Abstract
Middle East respiratory syndrome coronavirus (MERS-CoV) has been a highly threatening zoonotic pathogen since its outbreak in 2012. Similar to SARS-CoV, MERS-CoV belongs to the coronavirus family and can induce severe respiratory symptoms in humans, with an average case fatality rate of 35% according to the World Health Organization. Spike (S) protein of MERS-CoV is immunogenic and can induce neutralizing antibodies, thus is a potential major target for vaccine development. Here we constructed a chimeric virus based on the vesicular stomatitis virus (VSV) in which the G gene was replaced by MERS-CoV S gene (VSVΔG-MERS). The S protein efficiently incorporated into the viral envelope and mediated cell entry through binding its receptor, human DPP4. Knockdown of clathrin expression by siRNA drastically abrogated the infection of VSVΔG-MERS in Vero cells. Furthermore, in animal studies, the recombinant virus induced neutralizing antibodies and T cell responses in rhesus monkeys after a single intramuscular or intranasal immunization dose. Our findings indicate the potential of the chimeric VSVΔG-MERS as a rapid response vaccine candidate against emerging MERS-CoV disease.
Highlights
-
•
Constructing two chimeric virus based on VSV which express MERS-CoV S gene.
-
•
The chimeric virus changed the entry mode and required DPP4 as its receptor.
-
•
The chimeric virus induced neutralizing antibodies and T cell responses in monkeys.
1. Introduction
Middle East respiratory syndrome (MERS) is a severe emerging zoonotic disease. Since its initial identification in June 2012 in Saudi Arabia, MERS has caused 2090 infections and 730 deaths (case fatality rate: ∼35%) in 27 countries as of November 2017 (WHO, 2017). MERS is caused by the MERS coronavirus (MERS-CoV), and belongs to the family of Coronaviridae, the genus ß-coronavirus. Like SARS-CoV that belongs in the same genus, MERS-CoV is a zoonotic disease that originates from bats, suggesting that bats are the most likely natural reservoir of MERS-CoV(Annan et al., 2013, Memish et al., 2013, Wang et al., 2014, Yang et al., 2014). Studies have confirmed the presence of MERS-CoV in dromedaries in the Arabian Peninsula and North Africa (Hemida et al., 2017, Kayali and Peiris, 2015, Reusken et al., 2013). Dromedaries are thought to be the main reservoir of MERS-CoV. Although transmission of MERS-CoV from camels to humans has not been reported to date, it has been postulated that primary human infection could result from close contact with camels, which shed the virus (Azhar et al., 2014). Of note, a major MERS outbreak in South Korea resulted in 186 cases, including 36 deaths in 2015. The majority of these cases were health care workers who were in close contact with infected patients (Korea Ministry of Health and Welfare, 2015). Thus developing a MERS vaccine that can provide rapid immune response for high-risk populations (such as health care workers) is of significant importance to public health.
The coronavirus Spike protein (S) is immunogenic and is capable of inducing protective immunity against coronavirus infections including MERS-CoV and Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) (Yang et al., 2004, Ying et al., 2014). Indeed, MVA-based and DNA-based MERS-CoV vaccines designed with S protein as the target immunogen have proven effective in animal models (Haagmans et al., 2016, Muthumani et al., 2015, Song et al., 2013, Volz et al., 2015, Wang et al., 2015). However, these vaccine strategies require multiple dosing to elicit desired immune responses, thus may not be ideal for emergency vaccinations when facing the emerging infectious disease pandemics.
Studies have demonstrated that single-dose recombinant vesicular stomatitis virus (VSV)-based Ebola, Marburg and Lassa fever vaccines can induce rapid immune protection in animal models (Geisbert et al., 2009, Marzi et al., 2015a, Marzi et al., 2015b); for example, a large scale clinical trial of VSV-vectored Ebola vaccine (rVSV-ZEBOV) conducted in west Africa in 2015 demonstrated that a single dose rVSV-ZEBOV immunization was highly safe and effective for humans (Henao-Restrepo et al., 2015). Here, we report a VSV-based chimeric recombinant virus, VSVΔG-MERS, in which VSV glycoprotein (G) gene was replaced by the MERS-CoV S gene. Single-dose immunization, either by the intramuscular or intranasal route, induced high-level and lasting MERS-CoV-specific neutralizing antibodies and T-cell responses in rhesus monkeys. Our results demonstrate, therefore, the potential of VSVΔG-MERS as a candidate vaccine against MERS-CoV.
2. Materials and methods
2.1. Recombinant virus construction and rescue
A previously described VSVΔG-eGFP pseudovirus system (Wang et al., 2006) was adapted and modified to construct VSVΔG-MERS and VSVΔG-eGFP-MERS. Chemically synthesized MERS-CoV S gene (GenBank accession No. KF186567.1) was amplified by PCR and flanked by NheI restriction site., VSV gene-start and gene-end sequences were introduced. The PCR product was sequenced and cloned into the NheI site after the eGFP gene of pVSVΔG-eGFP (plasmid containing VSV genomic cDNA without G gene). The resultant plasmid was named pVSVΔG-eGFP-MERS. There were two MluI sites flanking the eGFP gene so construction of the pVSVΔG-MERS plasmid was achieved by MluI digestion and self-ligation. pVSVΔG-eGFP-MERS or pVSVΔG-MERS was co-transfected with a eukaryotic plasmid expressing VSV N, P and L protein, respectively, in BSR-T7/5 cells to rescue the recombinant virus. At 96 h post-transfection, the supernatant was harvested and clarified by low speed centrifugation, and serially passaged on Vero E6 cells for at least 3 passages until obvious green fluorescence or cytopathic effect (CPE) was observed. The rescued viruses were named VSVΔG-eGFP-MERS and VSVΔG-MERS respectively. The growth kinetics of the recombinant viruses was determined. VSVΔG-eGFP-MERS and VSVΔG-MERS were, respectively, inoculated at an MOI = 0.01 onto Vero E6 cells growing in a 6-well plate and the supernatant was removed at 12-h intervals from 12 h to 96 h. The samples of each time-point were titrated on Vero E6 cells using indirect immunofluorescence by staining with mouse anti-S serum and TRITC-labeled goat anti-mouse IgG as primary and secondary antibodies. The titer was expressed as the reciprocal of the highest dilution titer (fluorescence forming unit, FFU).
2.2. Indirect immunofluorescence and Western blot assay
For Indirect immunofluorescence assay, Vero E6 cells were infected with either VSVΔG-eGFP-MERS or VSVΔG-MERS at an MOI = 1. At 24 h post-infection, cells were fixed with 3% paraformaldehyde, and cells were stained with mouse anti-S serum (pCAGGS-MERS-S immunized mouse serum) as primary antibody and TRITC-conjugated goat anti-mouse IgG as secondary antibody. Cell nuclei were stained with Hoechst 33342 (Invitrogen, Oregon, USA). Stained cells were analyzed with a Leica TCS SP5 laser scanning confocal microscope (Leica, Mannheim, Germany).
For Western blot assay, Vero E6 cells were infected with either VSVΔG-eGFP-MERS or VSVΔG-MERS at an MOI = 0.1. At 72 h post-infection, the cells were collected and lysed, the cell lysates were mixed with protein loading buffer, subjected to SDS-PAGE and subsequently electro-transferred to nitrocellulose membranes. Target band(s) were detected with mouse anti S serum and Alexa Fluor 680-conjugated donkey anti mouse IgG (Invitrogen, Oregon, USA). The bands were visualized with an Odyssey digital fluorescence imaging system (LI-COR, Nebraska, USA).
