Highlights
-
•
This work describes a minimalist approach to the construction and validation of a coronavirus reverse genetics system utilizing homologous recombination for vector construction and a variety of molecular techniques for virus detection.
-
•
Homologous recombination in S. cerevisiae proves an efficient and fast method of constructing the large and complex genome of MERS-CoV, this strategy will be helpful for future construction of other virus genomes.
-
•
Detection of rescued virus by molecular assay (i.e.: RT-PCR) is a strong alternative to the more traditional immunological detection assays.
-
•
Rescued MERS-CoV was genomically and phenotypically similar to the original isolate MERS-CoV/EMC-2012.
Keywords: Coronavirus, Middle East Respiratory Syndrome, Infectious clone system, Molecular cloning, Reverse genetics, Homologous recombination
Abstract
Background
Viral Infectious clone systems serve as robust platforms to study viral gene or replicative function by reverse genetics, formulate vaccines and adapt a wild type-virus to an animal host. Since the development of the first viral infectious clone system for the poliovirus, novel strategies of viral genome construction have allowed for the assembly of viral genomes across the identified viral families. However, the molecular profiles of some viruses make their genome more difficult to construct than others. Two factors that affect the difficulty of infectious clone construction are genome length and genome complexity.
Results
This work examines the available strategies for overcoming the obstacles of assembling the long and complex RNA genomes of coronaviruses and reports one-step construction of an infectious clone system for the Middle East Respiratory Syndrome coronavirus (MERS-CoV) by homologous recombination in S. cerevisiae.
Conclusions
Future use of this methodology will shorten the time between emergence of a novel viral pathogen and construction of an infectious clone system. Completion of a viral infectious clone system facilitates further study of a virus’s biology, improvement of diagnostic tests, vaccine production and the screening of antiviral compounds.
1. Background
In June of 2012, the Middle East Respiratory Syndrome (MERS) coronavirus (CoV) was isolated from a patient suffering from symptoms of respiratory disease in Jeddah, Kingdom of Saudi Arabia (Zaki et al., 2012). MERS-CoV genetically clusters with the bat coronaviruses Neoromicia/PML, HKU4-1 and HKU5-1 which occupy lineage C of the betacoronaviridae, no other identified human coronavirus exists within this genus (Raj et al., 2014). Epidemiological studies of MERS-CoV implicate camels as a possible zoonotic host (Memish et al., 2014, Reusken et al., 2013). Since its emergence, MERS-CoV has spread between 26 countries causing 1375 laboratory confirmed cases and 587 deaths (ECDC, 2015, ProMED-mail, 2016). No other coronavirus has so greatly impacted public health, or global economics since severe acute respiratory syndrome coronavirus (SARS-CoV) in 2002 (Hilgenfeld and Peiris, 2013). The unexpected introduction of SARS-CoV and MERS-CoV into the human population combined with a lack of current antiviral therapies or vaccines to protect the public from coronavirus related disease, makes study of these and similar viruses important to public health. In order to improve the timeline between discovery of a novel coronavirus and completion of an infectious clone system, we undertook the rapid construction of the MERS-CoV cDNA genome EMC/2012 (JX869059.2) by homologous recombination in S. cerevisiae.
Virus infectious clone systems allow for the expression of a homogenous virus population within mammalian cell culture from a sequence of DNA or RNA (Ebihara et al., 2005). The construction of such systems for RNA viruses involves several steps: 1) possession of a virus isolate, 2) sequencing of the viral genome, 3) reverse transcription of the viral RNA genome to complementary DNA (cDNA) and 4) assembly of the PCR cDNA amplicons into the full-length genome. The timing and technical expertise required to perform these steps depends on the type of viral genome being constructed. Infectious clone systems for viruses with small un-fragmented positive sense RNA genomes are less demanding to construct than those with large negative sense, positive sense or fragmented genomes (Ebihara et al., 2005, Yount et al., 2000, Stobart and Moore, 2014).
