Abstract
The partial-thickness rotator cuff tears (PTRCTs) are known as a prevalent pathology, which cause inability mostly in athletes. So far, a number of treatments have been suggested depending on patient characteristics and size and location of the tears. Surgical repair in rotator cuff tears that include 50% or more of the tendon thickness is the accepted practice in the following failure of nonoperative treatment. In the surgical procedure, acromioplasty is known as a long-established component and used to modify the detrimental acromion morphology, which accounts for rotator cuff tearing. A range of trials has been reported that compare the results of surgical procedure with and without acromioplasty in patients undergoing rotator cuff repairs. According to the findings of 15 studies including ~1,500 patients, with mean age 60 years (range 5–80 years) and mean follow-up of 22 months (range 13–26 months) found by searching on Cochrane Register of Controlled Trials databases, Excerpta Medica/Embase, and Medline/PubMed, we revealed that acromioplasty cannot present an impressive effect on patient outcome scores at intermediate and short-term follow-ups. In fact, despite the theoretic advantages of acromioplasty in the setting of PTRCTs, it has reported little or no efficacy on outcomes of postoperative patients.
Keywords: Acromioplasty, partial-thickness rotator cuff tear, shoulder pain, surgical operation
Introduction
After lower back pain, shoulder pain is well-known as the second prevalent musculoskeletal disorder, which resulted from the rotator cuff disorders.[1] Rotator cuff tears (RCTs) are divided into two groups partial-thickness rotator cuff tears (PTRCTs) and full-thickness rotator cuff tears (FTRCTs). A partial-thickness tear goes only part of the way into the tendon[2] [Figure 1]. In fact, PTRCT is considered a prevalent pathology that can remarkably affect a range of patients such as athletes, workers, and sedentary individuals.[3] Despite the high outbreak of PTRCTs, most of the researches conducted on the treatment of RCT have centralized on FTRCTs.[4] Accordingly, PTRCT has been disregarded and, thus, its therapy remains controversial in the field of the tears of the rotator cuff.
Figure 1.
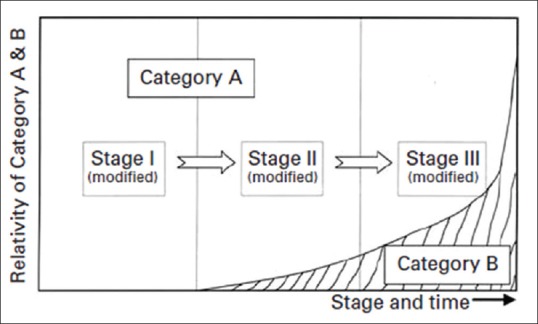
Diagram indicating how the symptoms of rotator cuff tears categorize as A and B. A group contains stage I and stage II as partial-thickness tears. B group contains stage III as full-thickness tears. Reprinted with permission[2]
So far, a number of researches have been carried out on the conservative management and the etiology of PTRCTs, and some on surgical techniques.[5,6] However, there is no review on the application of acromioplasty in the setting of PTRCTs. As mentioned above, this review was aimed at the assessment of the current state of knowledge regarding the application of acromioplasty in the setting of PTRCTs.
Partial-Thickness Rotator Cuff Tears (PTRCTs)
The most clinical algorithms and classification systems of how to treat PTRCTs are according to Clark and Harryman,[3] although the accurate anatomy of the RCTs continues to be developed. They indicated that the rotator cuff comprises five discrete histologic layers. The tendinous fibers can be observed in the second and third layers, whereas the remaining layers loose connective tissue and contain arterioles [Figure 2].
Figure 2.
