Abstract
Background:
Sustaining interest and promoting deep learning is a challenge in any teaching method. The purpose of the study is to find the perception of trainee doctors in Internal Medicine and teaching faculty on the usefulness of case-based learning (CBL) and to compare assessment knowledge outcome with didactic seminars.
Methods and Materials:
We developed and conducted a CBL teaching program on eight topics in infectious diseases. First group had CBL and second group had didactic seminars. In step 1, a clinical case was introduced in stages. Learning objectives were formulated and topics were divided among the trainees. At step 2, trainees shared what they had learnt from self-directed learning. Faculty summarized the case and learning points. In the seminar group, trainees made presentations on the given topics. Trainees who had CBL underwent a questionnaire survey. Multiple choice questions-based test was administered for both the groups.
Results:
The trainee doctors and staff overwhelmingly found CBL to be more interesting, stimulating, and useful compared to didactic seminars. There was no statistical difference in the test scores.
Conclusions:
CBL is a useful and interesting method of learning and should be employed more often in teaching for trainee doctors.
Keywords: Case-based learning, case-based teaching, medical education
Introduction
Case-based learning (CBL) is a student centerd pedagogical method where learning occurs around a case presented by the teacher in stages and the students solve the problem, understand their knowledge gaps, and then work to fill those gaps. While conventional teaching methods are centerd on a topic and cases are used as illustrations, in CBL, the case itself becomes the center around which suitable and contextual learning occurs. A useful definition for CBL is provided by Thistlethwaite et al.: The goal of CBL is to prepare students for clinical practice, through the use of authentic clinical cases. It links theory to practice, through the application of knowledge to the cases, using inquiry-based learning methods.[1]
CBL is used as a teaching method in various health disciplines. It has been used for undergraduate medical students at clinical and preclinical levels. In a study from India, CBL was employed in teaching pharmacotherapy for undergraduate medical students and the investigators found that the students scored higher in knowledge than the group which had the traditional teaching methods.[2] In a study done in dental students doing internship, CBL was found to improve medical record writing, case analysis, and the ability of winning the trust of the patients during their clinical internship.[3] Hansen et al. compared CBL with traditional lectures in an obstetrics and gynecology clerkship program for undergraduate students. They found that students favored CBL over traditional lectures and reported that CBL helped them understand the relationship between knowledge and clinical practice.[4] The motivation of students to learn also seems to be high in CBL.[5] Nair et al. used CBL for teaching biochemistry for preclinical year medical students and reported that most students found it an interesting way of learning and that it helped them in logical application of knowledge to the cases.[6] However, in our knowledge, CBL has not been studied in Internal Medicine trainee doctors.
We did this study to find the perception of students and faculty on the usefulness of CBL and to compare assessment outcomes in trainees after CBL and after didactic seminars.
Methods
Study design and setting
Our study was conducted in the Department of Medicine at a tertiary teaching hospital in South India with undergraduate and postgraduate students across a variety of health disciplines. The Department of Internal Medicine has 5 units and runs a 3-year residency program in internal medicine apart from training for undergraduate medical students. The trainee doctors in any unit consist of the undergraduate students in their internship or foundation year training and the postgraduate residents doing General Medicine.
After discussion within the unit, we developed a CBL teaching program on infectious diseases for the trainee doctors. A total of 8 topics were chosen. The study was conducted over a 4-month period. In the first 2 months, the trainee doctors had case-based learning. In the next 2 months, the trainee doctors had didactic seminars. There were 16 trainees each in the CBL group and the seminar group.
In case-based learning, a list of learning objectives was written down for each topic. The CBL was facilitated by one of the faculty members. Each topic was covered in two steps. In step 1, a clinical case was introduced in a stepwise manner and the students were asked to discuss possible differential diagnoses, diagnostic approach, and treatment plans. The final diagnosis and outcome of the patient were also revealed in the end. A list of learning objectives was formulated at the end of step 2 and the topics were divided between the students to make presentations during step 2. At step 2, the topics were presented and discussed by the students. The faculty helped in summarizing the case and the learning points from both sessions. [Figure 1].
Figure 1.
