Abstract
Caregivers providing care to chronically ill family members at home are potentially at risk for caregiver burden and declining physical and psychological health. This study aims to understand how family caregivers’ mental health and caregiver burden affects physical health simultaneously, controlling for factors such as age, education level, caring hours per day, and emotional, functional, and physical support systems used by caregivers. We recruited 388 caregivers from Kaohsiung and Pingtong region in Taiwan. Caregivers had to be 18 years or older and spend most of their time taking care of an ill family member at home. Mental health was assessed by the 12-item Chinese Health Questionnaire (CHQ-12) and burden was measured using a modified scale for caregiver's burden. Health status was assessed by self-perceived health (SPH), illness symptoms and the number of diagnosed chronic diseases. A high number of hours per day of caregiving was associated with low emotional support and SPH, poor mental health and high burden. Higher emotional support was associated with better mental health and fewer illness symptoms. Higher physical support was associated with poorer mental health, higher burden, a greater number of illness symptoms and chronic diseases, and a lower SPH score. Hours per day of caregiving, and use of emotional, functional, and physical support were associated with mental health, and the hours per day of caregiving and use of physical support were predictors of burden. Mental health and burden were significantly associated with caregivers’ health problems simultaneously. Our results show the important influence of mental health on caregivers’ physical health. Interventions for caregivers need to target health in a holistic way.
Keywords: Family caregivers, Cargiver burden, Mental health, Physical health
1. Introduction
Caregivers who provide care to a chronically ill family member at home are potentially at risk for caregiver burden and declining physical and mental health. Family caregivers of older people with disabilities report burden and stress as a consequence of caregiving, which in turn contributes to psychiatric morbidity (Schulz and Beach, 1999). Both caregiver's health and the recipient's health have a strong influence on caregiver burden (Bull, 1990). Caregivers often neglect their own health and hide information about their health problems (Ward-Griffin and McKeever, 2000). For family caregivers, burden comes from many different sources. Researchers have tried to investigate caregiver burden in order to design programs to ease burden.
1.1. Impacts of caregiving
Many studies have investigated how a caregiver's burden affects different aspects of his or her life (Pickett et al., 1997, Song et al., 1997, Happe and Berger, 2002, Morimoto et al., 2003). In these studies, burden was a mediator of other outcome variables and was shown to be strongly related to sleep disturbances (Happe and Berger, 2002) and depressive symptoms in caregivers (Song et al., 1997). Burden is negatively related to health-related quality of life, particularly mental health (Morimoto et al., 2003). Furthermore, burden is negatively associated with caregivers’ positive appraisal of their relationships with their ill family members (Pickett et al., 1997). Efforts have been made to reduce the burden of care in carers (Marriott et al., 2000).
Caring for ill family members can have negative impacts on caregivers’ mental health (Schulz et al., 1990). One study found that dementia patients’ caregivers appeared more vulnerable to depression as a consequence of their experience (Waite et al., 2004). Another study observed that caregivers providing care to a family member with dementia at home had higher levels of depression than those whose family members were in an institution (Grunfeld et al., 1997). White et al. (2003) found that caregivers of people who had suffered a stroke had lower mental-health-related quality of life compared to their counterparts who were not caregivers. Another study used the same questionnaire (SF-36) to measure caregivers’ health-related quality of life, and found that caregivers of people with cerebrovascular disease or diabetes had significantly negative mental-health-related quality of life (Li et al., 2004).
The physical consequences of caregiving have received less attention than psychiatric outcomes. One study indicated that caregivers often experience several physical problems, including back injuries, arthritis, high blood pressure, gastric ulcers, and headaches (Sawatzky and Fowler-Kerry, 2003). Although these physical problems may not be directly caused by caregiving responsibilities, they are likely aggravated by them. Other research has found that the physical health of caregivers of long-term patients declined after the patients were discharged from hospital (Douglas and Daly, 2003). These studies indicate that caring for an ill family member at home is negatively related to physical health.
The causal relationship between health and caregiving burden is unclear, that is, whether poor health leads to burden or whether caregiving burden has a negative effect on health remains to be clarified (Nijboer et al., 1998). Caregiving burden, in terms of physical strain, has been found to predict caregivers’ perceived health (Beach et al., 2000). On the other hand, Stommel et al. (1999) reported that mental health, in terms of depression, could predict burden. According to Bull (1990), caregiver's health is a factor that contributes to burden.