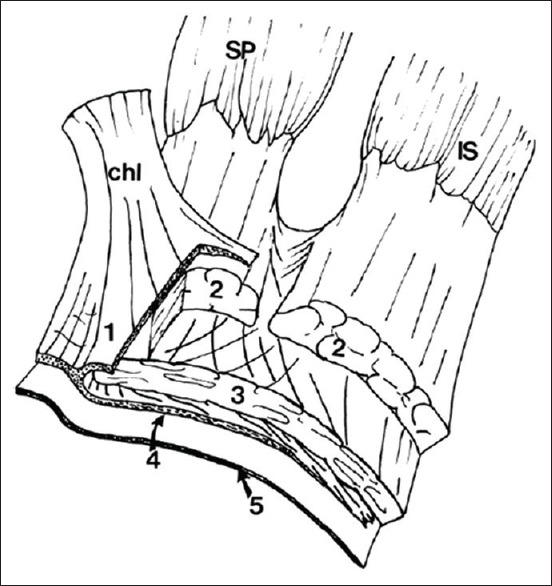
Diagram indicating five distinct histologic layers for rotator cuff insertion. IS = infraspinatus, SP = supraspinatus, Chl = coracohumeral ligament. Reprinted with permission[5]
The results from imaging and cadaveric research revealed that the prevalence of PTRCTs ranges from 14% to 33%, which strongly correlated to age in patients.[2] Sher et al.[7] in an MRI study on symptomless subjects averagely estimated the prevalence of PTRCTs as 21%. The authors represented the prevalence of 26% for subjects over 60 years old, and the prevalence of 4% for subjects under 60 years old. The age-related prevalence was also stated by a study on rotator-cuff changes in symptomless subjects that found a prevalence of PTRCTs of 80% in patients aged 70 years or older, and 10% in patients aged 40–60.[8] The authors showed a linear growth in the prevalence of RCT in subjects aged over 50 years old.
The pathogenesis and etiology of PTRCTs suggest that an individual's rotator cuff lesion is affected by both extrinsic and intrinsic factors. Intrinsic factors comprising the declined tissue vascularity and age-related microscopic shifts (granulation tissue, fascicular thinning, and hypocellularity) can make susceptible a tendon to degenerative tearing.[9,10] Extrinsic factors comprising internal impingement, glenohumeral instability, and subacromial impingement result in a continuing pathology of PTRCTs.[5,11] Furthermore, traumatic accidents contribute to elastic overload and fiber failure of the RC. It assumes that PTRCTs usually augment in size over time because of the boosted tendon strain due to a tear.
The clinical appearance of PTRCTs is different extensively, although pain is considered as the most prevalent symptom. The ordinary appearances observed at patients comprise positive impingement signs, weakness, as well as the painful arc of motion.[12] Furthermore, it was documented that strains with overhead sports or activities are common in terms of PTRCTs.[10] It is notably the relation between imaging research and clinical outcome is crucial because of the high prevalence of asymptomatic PTRCTs in patients. PTRCTs can be discovered by ultrasonography and MRI, with similar efficacy. This finding has been supported by arthroscopy studies.[13] Despite development in imaging methods, arthroscopy yet remains the routine procedure for diagnosing PTRCTs.[5]
Treatments for PTRCTs includes nonoperative treatment and operative treatment. Surgical treatment is usually used in young subjects with a traumatic injury and in subjects with failure of nonoperative treatment for an average 4.5 months.[14] In surgical treatment, arthroscopic debridement can be combined with or without acromioplasty and carried out in patients that involve <50% of the tendon thickness.[14] The surgical treatments are described based on four procedures: completion and repair, repair in situ, subacromial decompression, and debridement. So far, appreciative findings have been achieved with conversion to full-thickness tears with repair,[15,16] repair in situ,[17,18] debridement and decompression,[18,19] and debridement.[20,21] However, operative treatment is mostly limited to tear debridement along acromioplasty or without this technique [Table 1].
Table 1.
