Abstract
Introduction:
Virtual clinic is a new concept in India. This summary describes that how a virtual clinic is transforming the healthcare scenario in rural India. Virtual clinic is based on a social business model, which may involve diverse stakeholders to promote primary care.
Aim:
This virtual e-clinic aims to expand health outreach in rural and hard-to-reach areas of India and provide primary health care services by connecting local practitioners and health workers visiting patients with qualified allopathic doctors in city through video conferencing technologies.
Methodology:
This was a cross-sectional study evaluating the feasibility and acceptance of virtual primary care. A convenient sampling method was used. Data on demographic profiles, morbidity patterns, and referrals were collected with proper consent. This virtual clinic comprises of smartphones, monitors, and assistive devices so that patient can interact with the doctors through video-conferencing and can have authenticated prescriptions with standardized protocols. The private organization who initiated the virtual care program had two centers at the beginning and gradually expanded them to 20 in Uttar Pradesh. Consultations charges were kept minimum to no-profit, no-loss. Data were collected from January 2019 to June 2010.
Results:
Total number of consultations made was 800. Out of 800 patients, 157 patients belonged to age group of ≥60 years. Mean age the patient was 56 ± 1.56 years, among them 421 (52.62%) were male. The participants actively engaged in clinical interactions and completed full sessions of consultations, which highlight the acceptability of the virtual care system and feasibility of effective patient-provider communication and service delivery using digital technologies.
Conclusion:
The concept of virtual primary care is becoming very popular in rural region where no qualified doctors are available. The initial results of this technological startup appears to be promising; however, it is necessary to evaluate the quality of care, health outcomes, potentials to integrate such innovations in existing primary care, and the legal as well as ethical issues in the future research.
Keywords: Digital health, e-clinic, e-referral, telehealth, telemedicine, virtual clinic
Introduction
Whenever we discuss the healthcare-related issues, availability of adequate number of doctors providing basic healthcare services in the under privileged areas is the key in improving health outcomes in our country. Though now, we have adequate strength of primary care physicians, the problem is their maldistribution.[1]
A new National Health Policy and the National Health Assurance Mission are already in the place. It is high time to critically analyze the options available to policy makers for resolving the current situation.[1]
Nearly 69% of India's population resides in its villages where only 26% (nearly) of its doctors serve that too mostly in the private sector. This is very expensive and beyond the reach of common people. In India, > 833 million people are dependent on 44,000 doctors, which highlight the severe scarcity of human resources for health.[2] Also, a major proportion of trained health workers including specialist physicians reside near major cities, which results in a massive maldistribution of health workforce. On an average each doctor serves 19,000 population, which critically impacts the quality of care. Moreover, this situation is responsible for to ever-increasing out of pocket expenditures (OOP) on health. This in turn, impoverishes 3.3% of India's population per year.[3] These issues are pertinent to primary care as a majority of population health needs are envisioned to address at the primary care level, resulting in a reduction in referral to specialist care through primary and secondary prevention, saving cost of care, and delivering optimal health services within the reach of the communities.[4,5]
The existing problems related to lack of access to primary care for a major proportion of population can be solved by some extent by virtual primary care (VPC) services, in which patients consult with a doctor or nurse via email, text, phone, or video.[6,7] It is presumed to offer a number of advantages over traditional, brick-and-mortar general practitioner (GP) services, particularly in terms of accessibility and cost. However, evidence of their effect on clinical outcomes and quality of care is scant in Indian context. Furthermore, if integrated poorly into existing care systems and payment regimes, VPC services will not create sustainable change but will instead have the potential to contribute to the fragmentation of the health system. This article reports the preliminary findings of a VPC system implemented in rural India and describes the feasibility and acceptability of VPC in advancing primary care in India[4]
Methodology
E-mitra clinic is a social business model innovated by Jiyyo Innovations a Chandigarh based startup. Jiyyo e-mitra clinic aims to outreach rural and interior parts of India and provide primary healthcare services by connecting local practitioners and health workers visiting patients with qualified allopathic doctors in city through video call. Jiyyo has changed the scenario of telemedicine and made it available to areas with poor infrastructure [Figures 1 and 2].[8] There is no need of costly equipment. A simple smartphone is the primary requirement. Additional devices like screen and printer are added so that patient can visualize the doctors, communicate their health problems, and can have printed authentic prescriptions as provided by the medical practitioners.