1.2. Social support and burden
Social support may have a buffering effect on caregiver burden. One study found that social support was negatively associated with caregiver's burden; that is, caregivers who obtained more social support reported less burden (Song et al., 1997). Strong relationships between the availability of support systems and caregiver distress have been reported (Pohl et al., 1994, Li et al., 1997, Sander et al., 1997, Edwards and Scheetz, 2002). Instrumental, emotional, and informational support are the most commonly cited functional dimensions of social support systems (Chak, 1996). Thompson et al. (1993), who studied the relationship between the functions of social support and caregiver burden, reported that not all functions were equally associated with caregiver burden. In their sample, they found that instrumental and emotional support were ineffective in reducing caregiver burden.
The Taiwanese government has established long-term care systems in response to the growth of the elderly population. Three major types of care systems are provided: institutions, community based care, and home care. Both the Department of Social Affairs, Ministry of Interior, and the Department of Health, Executive Yuan supervise these long-term care systems. Home care is partly covered by the National Health Insurance, which pays for two home nursing visits per month. Most of these visits are to care for people with physical disabilities. There is a separate independent system for caring for people with mental illness.
Previous studies examined the relationships between burden and mental health or physical health separately. The objective of this study was to better understand the needs of family caregivers who were covered by the National Health Insurance and, specifically, to clarify the factors associated with their mental and physical health simultaneously. By doing this, we hope to find ways to provide useful help to caregivers of disabled family members, particularly as demographic parameters shift toward a larger population of older people in Taiwan.
2. Subjects and methods
2.1. Sample
There are 46 home-care agencies providing services to clients in the Kaohsiung and Pingtong areas in Southern Taiwan. All of them are certified agencies and are covered by the National Health Insurance. However, only clients with a Barthel score less than 60 are eligible for the home care services provided by the government, which means that the dependency levels of clients are high. After excluding 12 agencies which care for less than 20 clients or that were converted to care for severe acute respiratory syndrome (SARS) patients instead of home-care clients, 16 home-care agencies serving 588 cases were eligible. We included only those individuals who were 18 years or older and spent most of their time taking care of at least one ill family member at home. Among the eligible cases, 50 were institutionalized, 96 refused or did not complete the interview, and 54 were cared for by hired carers and their families could not be reached. This resulted in a total of 388 family caregivers (∼66%) of clients served by these agencies, recruited between 20 June 2003 and 30 November 2003. All the clients were physically ill. Over half of them were unconscious (Chiou et al., 2005), with 84.7% being totally dependent. A considerable number of care receivers were suffering from cerebrovascular disease (66.8%), followed by diabetes (28.6%) and cardiovascular disease (19.8%) (Chiou et al., 2005). Written consent was obtained from each participating caregiver.
2.2. Measures
The CHQ-12 was used to measure mental health. Respondents were asked to rate aspects of their psychosocial health on a four-point scale, which ranged from 1 (not at all) to 4 (more than usual). The items included headaches, heart palpitations, chest pain or tightening, trembling or pins and needles, sleeplessness, nervousness, and hopelessness. A higher score represented a more severe psychosocial impairment. The CHQ-12 has been tested among the elderly in the community with acceptable validity. The Relative Operating Characteristic (ROC) curve was used to determine the optimal cut-off point. At the optimal cut-off point of two-thirds, the CHQ-12 had a sensitivity of 79.7% and a specificity of 83.6% (Chen et al., 2000). This study had a reasonable reliability (Cronbach's α = 0.80).
Caregivers were asked to rate their overall health on a three-item scale, developed on the basis of the General Health Perceptions Subscale of the SF-36 Health Status Scale (Ware et al., 1994). Ratings ranged from 1 (bad) to 3 (good), with a higher score representing better SPH. The items have been shown to have a reasonable reliability in Taiwan (Cronbach's α = 0.68) (Chen, 2004), and good reliability was achieved in this study (Cronbach's α = 0.74).
Participants’ illness symptoms were assessed using a list of physical and psychological aliments that may have arisen during their caregiving duties. The seven symptoms were headache, dizziness, joint pains, insomnia, backache, stomach discomfort, and depressed mood. The presence of diagnosed chronic diseases such as diabetes, hypertension, cardiovascular disease, and gout was also assessed. We developed this measure specifically for this study.