The surgical outcomes of partial-thickness rotator cuff tears (PTRCTs) reported by previous studies
| Surgical intervention | Number of patients | Tear size treated (% articular) | Age, years (range) | Mean follow-up (months) | Conclusion | Study |
|---|---|---|---|---|---|---|
| Debridement only | 36 | All (N/R) | 22 (16-29) | 13 | Good or excellent results in 85%. | Andrews et al.[22] |
| Debridement, decompression and repair | 66 | All (33% articular) | 54 (20-75) | 32 | Excellent result in 59% | Fukuda et al.[17] |
| Debridement, bursectomy, decompression, and repair | 39 | N/R (54% articular) | 52 (21-73) | 55 | Good outcome in 44% | Wright et al.[6] |
| Debridement and Decompression Debridement, decompression, and open repair | 32 33 | >6 mm (89% articular) | 49 (N/R) 49 (N/R) | 47 38 | Good or excellent outcome in 94%. | Weber et al.[23] |
| Debridement and decompression | 25 52 | >3 mm (Grade I) 4-6 mm (Grade II) (84% articular) | 57 (36-90) 53 (33-73) | 53 | Mean L’Insalata score of 90 postoperatively | Cordasco et al.[14] |
| Debridement and decompression | 37 | <50% (<6 mm) (65% Articular) | 52 (34-70) | 42 | 84% Satisfactory outcomes for articular-sided, 93% for bursal-sided | Park et al.[4] |
| Debridement, decompression, and repair | 22 | >50% (>6 mm) (27% articular) | 55 (N/R) | 34 | Excellent outcome in 94% | Park et al.[18] |
| Debridement, bursectomy, and repair | 17 | >6 mm (100% Articular) | 42 (17-51) | 39 | Excellent result in 93% | Ide et al.[24] |
| Debridement and decompression | 26 | 3-6 mm (50% articular) | 51 (26-66) | 101 | 36% Progress to full-thickness rotator cuff tears (FTRCT) 37% stay PTRCT | Kartus et al.[25] |
| Debridement, completion and repair | 41 | >50% (80% Articular) | 49 (23-70) | 38 | Excellent good or result in 91% | Deutsch et al.[15] |
| Debridement, bursectomy and decompression | 46 | >50% (80% Articular) | 59 (33-76) | 50 | Excellent or good result in 91% | Liem et al.[19] |
| Debridement, bursectomy Decompression completion and repair | 42 | >50% (79% articular) | 53 (34-72) | 39 | Excellent or good result in 91%, 88% healing | Kamath et al.[26] |
Acromioplasty in the setting of PTRCTs
Acromioplasty is known as an arthroscopic surgical procedure of acromion, in which the subacromial space is decompressed and thereby the impingement of repaired structures is prevented [Figure 3]. In the open repair of the rotator cuff, the mechanical pressure on the rotator cuff was relieved by using the procedure of reshaping the acromion with acromioplasty. Ellman[27] first described the capability to carry out an arthroscopic acromioplasty. Since then, researchers have focused on determining the benefits and risks of open acromioplasty in contrast to the arthroscopic methodology.[28] The main benefit of the open procedure is easy to perform technically and low need for surgeon expertise.[28]
Figure 3.