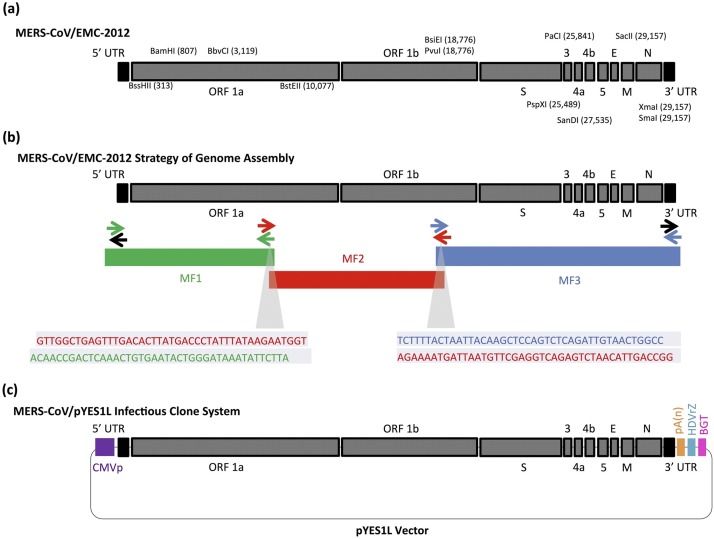
Construction of infectious clone systems for viruses of the Coronaviridae has lagged in comparison to those of other viral families because qualities of the coronavirus genome restrict the use of traditional molecular cloning techniques (Stobart and Moore, 2014). The prototypical coronavirus possesses a positive sense RNA genome from 27 to 32 kb in length. Multiple regions of sequence redundancy exist (Gorbalenya et al., 2006), whichdecrease the availability of unique restriction sites. The MERS-CoV genome (JX869059.2) has only 12 unique restriction sites (Fig. 1 a); their positions and the sizes of the corresponding DNA fragments preclude a simple cloning strategy. Highly cytotoxic regions have also been described within coronavirus genomes, which cause E. coli cloning strains to poorly tolerate plasmids carrying coronavirus genome cassettes (González et al., 2002, Yount et al., 2002). Performing polymerase chain reaction (PCR), especially reverse transcription PCR (RT-PCR) on coronavirus genomes proves troublesome, as the error rate of DNA polymerases increases in relation to copy number and amplicon size (Eckert and Kunkel, 1991). In combination, these factors make the assembly of coronavirus genome’s by traditional molecular cloning tedious and time consuming (Almazán et al., 2014, Enjuanes, 2005). Virologists have developed several alternative methods to overcome these obstacles; however, none of them allow for rapid construction and expression of a coronavirus infectious clone system. The attempted strategies include targeted RNA recombination, transfection of multiple or single plasmid vectors and vaccinia virus transduction. Almazan et al. conducted a concise summary of available strategies for coronavirus genome construction in their 2014 review. In summary, they concluded that several alternatives to conventional approaches have benefited the science of coronavirus genome construction over the last thirteen years. We hypothesize that construction of a coronavirus genome by homologous recombination within S. cerevisiae, will prove an additional efficient means to molecular cloning coronaviruses while preserving the strengths of the plasmid based method: long term stability and efficient expression (Fig. 1c) (Almazán et al., 2014).
Fig 1.
(a) Illustration of the MERS-CoV/EMC-2012 genome, the location of unique restriction sites are shown. (b) A full-length cDNA version of the MERS-CoV/EMC-2012 genome was assembled from three large fragments by homologous recombination. Primers sharing end homology are coded by color: black (vector), green (MF1), red (MF2) and blue (MF3). The full sequences of primers are shown in Table 1.0. (c) The complete MERS-CoV infectious clone system, including the pYES1L-BAC vector and regulator elements necessary for transcription of viral RNA (for interpretation of the references to color in this figure legend, the reader is referred to the online version of this article.)
2. Methods
2.1. Chemical synthesis of MERS-CoV cDNA, plasmid selection and primer design
Thirty-one, 1-kb gene fragments of the MERS-CoV EMC/2012 genome (NC_019843.2, JX869059.2) were chemically synthesized and cloned into the EcoR1 sites of pCR® 2.1 (Life Technologies) by Eurofins MWG Operon. The pYES1L-BAC vector (Life Technologies) was chosen for conducting homologous recombination in S. cerevisiae and maintenance of the completed MERS-CoV infectious clone system in E. coli. Primers were designed for stepwise assembly of the synthetic MERS-CoV gene fragments and amplifying products for homologous assembly in S. cerevisiae (Table 1.0 and Supplementary Table 1.0).
