Abstract
Hiltonol®, (Poly IC:LC), a potent immunomodulator, is a synthetic, double-stranded polyriboinosinic-polyribocytidylic acid (poly IC) stabilized with Poly-L-lysine and carboxymethyl cellulose (LC). Hiltonol® was tested for efficacy in a lethal SARS-CoV-infected BALB/c mouse model. Hiltonol® at 5, 1, 0.5 or 0.25 mg/kg/day by intranasal (i.n.) route resulted in significant survival benefit when administered at selected times 24 h prior to challenge with a lethal dose of mouse-adapted severe acute respiratory syndrome coronavirus (SARS-CoV). The infected BALB/c mice receiving the Hiltonol® treatments were also significantly effective in protecting mice against weight loss due to infection (p < 0.001). Groups of 20 mice were dosed with Hiltonol® at 2.5 or 0.75 mg/kg by intranasal instillation 7, 14, and 21 days before virus exposure and a second dose was given 24 h later, prophylactic Hiltonol® treatments (2.5 mg/kg/day) were completely protective in preventing death, and in causing significant reduction in lung hemorrhage scores, lung weights and lung virus titers. Hiltonol® was also effective as a therapeutic when give up to 8 h post virus exposure; 100% of the-infected mice were protected against death when Hiltonol® was administered at 5 mg/kg/day 8 h after infection. Our data suggest that Hiltonol® treatment of SARS-CoV infection in mice leads to substantial prophylactic and therapeutic effects and could be used for treatment of other virus disease such as those caused by MERS-CoV a related coronavirus. These properties might be therapeutically advantageous if Hiltonol® is considered for possible clinical use.
Keywords: BALB/c mouse, Hiltonol®, SARS-CoV, MERS-CoV
Highlights
-
•
We evaluated the use of Hiltonol® for treating lethal SARS-CoV-infected BALB/c mice.
-
•
Hiltonol® treatment leads to prophylactic and therapeutic effects.
-
•
These properties might be therapeutically advantageous.
1. Introduction
Severe acute respiratory syndrome coronavirus (SARS-CoV) is the causative agent of an emerging human infectious disease, severe acute respiratory syndrome (SARS) (Drosten et al., 2003, Ksiazek et al., 2003, Peiris et al., 2003b, Rota et al., 2003) and is related to the Middle East respiratory syndrome (MERS-CoV). Infections from either virus are associated with high morbidity and mortality. Due to its high morbidity and mortality, SARS has evolved as an important global respiratory disease. Even in a situation of no new infections, SARS remains a potential major health hazard, as re-emerging epidemics may arise. The serious consequences posed by virulent emerging pathogens such as SARS-CoV and MERS-CoV to which our populations have little or no immunity was highlighted by SARS outbreak in 2002–2003. The principal containment strategy to date has emphasized rapid diagnosis and isolation of infected patients and to some extent contacts with those patients. However, in spite of enormous effects and funds expended, no agents have been approved for treating SARS-CoV or MERS-CoV.
SARS-CoV has posed a serious threat to the human population and still represents a challenge for antiviral drug development and administration (Groneberg et al., 2003, Groneberg et al., 2004). Thus, numerous types of agents have been tested against SARS-CoV both in vitro and in vivo (Barnard and Kumaki, 2009). Notably, it has been shown that antibodies to the SARS-CoV spike protein block entry of the virus into cells (Sui et al., 2004) and small peptides derived from the heptad repeat (HR) regions of SARS-CoV S protein have been shown to inhibit SARS-CoV infection by interfering with SARS-CoV fusion to target cells (Bosch et al., 2004, Ho et al., 2006). Additionally, the main protease of SARS-CoV, which is essential for the replication cycle of SARS-CoV, has been a key target for developing anti-SARS-CoV drugs (Anand et al., 2003, Barnard and Kumaki, 2009, Yang et al., 2003). Another approach that was explored for treating SARS-CoV infections was to evaluate RNA species as therapies. Thus, antisense ribonucleic acid (RNA) and RNA interference (RNAi) technologies have shown potential in treating some severe diseases including SARS-CoV infection (Ahlquist, 2002, Gibson, 1994, Johnson-Saliba and Jans, 2001, Leonard and Schaffer, 2006). Using siRNAs to inhibit SARS-CoV infection in Rhesus macaques, it was demonstrated that siRNAs were effective both prophylactically and therapeutically (Chang et al., 2007). Another approach has been the use of drug combination. The combination of ribavirin and corticosteroids was the most frequently administered antiviral therapy used during the SARS outbreak (Booth et al., 2003, Ho et al., 2003, Peiris et al., 2003a, Tsang et al., 2003, Tsui et al., 2003). However, ribavirin alone at nontoxic concentrations was found to have little in vitro activity against SARS-CoV (Cinatl et al., 2003), although an improved clinical outcome was reported among SARS patients receiving early administration of Kaletra plus ribavirin and corticosteroids (Tsang and Seto, 2004). In several mouse models and in vitro, ribavirin was even found to enhance the SARS-CoV infection (Barnard et al., 2006a, Barnard et al., 2006b, Day et al., 2009). More recent data demonstrated that Urtica dioica agglutinin (UDA) treatment of SARS-CoV-infected mice lead to a substantial therapeutic effect that protected mice against death and weight loss that result from the infection (Kumaki et al., 2011b).
A class of “natural” molecules, interferons are considered as a first line of defense against viral infections in humans (Isaacs and Lindenmann, 1957, Isaacs et al., 1957). In earlier studies, we evaluated a few compounds approved for therapeutic use in humans and some in vitro inhibitors of SARS-CoV for inhibition in the mouse SARS-CoV replication model (Barnard et al., 2006a). A hybrid interferon, interferon alpha (IFN-α) B/D, and a mismatched double-stranded (ds) RNA interferon inducer, Ampligen (poly I:poly C124), were shown to potently inhibit virus titers in the lungs of infected mice (Barnard et al., 2006a). To evaluate the prophylactic potential of antivirals directed against SARS-CoV infection, new lethal animal models for SARS are needed to facilitate antiviral research. We adapted and characterized a new strain of SARS-CoV (strain v2163) that was highly lethal in 5- to 6-week-old BALB/c mice (Day et al., 2009). A number of compounds were tested for the efficacy in SARS-CoV-infected BALB/c mice (Day et al., 2009). The use of adenovirus vectored mouse interferon-alpha (mDEF201) as a prophylactic treatment and a therapeutic countermeasure for treating lethal SARS-CoV infection in BALB/c mice was very efficacious in protecting mice against death (Kumaki et al., 2011a). In other studies, treatment with an interferon inducer, polyriboinosinic-polyribocytidylic acid stabilized with poly-L-lysine and carboxymethyl cellulose (poly IC:LC), given by the intranasal route, was effective in protecting mice against a lethal infection with mouse-adapted SARS-CoV and reduced viral lung titers (Kumaki et al., 2010). The active immunomodulator, poly IC:LC (Hiltonol®), was effective when therapy was initiated 24 h before infection or as late as 8 h after virus inoculation, at a time when clinical signs of SARS were being manifested in the BALB/c mice. In this report, we further evaluated the use of Hiltonol® as an extended prophylactic or therapeutic countermeasure for treating lethal SARS-CoV infection in BALB/c mice caused by a mouse-adapted SARS-CoV. In addition, its value as a vaccine adjuvant was assessed.
2. Materials and methods
2.1. Cells
Vero 76 cells were obtained from American Type Culture Collection (ATCC, Manassas, VA), and were routinely grown in minimal essential medium (MEM) supplemented with 10% heat-inactivated fetal bovine serum (FBS, Thermo Fisher Scientific Co., Logan, UT). For in vitro antiviral assays, the serum was reduced to 2% FBS and gentamicin was added to the medium up to a final concentration of 50 μg/ml.
2.2. SARS-CoV Urbani strain and mouse-adapted SARS-CoV
SARS-CoV, strain Urbani (200300592), was obtained from Centers for Disease Control and Prevention (CDC, Atlanta, GA, USA). This strain was propagated and titrated in Vero 76 cells.
The mouse-adapted SARS-CoV strain has previously been described (Day et al., 2009). Briefly, the mice were infected with the Urbani strain. Three or five days after infection, the lungs were removed and homogenized and then used to re-infect a subsequent group of mice. This infection step was continued 25 times through BALB/c mice lungs. The virus was then plaque-purified 3 times and yielded a virus causing severe lung disease and mortality in infected mice. The virus was verified as SARS-CoV by enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR). All experiments involving infectious viruses were conducted in an approved biosafety level 3+ (BSL-3+) laboratory.
2.3. Test interferon inducer
The interferon inducer, polyriboinosinic-polyribocytidylic acid stabilized with poly-L-lysine and carboxymethyl cellulose Hiltonol® (poly IC:LC) was obtained from Andres M. Salazar (Oncovir, Inc., Washington, DC 20008). Hiltonol® was diluted in physiologically sterile saline (PSS) for in vivo experiments just before use. Ampligen® was provided by Hemispherx Biopharma (Philadelphia, PA 19103).
2.4. Animals
Specific pathogen-free female 16–20 g BALB/c mice were obtained from Charles River Laboratories (Wilmington, MA) for this study mainly. Female 16–18 g B6.129S2-Il6tm1Kopf/J and the parent strain C57BL/6J were obtained from Jackson Laboratories (Bar Harbor, Maine). Female 17–20 g C57BL/6J/10ScNJ and the parental strain mice C57BL/6J were obtained from Charles River Laboratories (Wilmington, MA). They were maintained on Wayne Lab Blox and fed with standard mouse chow and tap water ad libitum. All the mice were quarantined for 24 h prior to use. The animal studies were done in an approved bio-safety level 3+ animal facility. Personnel entering the facility wore powered air-purifying respirators (3M HEPA Air-Mate; 3M, Saint Paul, MN) and Tyvek body protection suits. Animal studies had been approved by Utah State University Animal Care Committee.
2.5. Experimental design
The general experimental design is described below. The BALB/c mice were anesthetized with a 0.1 ml intraperitoneal injection of 20 mg/kg of Ketamine® and the mouse-adapted SARS-CoV was administered intranasally (i.n.) in a volume of 0.05 ml. Groups of 10 mice were administered Hiltonol® or vehicle placebo i.n. at selected times prior to challenge with 2.5 × 103 PFU of mouse-adapted SARS-CoV. Ampligen was administered i.n. 24 h before virus exposure and 8 h after exposure to virus and served as a positive control for controlling the virus infection. Fifteen mice were treated i.n. with PSS at various times prior to virus exposure. Mice in this group represented the placebo controls. SARS-CoV-infected and mock-infected mice were weighed every day and clinical signs of disease were also observed and recorded daily. Animal deaths were recorded for up to 21 days post virus exposure. Following intranasal administration of SARS-CoV, five mice from each group were sacrificed on day 3 and 6 for lung score, lung weight and lung titer determinations. Animals that lost greater than 30% of their initial body weight were humanely euthanized by CO2 asphyxiation, and the day of euthanization was designated as the day of death due to infection.
2.6. Compound toxicity determination
For Hiltonol®, a dose range finding experiment was carried out to determine the maximum tolerated concentration. Three mice were used per treatment group. Toxicity was evaluated in terms of weight change and adverse events. Mice were weighed every day from 24 h prior to virus infection to day 21 post virus exposure. Adverse events for which observations were made included ruffling of fur, lethargy, paralysis, incontinence, repetitive circular motion, and aggression.
2.7. Lung score/lung weight determinations
Samples from each mouse lung lobe were weighed and placed in a petri dish. Lungs were scored based on surface appearance of lungs. Lungs were then assigned a score ranging from 0 to 4, with 0 indicating that the lungs looked normal and 4 denoting that the entire surface area of the lungs was inflamed and exhibited plum colored lung discoloration (Sidwell et al., 1995). Significant differences in lung scores were determined by Kruskal-Wallis test followed by Dunn's pairwise comparison post tests. One-way analysis of variance (ANOVA) was used to probe for significant differences in lung weights. Pairwise comparisons were made by Sidak's multiple comparison tests.