A modified scale for caregiver's burden was used in this study (Song, 2002); the subscale for stigma was not used because it did not apply to the research objectives. The 16-item scale measured the caregiver's feelings towards the ill family member based on the dimensions of family disruption and strain, and patient dependency. Respondents scored each item on a five-point scale from 0 (never) to 4 (always true), with higher scores indicating heavier burden. The original scale achieved an acceptable reliability rating (Cronbach's α = 0.93). The reliability of the modified scale used in this study was also good (Cronbach's α = 0.84).
Data regarding demographic characteristics, employment status, hours per day devoted to caregiving, and whether care and expenses were being shared were collected. Participants rated their use of emotional support systems (face-to-face counseling, telephone counseling, caregiver groups, or other support groups) on a three-point scale. Higher scores represented more frequent use of these support systems. Similarly, the use of functional support systems (home nursing aids, in home respite care, in institution respite care, in home services, rehabilitation, day-care providers, and temporary care) was assessed. Physical support included the use of transportation support, emergency help, and telephone consultation. Together, these items were analyzed with regard to their effects on caregivers’ mental health and burden scores as well as their physical health. The recruitment method and measures have been reported elsewhere (Chiou et al., 2005).
2.3. Data analysis
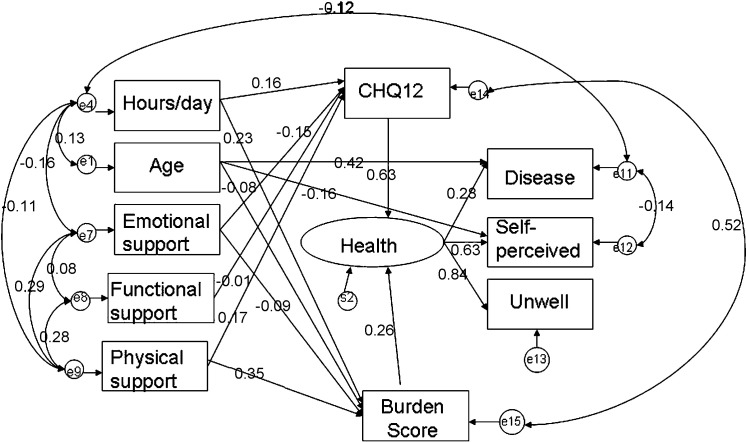
Descriptive statistics were used to examine demographic characteristics, caregivers’ mental and physical health, and caregiver burden. Analyses were performed using SAS version 9.0 (SAS Institute, Inc., Cary, NC, USA). We then used a path diagram to clarify relationships among the factors associated with caregiver's mental health, burden, and physical health. A structural equation model was a valid measure for investigating the causal relationships among the variables, because: (1) several variables were correlated; (2) physical health was measured by the combination of three items: the number of diagnosed chronic diseases, number of illness symptoms, and SPH; and (3) when the correlated measurement errors were taken into account, the model was able to specify the relationships among the observed variables and health status (Lin and Wan, 2001).
We hypothesized that mental health (measured by CHQ-12) and burden (measured by the burden scale) would affect caregiver's health, and that caring hours per day, age, and use of support systems would affect the mental health and burden scores. The correlation among variables were examined. We then constructed a model of the latent variable physical health, which was measured by the number of diagnosed chronic diseases, number of illness symptoms, and SPH. Next, we constructed the structural equation model to examine the relationships among the variables. Individual characteristics such as age, education level, working status, and the use of emotional, functional, and/or physical support were considered as exogenous variables that had effects on the mental health score (represented by CHQ-12) and burden score. Finally, we examined how the correlated variables of mental health and burden scores affected the physical health of caregivers.
3. Results
Demographic, health, and burden characteristics of caregivers are presented in Table 1 . Half of the participants (N = 220, 56.7%) had less than or equal to 9 years of education. About one-third (N = 113, 29.1%) finished senior high school and 14.1% (N = 55) had college or higher education. The mean ages of care receivers were 72.6 ± 12.8 and 69.6 ± 16.4 years for males and females, respectively. Most of the caregivers were females (72%). Over half of male caregivers were sons of the care receivers. One-third of female caregivers were daughters-in-law of the care receivers, and another 30% were spouses (data not shown).
Table 1.
