Abstract
Rhinosporidiosis is a type of nasal polypoidal growth arising from the mucosa of nasal cavity and often extending to nasopharynx. Occasionally, this growth may invade the lower airways and cause airway obstruction. The clinical presentation of such cases is often contradictory and airway management during induction of anesthesia requires caution to prevent potential life-threatening situations. A case of large pedunculated rhinosporidiosis involving the epiglottis and laryngeal inlet, with significant airway management challenge has been presented here. Clinical significance: Primary care physicians should be diligent in evaluating patients with rhinosporidiosis and look for signs of airway obstruction to rule out lower airway involvement.
Keywords: Airway management, larynx, rhinosporidiosis, tracheostomy
Abbreviations
FOB: Fiber optic bronchoscope
CT scan: Computed tomography scan.
Introduction
Rhinosporidiosis is a common type of nasal polypoidal mass seen in Indian subcontinent.[1] This usually occurs as a soft, friable highly vascular polypoidal mass arising from the nasal mucosa, often invading to nasopharynx and rarely may involve lower airways.[2] The latter scenario can engender significant airway management challenge.
Case Report
A 20-year-old male patient presented to the Department of Otolaryngology at our hospital with complaints of nasal blockage, intermittent discharge, and bleeding from right side of the nose for the past 10 years. Upon enquiry, the patient revealed to have dysphagia, difficulty in breathing in supine position, and occasional choking sensation on deep inspiration. He was unable to lie supine and used to adopt a lateral decubitus position while sleeping.
On examination, the right nostril was found to be completely blocked with the polypoidal growth. There was no visible growth in the oropharynx, which initially misled us to think that the growth was confined to the nose and nasopharynx [Figure 1]. Interestingly, when the patient coughed or made a grunting sound, a papillomatous growth appeared in the posterior part of the tongue, filling up the oral cavity [Figure 2]. The CT scan of the head and neck revealed a growth extending from the right side of the nose to the hypopharynx and completely obstructing the laryngeal aperture [Figures 3-5]. The patient was scheduled for a fine endoscopic sinus surgery under general anesthesia. In the operating room, awake fiberoptic bronchoscope (FOB)-guided orotracheal intubation was planned and airway was anesthetized by nebulization with 4% lignocaine. Prior to attempting any airway intervention, a flexible endoscopic examination revealed a large friable growth completely covering the epiglottis and laryngeal inlet, which made FOB-guided endotracheal intubation impractical [Figure 6]. A decision was, therefore, taken to secure the airway by surgical tracheostomy under local anesthesia. Anesthesia team was ready for cricothyroidotomy in case of any emergency. Tracheostomy was successfully performed by the otolaryngologist in a modified semi-recumbent position. General Anesthesia was induced with intravenous fentanyl 2 μg/kg, propofol 2 mg/kg, and vecuronium 0.1 mg/kg, and maintained with N2O/O2 and isoflurane. The fleshy mass was removed in piecemeal. Intraoperative blood loss was 1500 ml which was managed with intravenous fluids and blood transfusion. After excision of the growth, there were raw areas on epiglottis and along the margins of the false vocal cords. Anterior and posterior nasal packing was done to control the oozing from the raw surfaces. After reversal of anesthesia, the patient was shifted to the postoperative ward with spontaneous respiration. Nasal packing was removed after 48 h and decannulation of tracheostomy tube was done on 3rd postoperative day of surgery. Patient was discharged from hospital on the 5th postoperative day. Histopathological examination of the excised mass confirmed the diagnosis of rhinosporidiosis.
Figure 1.

No visible growth on mouth opening
Figure 2.

A papillomatous rhinosporidiosis mass fills up the oral cavity on coughing
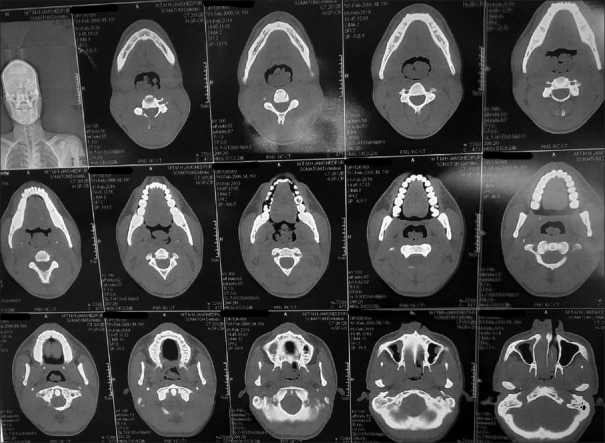
Figure 3.
CT scan of head and neck (axial view) showing the rhinosporidiosis mass
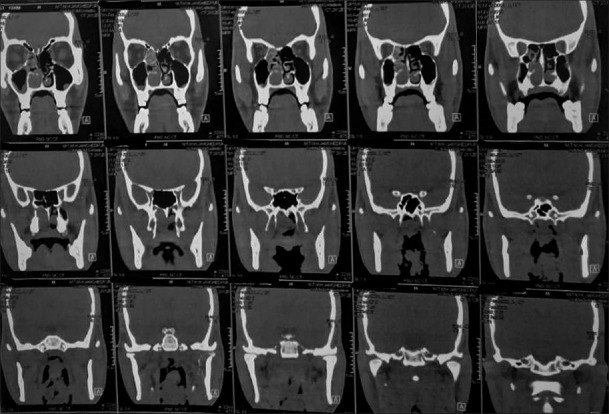
Figure 5.
CT scan of head and neck (coronal view) showing the rhinosporidiosis mass
Figure 6.