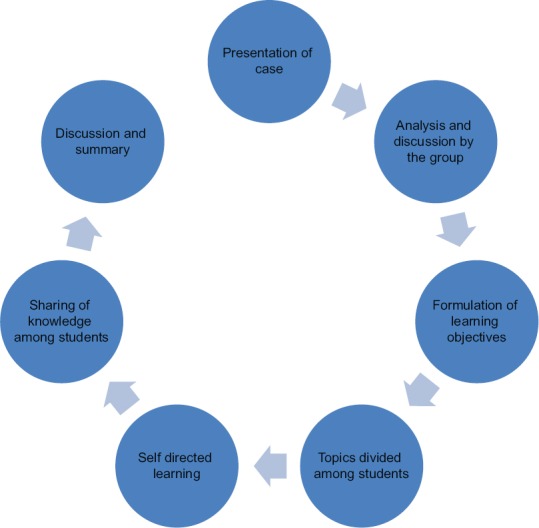
Steps involved in case-based learning
In the seminar group, the students were given the topics and the learning objectives and were asked to prepare presentations and present them to the rest of the group. There were no cases discussed before or after the seminar. The topics included for the sessions were dengue infection, influenza, malaria, severe Gram-negative bacterial infections, management of HIV infection, infections due to Staphylococcus aureus, multi-drug resistant tuberculosis, and histoplasmosis.
Approval by institutional review and ethics board
The study was approved by the institutional review board and ethics committee. (IRB: 10807 (INTERVE) dated: 23.08.2017).
CBL survey
Perception regarding CBL in students and faculty in the unit was assessed using a questionnaire. The questionnaire had 10 statements and the responders were asked to grade their responses on a five-point Likert scale. Options were strongly agree (rated 5), agree (4), neutral (3), disagree (2), and strongly disagree (1). The questionnaire assessed the following aspects of CBL: How the students perceived CBL, ability of CBL to foster learning, critical thinking, approach to patients, identification of knowledge gaps when compared to traditional lectures and student-led seminars, role of the facilitator, usefulness of discussion, and the mode of assessment. A final overall impression was also asked. Free text responses on the major strengths of the teaching program and ways to improve the program were also asked.
Student assessment
Students were assessed using a multiple choice-based test at the end of the teaching period in each group. There were 4 questions in each test and questions were framed in such a way to assess the learning outcomes. The same questions were administered for the groups and the second group did not have access to the questions prior hand. The baseline knowledge was assumed to be equal in both groups.
Statistical analysis
We compared the mean results of the test scores of both the groups using T-test. An alpha level of 0.05 was considered significant. Mean and standard deviation was calculated for the responses to the closed questions of the survey. The free text response to the open question was analyzed using conventional content analysis. Words, phrases, and sentences expressing the same line of thought were grouped into one theme and were the unit of analysis. One of the researchers worked with the biostatistician to decide on grouping the responses into mutually agreeable themes.
Results
CBL survey
All 16 (100%) students in the CBL group completed the questionnaire regarding CBL. Table 1 shows the responses given by the students on the various statements regarding the CBL program. The CBL program was perceived to be useful on all accounts. All 16 (100%) students completed free-text responses. 11 students commented on the benefits of CBL compared with traditional lectures and seminars. Feedback was also collected from six of the faculty members who were present during both the CBL sessions and the seminars.
Table 1.
CBL survey (1=strongly disagree to 5=strongly agree)
| Statements | Students | Faculty | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Students enjoyed CBL more than seminars or lectures | 4.68 | 0.58 | 3.83 | 0.41 |
| CBL helped students to learn about the topic better than a seminar | 4.43 | 0.62 | 4.00 | 0.89 |
| CBL develops critical thinking | 4.31 | 0.47 | 4.16 | 0.40 |
| CBL will help students approach cases better than seminars | 4.86 | 0.36 | 4.00 | 0.00 |
| CBL motivates students to read more than seminars | 4.30 | 0.61 | 3.33 | 0.51 |
| CBL helps students identify areas where they lack knowledge | 4.50 | 0.51 | 3.60 | 0.51 |
| Role of facilitator in CBL is useful | 4.43 | 0.63 | 3.50 | 0.55 |
| CBL should be used frequently in training | 4.37 | 0.80 | 4.00 | 0.63 |
| Discussion with peers is useful | 4.43 | 0.62 | 4.33 | 0.81 |
| MCQ test is a good way of assessing the impact of CBL | 3.50 | 1.03 | 3.50 | 0.55 |
| Overall, CBL was a very useful learning experience | 4.69 | 0.48 | 4.50 | 0.55 |
As part of the survey, we asked one open-ended question which was “What do you think are the major strengths of CBL?” We categorized the answers into four categories and are presented in Table 2.
Table 2.
Strengths of CBL as perceived by students and faculty
| Themes | Responses |
|---|---|
| CBL helps the students acquire practical knowledge | Helps to think practically |
| Develops a holistic approach to patients | |
| In CBL, learning is contextualized | |
| CBL encourages individual involvement | Promotes individual participation in learning, teaching, and presentation |
| Helps in figuring out the lack of knowledge ourselves | |
| A good platform for asking questions and clarifying doubts | |
| Self-directed and self-motivated learning occurs in CBL | |
| CBL promotes critical thinking | Makes you think about aspects of a case that you may not normally think about |
| Encourages us to apply our knowledge to come to a conclusion rather than by rote | |
| Helps approaching the patient from various angles | |
| Questions asked by everyone helps in thinking differently | |
| CBL is more enjoyable | More enjoyable and interactive than lectures and seminars and promotes attention |
| Builds team spirit |
MCQ test
The mean score obtained by the trainees in CBL group was 50.3% (SD 12.3%) and the seminar group was 53.25% (SD 12.3%). The difference between the two groups was not statistically significant (P value = 0.24).