2.3. Immunoelectron microscopy
VSVΔG-eGFP-MERS and VSVΔG-MERS were cultured and harvested from infected Vero E6 cells. Next, 1 ml supernatant was clarified by low speed centrifugation to remove cell debris, and subjected to high speed centrifugation (12,000 rpm, 10 min), after which 0.9 ml supernatant was carefully taken out and discarded. The remaining sample was gently vortexed and prepared for electron microscopy following a previously described protocol (Ge et al., 2011). Briefly, purified virus was bound to 200-mesh Formvar carbon-coated nickel grids (Electron Microscopy Sciences, Hatfield, PA). For immunolabeling, grids were blocked in PBS containing 2% globulin-free BSA (Sigma-Aldrich, St. Louis, MO) and incubated with mouse anti-S antibody. Grids were then washed in blocking buffer and incubated with 10-nm gold particle-conjugated goat anti-mouse IgG (Sigma-Aldrich, St. Louis, MO). After the final wash, the grids were negatively stained with 1% phosphotungstic acid, and subsequently examined under a model H7500 transmission electron microscope (Hitachi High Technologies, Schaumburg, IL) at 80 kV. Images were obtained by using an XR100 digital camera system (Advanced Microscopy Techniques, Danvers, MA).
2.4. Gene expression knockdown by RNA interference
To knock down the expression of the human DPP4 and clathrin gene in HEK-293 cells, we used Ambion Validated Silencer Selected siRNA (Thermo Fisher, Waltham, MA) respectively targeted to the specific sequence of DPP4 or clathrin. Briefly, siRNA (200 nM, 5 μl per well) targeting to DPP4, clathrin, VSV L gene (positive control) or irrelevant siRNA (negative control, Ambion cat no. 4390843) was pre-arrayed on 96-well cell carrier plates (Perkin Elmer, Waltham, MA), respectively. Next, 35 μl OptiMEM medium (Invitrogen, Oregon, USA) containing 0.15 μl Lipofectamine RNAiMAX transfection reagent (Invitrogen, Oregon, USA) was mixed with 60 μl OptiMEM medium containing 1 × 104 Vero E6 cells. The cell-RNAiMAX mix was then added to the wells. Cells were incubated for 48 h to knockdown gene expression, after which the cells were infected with VSVΔG-eGFP-MERS or VSV-eGFP at an MOI = 0.01. At 48 h post-infection (15 h for VSV-eGFP), cells were fixed with 3% paraformaldehyde and stained with Hoechst 33342 (Invitrogen, Oregon, USA) in PBS for 1 h. Stained cells were imaged by PerkinElmer Operetta high-content system (PerkinElmer, Waltham, MA). Uninfected cells served as the reference population for background fluorescence. Fifty-two fields per well were imaged at 20 × magnification. Columbus software (PerkinElmer, Waltham, MA) was used to automatically identify and quantify green fluorescence and cell nuclei. The infection ratio was determined according to the numbers of infected versus non-infected cells. The assay was independently repeated three times.
2.5. ELISA
Enzyme-linked immunosorbent assay (ELISA) for determining S protein-specific IgG in mouse or monkey serum was performed as described previously (Kong et al., 2012). Briefly, BSR-T7/5 cells were seeded onto two wells of a 6-well plate. Cells were infected with recombinant Newcastle disease virus expressing MERS-CoV S protein (Liu et al., 2017) at an MOI = 0.1. At 24 h post-infection, the cell pellet was collected and lysed with vigorous pipetting, and the supernatant was used as coating antigen. Antibodies were detected using HRP-labeled goat anti-mouse (or monkey) IgG (Southern Biotech, Birmingham, AL). A standard curve was generated by coating the ELISA plate with serially diluted purified mouse or monkey IgG (Southern Biotech, Birmingham, AL) at known concentrations. A linear equation was obtained based on the standard IgG concentrations and their O.D values, thus the concentration of MERS-specific IgG was calculated according to the linear equation based on their O.D values and expressed as the amount of IgG per ml of serum (ng/ml).
2.6. Neutralization assay
Mouse and monkey serum neutralizing antibody levels were determined using VSVΔG-eGFP-MERS. To perform the neutralization assay, 25 μl of 2-fold serially-diluted serum (heat inactivated at 56 °C for 30 min before use) was mixed with 25 μl DMEM containing 5 × 102 TCID50 VSVΔG-eGFP-MERS and incubated at 37 °C for 1 h. After incubation, 50 μl of the pre-incubated mixture was added onto Vero E6 cells in triplicate wells of a 96-well plate. The GFP-expressing cells were counted at 36 h post-infection under a fluorescence microscope. Virus neutralization titers (VNT) were expressed as the reciprocal of the highest dilution of serum that showed at least 50% reduction in the number of fluorescent cells as compared with the negative control.
2.7. Animals and immunization protocol
For monkey immunizations, eight 2-year old male rhesus monkeys (obtained from Academy of Military Medical Sciences, Beijing, China) were randomly divided into two groups. Group 1 was intramuscularly (i.m) immunized with 2 × 107 FFU VSVΔG-MERS (preparation described below) in 2 ml medium via hind limb muscle injection under anesthesia. Group 2 was intranasally (i.n) immunized with the same regimen as Group 1 via nostril instillation under anesthesia. All monkeys were housed in separate cages in a Biosafety Level-3 laboratory equipped with stable moisture and temperature. Monkeys were fed 3 times a day with specialized monkey puffed diet and various fresh fruits and adequate drinking water.
Ten 6-week female Balb/c mice (Vital River, Beijing, China) were intramuscularly immunized with 1 × 106 FFU VSVΔG-MERS in 0.1 ml medium via hind limb muscle injection. Ten control mice were intramuscularly injected with 0.1 ml medium. Mice were monitored daily for weight changes and signs of illness for 14 days. Mice were given the booster dose 3 weeks after the first dose. Mice blood was collected 2 weeks after the prime and boost immunizations, and mice sera were prepared for determining the MERS-specific IgG and neutralizing antibodies.
All animal usage was in strict accordance with the Guide for the Care and Use of Laboratory Animals of the Ministry of Science and Technology of the People's Republic of China. The protocols were approved by the Animal Research Ethics Committee of Harbin Veterinary Research Institute, Chinese Academy of Agricultural Sciences.