Endoscopic image of the rhinosporidiosis mass
Figure 4.
CT scan of head and neck (sagittal view) showing the rhinosporidiosis mass
Discussion
The most common symptoms in patients with nasal rhinosporidiosis are nasal blockage and rhinorrhea. In the present case, the patient had unusual presentations of dysphagia and breathing difficulty, especially in supine position, which was indicative of possible airway involvement by the mass causing obstruction. The anesthetic challenges in our case were the difficulty in securing the airway and the risk of bleeding from the polyp during airway manipulation. Therefore, awake FOB-guided endotracheal intubation was planned with emergency tracheostomy as standby. However, a preoperative check endoscopy of airway revealed a mass of significant size present over the laryngeal inlet, which refrained us from going for awake endotracheal intubation. Even the option of tracheostomy was difficult in our case, as the patient was unable to lie supine for a long duration. However, tracheostomy was successfully performed by keeping the patient in semi-recumbent position under local anesthesia.
Extranasal involvement of rhinosporidiosis is rare and there are few case reports describing the management of laryngotracheal extension.[3,4,5] The overall incidence of laryngeal rhinosporidiosis was reported to be 0.89%.[6]
Anesthetic management of a large antrochoanal polyp has been previously reported.[7,8] In one of the case reports, there was difficulty in mask ventilation due to collapse and obstruction of the airway by the polyp after administration of muscle relaxant during induction of anesthesia and endotracheal intubation was finally done using FOB by manipulating the bronchoscope around the growth.[8] However, there is always the risk of failed intubation in such scenarios. Therefore, it is always prudent to go for awake endotracheal intubation or elective tracheostomy whenever there is a suspicion of airway involvement by the nasal polyp.
Awake FOB-guided intubation was not an option in this case, as the polyp in our case was a large friable rhinosporidiosis, which is known to be highly vascular.[9] Any uncontrolled airway manipulation around the mass would have caused trauma to the growth, which not only would have led to massive bleeding and pulmonary aspiration but also may have caused spillage of endospores. The latter condition might cause autoinoculation into the lower airways, inadvertently contributing to recurrence.[10]
It is mandatory to examine these patients thoroughly, as the initial impression of a normal-appearing airway may be misleading. In our case, the initial assessment did not reveal any mass at the posterior pharyngeal wall until the patient coughed, which brought out the mass. However, the history (breathing difficulty in supine position) was suggestive of airway obstruction. A thorough preoperative examination including a flexible endoscopy should be performed to evaluate the extent of the growth to avoid any judgmental errors in handling the airway.
In our case, we could have ended up in “Cannot Intubate Cannot Oxygenate” situation, if the potential hazardous airway had not been anticipated. Therefore, elective tracheostomy was probably the safest available option in our case.
Conclusion
Anesthetic management of laryngeal rhinosporidiosis is challenging. Diligent history taking, meticulous examination, and review of investigations aid in appropriate decision making, minimizing judgmental errors, and preventing airway-related catastrophe.
Clinical significance: The role of the primary care physician in diagnosing airway obstruction due to laryngeal rhinosporidiosis is of utmost importance and aids in planning the optimal airway management technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vukovic Z, Bobic-Radovanovic A, Latkovic Z, Radovanovic Z. An epidemiological investigation of the first outbreak of rhinosporidiosis in Europe. J Trop Med Hyg. 1995;98:333–7. [PubMed] [Google Scholar]
- 2.Sharma KD, Junnarkay RV, Ararwal S. Rhinosporidiosis. J Indian Med Assoc. 1962;38:640–2. [PubMed] [Google Scholar]
- 3.Kini G, Gopalkrishna A, Thomas D. Anaesthesia for unusual presentation of rhinosporidiosis: A case report. Sri Lankan J Anaesthesiol. 2010;18:39–42. [Google Scholar]
- 4.Banjara H, Panda RK, Daharwal AV, Sudarshan V, Singh D, Gupta A. Bronchial rhinosporidiosis: An unusual presentation. Lung India. 2012;29:173–5. doi: 10.4103/0970-2113.95336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tiwari D, Bakshi SS, Das S, Gopalakrishnan S. Disseminated rhinosporidiosis. Arch Med Health Sci. 2019;7:84–6. [Google Scholar]
- 6.Chakraborty D, Das C, Hansdah R. Three years’ experience of management of different types of rhinosporidiosis in rural part of western West Bengal. Bengal J Otolaryngol Head Neck Surg. 2015;23:92–8. [Google Scholar]
- 7.Prakash R, Bhatia VK. Anaesthetic management of a large atypical antrochoanal polyp for FESS. Int J Sci Res. 2013;2:90–1. [Google Scholar]
- 8.Chakravarty N, Shende S, Dave SP, Shidhaye RV. Airway management in a patient with large antrochoanal polyp. Anaesth Pain Intensive Care. 2014;18:198–200. [Google Scholar]
- 9.Prabhakar M, Ramesh S. Management of rhinosporidiosis: Our experience. Int J Sci Stud. 2015;3:62–5. [Google Scholar]
- 10.Capoor MR, Khanna G, Rajni, Batra K, Nair D, Venkatchalam VP, et al. Rhinosporidiosis in Delhi, North India: Case series from a non-endemic area and mini review. Mycopathologia. 2008;168:89–94. doi: 10.1007/s11046-009-9200-1. [DOI] [PubMed] [Google Scholar]