2.2. Assembly of MERS-CoV cDNA by polymerase chain reaction
The 1-kb MERS-CoV gene fragments and regulatory genetic elements (i.e. cytomegalovirus promoter, beta globulin terminator and hepatitis delta virus ribozyme) were stepwise assembled by splice-by-overlap extension polymerase chain reaction. Three large PCR amplicons were produced by this method ranging from: (MF1) CMVpF Start (TATTA)- EMC/2012 (6023 bp), (MF2) EMC/2012 (5981 bp)-EMC/2012 (18,020 bp) and (MF3) EMC/2012 (17,978 bp)- Beta-Globulin Terminator end (TGCTC). The three templates MF1, MF2 and MF3 were PCR amplified using primers with ∼30 bps of homology to the neighbouring fragment or blunt ends of the pYES1L vector (Fig. 1b) (Table 1 ) with PrimeSTAR® GXL polymerase. The resulting amplicons were purified by gel electrophoresis and extracted using the NucleoSpin® kit (Macherey-Nagel). The elution buffer NE was pre-warmed to 70 °C to increase the yield of purified DNA from the silica membrane spin columns. MF1,MF2 and MF3 were not subcloned into maintenance vectors, instead they were transfected directly into the yeast cells for homologous recombination.
Table 1.
Oligo-nucleotide primers used for assembly of MERS-CoV cDNA by homologous recombination.
| Primer Name | Use | Sequence (5′–3′) |
|---|---|---|
| CMVpF | MF1-F | CGCTGATACCGCCGCTATTAATAGTAATCAATTACGGGGTCAT |
| M-CoV6, 000R | MF1-R | ATTCTTATAAATAGGGTCATAAGTGTCAAACTCAGCCAACA |
| M-CoV6, 001F | MF2-F | GTTGGCTGAGTTTGACACTTATGACCCTATTTATAAGAATGGT |
| M-CoV18, 000R | MF2-R | GGCCAGTTACAATCTGAGACTGGAGCTTGTAATTAGTAAAAGA |
| M-CoV18, 001F | MF3-F | TCTTTTACTAATTACAAGCTCCAGTCTCAGATTGTAACTGGCC |
| BGTR | MF3-R | TTAACTGCGGCGAGGCAGCATATGGCATATGTTGCCAAACTCTAAACCAAATAC |
| pYES1L F | Vector | CATATGCCATATGCTGCCTCGCCGCAGTTAATTAAAGTCA |
| pYES1L R | Vector | TGATTACTATTAATAGCGGCGGTATCAGCG |
Primers containing ∼ 30 bps of homology between MERS-CoV cDNA fragments (MF1, MF2 and MF3) and the pYES1L-BAC vector were used to amplify the regions in preparation for assembly by homologous recombination.
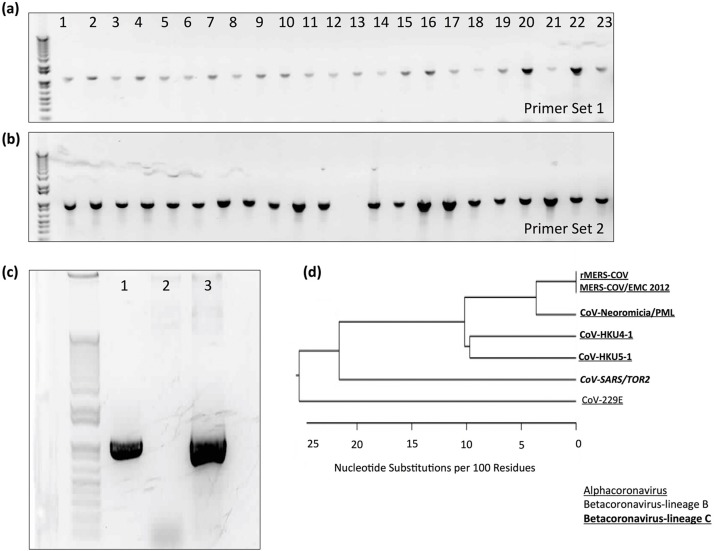
2.3. Homologous recombination of MERS-CoV cDNA
Homologous recombination of the three MERS-CoV gene fragments (MF1, MF2 and MF3) and the pYES1L-BAC vector was performed using the GeneArt® High-Order Genetic Assembly System (Life Technologies). Chemically induced MaV203 cells (Life Technologies) were transformed with 100 ng of pYES1 L Vector, 173 ng of MF1, 205 ng of MF2 and 100 ng of MF3. Transformed cells were grown on complete supplement mixture deficient in tryptophan (CSM-Trp) agar plates for three days at 30 °C. The resulting colonies were replica plated and screened for presence of the MERS-CoV genome by PCR with the GoTaq® polymerase (Promega). S. cerevisiae cells were disrupted by suspension in 30 μL of 0.2% w/v sodium dodecyl sulfate (SDS) (Sigma-Aldrich) and heat treatment at 95 °C for 5 min. The samples were diluted with 20 μL of nuclease-free water and chilled on wet ice. Half of a microliter of lysed S. cerevisiae colony supernatant was used as a template in PCR reactions. Positively screened colonies were grown in 5 mL volumes of CSM-Trp liquid media and the pYES1L-BAC/MERS-CoV plasmids were isolated using the Easy Yeast plasmid Isolation Kit (Takara, Clontech). A 5 μL volume of isolated plasmid was electroporated into Max Efficiency DH10B cells (Life Technologies). DH10B colonies were screened by PCR with GoTaq® polymerase and positive pYES1L-BAC/MERS-CoV plasmids were isolated using the HiSpeed Plasmid Maxi Kit (Qiagen). To view the primers used for the screening reactions refer to the caption of Fig. 2 (Fig. 2a and b).