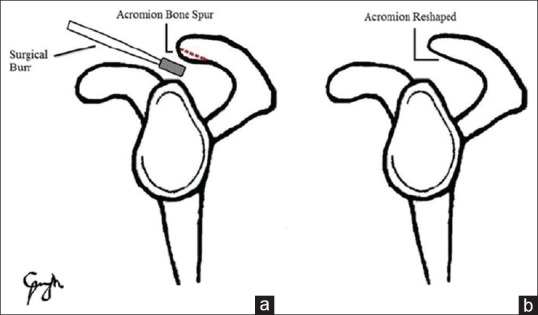
Acromioplasty. (a) removing the detrimental acromion morphology. (b) smoothing and reshaping the acromion, and removing the pressure placed on the rotator cuff. Reprinted with permission[29]
The growing evidence on RCTs revealed that the incidence of acromioplasty has dramatically elevated in a few decades ago.[30] Yu et al.[31] also found a 575% increment for the incidence of acromioplasty between 1980 and 2005 that reflects the widespread popularity of acromioplasty. Despite prevalent uses of acromioplasty, the function of the acromion was questioned in the pathogenesis of rotator cuff.[32,33] In regards, Tibone et al.[34] showed that acromioplasty cannot improve the pain in athletes with RCTs. Furthermore, acromioplasty with coracoacromial (CA) ligament release has been shown that may increase the instability in superior glenohumeral ligaments.[35,36,37] Reviews on the effect of acromioplasty for rotator cuff signs demonstrated the failure rates of 15–20%, and the findings were not as good as expected.[33,38] In fact, these researches questioned not only the function of the acromion in the pathogenesis of rotator cuff but also the meaning of RCT,[39,40] so that most of these researches propose that rotator cuff is a multifactorial disease, which resulted from both extrinsic and intrinsic causes.[12,41]
In the effort toward comparing the outcomes of the arthroscopic procedure with and without acromioplasty, similar results have been reported for PTRCT debridement along with and without acromioplasty. For instance, Ellman[42] reported the same reoperation rate for patients treated by debridement with and without acromioplasty. Itoi and Tabata[43] in a study on treatment a total of 38 shoulders with PTRCT by open repair and completion for 5 years indicated that the good outcomes were retained in 83%, with no diversities in repair technique with or without acromioplasty. Cordasco et al.[14] observed the same and poor findings in patients with 3–6 mm tear when treated by debridement with and without acromioplasty.
However, some studies revealed the different results for the outcomes of the arthroscopic procedure with and without acromioplasty. For instance, Liem et al.[19] in an effort on assessment the RCTs in 46 patients revealed that 20 patients with Ellman grade 2 tear were remedied with debridement combined with acromioplasty, whereas 26 subjects with Ellman grade 1 tear were remedied with acromioplasty alone. However, Neer[44] stated that acromioplasty must be carefully supplied for subjects with mechanical impingement. The author also suggested that acromioplasty must be carried out at least 1 year after nonoperative treatment, and only for subjects with reasonable life expectancy. Weber's in a study on 32 patients treated by arthroscopic acromioplasty found the satisfactory outcome in 45%, but 94% in 33 subjects treated by mini-open repair and acromioplasty.[23]
Hyvönen et al.[45] elucidated the result after acromioplasty with a mean follow-up of 10 years. Their findings discovered that the early outcome was good, but 12% of their subjects worsen after 5 years. The authors suggested that the tendon may tear even after removing the subacromial impingement. Similarly, Kartus et al.[25] recorded the higher progression of rotator cuff disease after debridement and acromioplasty in patients with partial-thickness Ellman grade 2 tear. The authors followed up 26 of 33 subjects for 5 years after debridement and acromioplasty by physical assessment and ultrasound. They observed a total of nine shoulders developed to FTRCT. Overall, for surgery of PTRCT, the repair along with acromioplasty appear to give satisfactory outcomes, such as 84–94 47%.[6,17,23,43,44,46,47]
Meanwhile, some researchers have suggested specific conditions for repair and acromioplasty success in treating the partial-thickness tears and have stated that it is impossible to comment on the usefulness of the surgical procedure combined with and without acromioplasty. For instance, Wright and Cofield[6] recommended cuff repair and open acromioplasty of PTRCTs that failed the conservative remedy. They observed that the satisfactory outcome may be expected after applying repair and acromioplasty for PTRCTs that embrace at least 50% of the cuff thickness. Weber[23] also suggested that if the tear includes more than 50% of tendon, debridement, and acromioplasty of PTRCTs would fail. They proposed that lesions repaired through a mini-open method own good outcomes than those that underwent debridement without repair, and suggested that this level of PTRCTs should be repaired. Fukuda et al.[17,48] believe that the open methodologies along with acromioplasty after excision of the diseased portion give some benefits, such as 1) the operation on the tendon is carried out with minimal risk and the same exposure; 2) concomitant intra-tendinous lamination is treated; 3) the tear progression is hindered by a suitable repair; 4) tissue repair is improved by cutting out of diseased tissue; 5) hidden lesions are uncovered through mobilization, palpation inspection, and exploration of tendon; 6) decompression is reinforced through tenorrhaphy; 7) beneficial repair of tendon is accomplished.