2.8. ELISPOT
Enzyme-linked immunospot (ELISPOT) assay was performed to evaluate the vaccine-induced T cell responses in monkeys. Ten days after immunization, monkey blood was drawn from lower extremity veins under anesthesia. Peripheral blood mononuclear cells (PBMC) were separated by monkey lymphocyte separation buffer (TBD sciences, Tianjin, China). To ensure adequate cell numbers, monkey PBMCs from the same group were pooled. A synthetic overlapping peptide pool spanning the whole MERS-CoV S protein, which consisted of 269 peptides (15mers with 10 amino acid overlapped, designed for CD8+ T cells) was used to evaluate the specific CD8+ T cell responses. Briefly, Millipore 96-well HTS HA sterile plates (Millipore, USA) were coated with 4 μg/ml purified mouse anti-human IFN-γ (BD Pharmingen, San Diego, CA) in 0.1 ml PBS at 4 °C. After 12 h, the coating solution was removed, then 0.05 ml RPMI 1640 medium containing 20 μg/ml diluted peptide was added into the well after which 5 × 105 PBMCs in 0.05 ml RPMI 1640 medium were added into the well and mixed with peptide. Cells were cultured with the peptides at 37 °C for 24 h to induce stimulation. The cells were removed from the plate by vigorous washing using PBST, then 0.1 ml biotin-labeled mouse anti human IFN-γ (BD Pharmingen, San Diego, CA) was added for 1 h, followed by adding 0.1 ml HRP-conjugated streptavidin (BD Pharmingen, San Diego, CA) for 1 h. After final wash, spots were developed by AEC substrate (BD Pharmingen, San Diego, CA). The images of spots were acquired and counted by a ChampSpot III ELISPOT reader (Sage Creation Science, Beijing, China), and the data was analyzed by Excel software (Microsoft, Redmond, WA). The cut-off threshold was set as 100 spots compared to the negative control. Six peptides that stimulated the most numbers of spots were selected. The information of these peptides is listed in Table 1 .
Table 1.
T cell reactive S protein peptides in monkeys vaccinated with VSVΔG-MERS.
| S peptidea |
T cell response to peptide |
|||
|---|---|---|---|---|
| Peptide # | Peptide sequence | Amino acid position | SFC/million PBMCb |
|
| i.m | i.n | |||
| S55 | VDLYGGNMFQFATLP | 271–285 | 1696 | 1720 |
| S124 | VFQNCTAVGVRQQRF | 616–630 | 1922 | 1860 |
| S154 | HPIQVDQLNSSYFKL | 766–780 | 1726 | 1620 |
| S174 | GGDFNLTLLEPVSIS | 866–880 | 1616 | 1660 |
| S221 | DKVNECVKAQSKRSG | 1101–1115 | 2306 | 2246 |
| S257 | IDLKELGNYTYYNKW | 1280–1295 | 1880 | 1842 |
Sequences were based on the S gene of MERS-CoV isolate Al-Hasa_4_2013.
The numbers of IFN-γ-positive T lymphocytes in PMBC samples expressed as spot-forming cells (SFC)/million PBMCs were determined by S overlapping peptides and IFN-ELISPOT assay.
2.9. .Statistical analysis
Two-way ANOVA with Bonferroni's multiple comparison tests was used for statistical analysis. All P-values were two-tailed and considered statistically very significant when the associated probability was less than 0.01.
3. Results
3.1. Construction of VSVΔG-MERS and VSVΔG-eGFP-MERS and in vitro characterization of the viruses
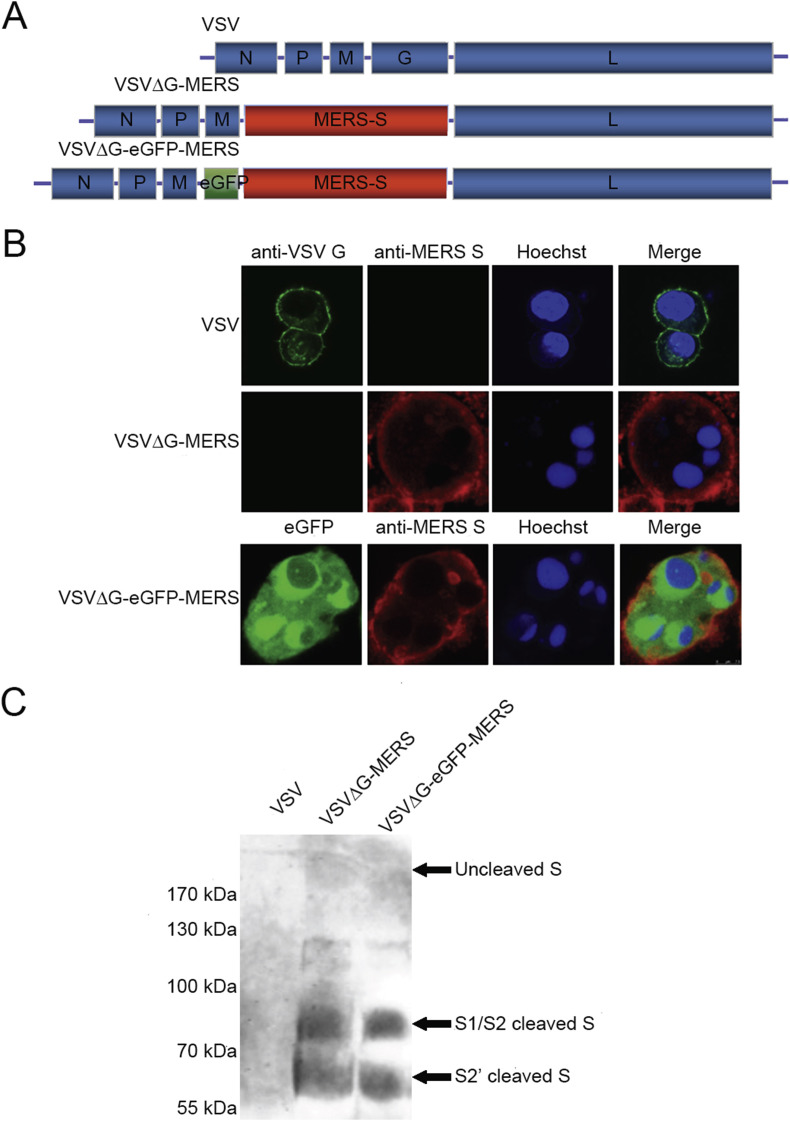
VSVΔG-MERS and VSVΔG-eGFP-MERS were constructed and rescued based on the established VSV Indiana strain reverse genetics system (Wang et al., 2006) in which the VSV G gene was replaced by MERS-CoV S gene (an eGFP gene was inserted between the M and S gene of VSVΔG-MERS to construct VSVΔG-eGFP-MERS) as shown in Fig. 1 A. The expression of S protein was confirmed by indirect immunofluorescence and Western blotting (Fig. 1B and C). Indirect immunofluorescence using anti-S protein antibody confirmed the surface expression of S protein in VSVΔG-MERS and VSVΔG-eGFP-MERS-infected Vero cells (Fig. 1B). eGFP expression was confirmed in VSVΔG-eGFP-MERS infected Vero cells. Both VSVΔG-MERS and VSVΔG-eGFP-MERS infected cells were not stained by VSV G monoclonal antibody. As shown in Fig. 1C, uncleaved S protein (faint bands above 170 kDa), S1/S2 cleaved S protein (∼80 kDa) and S2' cleaved S protein (∼65 kDa) (Millet and Whittaker, 2014) was detected in the purified VSVΔG-MERS and VSVΔG-eGFP-MERS virions indicating incorporation of S protein into the viral particles.
Fig. 1.
Generation of VSVΔG-MERS and VSVΔG-eGFP-MERS and expression of S protein. Schematic representation of the recombinant viruses (A). S protein expression in VSVΔG-MERS and VSVΔG-eGFP-MERS infected Vero E6 cells by indirect immunofluorescence staining (B) and Western blot (C).