Fig 2.
(a,b) Transformed S. cerevisiae colonies were screened for the MERS-CoV/pYES1L plasmid vector by PCR (Primer Set 1: F- GTGCTGATGACGAAGGCTTCATCACATTAAAG-AACAATCTATA and R- AGTTGCAAACCTTATACGGTATGGTTGCAACTTTCTTAAAGGAC, Primer Set 2: F- AAGCTTGCACCATGTTGAAACTTTTGGTGGAAGTGCGCTTGT and R- TTAACTGCGGCGAGGCAGCATATGGCATATGTTGCCAAACTCTAAACCAAATAC). Each well (1–23) represents a single colony; positive colonies were defined as those producing an amplicon for both Primer set 1 and Primer set 2. (c) Cellular supernatant was withdrawn from cells infected with either rescued rMERS-CoV virus or rescued rSARS-CoV virus and used in a RT-PCR assay to detect a region of the MERS-CoV polymerase gene (Primer set: F-CAAGATGAACTTTTTGCCATGACAAAGCGTAACGTCATTCC and R- TGTGAGAGGGTAAGCATCTATAGCCAAAGACACAAACCGCT). The MERS-CoV polymerase gene was detected in Lane 1 (rMERS-CoV supernatant) and not Lane 2 (rSARS-CoV supernatant). Lane 3 serves as a positive control, it shows PCR amplification of the MERS-CoV polymerase gene from the infectious clone system. (d) The polymerase gene fragment amplified from rMERS-CoV infected cell supernatant was sequenced and used in a phylogenetic comparison (ClustalW Algorithim) with six coronaviruses: CoV-HKU4-1 (NC_009019.1), CoV-HKU5-1 (NC_009020.1), SARS-CoV/Tor 2 (NC_004718.3), CoV-Neoromicia/PML (KC_869678.4), CoV-229E (NC_002645.1) and MERS-CoV/EMC/2012 (NC_019843.3).
2.4. Sequencing of the MERS-CoV genome
The assembled MERS-CoV genome was sequenced by Sanger sequencing at the DNA Core Facility, Canadian Science Centre for Human and Animal Health, Winnipeg, Manitoba. The sequences were aligned and interpreted using the SeqMan Pro software of the DNASTAR Lasergene 11 Core Suite.