In total, our review revealed no discrepancy in short-term clinical outcomes between PTRCTs patients treated with and without acromioplasty procedure. In fact, our findings were according to the American Academy of Orthopaedic Surgeons (AAOS),[49] which suggested acromioplasty at a moderately advice for the rotator cuff treatment. On the findings resulted from a number of research,[50,51] acromioplasty was appeared not required for repairing RCTs. Despite theoretic advantages of acromioplasty in the setting of PTRCTs, it has reported little or no efficacy on outcomes of postoperative patients. In addition, one meta-analysis on patients undergoing arthroscopic repair of rotator cuff found no difference between patients treated with subacromial decompression and those treated without this procedure.[38]
It is notable that performing studies on rotator cuff disease and interpreting their outcomes are challenged with some difficulties. First, the pain origin in RCTs has not been well-known, making operation practical. Second, the rotator cuff disease includes a wide range of abnormalities. The patients who have a PTRCT or FTRCT may be a totally distinct from patient with impingement pain without any rotator cuff malformation at the time of arthroscopy. Similarly, the treatment may be dependent on the degree of partial tear as a critical factor.[52]
Conclusion
There are an increasing number of documents on assessment and the importance of acromioplasty in the rotator cuff treatment. Regardless of acromion morphology, the similar outcomes have been showed at intermediate and short-term follow-up of PTRCTs, either with or without acromioplasty.[53] As a result, these results do not defend the common application of acromioplasty as a supplement to arthroscopic for treatment of PTRCTs.[54] Nonetheless, our knowledge on the treatment of PTRCTs has been limited through the incapacity to know precisely what generates a satisfactory outcome with surgery of rotator cuff, and the unknown pathophysiology of disease of rotator cuff in patients. As mentioned above, more research is required to assay the important of acromioplasty alone in the PTRCTs treatment.[14]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Khan Y, Nagy MT, Malal J, Waseem M. The painful shoulder: Shoulder impingement syndrome. Open Orthop J. 2013;7:347–51. doi: 10.2174/1874325001307010347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85:3–11. doi: 10.1302/0301-620x.85b1.13846. [DOI] [PubMed] [Google Scholar]
- 3.Clark JM, Harryman DT. Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint SurgAm. 1992;74:713–25. [PubMed] [Google Scholar]
- 4.Park JY, Chung KT, Yoo MJ. A serial comparison of arthroscopic repairs for partial- and full-thickness rotator cuff tears. Arthroscopy. 2004;20:705–11. doi: 10.1016/j.arthro.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Elkins A, Lam PH, Murrell GA. A novel, fast, safe, and effective all-inside arthroscopic rotator cuff repair technique: Results of 1000 consecutive cases. Orthop J Sports Med. 2019;7:2325967119864088. doi: 10.1177/2325967119864088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright SA, Cofield RH. Management of partial-thickness rotator cuff tears. J Shoulder Elbow Surg. 1996;5:458–66. doi: 10.1016/s1058-2746(96)80018-8. [DOI] [PubMed] [Google Scholar]
- 7.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Milgrom C, Schaffler M, Gilbert S, Van-Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surgery Br. 1995;77:296–8. [PubMed] [Google Scholar]