Figure 1.
Work flow of Jiyyo Mitra e-Clinic-Step-1 Jiyyo app is installed from google play store. Step-2 Jiyyo account is created. Step-3 Entering patient details, selection of doctors and referral are done in a single user-friendly screen. Step-4 Scroll down and tap outgoing consultation. Step-5 Find the outgoing tap the video icon. Step-6 Video consultation starts with the doctor
Figure 2.
Patient consultations (permission taken for the pictures)
This was a cross-sectional prospective study. A convenient sampling method was used. Data were collected after taking proper consent. Such data comprised of the demographic profiles, morbidity patterns, and referrals for individual patients participating in E-mitra clinic. The private organization implementing this clinic initiated the project with two centers and gradually increased them to 20 within Uttar Pradesh. In this initiative, the consultations charges were kept at minimal level based on a no profit and no loss model. Data for this project were collected from January 2019 to June 2019.
Results
Our study revealed that most of the patients were given consultations by general physicians but specialist and super specialist consultations were also provided including pediatrics, orthopedics, dermatology, urology, nephrology, cardiology, and neurosurgery. This e-clinic provided neurosurgery consultations to two paraplegic patients. We analyzed the data of five centers. Total number of consultations was 800. Out of 800 patients 157 patients belonged to age group 60 years and above. Mean age of the patient was 56 ± 1.56 years; among them, 421 (52.62%) were male. In a different study, data highlight that 53% of Babylon GP at Hand's users are male and 89% are between the ages of 18 and 39 years, and just 1% are > 65 years.[9] It is found in Sweden, children and metropolitan residents are the main users, whereas people > 65 years, people with chronic diseases, and rural residents account for only a small proportion of consultations by virtual clinics.[10] All the patients were from rural background. Highest education level was middle school (10%) followed by primary school (21%) and illiterate was (69%). We found that osteoarthritis, lower backaches, allergic problems (bronchial asthma), and skin problems are the major problems affecting the patients in this region and more than two-third of the people chew tobacco [Table 1]. Thus, poor dental hygiene was also commonly seen. These e-clinics referred about six patients to higher center with trismus or poorly healing mouth ulcers for oral cancer screenings. Patients suspected to have tuberculosis were sent to nearby dispensary for diagnosis and treatment. But the most disturbing fact observed was that all these patients are taking steroids regularly. A 10-mg prednisolone is almost prescribed to all (87.5%) and > 50% of patients are taking benzodiazepines from years.
Table 1.
Disease pattern among the participants
| Disease | n=157 | Percentage |
|---|---|---|
| Knee osteoarthritis | 28 | 17.81 |
| Skin problems | 23 | 4.6 |
| Lower back aches | 21 | 13.4 |
| Bronchial asthma | 18 | 11.5 |
| Gastrointestinal problems | 12 | 7.6 |
| Hypertension | 10 | 6.3 |
| Oral problems | 7 | 4.4 |
| Cardiac problems | 5 | 3.2 |
| Diabetes | 6 | 3.8 |
| URI | 5 | 3.2 |
| Urological problems | 4 | 2.5 |
| Blood malignancy | 3 | 1.9 |
| Pulmonary TB | 3 | 1.9 |
| Neurological problems | 3 | 1.9 |
| UTI | 2 | 1.3 |
| Uterine prolapse | 2 | 1.3 |
| Others | 5 | 3.2 |
The participants (n = 157) willingly participated and completed the entire sessions of consultation, which illustrate the acceptability of the E-mitra clinic system. Also, the dispatched prescriptions revealed diagnosis, offered treatment, and referred advanced or complex cases, which highlight the feasibility of the VPC in the context of rural India.