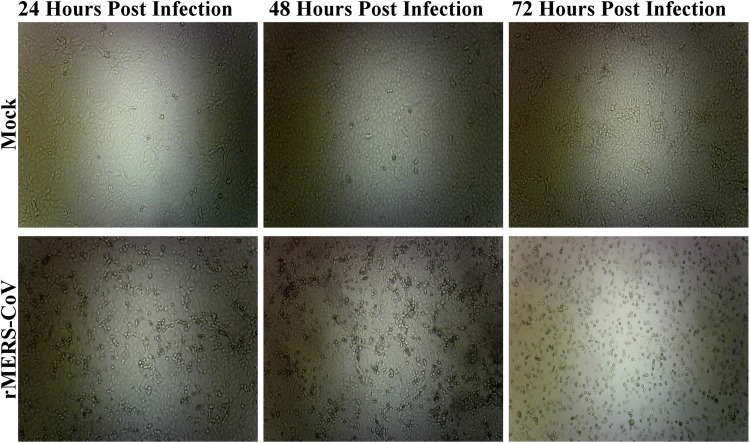
2.5. Rescue of infectious MERS-CoV virus from the infectious clone system
Functionality of the MERS-CoV infectious clone system was examined by rescue in mammalian cell culture. Baby Hamster Kidney cells (BHK-21) (ATCC: CCL-10™) were grown in a T75 flask (NUNC) in Eagle’s Minimal Essential Medium (EMEM) supplemented with 5% v/v fetal bovine serum and 1% v/v penicillin/streptomycin (HyClone) to full confluence at 37 °C 5% CO2. Transfection complexes of pYES1L-BAC/MERS-CoV plasmid (300 ng) were prepared in Opti-MEM™(Life Technologies) using Fugene6® (Promega) transfection reagent and added to a 6-well plate of 70% confluent BHK-21 following 15 min of incubation at room temperature. The transfected BHK-21 cells were incubated overnight at 37 °C, 5% CO2. They were then treated with 0.25% v/v trypsin-EDTA (Gibco™) and a suspension of BHK-21 cells was overlaid onto a monolayer of Vero Cells (ATCC: CCL-81) grown to ∼80% confluence in a T75 flask with Dulbecco’s modified eagle medium (DMEM) supplemented with 5% v/v fetal bovine serum and 1% v/v penicillin/streptomycin. The Vero cells were incubated at 37 °C, 5% C02 for 3 days and then examined for cytopathic effect. The same protocol was used to rescue SARS-CoV virus from an infectious clone system as a control.
2.6. Confirmation of MERS-CoV virus rescue
Three techniques were used to confirm the rescue of infectious MERS-CoV (rMERS-CoV) virus from the infectious clone system. Production of infectious virions from the Vero/BHK-21 cell overlay was confirmed by triplicate blind passage of the cellular supernatant into fresh cultures of Vero Cells grown in a T150 in DMEM with 2% v/v fetal bovine serum and 1% v/v penicillin/streptomycin. Supernatant from the third blind passage was collected at 72 h post infection and rMERS-CoV RNA was extracted using the Viral RNA isolation kit (Qiagen). The viral RNA was treated with DNase I (New England Biolabs) to eliminate any plasmid contamination before being used as a template for reverse transcriptase PCR carried out with Superscript II™(Thermo Fisher) (First Strand Primer: TGTGAGAGGGTAAGCATCTATAGCCAAAGACACAAACCGCT and Forward Primer: CAAGATGAACTTTTTGCCATGACAAAGCGTAACGTCATTCC). The amplified cDNA was then treated with RNase H (New England Biolabs) before being removed from a containment level three laboratory (CL-3). The RT-PCR amplicon was sequenced by the Sanger method and used for phylogenetic comparison with other coronavirus sequences taken from NCBI Genbank. Stocks of the rMERS-CoV virus were frozen at −80 °C degrees. These stocks were later used to compare growth kinetics of the rescued virus with the wild type MERS-CoV EMC/2012 virus.
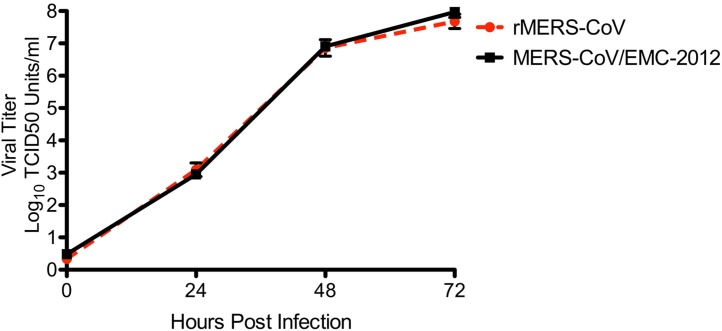
2.7. MERS-CoV growth kinetics
Growth kinetics of the virus rescued from the infectious clone system rMERS-CoV and the clinical isolate MERS-CoV/EMC-2012 were compared by infection of Vero cells in a 12 well tissue culture plate at an MOI of 0.001. Vero Cell supernatants were collected at 24, 48 or 72 h post infection and virus titre was quantified by TCID50 Assay.