2.8. Lung virus titer determination
Lung virus titers were analyzed from mice sacrificed on day 3 and 6 post virus exposure. A lobe from each mouse lung was homogenized in MEM supplemented with 10% FBS and the tissue fragments were allowed to settle. The varying dilutions of the supernatant fluids were assayed in triplicate for infectious virus in Vero 76 cells by cytopathic effect (CPE) assay. The titers (50% tissue culture infectious dose, CCID50 values) were calculated using the Reed-Muench method (Reed and Muench, 1938). Significant differences were detected by ANOVA. Pairwise comparisons were made by Sidak's multiple comparison tests.
2.9. Neutralizing antibody assay
Sera were harvested by submandibular bleeding from surviving mice at day 7 and day14 after virus challenge. 7 μl aliquot of each serum sample was added to approximately 63 μl of MEM, mixed, then serially diluted by 1/2 to achieve 1/40 to 1/8192 dilutions in 96-well plates. Virus stock was diluted in MEM to approximately 200 CCID50 per 60 μl. Next 60 μl of virus was added to each well, the plates vibrated for approximately 1 min, and then incubated for 1 h at 37 °C for neutralization. 100 μl of the liquid from each well was then transferred to 96-well plates containing sub-confluent monolayers of Vero 76 cells, and 100 μl of MEM + 4% FBS was added to each well. Plates were sealed with tape, incubated for 5 days at 37 °C with 5% CO2, and scored for the presence or absence of virus cytopathic effect. Uninfected wells served as a negative cell control, and a serum sample with known anti-SARS antibody served as a positive control. Results were reported as the inverse of the greatest dilution where virus CPE was not detected.
2.10. Histopathology
Group of mice infected as described previously were sacrificed on day 3 and either on 6 or 7 post virus exposure. The lungs from these mock-infected or infected mice were collected and formalin-fixed. The lungs from each group were sectioned and stained with H&E stain and evaluated by a board certified veterinary pathologist for histopathological changes.
2.11. Statistical analysis
Mice were weighed in groups prior to treatment and then every day thereafter to determine the average weight change for all animals in each treatment group. Weights were expressed as group averages for each day and evaluated by the two-way analysis of variance for significant differences among treatment groups followed by pairwise comparisons using Dunnett's multiple comparison tests.
Survival analysis was done using the Kaplan-Meier graphical method and a Logrank test. The analysis revealed significant differences among the treatment groups. Therefore, pairwise comparisons of survivor curves (PSS versus any treatment) were analyzed by the Gehan-Breslow-Wilcoxon pairwise comparisons test, and the relative significance was adjusted to a Bonferroni-corrected significance threshold for the number of treatment comparisons done. Mean day of death was calculated and analyzed by the Kruskal-Wallis test, followed by Dunn's post tests for evaluating the significant pairwise comparisons. Live numbers per total mice in a group differences were evaluated by contingency table analysis. Fisher's exact tests were used to make pairwise comparisons to placebo-treated mice.
3. Results
3.1. Effects of Hiltonol® on weight change of uninfected female BALB/c mice
Most mice randomly assigned to the toxicity control groups gained weight at rates nearly equal to mice receiving PSS (data not shown). The mice treated with Hiltonol® at 5.0 or 2.5 or 1.0 mg/kg/day were the groups to lose noticeable amounts of weight, which occurred at day 2. However, they regained the lost body weight after the nadir of weight loss at day 2. The mice in these groups managed to rapidly regain all lost weight by the end of the experiment. No other adverse events were observed for any of the toxicity control mice used in the experiment.
3.2. Evaluation various dosing regimens of Hiltonol® in a lethal SARS-CoV infection in a BALB/c mouse model
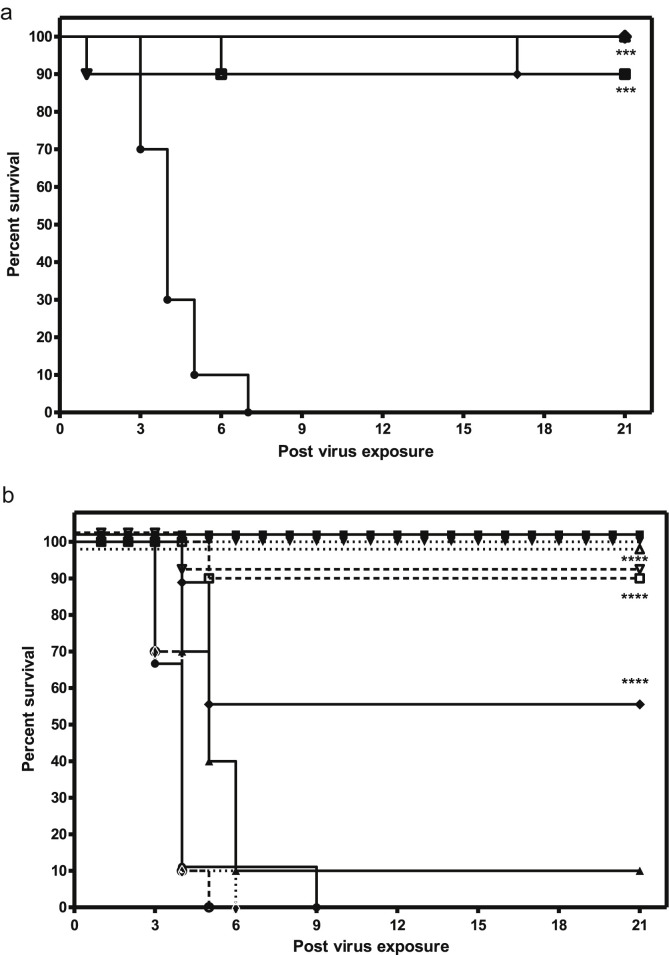
In a previous study, BALB/c mice inoculated intranasally with mouse-adapted SARS-CoV, the infected mice died between 4 and 8 days, with 90–100% mortality rate achieved by day 8. The lungs were severely inflamed and exhibited extreme lung consolidation. The efficient viral replication was observed from day 3–6 in the lungs (Day et al., 2009). Virus titers often exceeded 106/ml at peak replication during day 3–4. Weight loss was excessive. In the current study, group of 10 mice were administered Hiltonol® or vehicle placebo i.n. at selected times prior to or after virus challenge with mouse-adapted SARS-CoV. Some mice received additional doses of Hiltonol® after virus challenge. All doses and treatment regimens of Hiltonol® significantly protected mice against a lethal infection of BALB/c mice exposed to SARS-CoV (Fig. 1 A, p < 0.0001; Table 1 ). Only three mice died using Hiltonol®, one mouse at day 4 post virus exposure when dosed with 5 mg/kg/day once 24 h before infection, and one mouse at day 4 when receiving Hiltonol® at 5 mg/kg/day dose given once 12 h after infection, and one mouse at day 11 when treated three times with a lower dose of Hiltonol® (1 mg/kg/day 24 before, and at 24 and 48 h after infection). These treated, SARS-CoV-infected mice receiving the various Hiltonol® dosing regimens were also significantly protected against weight loss due to virus infection (Table 1, p < 0.05-p<0.001) from days 0–3 post virus exposure when the greatest weight loss occurred in this mouse model.
Fig. 1.
A. Effects of Hiltonol® on survival of BALB/c mice with a lethal SARS-CoV infection. ***p < 0.001 versus PSS. The SARS-CoV-infected BALB/c mice were treated with PSS (●: −24 h, +24 h, +48 h); Hiltonol® at 5 mg/kg/day (■: −24 h, +24 h, +48 h), (▲: −24 h, +8 h, +48 h), (▼: −16 h, +8 h, +24 h), (◆: +12 h), (○: −24 h); Hiltonol® at 1.0 mg/kg/day (□: −24 h, +24 h, +48 h), (△: −24 h, +8 h, +24 h), (▽: −16 h, +8 h, +32 h), (◇: −24 h). B. Effects of various long-term dosing regimens of Hiltonol® on survival of BALB/c mice with a lethal SARS-CoV infection. ****p < 0.0001 versus PSS. The SARS-CoV-infected BALB/c mice were treated with PSS (●: day −21), (○: day −14), (◇: day −7); Hiltonol® (■: 2.5 mg/kg/day −21), (□: 2.5 mg/kg/day −14), (▼: 2.5 mg/kg/day −7); (▲: 0.75 mg/kg/day −21), (▽: 0.75 mg/kg/day −14), (△: 0.75 mg/kg/day −7). A second dose was given 24 h later. (♦) Ampligen® 10 mg/kg/day (bid x 2 beg, 4 h).
Table 1.
Effects of various dosing regimens of Hiltonol® on a lethal SARS-CoV infection in a BALB/c mouse model.
| Treatments | Live/total | Mean day of death ± SD | Weight loss from day 0 to day 3 (g) | Average weight through day 18 (g) ± SD |
|---|---|---|---|---|
| PSS (−24, +24, +48 h) | 0/10 | 4.2 ± 1.2*** | 2.5 | 15.9 ± 2.7 |
| Hiltonol® 5 mg/kg/day (−24, +24, +48 h) | 10/10 | >18 | 0.4 | 17.8 ± 0.5*** |
| Hiltonol® 5 mg/kg/day (−24, +8, +24 h) | 10/10 | >18 | 0.7 | 17.7 ± 0.5*** |
| Hiltonol® 5 mg/kg/day (−16, +8, +32 h) | 10/10 | >18 | 1.0 | 17.9 ± 0.7*** |
| Hiltonol® 5 mg/kg/day (−24 h) | 9/10 | 4 | 2.7 | 16.7 ± 1.13* |
| Hiltonol® 5 mg/kg/day (+12 h) | 9/10 | 4 | 0.7 | 18.2 ± 0.5*** |
| Hiltonol® 1 mg/kg/day (−24, +24, +48 h) | 9/10 | 11 | 1.1 | 17.4 ± 0.5* |
| Hiltonol® 1 mg/kg/day (−24, +8, +24 h) | 10/10 | >18 | 0.1 | 17.3 ± 0.6* |
| Hiltonol® 1 mg/kg/day (−16, +8, +32 h) | 10/10 | >18 | 0.5 | 17.3 ± 0.8* |
| Hiltonol® 1 mg/kg/day (−24 h) | 10/10 | >18 | 0.3 | 18.4 ± 0.2*** |
| Hiltonol® 0.5 mg/kg/day (−24, +24, +48 h) | 10/10 | >18 | 0.2 | 17.6 ± 0.3* |
| Hiltonol® 0.5 mg/kg/day (−24, +8, +24 h) | 10/10 | >18 | 0.4 | 17.2 ± 0.3* |
| Hiltonol® 0.5 mg/kg/day (−16, +8, +32 h) | 10/10 | >18 | 0.3 | 17.3 ± 0.5* |
| Hiltonol® 0.25 mg/kg/day (−24, +24, +48 h) | 10/10 | >18 | 0.2 | 17.6 ± 0.4** |
| Hiltonol® 0.25 mg/kg/day (−24, +8, +24 h) | 10/10 | >18 | 0.0 | 17.5 ± 0.4** |
| Hiltonol® 0.25 mg/kg/day (−16, +8, +32 h) | 10/10 | >18 | 0.0 | 18.0 ± 0.4*** |
*p < 0.05, **p < 0.01, ***p < 0.001.