Discussion
The preliminary findings of this study indicate the acceptability and feasibility of VPC in rural India, which may improve access to qualified healthcare providers for a massive population. Significant number of patients requiring more tests for diagnosis or referral to higher center expressed inability to do so, due to financial constraints. Most patients rely on steroids for treatment, which necessitate adequate preventive and therapeutic measures to address misuse of steroids at grassroot level. We think that with continuous efforts and counseling, we will able to inoculate and promote healthy lifestyle habits among people in this region. The existing efforts show that the e-clinics becoming popular in a rapid pace, which may help to alleviate the burden of primary care centers by offering remotely available virtual services without compromising access to qualified providers. The acceptability from provider side and recipient side was good, which implies potential sustainability and possibilities for expansion of such services in a wider geographical area. The patient turnover is getting high and most of the patients are satisfied which is indicated by re-visits in these e-clinics. Thus, e-clinics can contribute to addressing inequity issues in healthcare in India.
Despite promising impacts and policy implications for improving rural and primary care, it is essential to evaluate the ethical issues related to VPC systems. For any medical interventions delivered through digital platforms, informed choice of patients and technology literacy plays a vital role.
Diffusion of new technology plays a vital role for implementation any new technology. It is better explained by Technology Acceptance Model (TAM) [Figure 3].
Figure 3.
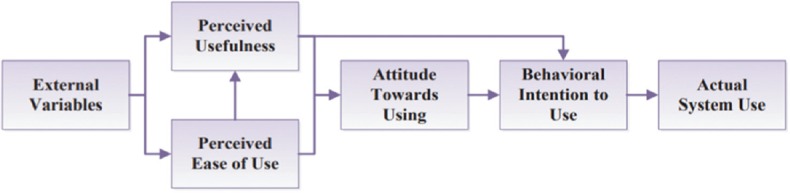
Technology acceptance model
TAM explains why some people accept technology very easily and some are not. This model describes that “an individual's behavioral intention to use a system is determined by two beliefs: perceived usefulness, and perceived ease of use.” This model assumes that the role of external factors, such as system features, development process, and training, on intention to use is mediated by perceived usefulness and perceived ease of use.[8,9,10,11,12]
However, VPC services are suitable for the people residing in remote areas where people do not have regular access to highly personalized or multidisciplinary services.
Regarding VPC, we few concerns which may inform future research and development in this area. First, in the near future VPC organizations, might also engage in risk selection or cream skimming, i.e., intentionally selecting or seeking to attract fewer complex patients, so that they can profit more by recurrent visits. Such approaches must be examined through implementation research so that technologies with potentials to improve health access do not leave those individuals who need the services most. Second, in the developed countries like England, when less complex patient groups deregister from their existing practices and they register themselves with virtual services, there is a possibility that GPs would be left with increasingly complex patient lists. A balanced and collaborative system is essential, which can incorporate virtual services within the existing service paradigm without affecting the service delivery process to the right individuals through the right provider in the right time. Third, VPCs might also introduce cost inflation and cost shifting, which is partly due to their high registration and turnover rates.[13,14,15,16,17,18] Such economic implications and health systems financing should be evaluated to determine how technological interventions can be optimally used ensuring economic sustainability. Last but not least, the quality of patient–provider interaction, consultations, health services, and patient-level outcomes in VPCs should be evaluated prior to large scale adoption. In a country like India, the quality of care should be placed at the heart of digital revolution in primary care so that quantitative measures like how much population does not affect the health rights of individuals and populations. VPCs should be further developed and adopted upholding the ethical and clinical values to promote primary care in India.
Limitations
The findings of this study are constrained by small sample size. Therefore, future studies with larger sample size and more explanatory variables are required. Moreover, mixed-method studies may inform more issues related to the adoption and use of VPC among the study population.
Conclusion
E-clinics (Virtual Primary Care) holds promise in bridging the rural urban health care gaps to a large extent, however, key issues like ethical and socioeconomic issues affecting the quality of care and population level health outcomes should be investigated in the future. The existing evidence show promising impacts in terms of acceptability and feasibility of VPC in improving primary care, which necessitates more research and policy discourses on successful integration of VPCs in primary care system in the context of India.
Consent
Taken from all patients for sharing their information for academic purpose.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Deo MG. Doctor population ratio for India-The reality. Indian J Med Res. 2013;137:632. [PMC free article] [PubMed] [Google Scholar]
- 2.Pages-RHS2017 [Internet] cited 2019 Feb 15. Available from: https://nrhm-mis.nic.in/Pages/RHS2017.aspx?RootFolder=%2FRURAL%20HEALTH%20STATISTICS%2F%28A%29RHS%20-%202017&FolderCTID=0×01200057278FD1EC909F429B03E86C7A7C3F31 and View=%7B9029EB52-8EA2-4991-9611-FDF53C824827%7D .