2.8. Phylogenetic analysis
The RT-PCR amplicon of rMERS-CoV was sequenced as described in Section 2.4. The sequence was then aligned with the genomes of six other coronaviruses, downloaded from Genbank, using the MegAlign Pro software available from the DNASTAR Lasergene 11 Core Suite. The ClustalW algorithm was chosen to compute the alignment of the RT-PCR amplicon from rMERS-CoV with the corresponding sequence of: MERS-CoV/EMC-2012, BtCoV-HKU4-1, BtCoV-HKU5-1, SARS-CoV/TOR2 and CoV-229E.
2.9. Statistical methods
The error bars in Fig. 4 were generated in GraphPad Prism by calculating the standard error of the mean across the biological replicates. The resulting values were then added and subtracted from the mean value of each time point.
Fig 4.
The replication kinetics of rMERS-CoV was compared with those of the clinical isolate MERS-CoV/EMC-2012 over a time course of 72 h. Vero cells were initially infected at an MOI of 0.001 and virus titre was measured every 24 h for 72 h. The viruses shared replication kinetics concluding that rMERS-CoV serves as a biological surrogate for the clinical isolate. Error bars represent the standard error of the mean +/− from the mean of three biological replicates.
3. Results
3.1. Successful assembly of the MERS-CoV genome by homologous recombination in S. cerevisiae
Transformation of three MERS-CoV DNA fragments (MF1, MF2, MF3) (Fig. 1b) and the pYES1L vector into S. cerevisiae MaV203 cells yielded an assembled MERS-CoV infectious clone system. The procedure seemed quite robust as the 578 ng of input DNA produced over 200 yeast colonies (TNTC) on the selective media, the technique was performed four times and each attempt produced an intact full-length genome. This approach has also successfully constructed a variety of smaller expression plasmid constructs (Ma et al., 1987). Screening S. cerevisiae colonies by PCR with two primer sets detected the MERS-CoV genome in 22/23 samples indicating that the transformation, homologous recombination and screening processes share a combined efficiency of approximately 95% (Fig. 2a and b). The MERS-CoV/pYES1L vector was sequenced by the Sanger method and the viral cDNA genome was 100% identical with that of the isolate MERS-CoV/EMC-2012.
3.2. Confirmation of MERS-CoV virus rescue from the infectious clone system
The utility of the MERS-CoV/pYES1L infectious clone system was examined via several techniques in BHK21 and Vero cells. Cytopathic effect suggestive of viral infection was observed when BHK21 cells transfected with the MERS-CoV/pYES1L plasmid were overlaid onto a monolayer of Vero cells. The presence of infectious viral particles in the cellular supernatant was confirmed by three blind passages in Vero cells (Fig. 3). Viral RNA extracted from the medium of infected Vero cells was tested for MERS-CoV RNA by RT-PCR (Fig. 2c); the identity of the rescued virus was confirmed as MERS-CoV/EMC-2012 by sequencing and phylogenetic analysis of the RT-PCR amplicon (Fig. 2d). Finally, comparison of rMERS-CoV fitness to that of the clinical isolate MERS-CoV/EMC-2012 over a time course of 72 h, showed similar results. The two viruses shared replication kinetics, implying that the rescued virus serves as an accurate phenotypic surrogate for the clinical isolate (Fig. 4).
Fig 3.
Supernatant from the BHK-21 and Vero cell overlay transfected with MERS-CoV/pYES1L plasmid was blind passaged three times to infect a fresh culture of Vero cells. These Vero cells were incubated for 3 days and observed for CPE. CPE was noted in the cells infected with the blind passage supernatant and not the negative control, indicating rescue of infectious virus (rMERS-CoV).
4. Discussion
Construction of infectious clone systems by homologous recombination in S.cerevisiae has potential to become the standard method for construction of coronavirus genomes or those of other similarly large and complex viruses. Use of our method avoided some of the obstacles to coronavirus genome assembly reported by other authors. For instance, regions of the coronavirus genome that show cytotoxicity in E. coli had no observed affect on the growth of S. cerevisiae. The issue of restriction site scarcity was also avoided, because unique sites were not needed to complete construction of the system. The strategy of homologous recombination seems particularly attractive when combined with the availability of viral genome sequences on Genbank and the commercial synthesis of cDNA fragments. These three resources, allow for the rapid construction of a viral infectious clone system without possession of a viral isolate or great risk of introducing mutations into a viral genome during repeated RT-PCR and PCR amplification. Combining homologous recombination in S. cerevisiae with other modern molecular methods (i.e: Gibson Assembly®) may further shorten the construction time of viral infectious clone systems (Gibson et al., 2010). Interestingly two other methods of coronavirus genome assembly (Targeted RNA recombination, and use of a Vaccinia virus backbone) both involve a variation of the homologous recombination mechanism (Almazán et al., 2014). Homologous recombination in S. cerevisiae builds upon these technologies because it allows for single-step construction of the viral cDNA genome in a BAC vector. The BAC based design does not have the stability issues of a targeted RNA based system or require multiple steps for RNA expression like the vaccinia virus one (Enjuanes, 2005).