3.3. Extended prophylaxis with Hiltonol® protects SARS-CoV-infected BALB/c mice from mortality
We also evaluated how far before the initial virus challenge time prophylactic dosing regimens would be efficacious in protecting mice from the lethal challenge with SARS-CoV. Groups of 20 mice were dosed with Hiltonol® at 2.5 or 0.75 mg/kg by intranasal (i.n.) instillation on days 7, 14, or 21 before virus exposure. A second dose was given 24 h later. Hiltonol® when administered at 2.5 mg/kg/day beginning at day 14 or 21 before virus exposure protected 90–100% of infected mice against death due to the virus infection (Fig. 1, p < 0.0001). The only Hiltonol® dosing regimen that was not very protective was when it was administered at 0.75 mg/kg, one time, 21 days prior to exposing mice to virus. Ampligen® used at 10 mg/kg, significantly (p < 0.0001), yet only protected 50% of the mice from death using the designated therapeutic treatment regimen. At the critical time of day 5 post virus exposure, when many mice began to die in the placebo treated groups, mice treated with Hiltonol® at 2.5 mg/kg 14 or 21 days before infection seemed to be least susceptible to weight loss due to virus infection compared to the corresponding the placebo controls (data not shown). The placebo-treated mice usually died at day 3–4 (Table 2 ), whereas mice treated with the higher dose of Hiltonol® survived in significant numbers (p < 0.001). It was also obvious that mice treated with lower dose of Hiltonol® survived in significant numbers provided that Hiltonol® was administered 14 or 7 days before virus infection. When administered at 0.75 mg/kg/day 21 days before virus infection, almost all treated mice in the Hiltonol® group died with a mean day of death equivalent to the corresponding placebo control group (Table 2). Ampligen® was given i.p. twice a day beginning 4 h before infection at 10 mg/kg. The mice receiving Ampligen® were slightly yet significantly protected against death (50% survivors Table 2, p < 0.05).
Table 2.
Effects of various long-term dosing regimens of Hiltonol® on survival of BALB/c mice with a lethal SARS-CoV infection.
| Treatment | Dosing regimen (day prior to virus exposure) | Survivors/total | Mean day of death ± SD |
|---|---|---|---|
| PSS | 21 | 0/10 | 4.4 ± 1.8 |
| Hiltonol® (2.5 mg/kg/day) | 21 | 10/10*** | >21*** |
| Hiltonol® (0.75 mg/kg/day) | 21 | 1/10 | 5.0 ± 0.9 |
| PSS | 14 | 0/10 | 3.8 ± 0.6 |
| Hiltonol® (2.5 mg/kg/day) | 14 | 9/10*** | 5.0 ± 0.0 |
| Hiltonol® (0.75 mg/kg/day) | 14 | 9/10*** | 4.0 ± 0.0 |
| PSS | 7 | 0/10 | 3.7 ± 0.5 |
| Hiltonol® (2.5 mg/kg/day) | 7 | 10/10*** | >21*** |
| Hiltonol® (0.75 mg/kg/day) | 7 | 10/10*** | >21*** |
| Ampligen® (10 mg/kg/day) | bid x 2, beg −4 h | 5/10* | 5.8 ± 2.4 |
*p < 0.05, ***p < 0.001 compared to PSS control.
3.4. Effects of Hiltonol® on lung scores, lung weights, and virus lung titers of female BALB/c mice infected with a lethal dose of mouse-adapted SARS-CoV at day 3 post virus exposure
Other parameters measured to determine the extent of the efficacy of the two prophylactic doses of Hiltonol® included effects on gross lung pathology, lung weights, and virus lung titers. At day 3 after mice were exposed to virus, the 2.5 mg/kg dose of Hiltonol® significantly ameliorated the extent of damage induced by the virus infection was observed on the surface of lungs of infected mice (p < 0.05, Table 3 ). There was little or no surface hemorrhaging observed. In addition, almost all mice treated with this dose of Hiltonol®, regardless of the time of administration, were protected to the same extent (Table 3). The treatment with the lower dose of Hiltonol® led to similar results of less observable surface lung pathology, especially for mice treated with Hiltonol® beginning at day 14 before virus exposure (p < 0.05).
Table 3.
Effects of various long-term dosing regimens of Hiltonol® at day 3 post virus exposure on various lung parameters in BALB/c mice infected with SARS-CoV.
| Treatment | Virus titer (Log10CCID50/g) ± SD | Virus Lung Score ± SD | Lung Weight (g) ± SD |
|---|---|---|---|
| Treatment Day -21 | |||
| PSS | 6.11 ± 0.41 | 2.1 ± 0.5 | 0.28 ± 0.02 |
| Hiltonol® (2.5 mg/kg/day) | 5.50 ± 0.39 | 0.3 ± 0.3* | 0.21 ± 0.03* |
| Hiltonol® (0.75 mg/kg/day) | 5.58 ± 0.30 | 0.4 ± 0.5 | 0.31 ± 0.03 |
| Treatment Day −14 | |||
| PSS | 5.76 ± 0.43 | 3.7 ± 0.3 | 0.34 ± 0.03 |
| Hiltonol® (2.5 mg/kg/day) | 4.95 ± 0.56** | 0.0 ± 0.0* | 0.20 ± 0.02** |
| Hiltonol® (0.75 mg/kg/day) | 6.04 ± 0.38 | 0.5 ± 0.0* | 0.24 ± 0.04 |
| Treatment Day -7 | |||
| PSS | 5.94 ± 0.34 | 3.4 ± 1.0 | 0.34 ± 0.05 |
| Hiltonol® (2.5 mg/kg/day) | 5.58 ± 0.65 | 0.0 ± 0.0* | 0.22 ± 0.02* |
| Hiltonol® (0.75 mg/kg/day) | 6.05 ± 0.27 | 0.4 ± 0.4 | 0.21 ± 0.04** |
| Ampligen® (10 mg/kg/day) bid x 2, beg −4 h | 6.49 ± 0.31 | 1.2 ± 1.4 | 0.26 ± 0.1 |
*p < 0.05, **p < 0.01 compared to PSS control.
Another indicator of the extent of an inflammatory response in the lungs is edema. Edema can be indirectly measured by evaluating the weight of an infected lung. At day 3 of the virus infection, dosing with the 2.5 mg/kg of Hiltonol® using any treatment regimen significantly prevented an increase in lung weights of treated mice, a manifestation of edema (Table 3, p < 0.05-p<0.01). However, the efficacy of repression edema was much less pronounced in mice receiving the 0.75 mg/kg dose of Hiltonol®. Ampligen® treatment resulted in a similar efficacy profile in preventing edema as was seen with mice dosed with Hiltonol® at 0.75 mg/kg. Did this apparent moderation of the inflammatory response both in the lungs and on the surface of the lungs due correlate with a reduction of virus replication in the lungs of infected mice, the presence of virus protein the likely culprit for inducing edema? In general, virus lung titers at day 3 after inoculation with virus were almost 0.5 log10 lower or more in mice treated with 2.5 mg/kg Hiltonol® compared to the placebo-treated control (Table 3). However, only the virus lungs titers of mice treated with 2.5 mg/kg Hiltonol® 14 days before infection were significantly reduced compared to the virus titers of mice receiving PSS. They were reduced by almost one log10 compared to the placebo treated mice (Table 3). None of the other treatments, including Ampligen®, achieved such a reduction in virus lung titer.
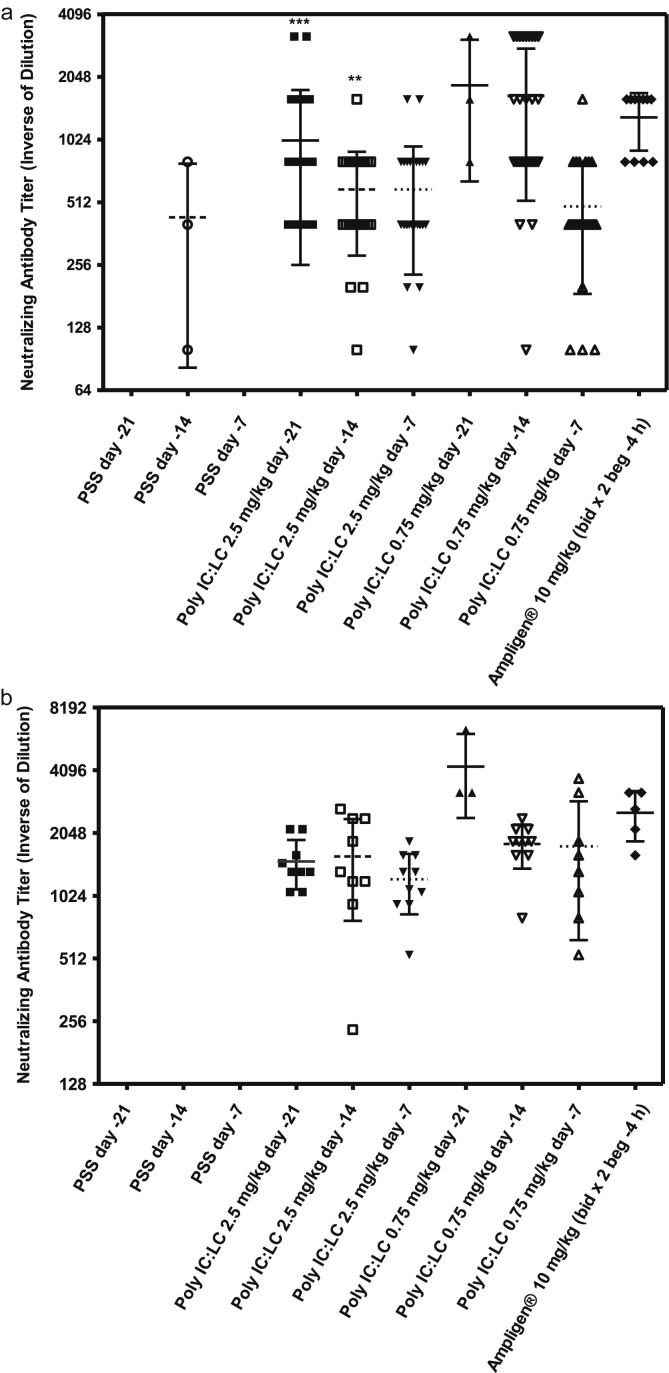
3.5. Effects of various long-term dosing regimens of Hiltonol® on neutralizing antibody titers of BALB/c mice at day 7 and 14 post challenge with a lethal dose of SARS-CoV
It is conceivable that an immune modulator such as an interferon inducer could suppress normal adaptive immune responses such as the formation of neutralizing antibody. The effects of Hiltonol® treatment on immune responsiveness were also investigated by analyzing the neutralizing antibody levels to the virus 7 and 14 days after virus challenge. Sera from all groups of mice used in the long term prophylaxis experiment were analyzed for neutralizing antibody (Fig. 2 A and B). The data suggest that the mice treated with the high dose of Hiltonol® could still mount a robust virus neutralization response, even though the drug did significantly reduce virus lung titers in only one case. In fact, mice receiving pretreatment with Hiltonol® beginning at day 21 and day 14 before virus challenge had significant higher neutralizing antibody titers than did the corresponding placebo-treated mice (Fig. 2A; p < 0.001, p < 0.0001; respectively). The neutralizing antibody titers remained equivalently high or higher at day 14 post virus challenge (Fig. 2B). Interestingly, the group of mice receiving the lowest dose of Hiltonol® appeared to have the higher neutralizing antibody titers at day 14 than at day 7. One could speculate that this observation was driven by the fact that virus titers were higher in these mice. Treatment of mice with low dose Hiltonol® and Ampligen® also showed similar results. This would suggest that this dose of Hiltonol® did not adversely affect the adaptive immune response.
Fig. 2.