Discussion
Seminars and lectures continue to dominate medical education in various parts of the world even though there is a systematic effort worldwide to incorporate learner-centric teaching methods. The problem with didactic teaching is that it does not promote deep learning. There is a good body of medical literature showing that deep and strategic, but not surface learning, is what predicts successful outcomes in the final year of medical studies[7] and that practicing physicians have higher deep learning scores than students.[8] The recent years also have seen a gradual, worldwide shift in the style of medical education toward small group teaching which promotes deep and strategic learning.
Our study is the first to study the effect of CBL in trainee doctors in Internal Medicine and compare it with didactic teaching. The results showed that overall, trainee doctors and staff, if given an option, prefer CBL to didactic teaching as a method of learning. However, there was no statistically significant difference in the knowledge outcome between the two groups as determined by MCQ-based tests.
The students in our study overwhelmingly acknowledged that they enjoyed CBL and thought that it was a better way of learning than didactic teaching. Both students and staff agreed that CBL helped in deeper learning and in promoting critical thinking than didactic teaching. Our findings are in consonance with the findings of a systematic review on CBL done in Australia in which the authors found that CBL was enjoyed and was thought to enhance their learning both by students and staff.[1]
In a study done in Malaysia, second-year medical students who had CBL in clinical pharmacology also felt that CBL was more enjoyable, stimulating and to increase the confidence on the subject that was taught.[9]
Both students and staff perceived that CBL promotes critical thinking which is essential for healthcare workers in all disciplines. Similar results have been found in a study in nursing students where the authors showed that case-based learning deepened understanding and critical thinking.[10] In a study from China, postgraduate students studying oncology scored higher in critical thinking and knowledge when compared to students who have traditional teaching.[11]
Our students also felt that CBL facilitated self-directed learning by helping them identify areas where they lack knowledge and to read more on the topic. The importance of self-directed learning cannot be overstated. A systematic review done on self-directed learning in health profession education showed that when compared to traditional teaching methods, self directed learning imoroved knowledge domains but skills and attitudes domain were similar.[12] A recent study from India also showed that first-year medical students who had CBL felt strongly that CBL enhanced their self-learning skills.[13]
Students also found the role of a facilitator useful. A Mayo clinic study showed similar perception among internal medicine trainees who felt that faculty support for self-directed learning was important and useful.[14]
The students and staff strongly agreed that discussion with other peers was useful. Learner-centerd teaching is best when done in groups, especially small groups,[15] and it is in agreement with Maslow's hierarchy of needs which states that learning begins only after physical, emotional, and social needs are met.[16] The discussion with peers in the group provides a nonintimidating environment for the student to freely ask questions and discuss difficult aspects of the case.
The enthusiasm of the students and the staff for CBL did not extend to multiple-choice questions as the method of assessing the impact of CBL. The marks in the assessment also did not differ from the didactic group. Our study had few limitations. MCQ-based tests may not be the best way to assess the practical knowledge of trainee doctors. We also have not assessed how CBL impacts patient outcomes. However, there are other studies which have shown that CBL does positively impact patient outcomes.[17,18,19,20]
The innate design of CBL also fits in with the ideals spelt out by the National Medical Commission of India on Competency-based undergraduate curriculum for the Indian medical graduate on making medical education more learner-centric and patient-centric.[21] The findings of our study also encourage leaders in newer and rapidly developing clinical specialties like Family Medicine to incorporate case-based learning in the academic program for trainee doctors in their specialties.