- 3.Furtado KM, Kar A. Health resources in a 200,000 Urban Indian population argues the need for a policy on private sector health services. Indian J Community Med. 2014;39:98–102. doi: 10.4103/0970-0218.132727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clarke JL, Bourn S, Skoufalos A, Beck EH, Castillo DJ. An innovative approach to health care delivery for patients with chronic conditions. Popul Health Manag. 2017;20:23–30. doi: 10.1089/pop.2016.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baillieu R, Kidd M, Phillips R, Roland M, Mueller M, Morgan D, et al. The primary care spend model: A systems approach to measuring investment in primary care. BMJ Glob Health. 2019;4:e001601. doi: 10.1136/bmjgh-2019-001601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lougheed T. Time to embrace the promise of virtual health care. CMAJ. 2019;191:E320–1. doi: 10.1503/cmaj.109-5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meehan D, Balhareth A, Gnanamoorthy M, Burke J, McNamara DA. Efficacy of physician associate delivered virtual outpatient clinic. Int J Health Care Qual Assur. 2019;32:1072–80. doi: 10.1108/IJHCQA-09-2018-0233. [DOI] [PubMed] [Google Scholar]
- 8.Wharton GA, Sood HS, Sissons A, Mossialos E. Virtual primary care: Fragmentation or integration? Lancet Digital Health. 2019;1:e330–1. doi: 10.1016/S2589-7500(19)30152-9. [DOI] [PubMed] [Google Scholar]
- 9.Jiyyo Mitra e-Clinic–Multispeciality Online Consultation Center | J iyyo. Internet. cited 2019 Aug 18. Available from: https://www.jiyyo.com/jiyyo-mitra-e-clinic-online-consultation-center .
- 10.Bostock N. GP online, in charts: How GP at hand pulled in 32,000 new patients in 12 months. [Last accessed on 2019 Jul 22]. Available from: https://www.gponline. com/charts-gp-hand-pulled32000-new-patients-12-months/article/1518915 .
- 11.Pulse. Digital practice patients three times more likely to return to prior GP surgery. [Last accessed on 2019 Oct 01]. Available from: http://www.pulsetoday.co.uk/news/all-news/digital-practicepatients-three-times-more-likely-to-return-to-prior-gpsurgery/20038965.article .
- 12.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13:319. [Google Scholar]
- 13.Kumar R, Bhattacharya S, Sharma N, Thiyagrajan A. Cultural competence in family practice and primary care setting. J Family Med Primary Care. 2019;8:1–4. doi: 10.4103/jfmpc.jfmpc_393_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhattacharya S, Sharma N, Singh A. Designing culturally acceptable screening for breast cancer through artificial intelligence-two case studies. J Family Med Primary Care. 2019;8:760. doi: 10.4103/jfmpc.jfmpc_391_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Economics Consortium. Evaluation of Babylon GP at hand. Final evaluation report. May. 2019. [Last accessed on 2019 Oct 01]. Available from: https://www. hammersmithfulhamccg.nhs.uk/media/156123/Evaluation-of-BabylonGP-at-Hand-Final-Report.pdf .
- 16.Ashwood JS, Mehrotra A, Cowling D, Uscher-Pines L. Direct-to-consumer telehealth may increase access to care but does not decrease spending. Health Aff. 2017;36:485–91. doi: 10.1377/hlthaff.2016.1130. [DOI] [PubMed] [Google Scholar]
- 17.Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: Cross sectional study of routinely collected, person level data. BMJ. 2017;356:j84. doi: 10.1136/bmj.j84. [DOI] [PubMed] [Google Scholar]
- 18.BMA and NHS England: Investment and evolution: A five-year framework for GP contract reform to implement The NHS Long Term Plan. 2019. [Last accessed on 2019 Oct 01]. Available from: https://www.bma.org.uk/-/media/files/pdfs/collective%20voice/committees/gpc/gpc%20england/investment-and-evolution-five-yearframework.pdf?la=en .