Effects of various long-term dosing regimens of Hiltonol® on neutralizing antibody titers of BALB/c mice at day 7 (A) and 14 (B) post virus challenge with a lethal dose of SARS-CoV. **p < 0.01 versus PSS (day −14), ***p < 0.001 versus Hiltonol® 2.5 mg/kg (day −14) or Hiltonol® 0.75 mg/kg (day −7). The SARS-CoV-infected BALB/c mice were treated with PSS (●: day −21), (○: day −14), (◇: day −7); Hiltonol® (■: 2.5 mg/kg/day −21), (□: 2.5 mg/kg/day −14), (▼: 2.5 mg/kg/day −7); (▲: 0.75 mg/kg/day −21), (▽: 0.75 mg/kg/day −14), (△: 0.75 mg/kg/day −7), (♦) Ampligen® 10 mg/kg/day (bid x 2 beg, 4 h).
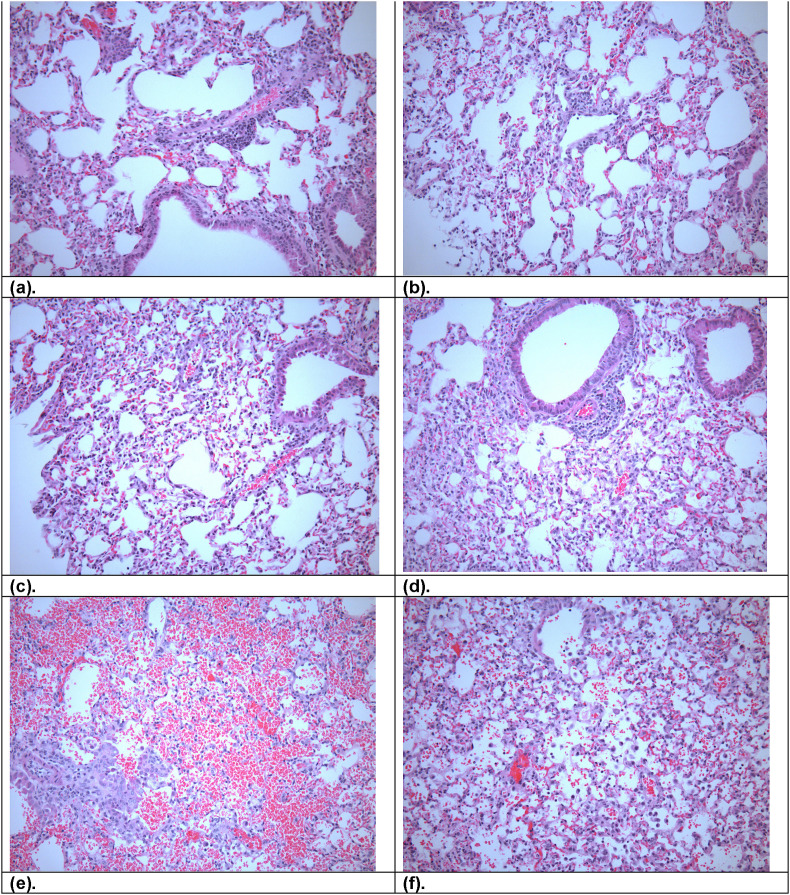
3.6. Histopathology
In general, lungs infected with SARS-CoV should show acute to subacute alveolitis with some perivascular edema in some sections. Lungs of mice inoculated with SARS-CoV showed no significant changes, and mock-infected controls showed no marked changes except moderate rims of lymphocytes surrounding scattered vessels (Fig. 3 ). Also, the pathological changes were not observed in the SARS-CoV-infected, Hiltonol®-treated lungs (Fig. 3). However, significant pathological differences in the distribution of inflammatory cells between the SARS-CoV-infected and the mock-infected lungs were not observed. Three SARS-CoV-infected, Hiltonol®-treated lung samples (2.5 mg/kg 7 days before virus exposure) were evaluated for pathological change on day 6 after inoculation. In Ampligen®-treated mice, the positive control-treated group, the infection was very limited with little or no evidence of an inflammatory response in the lungs from the mouse that was observed, although there was a tremendous amount of erythrocyte infiltration in the air spaces (Fig. 3f).
Fig. 3.
Histological slides show representative lung pathology. (a). SARS-CoV-infected, Hiltonol®-treated lung with small numbers of neutrophils within groups of alveoli and moderate rims of lymphocytes surrounding scattered vessels. (b). SARS-CoV-infected, Hiltonol®-treated lung with moderate rims of lymphocytes surrounding scattered vessels. (c). SARS-CoV-infected, Hiltonol®-treated lung with clusters of alveolar macrophages and neutrophils filled small groups of alveoli. (d). Un-infected, Hiltonol®-treated lung with moderate rims of lymphocytes surround scattered vessels. (e). SARS-CoV-infected, Ampligen®-treated lung with approximately 80% airspaces contain erythrocytes. (f). SARS-CoV-infected, PSS-treated lung with small number of alveolar macrophages and fewer neutrophils within alveoli.
3.7. SARS-CoV-infected mice were protected against death when Hiltonol® was administered 8 h after infection
The efficacy of Hiltonol® (5 mg/kg/day) as a treatment for SARS-CoV infection was evaluated with Hiltonol® at 8, 16, 24, 32, 48 or 72 h post virus challenge. Survival and weights were monitored daily for at least 14 days. Hiltonol® given at 5 mg/kg/day resulted in 90% survival of treated, infected mice when administered 8 h post virus challenge, at a time when clinical signs of SARS are starting to be manifested in the untreated BALB/c mice (p < 0.001, Table 4 ). In addition, treatment with Hiltonol® at 5 mg/kg/day by intranasal route resulted in 100% survival when it was given twice, 8 and then 24 h post virus exposure (Table 4, p < 0.001). These data suggest that Hiltonol® treatment of SARS-CoV infection in mice leads to substantial therapeutic effect that protects mice against death only when administered within 8 h after virus exposure or when using a therapeutic multiple dosing regimen. Hiltonol® given one time at 5 mg/kg/day was not protective against death when treatment was at 32, 48 or 72 h after SARS-CoV infection (Table 4). When Hiltonol® was administered intranasally 16 or 24 h post virus challenge, the data showed partial survival (Table 4). In another subsequent therapeutic experiment, Hiltonol® was administered intranasally 16 and 24 h post virus exposure. At day 6, 60% of mice receiving Hiltonol® 16 and 24 h after exposure to virus were still alive compared with the other therapeutic regimens in which all were dead or only one mouse had survived (data not shown). This data suggest that treatment beginning 16 h after virus exposure might temporarily prolong survival, but that the pathogenesis caused by the virus finally overwhelms the mice.
Table 4.
Effects of various long-term dosing regimens of Hiltonol® on death of BALB/c mice infected with a lethal dose of SARS-CoV post virus exposure.
| Treatment | Dosing regimen (hour post virus exposure) | Live/total | Mean day of death |
|---|---|---|---|
| PSS | −24, + 24, +48, 72 h | 1/10 | 6.0 |
| Hiltonol® (5 mg/kg/day) | +8 h | 9/10*** | Undefined |
| Hiltonol® (5 mg/kg/day) | +16 h | 4/10 | 6.5 |
| Hiltonol® (5 mg/kg/day) | +24 h | 3/10 | 6.0 |
| Hiltonol® (5 mg/kg/day) | +32 h | 1/10 | 4.0 |
| Hiltonol® (5 mg/kg/day) | +48 h | 0/10 | 5.0 |
| Hiltonol® (5 mg/kg/day) | +72 h | 0/10 | 6.0 |
| Hiltonol® (5 mg/kg/day) | +8, + 24 h | 10/10*** | Undefined |
| Hiltonol® (5 mg/kg/day) | −24, +8, +32 h | 10/10*** | Undefined |
***p < 0.001 versus PSS control.
3.8. Evaluating therapeutic dosing regimens of treating SARS-CoV infection in interleukin 6 knockout (IL-6 -/-) mice with Hiltonol®
Interleukin 6 (IL-6) is a multifunctional cytokine that regulates the immune response, hematopoiesis, the acute phase response, and inflammation (Hirano, 1998). We have previously reported that IL-6 levels were increased in SARS-CoV-infected mice, and high IL-6 expression was associated with mortality (Day et al., 2009). Therefore, we evaluated the effects of virus infection in mice deficient in IL-6 (B6.129S2-IL6tmlKopf/J). Since these IL-6 mutant mice show defects in responses to various viruses and in inflammatory responses to infection, we hypothesized that mortality and disease parameters might be reduced in IL-6 -/- mice infected with SARS-CoV because increased IL-6 levels contributed greatly to the lethality of the infection in normal mice (Day et al., 2009). This hypothesis assumed that IL-6 production was a major source of lung disease in SARS-CoV-infected mice. When both SARS-CoV-infected mice (C57BL/6J, IL-6 +/+ and B6.129S2-IL6tm1Kopf/J, IL-6 -/-) were treated with Hiltonol® at 1.0 mg/kg/day, the typical depression of weight gain by Hiltonol® treatment was observed at days 3–4, although it was significantly more severe in the B6.129S2-IL6tm1Kopf/J mice (IL-6 -/-) (data not shown). However, the surviving mice gained back the lost weight by the end of the experiment. Hiltonol® did not significantly protect mice from death in either strain of mouse compared to the placebo-treated mice of both strains (Table 5 ) and IL-6 -/- mice still supported virus lung replication. In addition, the mean day of death was the same for all groups. However, the virus lung titers in these mice were significantly reduced at day 3 post virus exposure (Table 6 , p < 0.001). All IL-6 -/- mice had significantly highly virus titers than did the normal C57BL/6J mice (Table 6, p < 0.001), suggesting that IL-6 was necessary to control virus replication in the lungs. Interestingly, at day 6, Hiltonol®-treated IL-6 -/- mice had significantly increased virus lung titers compared to untreated, infected IL-6 +/+ mice (Table 6, p < 0.001). In addition, the virus infection of the lungs likely induced a significant yet slight inflammatory response in untreated, infected IL-6 -/- mice (p < 0.05), as measured by the increase in lung score but there was no induction of edema in these mice as can be seen by the normal lung weights (Table 6). The inability to significantly control virus replication may be one of reasons why IL-6 -/- mice were not protected against death. Thus, virus cytopathic effects may have sufficiently destroyed enough lung cells to contribute to poor lung function that may have lead to death for mice that succumbed because of the virus infection. Our data suggest that these mice (57BL/6J mice, B6.129S2-Il6tm1Kopf/J mice, IL-6 -/-) lack a pathway with which Hiltonol® interacts to prevent lethal SARS-CoV infection in mice.
Table 5.
Effects of Hiltonol® on the death of C57BL/6J and B6.129S2-IL6m1kopf/J mice infected with a lethal dose of mouse-adapted SARS-CoV.
| Treatment | Dosing regimen (hour post virus exposure) | Live/total | Mean day of death |
|---|---|---|---|
| PSS C57BL/6J | −24, +8, +32 h | 8/20 | 4.8 ± 2.3 |
| Hiltonol® C57BL/6J | −24, +8, +32 h | 7/20 | 4.6 ± 2.2 |
| PSS B6.129S2-IL6tm1Kopf/J | −24, +8, +32 h | 4/10 | 4.5 ± 2.3 |
| Hiltonol® B6.129S2-IL6tm1Kopf/J | −24, +8, +32 h | 4/10 | 4.8 ± 1.7 |
***p < 0.001 versus PSS control.
Table 6.