VSVΔG-MERS and VSVΔG-eGFP-MERS showed similar growth kinetics in Vero cells and their peak titers reached 1 × 107 FFU/ml at 72 h post-infection (Fig. 2 ). The recombinant viruses showed delayed growth kinetics and decreased titers compared with native VSV that reached 1 × 109 FFU/ml at 24 h post-infection. The genetic stability of VSVΔG-MERS and VSVΔG-eGFP-MERS was assessed by serially passaging the virus on Vero E6 cells for 10 passages, and the expression of S gene (plus eGFP gene for VSVΔG-eGFP-MERS) was confirmed by RT-PCR and immunofluorescence analyses (data not shown).
Fig. 2.
Growth properties of recombinant viruses in Vero E6 cells. VSV, VSVΔG-MERS and VSVΔG-eGFP-MERS were inoculated on Vero E6 cells on 6-well plate at a MOI = 0.01, supernatant was taken out from 12 h to 96 h at 12-h intervals. The titer was expressed as the reciprocal of the highest dilution titer (fluorescence forming unit, FFU).
3.2. MERS-CoV S incorporates into the envelope of recombinant VSV and mediates cell infection by using the receptor DPP4
To further confirm the incorporation of S protein into the viral particles, electron and immunoelectron microscopy were performed. Results clearly showed the S protein incorporated into VSVΔG-MERS, VSVΔG-eGFP-MERS, and VSV-MERS (Fig. 3 A, long arrows). VSV G protein was also shown on VSV and VSV-MERS particles with discrepant shape compared with MERS-CoV S protein (Fig. 3 upper panel, short stealth arrows). Immunoelectron microscopy showed the binding of gold-labeled secondary antibody to the anti-S antibody-bound S protein on the VSVΔG-MERS, VSVΔG-eGFP-MERS, and VSV-MERS particles (Fig. 3A, lower panel, long arrow indicating S protein). These results confirmed the incorporation of S protein into the chimeric viral particles.
Fig. 3.
Incorporation of S protein into viral particles. S protein efficiently incorporated into the viral particles as indicated by electron and immunoelectron microscopy (A). VSV-MERS, a recombinant VSV virus has MERS-CoV S gene inserted between VSV M and G gene as an additional transcription unit (unpublished work). VSV-MERS has both G and S protein on viral surface. Long arrows indicate S protein; short stealth arrows indicate VSV G protein.
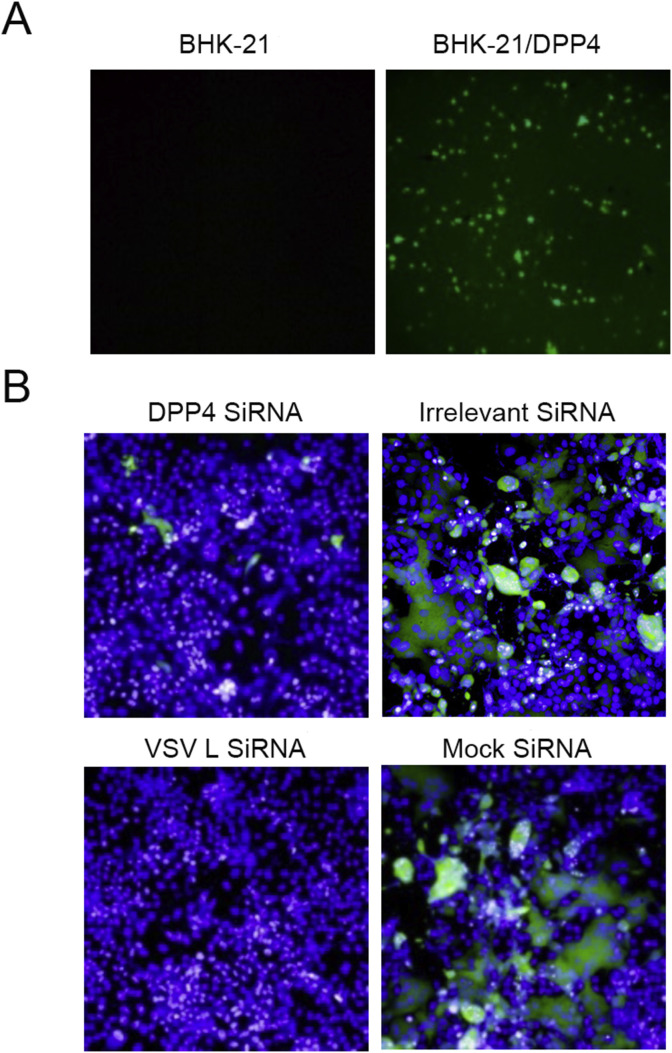
Since VSVΔG-MERS and VSVΔG-eGFP-MERS had the native G protein replaced with MERS-CoV S protein to execute viral attachment and entry, the viruses should use human dipeptidyl peptidase 4 (DPP4) as their entry receptor (Raj et al., 2013). BHK-21 cells do not express human DPP4, and are non-permissive to MERS-CoV infection so we transfected BHK-21 cells with pCAGGS-DPP4 (a eukaryotic plasmid encoding human DPP4) prior to infecting the cells with VSVΔG-eGFP-MERS. As shown in Fig. 4 A, BHK-21 cells were not infected by VSVΔG-eGFP-MERS, while DPP4-transfected BHK-21 cells were infected by the virus. Vero E6 cells are permissive cells for MERS-CoV, and our results demonstrated that VSVΔG-eGFP-MERS and VSVΔG-MERS could infect Vero E6 cells and form large syncytia (Figs. 1B and 4B). We then used human DPP4 siRNA to knock-down DPP4 expression in Vero E6 cells in advance of infection, and results showed infection of VSVΔG-eGFP-MERS was significantly reduced (Fig. 4B). These results confirmed the incorporation of functional S protein into the chimeric viral particles and demonstrated their use of human DPP4 as the cellular receptor for infection.
Fig. 4.
VSVΔG-MERS and VSVΔG-eGFP-MERS utilize human DPP4 as receptor. BHK-21 cells and human DPP4-transfected BHK-21 cells were infected with VSVΔG-eGFP-MERS (A). Vero E6 cells transfected with DPP4 siRNA, irrelevant siRNA, VSV L siRNA and mock siRNA were infected with VSVΔG-eGFP-MERS (B).
3.3. VSVΔG-MERS and VSVΔG-eGFP-MERS enter cells partially in a clathrin-dependent endocytic pathway
It has been well demonstrated that VSV enters cells by a clathrin-dependent endocytic pathway (Cureton et al., 2009). To determine whether replacement of VSV G with the MERS-CoV S altered the endocytic pathway of VSVΔG-MERS, clathrin knockdown and viral infection assays were carried out. Results showed significant reduction of VSV-eGFP and VSVΔG-eGFP-MERS infection after clathrin knockdown (Fig. 5 ). In fact, clathrin knock-down had a more severe influence on the infection rate of VSV-eGFP than for VSVΔG-eGFP-MERS, as indicated by the infection ratio decrease of VSV-eGFP (from ∼70% to ∼15%) versus that of VSVΔG-eGFP-MERS (from ∼55% to ∼20%) (Fig. 5 II). Taken together, our results indicated that VSVΔG-eGFP-MERS utilized more than one way to enter cells as shown by syncytia formation (Fig. 1B) and clathrin-mediated endocytosis (Fig. 5).