Demographic, health, and burden characteristics of caregivers, mean ± S.D.
| Variable | Total | Male | Female |
|---|---|---|---|
| Number | 388 | 108 | 280 |
| Age (year) | 50.8 ± 13.8 | 55.6 ± 14.9 | 48.9 ± 12.9 |
| Hours per day | 12.5 ± 7.6 | 11.9 ± 7.6 | 12.8 ± 7.6 |
| Emotional supporta (sum) | 4.8 ± 1.1 | 4.9 ± 1.1 | 4.8 ± 1.1 |
| Functional supportb (sum) | 6.1 ± 0.5 | 6.1 ± 0.4 | 6.1 ± 0.5 |
| Physical supportc (sum) | 3.3 ± 0.6 | 3.3 ± 0.6 | 3.3 ± 0.7 |
| Mental health score (CHQ-12) | 4.3 ± 2.7 | 3.8 ± 2.3 | 4.6 ± 2.8 |
| Burden score (0–49) | 23.9 ± 9.3 | 23.6 ± 9.7 | 24.0 ± 9.2 |
| Number of illness symptoms (0–7) | 2.0 ± 1.7 | 1.6 ± 1.5 | 2.1 ± 1.7 |
| Number of chronic diseases (0–4) | 0.5 ± 0.8 | 0.6 ± 0.8 | 0.5 ± 0.8 |
| Sum of SPH (3–9) | 5.2 ± 1.3 | 5.5 ± 1.0 | 5.1 ± 1.4 |
Including face-to-face counseling, telephone counseling, caregiver groups, or other support groups. Scores ranged 4–8.
Including, e.g., day-care and home-care providers. Scores ranged 6–11.
Including transportation, emergency support, and telephone consultation. Scores ranged 3–7.
The correlations among the variables are presented in Table 2 . Age was positively related to the number of chronic diseases and negatively related to SPH. That meant as age increased, number of chronic diseases increased, and SPH worsen. Number of hours per day devoted to caregiving was negatively related to emotional support and SPH but positively related to mental health and burden scores. As caregivers devoted more time in caring, they had less time to use emotional support. Their SPH got worse, and mental health declined. Emotional support was positively associated with functional support but negatively related to mental health score and number of illness symptoms. Physical support was positively associated with mental health and burden scores, number of illness symptoms, and number of chronic diseases but negatively associated with SPH. Similar patterns were found for mental health and burden scores. Even though several correlations reached statistical significance, most of them were small in magnitude with coefficients less than 0.5. The exceptions were the correlations between mental health score and burden score, mental health score and number of illness symptoms, and burden score and number of illness symptoms. This is also the case for the correlation between number of illness symptoms and SPH.
Table 2.
Pearson correlations among factors, burden scores, mental and physical health.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 1.000 | |||||||||
| 2. Hours per day | 0.129a | 1.000 | ||||||||
| 3. Emotional supportb (sum) | −0.040 | −0.159a | 1.000 | |||||||
| 4. Functional supportb (sum) | 0.009 | 0.044 | 0.068 | 1.000 | ||||||
| 5. Physical supportb (sum) | 0.060 | −0.088 | 0.284† | 0.270a | 1.000 | |||||
| 6. CHQ-12 | 0.024 | 0.168a | −0.129† | 0.023 | 0.106a | 1.000 | ||||
| 7. Burden score (0–49) | −0.034 | 0.198a | −0.024 | 0.086 | 0.295a | 0.545a | 1.000 | |||
| 8. No of illness symptoms | 0.031 | 0.172a | −0.113a | 0.006 | 0.111a | 0.639a | 0.516a | 1.000 | ||
| 9. No of chronic diseases | 0.423a | 0.040 | −0.010 | −0.070 | 0.121a | 0.238a | 0.104a | 0.254a | 1.000 | |
| Sum of SPH | −0.174a | −0.213a | 0.078 | 0.044 | −0.103a | −0.511a | −0.370a | −0.541a | −0.340a | 1.000 |
Significantly different from zero (p < 0.05).
See footnotes to Table 1 for details.
The standardized regression weights for the significant variables are listed in Table 3 , and Fig. 1 illustrates the structural equation model for the physical health of caregivers. The model indicated that hours per day of caregiving, and the use of emotional, functional, and physical support systems were explanatory variables for mental health; and the hours per day of caregiving and use of physical support were explanatory variables for burden. The health measures were significant predictors of actual health problems. The negative coefficient between health problems and SPH was due to the scoring of SPH status, with a higher score representing better health. Mental health and burden were significantly associated with health problems.
Table 3.