Two other infectious clone systems for MERS-CoV have been constructed and used to make a replication-competent propagation-deficient vaccine candidate and assess the affect of reporter gene insertion and accessory gene deletion on viral fitness (Almazán et al., 2013, Scobey et al., 2013). Many additional uses of such systems remain including further reverse genetics studies on coronavirus non-structural genes, adaption of the viral genome to infect a suitable animal model and the creation of coronavirus vaccines (Cook et al., 2012, Stobart and Moore, 2014). Future studies will utilize our system to better understand coronavirus replicative function and potentially prepare vaccines or treatments against MERS-CoV.
5. Conclusion
The use of homologous recombination in S.cerevisiae allowed for rapid- single-step- construction of a MERS-CoV infectious clone system, making it a promising candidate methodology for future assembly of large and complex viral genomes or those of recently emerged zoonotic viruses.
Funding
Funding from the Public Health Agency of Canada to Dr. Darwyn Kobasa and Dr. Steven Theriault was used to complete this work. This research did not receive any specific grant from funding agencies in the public, commercial or not for profit sectors.
Contributions
A.N, A.L and B.C completed the laboratory work. D.K designed the infectious clone system, funded the project, provided expertise and edited the manuscript. D.C and S.T provided guidance, funding and edited the manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgements
We would like to thank the Canadian Science Centre of Human and Animal Health’s staff for media preparation and Sanger sequencing. We would also like to recognize Mr. Todd Cutts for his guidance in training and management of the laboratory space.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jviromet.2016.07.022.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Almazán F., Dediego M.L., Sola I., Zuñiga S., Nieto-torres J.L., Marquez-jurado S., Andrés G. Engineering a replication-competent, propogation-defective middle east respiratory syndrome corronavirus as a vaccine candidate. mBio. 2013;4(5) doi: 10.1128/mBio.00650-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almazán F., Sola I., Zuñiga S., Marquez-Jurado S., Morales L., Becares M., Enjuanes L. Coronavirus reverse genetic systems: infectious clones and replicons. Virus Res. 2014;189:262–270. doi: 10.1016/j.virusres.2014.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B.W.M., Cutts T.A., Court D.A., Theriault S. The generation of a reverse genetics system for kyasanur forest disease virus and the ability to antagonize the induction of the antiviral state in vitro. Virus Res. 2012;163:431–438. doi: 10.1016/j.virusres.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Ebihara H., Groseth A., Neumann G., Kawaoka Y., Feldmann H. The role of reverse genetics systems in studying viral hemorrhagic fevers. Thromb. Haemost. 2005;94(2):240–253. doi: 10.1160/TH05-05-0335. http://www.ncbi.nlm.nih.gov/pubmed/16113812 Retrieved from. [DOI] [PubMed] [Google Scholar]
- ECDC . 2015. Epidemiological Update: Middle East Respiratory Syndrome Coronavirus MERS-CoV.http://ecdc.europa.eu/en/press/news/_layouts/forms/News_DispForm.aspx?ID=1278&List=8db7286c-fe2d-476c-9133-18ff4cb1b568&Source=http://ecdc.europa.eu/en/Pages/home.aspx Retrieved from. [Google Scholar]
- Eckert K.A., Kunkel T.A. DNA polymerase fidelity and the polymerase chain reaction. PCR Methods Appl. 1991;1:17–24. doi: 10.1101/gr.1.1.17. [DOI] [PubMed] [Google Scholar]
- Enjuanes L. Coronavirus replication and reverse genetics. In: Lange D.R., editor. Ebooks Corporation Limited. Springer; Berlin Heidelberg: 2005. http://www.utxa.eblib.com/EBLWeb/patron?target=patron&extendedid=P_303939_0& Retrieved from. [Google Scholar]