Fig. 5.
Clathrin is important for VSVΔG-eGFP-MERS infection. Vero E6 cells were transfected with clathrin siRNA, VSV L siRNA, mock siRNA and irrelevant siRNA to observe the impact of clathrin-knockdown on VSVΔG-eGFP-MERS (I A) or VSV-eGFP (I B) infection. The infection ratio (mean ± SD) and statistical analysis is presented (II A and B); significant differences between conditions is designated with (a) in panel II A and (b) in panel II B; p < .01.
3.4. VSVΔG-MERS induces significant MERS S-specific IgG and neutralizing antibody in mice
We first characterized the safety and immunogenicity of VSVΔG-MERS in Balb/c mice. Mice were intramuscularly inoculated with 1 × 106 FFU VSVΔG-MERS and were monitored daily to detect body weight changes and signs of illness or death. Results showed all mice were healthy and did not exhibit untoward clinical signs. Body weight gain was similar between the experimental and the PBS control group mice for two weeks post-inoculation (Fig. 6 A). We then evaluated VSVΔG-MERS-induced humoral immune responses for S protein-specific IgG and neutralizing antibodies. Results showed high levels of specific IgG were detectable after the initial inoculation (measured day 14, 13 μg/ml), and specific IgG was significantly boosted after the second dose on day 21 (measured day 35, 20 μg/ml) (p < .05) (Fig. 6B). MERS neutralizing antibody was also detected after the first dose, and was significantly boosted after the second dose (p < .05) (Fig. 6C). Due to the fact that mice cannot be infected by VSVΔG-MERS, as they do not express human DPP4, these results demonstrated the potential of VSVΔG-MERS to serve as an inactivated MERS vaccine.
Fig. 6.
Humoral responses of VSVΔG-MERS-immunized mice. 10 mice were intramuscularly immunized with 1 × 106 FFU VSVΔG-MERS, mice were observed and weighed daily for 14 days (A). At 21 days after the first dose, mice were given the booster dose. S protein specific IgG (B) and neutralizing antibody (C) was analyzed. (a), (b) p < .01.
3.5. Single dose intramuscular or intranasal immunization of VSVΔG-MERS induces significant MERS-CoV specific humoral and T cell responses in rhesus monkeys
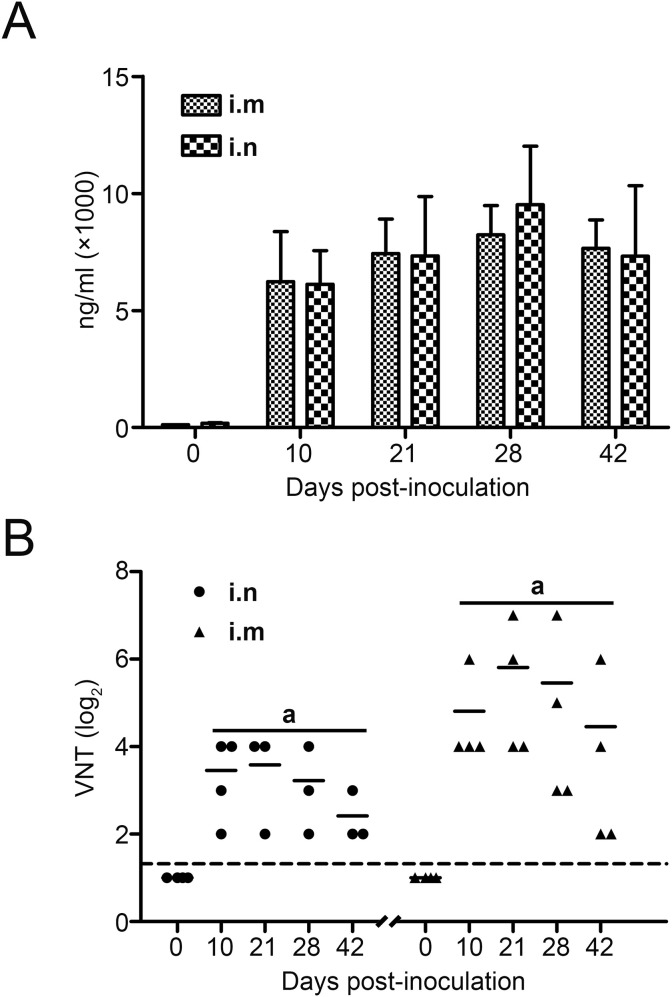
To further investigate the immunogenicity of the VSVΔG-MERS vaccine in non-human primates, rhesus monkeys were intramuscularly or intranasally immunized once with 2 × 107 FFU of VSVΔG-MERS then specific humoral and T cell responses were evaluated. As shown in Fig. 7 , single dose immunization induced significant MERS S protein specific IgG in monkeys vaccinated via both the intramuscular (i.m) and intranasal (i.n) route. IgG was detected 10-days post immunization and remained elevated for at least 42 days with the peak IgG level appearing on day 28. No statistical difference existed between i.m- and i.n-immunized monkeys at any time-point (Fig. 7A). Monkey MERS S protein neutralizing antibodies were induced after i.m or i.n immunization, and were detected on day 10 post immunization, reaching peak level at day 21 (Fig. 7B). The neutralizing antibody titer of i.m group was significantly higher than that of the i.n group at both time-points (Fig. 7B), indicating that the i.m route might better facilitate the production of neutralizing antibodies in the case of VSVΔG-MERS immunization in monkeys.
Fig. 7.
Humoral immune responses of rhesus monkeys to VSVΔG-MERS vaccination. Monkeys were immunized with 2 × 107 FFU of recombinant virus intramuscularly (i.m) or intranasally (i.n). Blood samples were collected at the indicated time-points. Serum IgG (A) and neutralizing antibody (B) were determined. The neutralizing antibody from both routes at the same time-point was compared. (a) p < .01.
We further evaluated the T cell response in immunized monkeys by ELISPOT. An overlapping peptide pool consisted of 269 peptides spanning the MERS S protein was used to stimulate the PBMCs. The 15-mer peptides (with 10 amino acid overlap) were designed to preferentially stimulate CD8+ T cells. The IFN-γ secreting cells were counted and analyzed. As shown in Fig. 8 , both i.m- and i.n-immunized monkeys produced active T cell responses specific to the S protein peptide stimulation. Of the 269 peptides, we selected the most “dominant” peptide that induced the highest level of IFN- γ secretion (900 spots/well on average) and compared responses with the PMA+IONO positive control (1500 spots/well on average). We hypothesized that these peptides potentially contained monkey S protein-specific CD8+ T cell epitopes. No statistical significance was observed between i.m- and i.n-immunized groups for these selected peptides (Fig. 8).
Fig. 8.
T cell responses of immunized rhesus monkeys to VSVΔG-MERS vaccination. PBMCs from immunized monkeys were tested for MERS-CoV S peptide-specific T cell responses by ELISPOT. An S protein overlapping peptide pool which contained 269 peptides (15-mers designed for CD8+ T cells) were used to stimulate the monkey PBMCs. Ex-vivo IFN-γ ELISPOT assay was performed to determine the active cells. Six peptides that yielded the most spots were selected for presentation. No statistical difference was observed in the peptides between the i.m and i.n groups.