- 9.Bey MJ, Ramsey ML, Soslowsky LJ. Intratendinous strain fields of the supraspinatus tendon: Effect of a surgically created articular-surface rotator cuff tear. J Shoulder Elbow Surg. 2002;11:562–9. doi: 10.1067/mse.2002.126767. [DOI] [PubMed] [Google Scholar]
- 10.Rudzki JR, Adler RS, Warren RF, Kadrmas WR, Verma N, Pearle AD, et al. Contrast-enhanced ultrasound characterization of the vascularity of the rotator cuff tendon: Age- and activity-related changes in the intact asymptomatic rotator cuff. J Shoulder Elbow Surg. 2008;17:S96–100. doi: 10.1016/j.jse.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Lomas G, Kippe MA, Brown GD, Gardner TR, Ding A, Levine WN, et al. In situ transtendon repair outperforms tear completion and repair for partial articular-sided supraspinatus tendon tears. J Shoulder Elbow Surg. 2008;17:722–8. doi: 10.1016/j.jse.2008.01.148. [DOI] [PubMed] [Google Scholar]
- 12.Borbas P, Hoy G. Surgical treatment options for partial rotator cuff tears: A review of the literature. Int J Orthop. 2019;6:1032–8. [Google Scholar]
- 13.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708–16. [PubMed] [Google Scholar]
- 14.Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial-thickness rotator cuff tear: Is acromioplasty without repair sufficient? Am J Sports Med. 2002;30:257–60. doi: 10.1177/03635465020300021801. [DOI] [PubMed] [Google Scholar]
- 15.Deutsch A. Arthroscopic repair of partial-thickness tears of the rotator cuff. J Shoulder Elbow Surg. 2007;16:193–201. doi: 10.1016/j.jse.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Porat S, Nottage WM, Fouse MN. Repair of partial thickness rotator cuff tears: A retrospective review with minimum two-year follow-up. J Shoulder Elbow Surg. 2008;17:729–31. doi: 10.1016/j.jse.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 17.Fukuda H, Hamada K, Nakajima T, Yamada N, Tomonaga A, Goto M. Partial-thickness tears of the rotator cuff. A clinicopathological review based on 66 surgically verified cases. Int Orthop. 1996;20:257–65. doi: 10.1007/s002640050075. [DOI] [PubMed] [Google Scholar]
- 18.Park JY, Yoo MJ, Kim MH. Comparison of surgical outcome between bursal and articular partial thickness rotator cuff tears. Orthopedics. 2003;26:387–90. doi: 10.3928/0147-7447-20030401-16. [DOI] [PubMed] [Google Scholar]
- 19.Liem D, Alci S, Dedy N, Steinbeck J, Marquardt B, Möllenhoff G. Clinical and structural results of partial supraspinatus tears treated by subacromial decompression without repair. Knee Surg Sports Traumatol Arthrosc. 2008;16:967–72. doi: 10.1007/s00167-008-0580-4. [DOI] [PubMed] [Google Scholar]
- 20.Jain NB, Ayers GD, Koudelková H, Archer KR, Dickinson R, Richardson B, et al. Operative vs nonoperative treatment for atraumatic rotator cuff tears: A trial protocol for the arthroscopic rotator cuff pragmatic randomized clinical trial. JAMA Netw Open. 2019;2:e199050. doi: 10.1001/jamanetworkopen.2019.9050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reynolds SB, Dugas JR, Cain EL, McMichael CS, Andrews JR. Debridement of small partial-thickness rotator cuff tears in elite overhead throwers. Clin Orthop Relat Res. 2008;466:614–21. doi: 10.1007/s11999-007-0107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrews JR, Broussard TS, Carson WG. Arthroscopy of the shoulder in the management of partial tears of the rotator cuff: A preliminary report. Arthroscopy. 1985;1:117–22. doi: 10.1016/s0749-8063(85)80041-4. [DOI] [PubMed] [Google Scholar]
- 23.Weber SC. Arthroscopic debridement and acromioplasty versus mini-open repair in the treatment of significant partial-thickness rotator cuff tears. Arthroscopy. 1999;15:126–31. doi: 10.1053/ar.1999.v15.0150121. [DOI] [PubMed] [Google Scholar]