Effects of Hiltonol® on various lung parameters measured in IL-6 knockout mice (IL-6 -/-) mice infected with mouse adapted SARS-CoV.
| Treatment | Virus titer (Log10 CCID50/g) ± SD | Visual lung score ± SD | Lung weight (g) ± SD |
|---|---|---|---|
| Day 3 | |||
| PSS C57BL/6J | 6.27 ± 0.07 | 0.0 ± 0.0 | 0.32 ± 0.35* |
| Hiltonol® (1 mg/kg/) C57BL/6J | 4.31 ± 0.09*** | 0.0 ± 0.0 | 0.12 ± 0.02 |
| PSS B6.129S2-IL6tm1Kopf/j | 6.75 ± 0.12 | 0.3 ± 0.3* | 0.06 ± 0.01 |
| Hiltonol® (1 mg/kg/) B6.129S2-IL6tm1Kopf/j | 5.02 ± 0.15*** | 0.0 ± 0.0 | 0.09 ± 0.02 |
| Day 6 | |||
| PSS C57BL/6J | 3.51 ± 0.09 | 0.0 ± 0.0 | 0.12 ± 0.05 |
| Hiltonol® (1 mg/kg/) C57BL/6J | 4.94 ± 0.02*** | 0.0 ± 0.0 | 0.12 ± 0.02 |
| PSS B6. 129S2-IL6tm1Kopf/j | 4.65 ± 0.12 | 0.3 ± 0.4 | 0.11 ± 0.01 |
| Hiltonol® (1 mg/kg/) B6.129S2-IL6tm1Kopf/j | 5.36 ± 0.00*** | 0.0 ± 0.0 | 0.09 ± 0.00 |
***p < 0.001 versus PSS control.
3.9. Evaluation of a therapeutic dosing regimen of Hiltonol® for treating SARS-CoV infections in toll-like receptor 4 (TLR-4) knockout mice
Khanolkar et al. reported that C3H/HeJ mice harboring a natural mutation in the gene that encodes Toll-like receptor 4 (TLR4) that disrupts its normal function exhibited the enhanced morbidity and mortality following i.n. mouse hepatitis virus strain 1 (MHV-1) infection, indicating that TLR-4 plays an important role in respiratory CoV pathogenesis (Khanolkar et al., 2009). In the current study, we hypothesized that intranasal infection of TLR4 -/- mice with mouse-adapted SARS-CoV would result in an acute respiratory disease with a higher lethality. When both strains (C57BL/6J and C57BL/6J/10ScNJ TLR-4 -/- mice) were infected with SARS-CoV and treated with Hiltonol®, infected, untreated C57BL/6J mice lost weight, but onset of weight loss was delayed relative to Hiltonol®-treated, infected mice (data not shown). An exception was the one C57BL/6J/10ScNJ TLR-4 -/- mouse that died at day 5 post virus exposure. Despite not inducing death of these strains of mice, the virus was able to replicate quite rigorously in the lungs of C57BL/6J mice (Table 7 ) as previously seen in other mice (Table 6). Yet the virus induced no significant inflammatory response, as manifested by lack of increased lung scores and lack of induction of edema manifested as normal lung weights (Table 7). Nevertheless, virus lung titers were dramatically reduced in both strains of mice treated with Hiltonol® (p < 0.001), but more so in the C57BL/6J/10ScNJ TLR-4 -/- mice, especially at day 6. In addition, the C57BL/6J/10ScNJ mice were less suitable hosts for prolonged lung virus replication than the C57BL/6J mice, because virus lung titers at day 6 in C57BL/6J/10ScNJ TLR-4 -/- mice were significantly lower than in C57BL/6J mice (p < 0.01). These data indicated that Hiltonol® action appeared to be independent of the TLR-4 locus.
Table 7.
Effects of Hiltonol® on various lung parameters of C57BL/6J mice and TLR-4 -/- mice infected with a lethal dose of mouse-adapted SARS-CoV.
| Treatment | Virus titers (Log10 CCID50/g) ± SD | Visual lung scores ± SD | Lung weights (g) ± SD |
|---|---|---|---|
| Day 3 | |||
| PSS in C57BL/6J mice | 5.06 ± 0.55 | 0.0 ± 0.0 | 0.18 ± 0.00 |
| Hiltonol® (1 mg/kg/) in C57BL/6J mice | 2.06 ± 0.38*** | 0.0 ± 0.0 | 0.22 ± 0.01 |
| PSS in C57BL/6J/10ScNJ TLR-4 -/- mice | 5.00 ± 0.29 | 0.0 ± 0.0 | 0.20 ± 0.02 |
| Hiltonol® (1 mg/kg/) in C57BL/6J/10ScNJ TLR-4 -/- mice | 1.81 ± 0.31*** | 0.0 ± 0.0 | 0.23 ± 0.21 |
| Day 6 | |||
| PSS in C57BL/6J mice | 3.44 ± 0.24 | 0.0 ± 0.0 | 0.17 ± 0.01 |
| Hiltonol® (1 mg/kg/) in C57BL/6J mice | 2.06 ± 0.66*** | 0.0 ± 0.0 | 0.20 ± 0.01 |
| PSS in C57BL/6J/10ScNJ TLR-4 -/- mice | 2.63 ± 0.43 | 0.0 ± 0.0 | 0.17 ± 0.01 |
| Hiltonol® (1 mg/kg/) in C57BL/6J/10ScNJ TLR-4 -/- mice | 1.50 ± 0.00*** | 0.0 ± 0.0 | 0.20 ± 0.01 |
***p < 0.001 versus PSS control.
4. Discussion
The host innate immune response against viral insult includes the production of interferon type I (IFN-α/β), which is initiated to limit viral replication. The virus-infected cells usually cause the activation of several transcription factors, such as interferon regulatory factor 3 (IRF-3), which play a central role in downstream gene activation (Lin et al., 1998). Once interferon is synthesized and secreted from the cells, it binds to cell surface receptors and induces transcription, which results in an anti-viral state in the target cells. Epithelial cells secrete interferon-β as an initial response to viral infection (Marie et al., 1998). Dendritic cells are able to produce INF-α subtypes (Diebold et al., 2003). However, the production of interferon type I by SARS-CoV-infected cells is limited (Chen and Subbarao, 2007, Spiegel et al., 2005) and neither endogenous interferon transcripts nor interferon promoter activity are detected (Spiegel et al., 2005). This lack of interferon activity has been attributed to proteins, which antagonize interferon and block transcription factors necessary for the expression of interferon (Kopecky-Bromberg et al., 2007). Although SARS-CoV antagonizes the production and effect of endogenous interferon, it remains susceptible to exogenous interferons (Chen and Subbarao, 2007, Kumaki et al., 2011a).
Interferon induction occurs mainly by an intracellular pathway: double-stranded (ds) RNA and 5’-triphosphorylated single-stranded (ss) RNA trigger a signaling chain, which activates interferon-β gene expression (Hornung et al., 2006, Pichlmair et al., 2006, Weber et al., 2006). Retinoic-acid-inducible gene I (RIG-I) and melanoma-differentiation-associated gene 5 (MDA-5) are the main intracellular receptors of viral RNA (Andrejeva et al., 2004, Kato et al., 2006, Yoneyama et al., 2004). The binding of a viral RNA to RIG-I and MDA-5 induces a signaling chain which results in the phosphorylation of the transcription factor IRF-3 (Fitzgerald et al., 2003, Sharma et al., 2003). 2′,5’-oligoadenylate synthetases (2′,5′-OAS) (Silverman, 1994) and the protein kinase R (PKR) (Williams, 1999) have also been characterized in detail. 2′,5′-OAS catalyses the synthesis of short 2′-5′ oligoadenylates that activate the latent endoribonuclease (Silverman, 1994). PKR is a serine-threonine kinase that phosphorylates the alpha subunit of the eukaryotic translation initiation factor eIF2 (Williams, 1999). In addition, interferon induction also does occur by an endosomal pathway in selected cells. Myeloid dendritic cells (mDCs) (Diebold et al., 2003) and plasmacytoid dendritic cells (pDCs) (Colonna et al., 2002) are the main interferon producers of the lymphatic system. Myeloid dendritic cells (mDCs) can sence dsRNA by the classic intracellular pathway (Diebold et al., 2003) and, the endosomal toll-like receptor (TLR) (Alexopoulou et al., 2001). TLR-7/8 and TLR-3 recognize viral ssRNA and dsRNA, respectively, and activate interferon-α/β transcription via the transcription factors IRF-7, IRF-3, and NF-κB.
The pathogenesis of severe acute respiratory syndrome has not yet been fully characterized. One hypothesis is that the pathogenesis of SARS-CoV is caused by a disproportionate immune response, illustrated by elevated levels of inflammatory cytokines and chemokines, such as interferon gamma inducible protein 10 (IP-10), monocyte chemoattractant protein-1 (MCP-1), interleukin 6 (IL-6) and interleukin 8 (IL-8) (Jiang et al., 2005, Wong et al., 2004). Chemokines are involved in the recruitment of leukocytes into sites of tissue inflammation (Sauty et al., 1999). SARS-CoV has been shown in vitro to induce changes of cytokines and chemokines in various human and animal cells (Spiegel and Weber, 2006, Yen et al., 2006). IL-6 is a monomor of 184 amino acids secreted by T-cells, macrophages and endothelial cells to stimulate immune response during the infection (Ray et al., 1989, Sehgal et al., 1988, Sehgal et al., 1995). Xiao et al. speculated that dampening of the proinflammatory cytokine response in SARS-CoV infection, in particular the production of IL-6, could have a clinically beneficial effect (Xiao et al., 2008). We noticed that SARS-CoV infection increased IL-6 in mice, and high IL-6 expression corrected with mortality (Day et al., 2009). Levels of IL-6 dropped when BALB/c mice were treated with ribavirin, UDA (5 mg/kg/day), Ampligen® or Hiltonol® (1 mg/kg/day) (Day et al., 2009, Kumaki et al., 2011b). IP-10 and other cytokines are released from both the apical and basolateral sides, while IL-6 is secreted through the apical surface (Yoshikawa et al., 2009). It can be speculated that IP-10 in SARS patients might directly be produced by virus-infected cells, whereas upregulation of IL-6 is likely a secondary response due to the activation of the immune system. In addition, the TRIF pathway leads to the production of type I interferons via interferon regulatory factor 3 (IRF-3) and also cause delayed NF-κB activation via activation of TNF receptor-associated factor 6 (TRAF6) (Hoebe et al., 2003, Sato et al., 2003). Imai et al. also showed that TRIF-dependent lung injury is likely to be mediated by production of interleukin 6 (IL-6), as IL-6-deficient mice were protected from injury (Imai et al., 2008).
Toll-like receptors (TLRs), a family of evolutionarily conserved pathogen recognition receptors, are a class of proteins that play a key role in the innate immune system. The TLR family consists of 13 mammalian members. Viral protein binds to TLR-2 and TLR-4. The single stranded RNA binds to TLR-7 and TLR-8. The double stranded RNA binds to TLR-3 while viral DNA binds to TLR-9. TLR-3, TLR-7, TLR-8, and TLR-9 recognize viral nucleic acids on endosomal membrane. The binding of ligands to TLRs might trigger downstream signaling pathways that are involved in both the cytokine release during the primary induction of inflammation and secondary activation of anti-inflammatory mechanism (Netea et al., 2004). Each TLR has its own intrinsic signaling pathway and induces specific biological responses against microorganisms, such as dendritic cell maturation, cytokine production, and the development of adaptive immunity (Akira et al., 2006, Murawski et al., 2009). TLR-4 recognizes the viral proteins, such as the fusion (F) protein from respiratory syncytial virus and the envelope protein of mouse mammary tumor virus (Uematsu and Akira, 2007). TLR-4-mutated C3H/HeJ mice are sensitive to respiratory syncytial virus infection (Murawski et al., 2009). TLR-4 triggers the induction of proinflammatory cytokines by myeloid differentiation primary response gene 88 (MyD88) pathway, and TLR-4 also interacts with TIR-domain-containing adapter-inducing interferon-β (TRIF)-mediated signaling pathways (Yamamoto et al., 2003) that are involved in interferon induction (Uematsu and Akira, 2007).