4. Discussion
In this study, we successfully constructed a VSV-based recombinant chimeric virus bearing MERS-CoV S protein as its new membrane glycoprotein to replace its own G protein. The chimeric virus, which is replication competent in permissive cells, utilized S protein as its sole membrane anchored glycoprotein and recognized human DPP4 as its receptor to complete attachment and cell entry. We further demonstrated that single-dose immunization, either by the intramuscular or intranasal route, induced a high-level and lasting MERS-CoV-specific neutralizing antibodies and T cell responses in rhesus monkeys.
To date, there are several types of MERS vaccines reported which mainly include live attenuated vaccine, DNA vaccine, subunit vaccine, and recombinant vectored vaccine (measles virus, MVA and adenovirus); thus far the DNA vaccine and recombinant vectored vaccines have been shown to be efficacious in experimental animals (Modjarrad et al., 2016). Of note, an MVA vectored vaccine was highly immunogenic and could significantly reduce the MERS-CoV excretion in dromedary camels (Haagmans et al., 2016). A measles virus vectored vaccine was also highly immunogenic and protective in human DPP4-transgenic mice (Malczyk et al., 2015). These results clearly demonstrate the great potential of a live-vectored vaccine. However, all of these are vaccines that require multiple dosing to generate desired immune responses, thus are not ideal in emergencies that necessitate rapid immune responses to emerging infectious diseases like MERS. By contrast, a single dose of VSVΔG-MERS immunization would suffice to induce ideal immune response.
In a previous study, we successfully generated a VSV pseudovirus bearing SARS-CoV S protein for neutralization assay and cell-entry assay (Ge et al., 2006), we further replaced the VSV G gene with the SARS-CoV S gene and successfully rescued the recombinant chimeric virus VSVΔG-SARS using a VSV reverse genetics system (unpublished work). Thus in the present study we constructed VSVΔG-MERS by deploying the same strategy. The rescued virus manifested delayed growth kinetics and decreased peak titer compared with the native vector virus (Fig. 2). S protein was, therefore, the sole viral membrane anchored glycoprotein instead of VSV G protein, and was critical in receptor binding and viral entry. Furthermore, the incorporation of S protein did not alter the morphology of the virus (bullet shaped virions, Fig. 3), but it did obviously alter the tropism and entry of the virus. The recombinant virus required human DPP4 as its cellular receptor (Fig. 4A and B). The S protein also influenced the entry mode of the recombinant virus, as shown in Fig. 1B, as significant syncytia formation was observed in VSVΔG-MERS and VSVΔG-eGFP-MERS-infected Vero E6 cells, but not in VSV-infected cells. This observation indicated that the virus utilized direct membrane fusion to enter cells, which was in accordance with the previous study that showed that MERS-CoV could enter the cells partially via direct membrane fusion (Qian et al., 2013). Our results further demonstrated clathrin played an important role in VSVΔG-eGFP-MERS entry, as shown in Fig. 5, where knocking down clathrin expression by siRNA in Vero E6 cells largely reduced the infection rate of VSVΔG-eGFP-MERS. This result indicated the recombinant virus could enter cells via clathrin-mediated endocytosis, which is in agreement with studies showing MERS-CoV could enter cells either by direct membrane fusion or by clathrin-mediated endocytosis (de Wit et al., 2016).
Our in vivo results demonstrated efficacious immunogenicity of VSVΔG-MERS in mice and rhesus monkeys. Theoretically, Balb/c mice cannot be infected by VSVΔG-MERS due to the lack of human DPP4, thus the recombinant virus was similar to an inactivated vaccine or virus-like particle vaccine for mice. Our results showed that VSVΔG-MERS induced a robust humoral immune response in mice after a two-dose i.m immunization. Most importantly, our results demonstrated that a single i.m or i.n inoculation dose could induce effective humoral and T cell responses in rhesus monkeys. Quantitative ELISA results showed that recombinant virus induced high level of S protein specific IgG in both groups, and no statistical difference existed between i.m and i.n groups at any time-point. However, results for the neutralizing antibodies were quite different where the i.m group demonstrated significantly higher levels of neutralizing antibodies than the i.n group at all time-points. While i.m inoculation was more effective in generating neutralizing antibodies than the i.n route, the levels of serum neutralizing antibodies following i.n inoculation were significantly higher than baseline and not trivial. We, therefore, suggest that in future application, a single dose vaccine can be given via both the i.n and i.m routes to ensure solid immunity. In the present study, we were unable to carry out a viral neutralizing assay using MERS-CoV due to the unavailability of MERS-CoV per se, thus we used VSVΔG-eGFP-MERS to mimic MERS-CoV to determine the neutralizing titers. This method was similar to that used with the S protein bearing pseudo-viruses, such as lentiviral particles (Grehan et al., 2015, Jaume et al., 2011); while VSVΔG-eGFP-MERS is replication competent, it is more stable and suitable for the neutralizing antibody assay. To date, several MERS-CoV animal models have been reported, including rhesus macaques (de Wit et al., 2013, Munster et al., 2013, Yao et al., 2014), common marmosets (Falzarano et al., 2014), DPP4 transgenic mice (Agrawal et al., 2015, Pascal et al., 2015) and DPP4-expressing adenovirus transduced mice (Zhao et al., 2014). Due to the unavailability of MERS-CoV, a monkey challenge study could not be undertaken in the current study setting but will be undertaken in a future study. Considering the neutralizing antibody levels generated and the correlation between neutralizing antibody and protection, we speculate that the VSVΔG-MERS vaccine will confer protection against MERS-CoV.
Funding information
This study was support by National Key Technology R&D Program (2013BAD12B05).
Acknowledgments
We thank Bernard Moss (University of Tennessee Health Science Center) for providing the VSVΔG-eGFP pseudovirus system.