- 24.Ide J, Takagi K. Early and long-term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg. 2004;13:174–9. doi: 10.1016/j.jse.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Kartus J, Kartus C, Rostgard-Christensen L, Sernert N, Read J, Perko M. Long-term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy. 2006;22:44–9. doi: 10.1016/j.arthro.2005.07.027. [DOI] [PubMed] [Google Scholar]
- 26.Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K, et al. Tendon integrity and functional outcome after arthroscopic repair of high-grade partialthickness supraspinatus tears. J Bone Joint Surg Am. 2009;91:1055–62. doi: 10.2106/JBJS.G.00118. [DOI] [PubMed] [Google Scholar]
- 27.Ellman H. Arthroscopic subacromial decompression: Analysis of one- to three-year results. Arthroscopy. 1987;33:173–81. doi: 10.1016/s0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 28.Spangehl MJ, Hawkins RH, McCormack RG, Loomer RL. Arthroscopic versus open acromioplasty: A prospective, randomized, blinded study. J Shoulder Elb Surg. 2002;11:101–7. doi: 10.1067/mse.2002.120915. [DOI] [PubMed] [Google Scholar]
- 29.Singh C, Lam PH, Murrell GA. Is acromioplasty of benefit for rotator cuff repair? Techniques in Shoulder & Elbow Surgery. 2015;16:15–9. [Google Scholar]
- 30.Vitale MA, Arons RR, Hurwitz S, Ahmad CS, Levine WN. The rising incidence of acromioplasty. J Bone Jt Surg Am. 2010;92:1842–50. doi: 10.2106/JBJS.I.01003. [DOI] [PubMed] [Google Scholar]
- 31.Yu E, Cil A, Harmsen WS, Schleck C, Sperling JW, Cofield RH. Arthroscopy and the dramatic increase in frequency of anterior acromioplasty from 1980 to 2005: An epidemiologic study. Arthroscopy. 2010;26:S142–7. doi: 10.1016/j.arthro.2010.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gill TJ, McIrvin E, Kocher MS, Homa K, Mair SD, Hawkins RJ. The relative importance of acromial morphology and age with respect to rotator cuff pathology. J Shoulder Elb Surg. 2002;11:327–30. doi: 10.1067/mse.2002.124425. [DOI] [PubMed] [Google Scholar]
- 33.Shin SJ, Oh JH, Chung SW, Song MH. The efficacy of acromioplasty in the arthroscopic repair of small- to mediumsized rotator cuff tears without acromial spur: Prospective comparative study. Arthroscopy. 2012;28:628–35. doi: 10.1016/j.arthro.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Tibone JE, Jobe FW, Kerlan RK, Carter VS, Shields CL, Lombardo SJ, et al. Shoulder impingement syndrome in athletes treated by an anterior acromioplasty. Clin Orthop. 1985;198:134–40. [PubMed] [Google Scholar]
- 35.Lee TQ, Black AD, Tibone JE, McMahon PJ. Release of the coracoacromial ligament can lead to glenohumeral laxity: A biomechanical study. J Shoulder Elb Surg. 2001;10:68–72. doi: 10.1067/mse.2001.111138. [DOI] [PubMed] [Google Scholar]
- 36.Scheibel M, Lichtenberg S, Habermeyer P. Reversed arthroscopic subacromial decompression for massive rotator cuff tears. J Shoulder Elb Surg. 2004;13:272–8. doi: 10.1016/j.jse.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 37.Su WR, Budoff JE, Luo ZP. The effect of coracoacromial ligament excision and acromioplasty on superior and anterosuperior glenohumeral stability. Arthrosc J Arthrosc Relat Surg Off publ Arthrosc Assoc North Am Int Arthrosc Assoc. 2009;25:13–8. doi: 10.1016/j.arthro.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Chahal J, Mall N, MacDonald PB, Van Thiel G, Cole BJ, Romeo AA, et al. The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: A systematic review and meta-analysis. Arthroscopy. 2012;28:720–7. doi: 10.1016/j.arthro.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 39.McFarland EG, Maffulli N, Del Buono A, Murrell GA, Garzon- Muvdi J, Petersen SA. Impingement is not impingement: The case for calling it ‘’rotator cuff disease’’. Muscles Ligaments Tendons J. 2013;3:196–200. [PMC free article] [PubMed] [Google Scholar]