The mechanisms of action behind these encouraging results remain to be further elucidated. Hiltonol® (Poly IC:LC, or polyinosinic-polycytidylic acid stabilized with polylysine and carboxymethylcellulose) is a chemically stabilized active double-stranded RNA (dsRNA) therapeutic that activates host innate and adaptive immunity by various pathways/mechanisms leading to induction of the immediate antiviral state. The immediate antiviral state is characterized by induction of a ‘natural mix’ of interferons, cytokines, and chemokines; activation of dsRNA-dependent host defense systems such as RIG-I, MDA-5, 2′,5′-OAS, PKR, stimulation of mDCs, of natural killer (NK) cells and others via toll-like receptors. Toll-like receptors are also implicated in lung airway injury as well as leading to beneficial responses to antigen insult. Imai et al. demonstrated that acute lung injury (ALI) is triggered by the signaling of oxidative stress through Toll-like receptor 4 (Imai et al., 2008). Khanolkar et al. reported that C3H/HeJ mice harboring a natural mutation in the gene that encodes Toll-like receptor 4 (TLR4) that disrupts its normal function exhibited the enhanced morbidity and mortality following i.n. mouse hepatitis virus strain 1 (MHV-1) infection, indicating that TLR-4 plays an important role in respiratory CoV pathogenesis (Khanolkar et al., 2009). In this study, we hypothesized whether intranasal infection of TLR-4 -/- mice with mouse-adapted SARS-CoV would result in an acute respiratory disease with a higher lethality. However, the data presented is not consistent with this hypothesis.
Toll-like receptor (TLR-3) is a member of the Toll-like receptor family of pattern recognition receptors of the innate immune system (Rock et al., 1998). TLR-3 is expressed on respiratory epithelium as well as on mDCs, especially in response to respiratory infections such as influenza. Using TLR-3-deficient mice, Gowen et al. indicate that TLR-3 plays an important role in Punta Toro virus (PTV) infection (Gowen et al., 2006). Ichinohe et al. have also demonstrated an even earlier activation of lung TLR-3 in response to nasal Hiltonol® or poly-IC in mice (Ichinohe et al., 2005). While these host defense mechanisms are typically activated by presentation of ‘foreign’ dsRNA species generated by viral replication, many of them are also frequently the target of inhibition by many neoplasms and viruses, including influenza virus and SARS-CoV. Treatment with mucosally applied Hiltonol® may preempt or reverse some of those viral evasive mechanisms. The apparent modulation by Hiltonol® of the usual relationship between host survival and replication of SARS-CoV, as manifested by clinical protection of animals in spite of some evidence of viral replication, is also of much interest. For example, complete inhibition of viral replication might be counterproductive to the generation of longer term adaptive immunity. Thus, while some of the dsRNA dependent antiviral/antiproliferative pathways mentioned above may help control replication, the potential activation of mDCs via TLR-3 Hiltonol®’s can be seen as improving the efficiency of antigen presentation and may be particularly suited to generation of a Th1 cellular antiviral immunity. In fact, the TLRs have been proposed as a ‘bridge’ between innate and adaptive immunity. It remains to be further determined whether TLR-3 is involved in SARS-CoV infection in mice.
Hiltonol® has been in extensive preclinical and experimental clinical therapeutic use, with evidence of clinical safety and potent antiviral, immune adjuvant, and antineoplastic actions, alone or combined with other agents (Levy et al., 1975). Initial high-dose studies were quasi-empirical and driven by its induction of interferon, yet only recently have its effectiveness at lower doses and broad mechanisms of action begun to be more fully elucidated. There is an extensive early, empirical experience on the broad in vivo antiviral actions of Hiltonol®, yet these actions have not been fully exploited in the context of prophylaxis of emerging infections, pandemic containment and biodefense. Mucosal (intranasal) Hiltonol® provides rapid and complete protection from respiratory viruses such as influenza virus, SARS-CoV, and RSV (Guerrero-Plata et al., 2005, Kumaki et al., 2010, Wong et al., 1995, Wong et al., 1999). Wong et al. has demonstrated 80–100% protection lasting up to 3 weeks provided by intranasal aqueous or liposomal Hiltonol® in otherwise lethal murine challenge models of influenza A and avian (H5N1) influenza viruses. Hiltonol® has been shown to have efficacy against yellow fever (Stephen et al., 1977), simian hemorrhagic fever (Levy et al., 1976), Japanese encephalitis (Harrington et al., 1977), rabies (Baer et al., 1977) and Rift Valley fever (Kende et al., 1987). The antiviral activity of Hiltonol® is believed to be mediated by its ability to augment the production of interferon-α, -β and -γ (Levy et al., 1975). Hiltonol® also activates natural killer cells and macrophages. The antiviral efficacy of Hiltonol® was previously evaluated against avian influenza virus and Hiltonol® appeared to provide effective and broad-spectrum prophylaxis against avian influenza virus (Wong et al., 2007). For our in vivo studies, we recommend to administer the safe dose of Hiltonol® at 2.5 mg/kg/day. In a pilot trial, Salazar et al. reported that low dose Hiltonol® (about 10–50 mcg/kg) was given intramuscularly two to three times weekly for up to 56 months to 38 malignant brain tumor patients (Salazar et al., 1996). Patients tolerated the regimen well, with little or no toxicity and a preserved quality of life. We conclude that the concept of long-term, broad spectrum stimulation of host defenses with non-toxic, inexpensive double-stranded ribonucleic acids, such as Hiltonol® at 50 mcg/kg, might be applicable to the treatment of virus infections.
In the current study, the data suggest that nasal Hiltonol® treatment of SARS-CoV infections in mice leads to a substantial long-term prophylactic and somewhat less robust therapeutic effect that protects mice against death and weight loss resulting from the infection. Host-targeted therapeutics such as Hiltonol® that activate innate immunity and provide immediate broad spectrum resistance could fill the early gap in protection by allowing time for more specific vaccination strategies to take effect, and could thus become an important element of the rapid response to a bioterror attack or pandemic outbreak. Hiltonol® represents a relatively new host-directed paradigm in therapeutics that seeks to activate non-specific and specific host defense systems that have been highly evolved over millions of years. Hiltonol® also has the potential to be used prophylactically in those who have been potentially exposed to the SARS-CoV, but not yet showing symptoms, thus enabling clinicians to “ring” and isolate the focus case with individuals prophylactically treated and unlikely get severe disease or unlikely not get disease at all. The demonstrated clinical safety of Hiltonol®'s, its immediate induction of an innate immune persistent broad spectrum antiviral state, its relatively low cost, its stability in storage and relative ease of use make it a potentially very valuable agent for containment of epidemics caused by respiratory pathogens. Because Hiltonol® has broad spectrum antiviral activity, it also represents a potential therapy for MERS-CoV infection as well, since MERS-CoV is a related coronavirus causing severe respiratory infections as dose SARS-CoV.
Acknowledgments
We thank Aaron J. Smith, Kevin W. Bailey, Michael A. Morrey for kindly providing technical assistance; Craig W. Day for scientific discussion and Ramona T. Skirpstunas for professional consultation. We are grateful to other colleagues for their support. This work was supported by a contract N01-AI-15435 and HHSN272201000039I/HHSN27200002/A14 from the Virology Branch, National Institute of Allergic and Infectious Diseases, National Institutes of Health.
References
- Ahlquist P. RNA-dependent RNA polymerases, viruses, and RNA silencing. Science. 2002;296:1270–1273. doi: 10.1126/science.1069132. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Akira S., Uematsu S., Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Alexopoulou L., Holt A.C., Medzhitov R., Flavell R.A. Recognition of double-stranded RNA and activation of NF-kappaB by Toll-like receptor 3. Nature. 2001;413:732–738. doi: 10.1038/35099560. [DOI] [PubMed] [Google Scholar]
- Anand K., Ziebuhr J., Wadhwani P., Mesters J.R., Hilgenfeld R. Coronavirus main proteinase (3CLpro) structure: basis for design of anti-SARS drugs. Science. 2003;300:1763–1767. doi: 10.1126/science.1085658. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Andrejeva J., Childs K.S., Young D.F., Carlos T.S., Stock N., Goodbourn S., Randall R.E. The V proteins of paramyxoviruses bind the IFN-inducible RNA helicase, mda-5, and inhibit its activation of the IFN-beta promoter. Proc. Natl. Acad. Sci. U. S. A. 2004;101:17264–17269. doi: 10.1073/pnas.0407639101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer G.M., Shaddock J.H., Moore S.A., Yager P.A., Baron S.S., Levy H.B. Successful prophylaxis against rabies in mice and Rhesus monkeys: the interferon system and vaccine. J. Infect. Dis. 1977;136:286–291. doi: 10.1093/infdis/136.2.286. [DOI] [PubMed] [Google Scholar]
- Barnard D.L., Day C.W., Bailey K., Heiner M., Montgomery R., Lauridsen L., Chan P.K., Sidwell R.W. Evaluation of immunomodulators, interferons and known in vitro SARS-coV inhibitors for inhibition of SARS-coV replication in BALB/c mice. Antivir. Chem. Chemother. 2006;17:275–284. doi: 10.1177/095632020601700505. [DOI] [PubMed] [Google Scholar]
- Barnard D.L., Day C.W., Bailey K., Heiner M., Montgomery R., Lauridsen L., Winslow S., Hoopes J., Li J.K., Lee J., Carson D.A., Cottam H.B., Sidwell R.W. Enhancement of the infectivity of SARS-CoV in BALB/c mice by IMP dehydrogenase inhibitors, including ribavirin. Antivir. Res. 2006;71:53–63. doi: 10.1016/j.antiviral.2006.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard D.L., Kumaki Y. Development in the search for the small-molecule inhibitors for treatment of severe acute respiratory syndrome coronavirus. In: LaFemina R.L., editor. Antiviral Research: Strategies in Antiviral Drug Discovery. 2009. pp. 209–222. [Google Scholar]
