensive disorders to enable a more focused remedial action. Things to be put in place to reduce the MM having identified the determinant such as developing protocols for management and involving the highest form of expertise in patient management will go a long way in improving outcome.
Furthermore, health education using the media and other religious gathering will create awareness as the importance of antenatal care in reducing disastrous outcome in pregnancy, during delivery and the puerperium cannot be overemphasized.
Further studies may be required to evaluate the incidence of hypertensive disorders in pregnancy to know if its rising or still at the same level but with a higher occurrence as the other causes of MM are being managed better.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The Centre for Research in Reproductive Health (CRRH), Sagamu, Nigeria coordinated the survey nationally. CRRH was financially supported by the Department of Reproductive Health and Research, World Health Organization, Geneva, Switzerland. The manuscript represents the views of the named authors only.
REFERENCES
- 1.George A, Timothy GO. Antenatal care. In: Edmonds DK, editor. Dewhurst's Textbook of Obstetrics and Gynaecology. 8th ed. UK: Blackwell Publishing; 2012. pp. 42–51. [Google Scholar]
- 2.Nashef SA. What is a near miss? Lancet. 2003;361:180–1. doi: 10.1016/S0140-6736(03)12218-0. [DOI] [PubMed] [Google Scholar]
- 3.Say L, Pattinson RC, Gülmezoglu AM. WHO systematic review of maternal morbidity and mortality: The prevalence of severe acute maternal morbidity (near miss) Reprod Health. 2004;1:3. doi: 10.1186/1742-4755-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Say L, Souza JP, Pattinson RC. WHO working group on Maternal Mortality and Morbidity classifications. Maternal near miss – Towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. 2009;23:287–96. doi: 10.1016/j.bpobgyn.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Baker PN, editor. Obstetrics by Ten Teachers. 18th ed. UK: Book Power Publishers; 2006. Maternal and perinatal mortality: The confidential enquiry; pp. 125–45. [Google Scholar]
- 6.Maternal Mortality Ratio (Modelled Estimate, per 100,00 live Birth), Trends in Maternal Mortality 1990-2010. Estimate Developed by WHO, UNICEF, UNFPA, and World Bank. Catalogue Services World Development Indicators. [Last accessed on 2014 Jan 06]. Available from: http://www.data.worldbank.org .
- 7.Storeng KT, Drabo S, Ganaba R, Sundby J, Calvert C, Filippe V, et al. Mortality after near-miss obstetric complications in Burkina Faso: Medical, social and health-care factors. Bull World Health Organ. 2012;90:418–25C. doi: 10.2471/BLT.11.094011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pattinson RC, Buchmann E, Mantel G, Schoon M, Rees H. Can enquiries into severe acute maternal morbidity act as a surrogate for maternal death enquiries? BJOG. 2003;110:889–93. [PubMed] [Google Scholar]
- 9.Mustafa R, Hashmi H. Near-miss obstetrical events and maternal deaths. J Coll Physicians Surg Pak. 2009;19:781–5. [PubMed] [Google Scholar]
- 10.WHOMCS Research Group. Souza JP, Gülmezoglu AM, Carroli G, Lumbiganon P, Qureshi Z, et al. The world health organization multicountry survey on maternal and newborn health: Study protocol. BMC Health Serv Res. 2011;11:286. doi: 10.1186/1472-6963-11-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oladapo OT, Adetoro OO, Ekele BA, Chama C, Etuk SJ, Aboyeji AP, et al. When getting there is not enough: A nationwide cross-sectional study of 998 maternal deaths and 1451 near-misses in public tertiary hospitals in a low-income country. BJOG. 2016;123:928–38. doi: 10.1111/1471-0528.13450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oladapo OT, Sule-Odu AO, Olatunji AO, Daniel OJ. Near-miss obstetric events and maternal deaths in Sagamu, Nigeria: A retrospective study. Reprod Health. 2005;2:9. doi: 10.1186/1742-4755-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akeju DO, Oladapo OT, Vidler M, Akinmade AA, Sawchuck D, Qureshi R. Determinants of health care seeking behaviour during pregnancy in Ogun state, Nigeria. Reprod Health. 2016;13(Suppl 1):32. doi: 10.1186/s12978-016-0139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria – Looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43. doi: 10.1186/1471-2393-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. [Last accessed on 2014 Jan 28]. Available from: http://www.unfpa.org/mothers/facts.htm .
- 16.Almerie Y, Almerie MQ, Matar HE, Shahrour Y, Al Chamat AA, Abdulsalam A, et al. Obstetric near-miss and maternal mortality in maternity University hospital, Damascus, Syria: A retrospective study. BMC Pregnancy Childbirth. 2010;10:65. doi: 10.1186/1471-2393-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mairiga AG, Saleh W. Maternal mortality at the state specialist hospital Bauchi, Northern Nigeria. East Afr Med J. 2009;86:25–30. doi: 10.4314/eamj.v86i1.46924. [DOI] [PubMed] [Google Scholar]