- 40.Papadonikolakis A, McKenna M, Warme W, Martin BI, Matsen FA., III Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Jt Surg Am. 2011;93:1827–32. doi: 10.2106/JBJS.J.01748. [DOI] [PubMed] [Google Scholar]
- 41.Mehta S, Gimbel JA, Soslowsky LJ. Etiologic and pathogenic factors for rotator cuff tendinopathy. Clin Sports Med. 2003;22:791–812. doi: 10.1016/s0278-5919(03)00012-7. [DOI] [PubMed] [Google Scholar]
- 42.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990:64–73. [PubMed] [Google Scholar]
- 43.Itoi E, Tabata S. Incomplete rotator cuff tears: Results of operative treatment. Clin Orthop Relat Res. 1992:128–35. [PubMed] [Google Scholar]
- 44.Neer CS II. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 45.Hyvönen P, Lohi S, Jalovaara P. Open acromioplasty does not prevent the progression of an impingement syndrome to a tear. J Bone Joint Surg [Br] 1998;80-B:813–6. doi: 10.1302/0301-620x.80b5.8533. [DOI] [PubMed] [Google Scholar]
- 46.Fukuda H, Craig EV, Yamanaka K. Surgical treatment of incomplete thickness tears of rotator cuff: Long-term follow-up. Orthop Trans. 1987;11:237–8. [Google Scholar]
- 47.Tabata S, Sano H, Itoi E. Treatment of partial-thickness tears of the rotator cuff. In: Wu JJ, Fukuda H, Shih LY, Chan KM, Soong TH, editors. Shoulder Surgery: The Asian Perspective. Taipei, Taiwan: Orthopaedic Department Veterans General Hospital; 1995. pp. 193–5. [Google Scholar]
- 48.Fukuda H. Partial-thickness rotator cuff tears: A modern view on Codman's classic. J Shoulder Elbow Surg. 2000;9:163–8. [PubMed] [Google Scholar]
- 49.Pedowitz RA, Yamaguchi K, Ahmad CS, Burks RT, Flatow EL, Green A, et al. Optimizing the management of rotator cuff problems. J Am Acad Orthop Surg. 2011;19:368–79. doi: 10.5435/00124635-201106000-00007. [DOI] [PubMed] [Google Scholar]
- 50.Gartsman GM, O’Connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: A prospective, randomized study of one-year outcomes. J Shoulder Elb Surg. 2004;13:424–6. doi: 10.1016/j.jse.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 51.Milano G, Grasso A, Salvatore M, Zarelli D, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with and without subacromial decompression: A prospective randomized study. Arthroscopy. 2007;23:81–8. doi: 10.1016/j.arthro.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 52.Karjalainen TV, Jain NB, Page CM, Lähdeoja TA, Johnston RV, Salamh P, et al. Subacromial decompression surgery for rotator cuff disease? Cochrane Database Syst Rev. 2019:CD005619. doi: 10.1002/14651858.CD005619.pub3. doi: 10.1002/14651858.CD005619.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Benson RT, McDonnell SM, Rees JL, Athanasou NA, Carr AJ. The morphological and immunocytochemical features of impingement syndrome and partial thickness rotator-cuff tear in relation to outcome after subacromial decompression. J Bone Joint Surg Br. 2009;91:119–23. doi: 10.1302/0301-620X.91B1.21058. [DOI] [PubMed] [Google Scholar]
- 54.Familiari F, Gonzalez-Zapata A, Iannò B, Galasso O, Gasparini G, McFarland EG. Is acromioplasty necessary in the setting of full-thickness rotator cuff tears? A systematic review. J Orthop Traumatol. 2015;16:167–74. doi: 10.1007/s10195-015-0353-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