Standardized regression weights for significant variables.
| Item | Variable | Estimate |
|---|---|---|
| Regression | ||
| CHQ-12 | Hours/day | 0.159* |
| Emotional support | −0.150* | |
| Functional support | −0.014 | |
| Physical support | 0.166 | |
| Burden | Age | −0.082* |
| Hours/day | 0.225* | |
| Emotional support | −0.089 | |
| Physical support | 0.346* | |
| Health | Burden | 0.258* |
| CHQ-12 | 0.631* | |
| Number of diseases | Health | 0.282* |
| Age | 0.418* | |
| SPH | Health | −0.626* |
| Age | −0.162* | |
| Unwell | Health | 0.835* |
| Latent variable | Indicators | Estimate |
|---|---|---|
| Health | No. of chronic diseases | 0.277* |
| No. of illness symptoms | 0.830* | |
| SPH | −0.674* |
| Model fitting | Statistics | p-Value or criteria |
|---|---|---|
| Chi-square | 20.353 (d.f. = 21) | 0.969 |
| Goodness of fit (GFI) | 0.990 | 0–1 for bad–good |
| Parsimonious normed fit index (PNFI) | 0.455 | >0.5 |
Significant at α = 0.05.
Fig. 1.
Structural equation model for the physical health of caregivers.
4. Discussion
Although predictors of caregiver mental health or burden have been well studied separately, the relationships between these two factors and the physical health of caregivers have rarely been studied simultaneously. This is one of the very few studies that has used structural equation modeling to examine relationships among caregivers’ burden, mental health, and physical health. We found that mental health had a stronger effect on physical health than did burden (standardized coefficients: 0.63 vs. 0.26). Our results are consistent with those of Grov et al. (2006), who used a path model to identify variables influencing caregivers’ burden. They reported significant associations between caregivers’ physical health and levels of anxiety and depression, but were unable to establish a direct association between physical health and burden.
The items on the CHQ-12 used to assess mental health included headaches, heart palpitations, chest pain or tightening, trembling or pins and needles, sleeplessness, nervousness, and hopelessness. These items were significantly related to the number of hours per day of caregiving and the use of emotional support, which included face-to-face interview, telephone counseling, caregiver groups, or other support groups. Our results are in line with the findings of Savard et al. (2006), who reported that caregivers receiving information, advice, or emotional support were more likely to be highly satisfied. Although we found that the use of functional support systems also decreased mental stress, the effect was not statistically significant. This may be due to a low level of awareness of the existence of these functional support systems or how to apply for them. Thus, based on our findings, the Taiwanese public health community and social service providers should strengthen and promote existing support systems as well as design new systems to ease the mental stress of family caregivers. The social workers or public health nurses should reach out the caregivers in the communities to help them use the existing or newly developed support systems.
The burden score measured caregivers’ feelings of not being able to provide good and sufficient care; how much caregiving interfered with daily life, leisure activities, social life, and marriage; as well as feelings of worry and irritation. Our study revealed that burden was significantly predicted by the number of hours per day devoted to caregiving and the use of physical support, suggesting that emotional and functional support were unable to alleviate these feelings of burden, as measured in our study. On the other hand, age was negatively related to burden score. It was possible that the older caregivers were more traditional people and accepted the role for caregiving. But as age increased the number of diseases increased and the self-perceived worsen. That implied that the older caregivers’ health condition was decelerating even though they did not think the burden was heavy.
The average duration of caregiving was around 194.5 months (16.2 years). The care receivers were around 70 years old. In Chinese society, most elderly people live with their children, especially their sons. Caring for ill family members can become a burden on the sons’ families, particularly on the wives. As women have become more independent in Taiwan, it has become very popular to hire foreign domestic helpers. The mental health and burden of these foreign helpers will be another important issue to study in the future.
5. Conclusions
In conclusion, this is one of the very few studies to use structural equation modeling to examine relationships among caregivers’ burden, mental health, and physical health simultaneously. Our results revealed the important influence of mental health on caregivers’ physical health. Intervention programs for caregivers need to target health in a holistic way.
Conflict of interest statement
None.
Acknowledgements
Appreciation should go to the participants and the home-care nurses who helped recruit the participants. Part of this study was sponsored by a grant from the Taiwan Department of Health (DOH92-TD-1026).
References
- Beach S.R., Schulz R., Yee J.L., Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from caregiver health effects study. Psychol. Aging. 2000;15:259–271. doi: 10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- Bull M.J. Factors influencing family caregiver burden and health. West. J. Nurs. Res. 1990;12:758–776. doi: 10.1177/019394599001200605. [DOI] [PubMed] [Google Scholar]
- Chak A. Conceptualizing social support: a micro or macro perspective. Psychologia. 1996;39:74–83. [Google Scholar]
- Chen C.S., Tsang H.Y., Chong M.Y., Tang T.C. Validation of the Chinese Health Questionnaire (CHQ-12) in community elders. Kaohsiung J. Med. Sci. 2000;16:559–565. [PubMed] [Google Scholar]
- Chen, L.J., 2004. The Relationship Between Hardiness, Health Status, and Quality of Life Among Primary Caregivers Involved in Home Care. Master Thesis. Kaohsiung Medical University, Taiwan (in Chinese).