References
- Agrawal A.S., Garron T., Tao X., Peng B.H., Wakamiya M., Chan T.S., Couch R.B., Tseng C.T. Generation of a transgenic mouse model of Middle East respiratory syndrome coronavirus infection and disease. J. Virol. 2015;89:3659–3670. doi: 10.1128/JVI.03427-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annan A., Baldwin H.J., Corman V.M., Klose S.M., Owusu M., Nkrumah E.E., Badu E.K., Anti P., Agbenyega O., Meyer B., Oppong S., Sarkodie Y.A., Kalko E.K., Lina P.H., Godlevska E.V., Reusken C., Seebens A., Gloza-Rausch F., Vallo P., Tschapka M., Drosten C., Drexler J.F. Human betacoronavirus 2c EMC/2012-related viruses in bats, Ghana and Europe. Emerg. Infect. Dis. 2013;19:456–459. doi: 10.3201/eid1903.121503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azhar E.I., El-Kafrawy S.A., Farraj S.A., Hassan A.M., Al-Saeed M.S., Hashem A.M., Madani T.A. Evidence for camel-to-human transmission of MERS coronavirus. N. Engl. J. Med. 2014;370:2499–2505. doi: 10.1056/NEJMoa1401505. [DOI] [PubMed] [Google Scholar]
- Cureton D.K., Massol R.H., Saffarian S., Kirchhausen T.L., Whelan S.P. Vesicular stomatitis virus enters cells through vesicles incompletely coated with clathrin that depend upon actin for internalization. PLoS Pathog. 2009;5 doi: 10.1371/journal.ppat.1000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit E., Rasmussen A.L., Falzarano D., Bushmaker T., Feldmann F., Brining D.L., Fischer E.R., Martellaro C., Okumura A., Chang J., Scott D., Benecke A.G., Katze M.G., Feldmann H., Munster V.J. Middle East respiratory syndrome coronavirus (MERS-CoV) causes transient lower respiratory tract infection in rhesus macaques. Proc. Natl. Acad. Sci. U. S. A. 2013;110:16598–16603. doi: 10.1073/pnas.1310744110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falzarano D., de Wit E., Feldmann F., Rasmussen A.L., Okumura A., Peng X., Thomas M.J., van Doremalen N., Haddock E., Nagy L., LaCasse R., Liu T., Zhu J., McLellan J.S., Scott D.P., Katze M.G., Feldmann H., Munster V.J. Infection with MERS-CoV causes lethal pneumonia in the common marmoset. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1004250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge J., Wang X., Tao L., Wen Z., Feng N., Yang S., Xia X., Yang C., Chen H., Bu Z. Newcastle disease virus-vectored rabies vaccine is safe, highly immunogenic, and provides long-lasting protection in dogs and cats. J. Virol. 2011;85:8241–8252. doi: 10.1128/JVI.00519-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge J., Wen Z., Wang X., Hu S., Liu Y., Kong X., Chen H., Bu Z. Generating vesicular stomatitis virus pseudotype bearing the severe acute respiratory syndrome coronavirus spike envelope glycoprotein for rapid and safe neutralization test or cell-entry assay. Ann. N. Y. Acad. Sci. 2006;1081:246–248. doi: 10.1196/annals.1373.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert T.W., Geisbert J.B., Leung A., Daddario-DiCaprio K.M., Hensley L.E., Grolla A., Feldmann H. Single-injection vaccine protects nonhuman primates against infection with marburg virus and three species of ebola virus. J. Virol. 2009;83:7296–7304. doi: 10.1128/JVI.00561-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grehan K., Ferrara F., Temperton N. An optimised method for the production of MERS-CoV spike expressing viral pseudotypes. MethodsX. 2015;2:379–384. doi: 10.1016/j.mex.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haagmans B.L., van den Brand J.M., Raj V.S., Volz A., Wohlsein P., Smits S.L., Schipper D., Bestebroer T.M., Okba N., Fux R., Bensaid A., Solanes Foz D., Kuiken T., Baumgartner W., Segales J., Sutter G., Osterhaus A.D. An orthopoxvirus-based vaccine reduces virus excretion after MERS-CoV infection in dromedary camels. Science. 2016;351:77–81. doi: 10.1126/science.aad1283. [DOI] [PubMed] [Google Scholar]
- Hemida M.G., Elmoslemany A., Al-Hizab F., Alnaeem A., Almathen F., Faye B., Chu D.K., Perera R.A., Peiris M. Dromedary camels and the transmission of Middle East respiratory syndrome coronavirus (MERS-CoV) Transbound. Emerg. Dis. 2017;64:344–353. doi: 10.1111/tbed.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henao-Restrepo A.M., Longini I.M., Egger M., Dean N.E., Edmunds W.J., Camacho A., Carroll M.W., Doumbia M., Draguez B., Duraffour S., Enwere G., Grais R., Gunther S., Hossmann S., Konde M.K., Kone S., Kuisma E., Levine M.M., Mandal S., Norheim G., Riveros X., Soumah A., Trelle S., Vicari A.S., Watson C.H., Keita S., Kieny M.P., Rottingen J.A. Efficacy and effectiveness of an rVSV-vectored vaccine expressing Ebola surface glycoprotein: interim results from the Guinea ring vaccination cluster-randomised trial. Lancet. 2015;386:857–866. doi: 10.1016/S0140-6736(15)61117-5. [DOI] [PubMed] [Google Scholar]
- Jaume M., Yip M.S., Cheung C.Y., Leung H.L., Li P.H., Kien F., Dutry I., Callendret B., Escriou N., Altmeyer R., Nal B., Daeron M., Bruzzone R., Peiris J.S. Anti-severe acute respiratory syndrome coronavirus spike antibodies trigger infection of human immune cells via a pH- and cysteine protease-independent FcgammaR pathway. J. Virol. 2011;85:10582–10597. doi: 10.1128/JVI.00671-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayali G., Peiris M. A more detailed picture of the epidemiology of Middle East respiratory syndrome coronavirus. Lancet Infect. Dis. 2015;15:495–497. doi: 10.1016/S1473-3099(15)70128-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong D., Wen Z., Su H., Ge J., Chen W., Wang X., Wu C., Yang C., Chen H., Bu Z. Newcastle disease virus-vectored Nipah encephalitis vaccines induce B and T cell responses in mice and long-lasting neutralizing antibodies in pigs. Virology. 2012;432:327–335. doi: 10.1016/j.virol.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Korea Ministry of Health and Welfare . Korea Ministry of Health and Welfare; Sejong: 2015. Press Release: MERS Statistics.http://www.mohw.go.kr/eng/sg/ssg0111vw.jsp?PAR_MENU_ID=1001&MENU_ID=100111&page=1&CONT_SEQ=326092 Available at: [Google Scholar]
- Liu R.Q., Ge J.Y., Wang J.L., Shao Y., Zhang H.L., Wang J.L., Wen Z.Y., Bu Z.G. Newcastle disease virus-based MERS-CoV candidate vaccine elicits high-level and lasting neutralizing antibodies in Bactrian camels. J. Integr. Agr. 2017;16:2264–2273. doi: 10.1016/S2095-3119(17)61660-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malczyk A.H., Kupke A., Prufer S., Scheuplein V.A., Hutzler S., Kreuz D., Beissert T., Bauer S., Hubich-Rau S., Tondera C., Eldin H.S., Schmidt J., Vergara-Alert J., Suzer Y., Seifried J., Hanschmann K.M., Kalinke U., Herold S., Sahin U., Cichutek K., Waibler Z., Eickmann M., Becker S., Muhlebach M.D. A highly immunogenic and protective Middle East respiratory syndrome coronavirus vaccine based on a recombinant measles virus vaccine platform. J. Virol. 2015;89:11654–11667. doi: 10.1128/JVI.01815-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzi A., Feldmann F., Geisbert T.W., Feldmann H., Safronetz D. Vesicular stomatitis virus-based vaccines against Lassa and Ebola viruses. Emerg. Infect. Dis. 2015;21:305–307. doi: 10.3201/eid2102.141649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzi A., Robertson S.J., Haddock E., Feldmann F., Hanley P.W., Scott D.P., Strong J.E., Kobinger G., Best S.M., Feldmann H. EBOLA VACCINE. VSV-EBOV rapidly protects macaques against infection with the 2014/15 Ebola virus outbreak strain. Science. 