- Booth C.M., Matukas L.M., Tomlinson G.A., Rachlis A.R., Rose D.B., Dwosh H.A., Walmsley S.L., Mazzulli T., Avendano M., Derkach P., Ephtimios I.E., Kitai I., Mederski B.D., Shadowitz S.B., Gold W.L., Hawryluck L.A., Rea E., Chenkin J.S., Cescon D.W., Poutanen S.M., Detsky A.S. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. Jama. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- Bosch B.J., Martina B.E., Van Der Zee R., Lepault J., Haijema B.J., Versluis C., Heck A.J., De Groot R., Osterhaus A.D., Rottier P.J. Severe acute respiratory syndrome coronavirus (SARS-CoV) infection inhibition using spike protein heptad repeat-derived peptides. Proc. Natl. Acad. Sci. U. S. A. 2004;101:8455–8460. doi: 10.1073/pnas.0400576101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Z., Babiuk L.A., Hu J. Therapeutic and prophylactic potential of small interfering RNAs against severe acute respiratory syndrome: progress to date. BioDrugs. 2007;21:9–15. doi: 10.2165/00063030-200721010-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Subbarao K. The immunobiology of SARS*. Annu. Rev. Immunol. 2007;25:443–472. doi: 10.1146/annurev.immunol.25.022106.141706. [DOI] [PubMed] [Google Scholar]
- Cinatl J., Morgenstern B., Bauer G., Chandra P., Rabenau H., Doerr H.W. Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet. 2003;361:2045–2046. doi: 10.1016/S0140-6736(03)13615-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colonna M., Krug A., Cella M. Interferon-producing cells: on the front line in immune responses against pathogens. Curr. Opin. Immunol. 2002;14:373–379. doi: 10.1016/s0952-7915(02)00349-7. [DOI] [PubMed] [Google Scholar]
- Day C.W., Baric R., Cai S.X., Frieman M., Kumaki Y., Morrey J.D., Smee D.F., Barnard D.L. A new mouse-adapted strain of SARS-CoV as a lethal model for evaluating antiviral agents in vitro and in vivo. Virology. 2009;395:210–222. doi: 10.1016/j.virol.2009.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diebold S.S., Montoya M., Unger H., Alexopoulou L., Roy P., Haswell L.E., Al-Shamkhani A., Flavell R., Borrow P., Reis e Sousa C. Viral infection switches non-plasmacytoid dendritic cells into high interferon producers. Nature. 2003;424:324–328. doi: 10.1038/nature01783. [DOI] [PubMed] [Google Scholar]
- Drosten C., Gunther S., Preiser W., van der Werf S., Brodt H.R., Becker S., Rabenau H., Panning M., Kolesnikova L., Fouchier R.A., Berger A., Burguiere A.M., Cinatl J., Eickmann M., Escriou N., Grywna K., Kramme S., Manuguerra J.C., Muller S., Rickerts V., Sturmer M., Vieth S., Klenk H.D., Osterhaus A.D., Schmitz H., Doerr H.W. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Fitzgerald K.A., McWhirter S.M., Faia K.L., Rowe D.C., Latz E., Golenbock D.T., Coyle A.J., Liao S.M., Maniatis T. IKKepsilon and TBK1 are essential components of the IRF3 signaling pathway. Nat. Immunol. 2003;4:491–496. doi: 10.1038/ni921. [DOI] [PubMed] [Google Scholar]
- Gibson I. Antisense DNA and RNA strategies: new approaches to therapy. J. R. Coll. Phys. Lond. 1994;28:507–511. [PMC free article] [PubMed] [Google Scholar]
- Gowen B.B., Hoopes J.D., Wong M.H., Jung K.H., Isakson K.C., Alexopoulou L., Flavell R.A., Sidwell R.W. TLR3 deletion limits mortality and disease severity due to Phlebovirus infection. J. Immunol. 2006;177:6301–6307. doi: 10.4049/jimmunol.177.9.6301. [DOI] [PubMed] [Google Scholar]
- Groneberg D.A., Fischer A., Chung K.F., Daniel H. Molecular mechanisms of pulmonary peptidomimetic drug and peptide transport. Am. J. Respir. Cell Mol. Biol. 2004;30:251–260. doi: 10.1165/rcmb.2003-0315TR. [DOI] [PubMed] [Google Scholar]
- Groneberg D.A., Witt C., Wagner U., Chung K.F., Fischer A. Fundamentals of pulmonary drug delivery. Respir. Med. 2003;97:382–387. doi: 10.1053/rmed.2002.1457. [DOI] [PubMed] [Google Scholar]
- Guerrero-Plata A., Baron S., Poast J.S., Adegboyega P.A., Casola A., Garofalo R.P. Activity and regulation of alpha interferon in respiratory syncytial virus and human metapneumovirus experimental infections. J. Virol. 2005;79:10190–10199. doi: 10.1128/JVI.79.16.10190-10199.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington D.G., Hilmas D.E., Elwell M.R., Whitmire R.E., Stephen E.L. Intranasal infection of monkeys with Japanese encephalitis virus: clinical response and treatment with a nuclease-resistant derivative of poly (I).poly (C) Am. J. Trop. Med. Hyg. 1977;26:1191–1198. doi: 10.4269/ajtmh.1977.26.1191. [DOI] [PubMed] [Google Scholar]
- Hirano T. Interleukin 6 and its receptor: ten years later. Int. Rev. Immunol. 1998;16:249–284. doi: 10.3109/08830189809042997. [DOI] [PubMed] [Google Scholar]
- Ho J.C., Ooi G.C., Mok T.Y., Chan J.W., Hung I., Lam B., Wong P.C., Li P.C., Ho P.L., Lam W.K., Ng C.K., Ip M.S., Lai K.N., Chan-Yeung M., Tsang K.W. High-dose pulse versus nonpulse corticosteroid regimens in severe acute respiratory syndrome. Am. J. Respir. Crit. Care Med. 2003;168:1449–1456. doi: 10.1164/rccm.200306-766OC. [DOI] [PubMed] [Google Scholar]
- Ho T.Y., Wu S.L., Chen J.C., Wei Y.C., Cheng S.E., Chang Y.H., Liu H.J., Hsiang C.Y. Design and biological activities of novel inhibitory peptides for SARS-CoV spike protein and angiotensin-converting enzyme 2 interaction. Antivir. Res. 2006;69:70–76. doi: 10.1016/j.antiviral.2005.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoebe K., Du X., Georgel P., Janssen E., Tabeta K., Kim S.O., Goode J., Lin P., Mann N., Mudd S., Crozat K., Sovath S., Han J., Beutler B. Identification of Lps2 as a key transducer of MyD88-independent TIR signalling. Nature. 2003;424:743–748. doi: 10.1038/nature01889. [DOI] [PubMed] [Google Scholar]
- Hornung V., Ellegast J., Kim S., Brzozka K., Jung A., Kato H., Poeck H., Akira S., Conzelmann K.K., Schlee M., Endres S., Hartmann G. 5'-Triphosphate RNA is the ligand for RIG-I. Science. 2006;314:994–997. doi: 10.1126/science.1132505. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Ichinohe T., Watanabe I., Ito S., Fujii H., Moriyama M., Tamura S., Takahashi H., Sawa H., Chiba J., Kurata T., Sata T., Hasegawa H. Synthetic double-stranded RNA poly(I: C) combined with mucosal vaccine protects against influenza virus infection. J. Virol. 2005;79:2910–2919. doi: 10.1128/JVI.79.5.2910-2919.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y., Kuba K., Neely G.G., Yaghubian-Malhami R., Perkmann T., van Loo G., Ermolaeva M., Veldhuizen R., Leung Y.H., Wang H., Liu H., Sun Y., Pasparakis M., Kopf M., Mech C., Bavari S., Peiris J.S., Slutsky A.S., Akira S., Hultqvist M., Holmdahl R., Nicholls J., Jiang C., Binder C.J., Penninger J.M. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133:235–249. doi: 10.1016/j.cell.2008.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs A., Lindenmann J. Virus interference. I. The interferon. Proc. R. Soc. Lond. B Biol. Sci. 1957;147:258–267. [PubMed] [Google Scholar]
- Isaacs A., Lindenmann J., Valentine R.C. Virus interference. II. Some properties of interferon. Proc. R. Soc. Lond. B Biol. Sci. 1957;147:268–273. [Google Scholar]
- Jiang Y., Xu J., Zhou C., Wu Z., Zhong S., Liu J., Luo W., Chen T., Qin Q., Deng P. Characterization of cytokine/chemokine profiles of severe acute respiratory syndrome. Am. J. Respir. Crit. Care Med. 2005;171:850–857. doi: 10.1164/rccm.200407-857OC. [DOI] [PubMed] [Google Scholar]
- Johnson-Saliba M., Jans D.A. Gene therapy: optimising DNA delivery to the nucleus. Curr. Drug Targets. 2001;2:371–399. doi: 10.2174/1389450013348245. [DOI] [PubMed] [Google Scholar]
- Kato H., Takeuchi O., Sato S., Yoneyama M., Yamamoto M., Matsui K., Uematsu S., Jung A., Kawai T., Ishii K.J., Yamaguchi O., Otsu K., Tsujimura T., Koh C.S., Reis e Sousa C., Matsuura Y., Fujita T., Akira S. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature. 2006;441:101–105. doi: 10.1038/nature04734. [DOI] [PubMed] [Google Scholar]
- Kende M., Lupton H.W., Rill W.L., Levy H.B., Canonico P.G. Enhanced therapeutic efficacy of poly(ICLC) and ribavirin combinations against Rift Valley fever virus infection in mice. Antimicrob. agents Chemother. 1987;31:986–990. doi: 10.1128/aac.31.7.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanolkar A., Hartwig S.M., Haag B.A., Meyerholz D.K., Harty J.T., Varga S.M. Toll-like receptor 4 deficiency increases disease and mortality after mouse hepatitis virus type 1 infection of susceptible C3H mice. J. Virol. 2009;83:8946–8956. doi: 10.1128/JVI.01857-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopecky-Bromberg S.A., Martinez-Sobrido L., Frieman M., Baric R.A., Palese P. Severe acute respiratory syndrome coronavirus open reading frame (ORF) 3b, ORF 6, and nucleocapsid proteins function as interferon antagonists. J. Virol. 2007;81:548–557. doi: 10.1128/JVI.01782-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S., Tong S., Urbani C., Comer J.A., Lim W., Rollin P.E., Dowell S.F., Ling A.E., Humphrey C.D., Shieh W.J., Guarner J., Paddock C.D., Rota P., Fields B., DeRisi J., Yang J.Y., Cox N., Hughes J.M., LeDuc J.W., Bellini W.J., Anderson L.J. A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- Kumaki Y., Day C.W., Bailey K.W., Wandersee M.K., Wong M.H., Madsen J.R., Madsen J.S., Nelson N.M., Hoopes J.D., Woolcott J.D., McLean T.Z., Blatt L.M., Salazar A.M., Smee D.F., Barnard D.L. Induction of interferon-gamma-inducible protein 10 by SARS-CoV infection, interferon alfacon 1 and interferon inducer in human bronchial epithelial Calu-3 cells and BALB/c mice. Antivir. Chem. Chemother. 2010;20:169–177. doi: 10.3851/IMP1477. [DOI] [PubMed] [Google Scholar]
- Kumaki Y., Ennis J., Rahbar R., Turner J.D., Wandersee M.K., Smith A.J., Bailey K.W., Vest Z.G., Madsen J.R., Li J.K., Barnard D.L. Single-dose intranasal administration with mDEF201 (adenovirus vectored mouse interferon-alpha) confers protection from mortality in a lethal SARS-CoV BALB/c mouse model. Antivir. Res. 2011;89:75–82. doi: 10.1016/j.antiviral.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumaki Y., Wandersee M.K., Smith A.J., Zhou Y., Simmons G., Nelson N.M., Bailey K.W., Vest Z.G., Li J.K., Chan P.K., Smee D.F., Barnard D.L. Inhibition of severe acute respiratory syndrome coronavirus replication in a lethal SARS-CoV BALB/c mouse model by stinging nettle lectin, Urtica dioica agglutinin. Antivir. Res. 2011;90:22–32. doi: 10.1016/j.antiviral.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard J.N., Schaffer D.V. Antiviral RNAi therapy: emerging approaches for hitting a moving target. Gene Ther. 2006;13:532–540. doi: 10.1038/sj.gt.3302645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy H.B., Baer G., Baron S., Buckler C.E., Gibbs C.J., Iadarola M.J., London W.T., Rice J. A modified polyriboinosinic-polyribocytidylic acid complex that induces interferon in primates. J. Infect. Dis. 1975;132:434–439. doi: 10.1093/infdis/132.4.434. [DOI] [PubMed] [Google Scholar]
- Levy H.B., London W., Fuccillo D.A., Baron S., Rice J. Prophylactic control of simian hemorrhagic fever in monkeys by an interferon inducer, polyriboinosinic-polyribocytidylic acid-poly-L-lysine. J. Infect. Dis. 1976;133(Suppl):A256–A259. doi: 10.1093/infdis/133.supplement_2.a256. [DOI] [PubMed] [Google Scholar]