Conclusion
Given the overall impression of the students and the staff that CBL is a useful learning experience and the same has been found in various other disciplines and different stages of healthcare learning, we recommend that CBL be incorporated in medical teaching at all levels and across the spectrum of healthcare education.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Thistlethwaite JE, Davies D, Ekeocha S, Kidd JM, MacDougall C, Matthews P, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME guide No. 23. Med Teach. 2012;34:e421–44. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 2.Kamat SK, Marathe PA, Patel TC, Shetty YC, Rege NN. Introduction of case based teaching to impart rational pharmacotherapy skills in undergraduate medical students. Indian J Pharmacol. 2012;44:634–8. doi: 10.4103/0253-7613.100400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu SB, Peng B, Song YL, Xu QA. Application of case-based learning in clinical internship teaching of conservative dentistry and endodontics. Shanghai Kou Qiang Yi Xue. 2013;22:711–4. [PubMed] [Google Scholar]
- 4.Hansen WF, Ferguson KJ, Sipe CS, Sorosky J. Attitudes of faculty and students toward case-based learning in the third-year obstetrics and gynecology clerkship. Am J Obstet Gynecol. 2005;192:644–7. doi: 10.1016/j.ajog.2004.10.595. [DOI] [PubMed] [Google Scholar]
- 5.Williams B. Case based learning--a review of the literature: Is there scope for this educational paradigm in prehospital education? Emerg Med J. 2005;22:577–8. doi: 10.1136/emj.2004.022707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nair SP, Shah T, Seth S, Pandit N, Shah GV. Case based learning: A method for better understanding of biochemistry in medical students. J Clin Diagn Res. 2013;7:1576–8. doi: 10.7860/JCDR/2013/5795.3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McManus IC, Richards P, Winder BC, Sproston KA. Clinical experience, performance in final examinations, and learning style in medical students: Prospective study. BMJ. 1998;316:345. doi: 10.1136/bmj.316.7128.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newble DI, Hejka EJ, Whelan G. The approaches to learning of specialist physicians. Med Educ. 1990;24:101–9. doi: 10.1111/j.1365-2923.1990.tb02507.x. [DOI] [PubMed] [Google Scholar]
- 9.Hasamnis AA, Arya A, Patil SS. Case-based learning: Our experience in clinical pharmacology teaching. J Pharm Bioallied Sci. 2019;11:187–9. doi: 10.4103/jpbs.JPBS_135_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hofsten A, Gustafsson C, Häggström E. Case seminars open doors to deeper understanding-Nursing students’ experiences of learning. Nurse Educ Today. 2010;30:533–8. doi: 10.1016/j.nedt.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Bi M, Zhao Z, Yang J, Wang Y. Comparison of case-based learning and traditional method in teaching postgraduate students of medical oncolog. Med Teach. 2019;10:1124–8. doi: 10.1080/0142159X.2019.1617414. [DOI] [PubMed] [Google Scholar]
- 12.Murad MH, Coto-Yglesias F, Varkey P, Prokop LJ, Murad AL. The effectiveness of self-directed learning in health professions education: A systematic review. Med Educ. 2010;44:1057–68. doi: 10.1111/j.1365-2923.2010.03750.x. [DOI] [PubMed] [Google Scholar]
- 13.Muthukrishnan SP, Chandran DS, Afreen N, Bir M, Dastidar SG, Jayappa H, et al. Planning, implementation, and evaluation of multicomponent, case-based learning for first-year Indian medical undergraduates. Adv Physiol Educ. 2019;43:504–11. doi: 10.1152/advan.00080.2019. [DOI] [PubMed] [Google Scholar]
- 14.Sawatsky AP, Ratelle JT, Bonnes SL, Egginton JS, Beckman TJ. Faculty support for self-directed learning in internal medicine residency: A qualitative study using grounded theory. Acad Med. 2018;93:943–51. doi: 10.1097/ACM.0000000000002077. [DOI] [PubMed] [Google Scholar]
- 15.Newble D, Cannon R. Teaching in Small Groups. A Handbook for Medical Teachers. 4th edition. Boston: Kluwer Academic Publishers; 2002. pp. 39–53. [Google Scholar]
- 16.Maslow AH. Higher and Lower Needs. Motivation and Personality. New York: Harper and Row; 1970. pp. 93–104. [Google Scholar]
- 17.Mitruka K, Thornton K, Cusick S, Orme C, Moore A, Manch RA, et al. Expanding primary care capacity to treat hepatitis C virus infection through an evidence-based care model--Arizona and Utah, 2012-2014. Morb Mortal Wkly Rep. 2014;63:393–8. [PMC free article] [PubMed] [Google Scholar]
- 18.O’Connor PJ, Sperl-Hillen JM, Johnson PE, Rush WA, Asche SE, Dutta P, et al. Simulated physician learning intervention to improve safety and quality of diabetes care: A randomized trial. Diabetes Care. 2009;32:585–90. doi: 10.2337/dc08-0944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansen WF, Ferguson KJ, Sipe CS, Sorosky Attitudes of faculty and students toward case-based learning in the third-year obstetrics and gynecology clerkship. J Am J Obstet Gynecol. 2005;192:644–7. doi: 10.1016/j.ajog.2004.10.595. [DOI] [PubMed] [Google Scholar]
- 20.Williams B. Case based learning--A review of the literature: Is there scope for this educational paradigm in prehospital education? Emerg Med J. 2005;22:577–81. doi: 10.1136/emj.2004.022707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Competency based undergraduate curriculum for the Indian medical graduate 2018. Medical Council of India. Available from: https://www.mciindia.org/CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-II.pdf . [PubMed]