2015;349:739–742. doi: 10.1126/science.aab3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memish Z.A., Mishra N., Olival K.J., Fagbo S.F., Kapoor V., Epstein J.H., Alhakeem R., Durosinloun A., Al Asmari M., Islam A., Kapoor A., Briese T., Daszak P., Al Rabeeah A.A., Lipkin W.I. Middle East respiratory syndrome coronavirus in bats, Saudi Arabia. Emerg. Infect. Dis. 2013;19:1819–1823. doi: 10.3201/eid1911.131172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millet J.K., Whittaker G.R. Host cell entry of Middle East respiratory syndrome coronavirus after two-step, furin-mediated activation of the spike protein. Proc. Natl. Acad. Sci. U. S. A. 2014;111:15214–15219. doi: 10.1073/pnas.1407087111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modjarrad K., Moorthy V.S., Ben Embarek P., Van Kerkhove M., Kim J., Kieny M.P. A roadmap for MERS-CoV research and product development: report from a World Health Organization consultation. Nat. Med. 2016;22:701–705. doi: 10.1038/nm.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster V.J., de Wit E., Feldmann H. Pneumonia from human coronavirus in a macaque model. N. Engl. J. Med. 2013;368:1560–1562. doi: 10.1056/NEJMc1215691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthumani K., Falzarano D., Reuschel E.L., Tingey C., Flingai S., Villarreal D.O., Wise M., Patel A., Izmirly A., Aljuaid A., Seliga A.M., Soule G., Morrow M., Kraynyak K.A., Khan A.S., Scott D.P., Feldmann F., LaCasse R., Meade-White K., Okumura A., Ugen K.E., Sardesai N.Y., Kim J.J., Kobinger G., Feldmann H., Weiner D.B. A synthetic consensus anti-spike protein DNA vaccine induces protective immunity against Middle East respiratory syndrome coronavirus in nonhuman primates. Sci. Transl. Med. 2015;7 doi: 10.1126/scitranslmed.aac7462. 301ra132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascal K.E., Coleman C.M., Mujica A.O., Kamat V., Badithe A., Fairhurst J., Hunt C., Strein J., Berrebi A., Sisk J.M., Matthews K.L., Babb R., Chen G., Lai K.M., Huang T.T., Olson W., Yancopoulos G.D., Stahl N., Frieman M.B., Kyratsous C.A. Pre- and postexposure efficacy of fully human antibodies against Spike protein in a novel humanized mouse model of MERS-CoV infection. Proc. Natl. Acad. Sci. U. S. A. 2015;112:8738–8743. doi: 10.1073/pnas.1510830112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Z., Dominguez S.R., Holmes K.V. Role of the spike glycoprotein of human Middle East respiratory syndrome coronavirus (MERS-CoV) in virus entry and syncytia formation. PLos One. 2013;8 doi: 10.1371/journal.pone.0076469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj V.S., Mou H., Smits S.L., Dekkers D.H., Muller M.A., Dijkman R., Muth D., Demmers J.A., Zaki A., Fouchier R.A., Thiel V., Drosten C., Rottier P.J., Osterhaus A.D., Bosch B.J., Haagmans B.L. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251–254. doi: 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reusken C.B., Haagmans B.L., Muller M.A., Gutierrez C., Godeke G.J., Meyer B., Muth D., Raj V.S., Smits-De Vries L., Corman V.M., Drexler J.F., Smits S.L., El Tahir Y.E., De Sousa R., van Beek J., Nowotny N., van Maanen K., Hidalgo-Hermoso E., Bosch B.J., Rottier P., Osterhaus A., Gortazar-Schmidt C., Drosten C., Koopmans M.P. Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect. Dis. 2013;13:859–866. doi: 10.1016/S1473-3099(13)70164-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song F., Fux R., Provacia L.B., Volz A., Eickmann M., Becker S., Osterhaus A.D., Haagmans B.L., Sutter G. Middle East respiratory syndrome coronavirus spike protein delivered by modified vaccinia virus Ankara efficiently induces virus-neutralizing antibodies. J. Virol. 2013;87:11950–11954. doi: 10.1128/JVI.01672-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volz A., Kupke A., Song F., Jany S., Fux R., Shams-Eldin H., Schmidt J., Becker C., Eickmann M., Becker S., Sutter G. Protective efficacy of recombinant modified vaccinia virus ankara delivering Middle East respiratory syndrome coronavirus spike glycoprotein. J. Virol. 2015;89:8651–8656. doi: 10.1128/JVI.00614-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Shi W., Joyce M.G., Modjarrad K., Zhang Y., Leung K., Lees C.R., Zhou T., Yassine H.M., Kanekiyo M., Yang Z.Y., Chen X., Becker M.M., Freeman M., Vogel L., Johnson J.C., Olinger G., Todd J.P., Bagci U., Solomon J., Mollura D.J., Hensley L., Jahrling P., Denison M.R., Rao S.S., Subbarao K., Kwong P.D., Mascola J.R., Kong W.P., Graham B.S. Evaluation of candidate vaccine approaches for MERS-CoV. Nat. Commun. 2015;6:7712. doi: 10.1038/ncomms8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Qi J., Yuan Y., Xuan Y., Han P., Wan Y., Ji W., Li Y., Wu Y., Wang J., Iwamoto A., Woo P.C., Yuen K.Y., Yan J., Lu G., Gao G.F. Bat origins of MERS-CoV supported by bat coronavirus HKU4 usage of human receptor CD26. Cell Host Microbe. 2014;16:328–337. doi: 10.1016/j.chom.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Ge J., Hu S., Wang Q., Wen Z., Chen H., Bu Z. Efficacy of DNA immunization with F and G protein genes of Nipah virus. Ann. N. Y. Acad. Sci. 2006;1081:243–245. doi: 10.1196/annals.1373.029. [DOI] [PubMed] [Google Scholar]
- WHO, 2017. Middle East respiratory syndrome coronavirus (MERS-CoV).
- Yang Y., Du L., Liu C., Wang L., Ma C., Tang J., Baric R.S., Jiang S., Li F. Receptor usage and cell entry of bat coronavirus HKU4 provide insight into bat-to-human transmission of MERS coronavirus. Proc. Natl. Acad. Sci. U. S. A. 2014;111:12516–12521. doi: 10.1073/pnas.1405889111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z.Y., Kong W.P., Huang Y., Roberts A., Murphy B.R., Subbarao K., Nabel G.J. A DNA vaccine induces SARS coronavirus neutralization and protective immunity in mice. Nature. 2004;428:561–564. doi: 10.1038/nature02463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Bao L., Deng W., Xu L., Li F., Lv Q., Yu P., Chen T., Xu Y., Zhu H., Yuan J., Gu S., Wei Q., Chen H., Yuen K.Y., Qin C. An animal model of MERS produced by infection of rhesus macaques with MERS coronavirus. J. Infect. Dis. 2014;209:236–242. doi: 10.1093/infdis/jit590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying T., Du L., Ju T.W., Prabakaran P., Lau C.C., Lu L., Liu Q., Wang L., Feng Y., Wang Y., Zheng B.J., Yuen K.Y., Jiang S., Dimitrov D.S. Exceptionally potent neutralization of Middle East respiratory syndrome coronavirus by human monoclonal antibodies. J. Virol. 2014;88:7796–7805. doi: 10.1128/JVI.00912-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Li K., Wohlford-Lenane C., Agnihothram S.S., Fett C., Zhao J., Gale M.J., Jr., Baric R.S., Enjuanes L., Gallagher T., McCray P.B., Jr., Perlman S. Rapid generation of a mouse model for Middle East respiratory syndrome. Proc. Natl. Acad. Sci. U. S. A. 2014;111:4970–4975. doi: 10.1073/pnas.1323279111. [DOI] [PMC free article] [PubMed] [Google Scholar]