- Gibson D.G., Glass J.I., Lartigue C., Noskov V.N., Chuang R., Algire M.A., Benders G.A. Creation of a bacterial cell controlled by a chemically synthesized genome. Science. 2010;329(5987) doi: 10.1126/science.1190719. http://science.sciencemag.org/content/329/5987/52.abstract Retrieved from. [DOI] [PubMed] [Google Scholar]
- González J.M., Pénzes Z., Almazán F., Calvo E., Enjuanes L. Stabilization of a full-length infectious cDNA clone of transmissible gastroenteritis coronavirus by insertion of an intron. J. Virol. 2002;76(9):4655–4661. doi: 10.1128/JVI.76.9.4655-4661.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbalenya A.E., Enjuanes L., Ziebuhr J., Snijder E.J. Nidovirales: evolving the largest RNA virus genome. Virus Res. 2006;117(1):17–37. doi: 10.1016/j.virusres.2006.01.017. htt://www.ncbi.nlm.nih.gov/ubmed/16503362 Retrieved March 20, 2015, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilgenfeld R., Peiris M. From SARS to MERS: 10 years of research on highly pathogenic human coronaviruses. Antiviral Res. 2013;100(1):286–295. doi: 10.1016/j.antiviral.2013.08.015. htt://www.ncbi.nlm.nih.gov/ubmed/24012996 Elsevier B.V. Retrieved September 15, 2014, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma H., Kunes S., Schatz P.J., Botstein D. Plasmid construction by homologous recombination in yeast. Gene. 1987;58(2–3):201–216. doi: 10.1016/0378-1119(87)90376-3. http://www.ncbi.nlm.nih.gov/pubmed/2828185 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Memish Z.A., Cotten M., Meyer B., Watson S.J., Alsahafi A.J., Al Rabeeah A.A., Corman V.M. Human infection with MERS coronavirus after exposure to infected camels, Saudi Arabia, 2014. Emerg. Infect. Dis. 2013;20(6):1012–1015. doi: 10.3201/eid2006.140402. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4036761&tool=pmcentrez&rendertype=abstract Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ProMED-mail . 2016. PRO/AH/EDR> MERS-CoV.http://www.promedmail.org Retrieved April 19, 2016, from. [Google Scholar]
- Raj V.S., Osterhaus A.D.M.E., Fouchier R.A.M., Haagmans B.L. MERS: emergence of a novel human coronavirus. Curr. Opin. Virol. 2014;5:58–62. doi: 10.1016/j.coviro.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reusken C.B.E.M., Haagmans B.L., Müller M.A., Gutierrez C., Godeke G.-J., Meyer B., Muth D. Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect. Dis. 2013;13(10):859–866. doi: 10.1016/S1473-3099(13)70164-6. http://www.ncbi.nlm.nih.gov/pubmed/23933067 Retrieved August 15, 2014, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scobey T., Yount B.L., Sims A.C., Donaldson E.F., Agnihothram S.S., Menachery V.D., Graham R.L. Reverse genetics with a full-length infectious cDNA of the Middle East respiratory syndrome coronavirus. Proc. Natl. Acad. Sci. U. S. A. 2013;110(40):16157–16162. doi: 10.1073/pnas.1311542110. htt://www.ubmedcentral.nih.gov/articlerender.fcgi?artid=3791741&tool=pmcentrez&rendertype=abstract Retrieved October 11, 2014, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stobart C.C., Moore M.L. RNA virus reverse genetics and vaccine design. Viruses. 2014;6(7):2531–2550. doi: 10.3390/v6072531. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4113782&tool=pmcentrez&rendertype=abstract Retrieved January 7, 2015, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B., Curtis K.M., Baric R.S. Strategy for systematic assembly of large RNA and DNA genomes: transmissible gastroenteritis virus model. J. Virol. 2000;74(22):10600–10611. doi: 10.1128/jvi.74.22.10600-10611.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B., Denison M.R., Weiss S.R., Baric R.S. Systematic assembly of a full-length infectious cDNA of mouse hepatitis virus strain A59. J. Virol. 2002;76(21):11065–11078. doi: 10.1128/JVI.76.21.11065-11078.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D.M.E. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. htt://www.ncbi.nlm.nih.gov/ubmed/23075143 Retrieved November 17, 2014, from. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.