- Lin R., Heylbroeck C., Pitha P.M., Hiscott J. Virus-dependent phosphorylation of the IRF-3 transcription factor regulates nuclear translocation, transactivation potential, and proteasome-mediated degradation. Mol. Cell Biol. 1998;18:2986–2996. doi: 10.1128/mcb.18.5.2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marie I., Durbin J.E., Levy D.E. Differential viral induction of distinct interferon-alpha genes by positive feedback through interferon regulatory factor-7. Embo J. 1998;17:6660–6669. doi: 10.1093/emboj/17.22.6660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murawski M.R., Bowen G.N., Cerny A.M., Anderson L.J., Haynes L.M., Tripp R.A., Kurt-Jones E.A., Finberg R.W. Respiratory syncytial virus activates innate immunity through Toll-like receptor 2. J. Virol. 2009;83:1492–1500. doi: 10.1128/JVI.00671-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netea M.G., van der Graaf C., Van der Meer J.W., Kullberg B.J. Toll-like receptors and the host defense against microbial pathogens: bringing specificity to the innate-immune system. J. Leukoc. Biol. 2004;75:749–755. doi: 10.1189/jlb.1103543. [DOI] [PubMed] [Google Scholar]
- Peiris J.S., Chu C.M., Cheng V.C., Chan K.S., Hung I.F., Poon L.L., Law K.I., Tang B.S., Hon T.Y., Chan C.S., Chan K.H., Ng J.S., Zheng B.J., Ng W.L., Lai R.W., Guan Y., Yuen K.Y. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris J.S., Lai S.T., Poon L.L., Guan Y., Yam L.Y., Lim W., Nicholls J., Yee W.K., Yan W.W., Cheung M.T., Cheng V.C., Chan K.H., Tsang D.N., Yung R.W., Ng T.K., Yuen K.Y. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pichlmair A., Schulz O., Tan C.P., Naslund T.I., Liljestrom P., Weber F., Reis e Sousa C. RIG-I-mediated antiviral responses to single-stranded RNA bearing 5'-phosphates. Science. 2006;314:997–1001. doi: 10.1126/science.1132998. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Ray A., Tatter S.B., Santhanam U., Helfgott D.C., May L.T., Sehgal P.B. Regulation of expression of interleukin-6. Molecular and clinical studies. Ann. N. Y. Acad. Sci. 1989;557:353–361. discussion 361–352. [PubMed] [Google Scholar]
- Reed L.J., Muench N. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 1938;27:493–497. [Google Scholar]
- Rock F.L., Hardiman G., Timans J.C., Kastelein R.A., Bazan J.F. A family of human receptors structurally related to Drosophila Toll. Proc. Natl. Acad. Sci. U. S. A. 1998;95:588–593. doi: 10.1073/pnas.95.2.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rota P.A., Oberste M.S., Monroe S.S., Nix W.A., Campagnoli R., Icenogle J.P., Penaranda S., Bankamp B., Maher K., Chen M.H., Tong S., Tamin A., Lowe L., Frace M., DeRisi J.L., Chen Q., Wang D., Erdman D.D., Peret T.C., Burns C., Ksiazek T.G., Rollin P.E., Sanchez A., Liffick S., Holloway B., Limor J., McCaustland K., Olsen-Rasmussen M., Fouchier R., Gunther S., Osterhaus A.D., Drosten C., Pallansch M.A., Anderson L.J., Bellini W.J. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Salazar A.M., Levy H.B., Ondra S., Kende M., Scherokman B., Brown D., Mena H., Martin N., Schwab K., Donovan D., Dougherty D., Pulliam M., Ippolito M., Graves M., Brown H., Ommaya A. Long-term treatment of malignant gliomas with intramuscularly administered polyinosinic-polycytidylic acid stabilized with polylysine and carboxymethylcellulose: an open pilot study. Neurosurgery. 1996;38:1096–1103. discussion 1103–1094. [PubMed] [Google Scholar]
- Sato S., Sugiyama M., Yamamoto M., Watanabe Y., Kawai T., Takeda K., Akira S. Toll/IL-1 receptor domain-containing adaptor inducing IFN-beta (TRIF) associates with TNF receptor-associated factor 6 and TANK-binding kinase 1, and activates two distinct transcription factors, NF-kappa B and IFN-regulatory factor-3, in the Toll-like receptor signaling. J. Immunol. 2003;171:4304–4310. doi: 10.4049/jimmunol.171.8.4304. [DOI] [PubMed] [Google Scholar]
- Sauty A., Dziejman M., Taha R.A., Iarossi A.S., Neote K., Garcia-Zepeda E.A., Hamid Q., Luster A.D. The T cell-specific CXC chemokines IP-10, Mig, and I-TAC are expressed by activated human bronchial epithelial cells. J. Immunol. 1999;162:3549–3558. [PubMed] [Google Scholar]
- Sehgal P.B., Helfgott D.C., Santhanam U., Tatter S.B., Clarick R.H., Ghrayeb J., May L.T. Regulation of the acute phase and immune responses in viral disease. Enhanced expression of the beta 2-interferon/hepatocyte-stimulating factor/interleukin 6 gene in virus-infected human fibroblasts. J. Exp. Med. 1988;167:1951–1956. doi: 10.1084/jem.167.6.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sehgal P.B., Wang L., Rayanade R., Pan H., Margulies L. Interleukin-6-type cytokines. Ann. N. Y. Acad. Sci. 1995;762:1–14. [PubMed] [Google Scholar]
- Sharma S., tenOever B.R., Grandvaux N., Zhou G.P., Lin R., Hiscott J. Triggering the interferon antiviral response through an IKK-related pathway. Science. 2003;300:1148–1151. doi: 10.1126/science.1081315. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Sidwell R.W., Bailey K.W., Wong M.H., Huffman J.H. In vitro and in vivo sensitivity of a non-mouse-adapted influenza A (Beijing) virus infection to amantadine and ribavirin. Chemotherapy. 1995;41:455–461. doi: 10.1159/000239382. [DOI] [PubMed] [Google Scholar]
- Silverman R.H. Fascination with 2-5A-dependent RNase: a unique enzyme that functions in interferon action. J. Interferon Res. 1994;14:101–104. doi: 10.1089/jir.1994.14.101. [DOI] [PubMed] [Google Scholar]
- Spiegel M., Pichlmair A., Martinez-Sobrido L., Cros J., Garcia-Sastre A., Haller O., Weber F. Inhibition of Beta interferon induction by severe acute respiratory syndrome coronavirus suggests a two-step model for activation of interferon regulatory factor 3. J. Virol. 2005;79:2079–2086. doi: 10.1128/JVI.79.4.2079-2086.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel M., Weber F. Inhibition of cytokine gene expression and induction of chemokine genes in non-lymphatic cells infected with SARS coronavirus. Virol. J. 2006;3:17. doi: 10.1186/1743-422X-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephen E.L., Sammons M.L., Pannier W.L., Baron S., Spertzel R.O., Levy H.B. Effect of a nuclease-resistant derivative of polyriboinosinic-polyribocytidylic acid complex on yellow fever in rhesus monkeys (Macaca mulatta) J. Infect. Dis. 1977;136:122–126. doi: 10.1093/infdis/136.1.122. [DOI] [PubMed] [Google Scholar]
- Sui J., Li W., Murakami A., Tamin A., Matthews L.J., Wong S.K., Moore M.J., Tallarico A.S., Olurinde M., Choe H., Anderson L.J., Bellini W.J., Farzan M., Marasco W.A. Potent neutralization of severe acute respiratory syndrome (SARS) coronavirus by a human mAb to S1 protein that blocks receptor association. Proc. Natl. Acad. Sci. U. S. A. 2004;101:2536–2541. doi: 10.1073/pnas.0307140101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang K., Seto W.H. Severe acute respiratory syndrome: scientific and anecdotal evidence for drug treatment. Curr. Opin. Investig. Drugs. 2004;5:179–185. [PubMed] [Google Scholar]
- Tsang K.W., Ho P.L., Ooi G.C., Yee W.K., Wang T., Chan-Yeung M., Lam W.K., Seto W.H., Yam L.Y., Cheung T.M., Wong P.C., Lam B., Ip M.S., Chan J., Yuen K.Y., Lai K.N. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N. Engl. J. Med. 2003;348:1977–1985. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- Tsui P.T., Kwok M.L., Yuen H., Lai S.T. Severe acute respiratory syndrome: clinical outcome and prognostic correlates. Emerg. Infect. Dis. 2003;9:1064–1069. doi: 10.3201/eid0909.030362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uematsu S., Akira S. Toll-like receptors and Type I interferons. J. Biol. Chem. 2007;282:15319–15323. doi: 10.1074/jbc.R700009200. [DOI] [PubMed] [Google Scholar]
- Weber F., Wagner V., Rasmussen S.B., Hartmann R., Paludan S.R. Double-stranded RNA is produced by positive-strand RNA viruses and DNA viruses but not in detectable amounts by negative-strand RNA viruses. J. Virol. 2006;80:5059–5064. doi: 10.1128/JVI.80.10.5059-5064.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams B.R. PKR; a sentinel kinase for cellular stress. Oncogene. 1999;18:6112–6120. doi: 10.1038/sj.onc.1203127. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Lam C.W., Wu A.K., Ip W.K., Lee N.L., Chan I.H., Lit L.C., Hui D.S., Chan M.H., Chung S.S., Sung J.J. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin. Exp. Immunol. 2004;136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J.P., Christopher M.E., Salazar A.M., Dale R.M., Sun L.Q., Wang M. Nucleic acid-based antiviral drugs against seasonal and avian influenza viruses. Vaccine. 2007;25:3175–3178. doi: 10.1016/j.vaccine.2007.01.051. [DOI] [PubMed] [Google Scholar]
- Wong J.P., Saravolac E.G., Sabuda D., Levy H.B., Kende M. Prophylactic and therapeutic efficacies of poly(IC.LC) against respiratory influenza A virus infection in mice. Antimicrob. Agents Chemother. 1995;39:2574–2576. doi: 10.1128/aac.39.11.2574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J.P., Yang H., Nagata L., Kende M., Levy H., Schnell G., Blasetti K. Liposome-mediated immunotherapy against respiratory influenza virus infection using double-stranded RNA poly ICLC. Vaccine. 1999;17:1788–1795. doi: 10.1016/s0264-410x(98)00439-3. [DOI] [PubMed] [Google Scholar]
- Xiao H., Xu L.H., Yamada Y., Liu D.X. Coronavirus spike protein inhibits host cell translation by interaction with eIF3f. PLoS One. 2008;3:e1494. doi: 10.1371/journal.pone.0001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto M., Sato S., Hemmi H., Hoshino K., Kaisho T., Sanjo H., Takeuchi O., Sugiyama M., Okabe M., Takeda K., Akira S. Role of adaptor TRIF in the MyD88-independent toll-like receptor signaling pathway. Science. 2003;301:640–643. doi: 10.1126/science.1087262. (New York, N.Y.) [DOI] [PubMed] [Google Scholar]
- Yang H., Yang M., Ding Y., Liu Y., Lou Z., Zhou Z., Sun L., Mo L., Ye S., Pang H., Gao G.F., Anand K., Bartlam M., Hilgenfeld R., Rao Z. The crystal structures of severe acute respiratory syndrome virus main protease and its complex with an inhibitor. Proc. Natl. Acad. Sci. U. S. A. 2003;100:13190–13195. doi: 10.1073/pnas.1835675100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen Y.T., Liao F., Hsiao C.H., Kao C.L., Chen Y.C., Wu-Hsieh B.A. Modeling the early events of severe acute respiratory syndrome coronavirus infection in vitro. J. Virol. 2006;80:2684–2693. doi: 10.1128/JVI.80.6.2684-2693.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoneyama M., Kikuchi M., Natsukawa T., Shinobu N., Imaizumi T., Miyagishi M., Taira K., Akira S., Fujita T. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat. Immunol. 2004;5:730–737. doi: 10.1038/ni1087. [DOI] [PubMed] [Google Scholar]
- Yoshikawa T., Hill T., Li K., Peters C.J., Tseng C.T. Severe acute respiratory syndrome (SARS) coronavirus-induced lung epithelial cytokines exacerbate SARS pathogenesis by modulating intrinsic functions of monocyte-derived macrophages and dendritic cells. J. Virol. 2009;83:3039–3048. doi: 10.1128/JVI.01792-08. [DOI] [PMC free article] [PubMed] [Google Scholar]