- Chiou C.J., Chen I.-P., Wang H.-H. The health status of family caregivers in Taiwan: an analysis of gender differences. Int. J. Geriatr. Psychiatry. 2005;20:821–826. doi: 10.1002/gps.1364. [DOI] [PubMed] [Google Scholar]
- Douglas S.L., Daly B.J. Caregivers of long-term ventilator patients: physical and psychological outcomes. Chest. 2003;123:1073–1081. doi: 10.1378/chest.123.4.1073. [DOI] [PubMed] [Google Scholar]
- Edwards N.E., Scheetz P.S. Predictors of burden for caregivers of patients with Parkinson's disease. J. Neurosci. Nurs. 2002;34:184–190. doi: 10.1097/01376517-200208000-00003. [DOI] [PubMed] [Google Scholar]
- Grov E.K., Fosså S.D., Sørebø Ø., Dahl A.A. Primary caregivers of cancer patients in the palliative phase: a path analysis of variables influencing their burden. Soc. Sci. Med. 2006;63:2429–2439. doi: 10.1016/j.socscimed.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Grunfeld E., Glossop R., McDowell I., Danbrook C. Caring for elderly people at home: the consequences to caregivers. Can. Med. Assoc. J. 1997;157:1101–1105. [PMC free article] [PubMed] [Google Scholar]
- Happe S., Berger K. The association between caregiver burden and sleep disturbances in partners of patients with Parkinson's disease. Age Aging. 2002;31:349–354. doi: 10.1093/ageing/31.5.349. [DOI] [PubMed] [Google Scholar]
- Li L.W., Seltzer M.M., Greenberg J.S. Social support and depressive symptoms: differential patterns in wife and daughter caregivers. J. Gerontol. B: Psychol. Sci. Soc. Sci. 1997;52:S200–S211. doi: 10.1093/geronb/52b.4.s200. [DOI] [PubMed] [Google Scholar]
- Li T.-C., Lee Y.-D., Lin C.-C., Amidon R.L. Quality of life of primary caregivers of elderly with cerebrovascular disease or diabetes hospitalized for acute care: assessment of well-being and functioning using the SF-36 health questionnaire. Qual. Life Res. 2004;13:1081–1088. doi: 10.1023/B:QURE.0000031349.25124.d6. [DOI] [PubMed] [Google Scholar]
- Lin Y.J., Wan T.T.H. Effect of organizational and environmental factors on service differentiation strategy of integrated healthcare networks. Health Serv. Manage. Res. 2001;14:18–26. doi: 10.1258/0951484011912492. [DOI] [PubMed] [Google Scholar]
- Marriott A., Donaldson C., Tarrier N., Burns A. Effectiveness of cognitive-behavioral family intervention in reducing the burden of care in carers of patients with Alzheimer's disease. Br. J. Psychiatry. 2000;176:557–562. doi: 10.1192/bjp.176.6.557. [DOI] [PubMed] [Google Scholar]
- Morimoto T., Schreiner A.S., Asano H. Caregiver burden and health-related quality of life among Japanese stroke caregivers. Age Ageing. 2003;32:218–223. doi: 10.1093/ageing/32.2.218. [DOI] [PubMed] [Google Scholar]
- Nijboer C., Tempelaar R., Sanderman R., Triemstra M., Spruijt R.J., Van den Bos G.A. Cancer and caregiving: the impact on the caregiver's health. Psychooncology. 1998;7:3–13. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<3::AID-PON320>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Pickett S.A., Cook J.A., Cohler J., Solomon M.L. Positive parent/adult child relationships: impact of severe mental illness and caregiving burden. Am. J. Orthopsychiatry. 1997;67:220–230. doi: 10.1037/h0080225. [DOI] [PubMed] [Google Scholar]
- Pohl J.M., Given C.W., Collins C.E., Given B.A. Caregiving in daughters and daughters-in-law caring for disabled aging parents. Health Care for Women Intern. 1994;15:385–395. doi: 10.1080/07399339409516131. [DOI] [PubMed] [Google Scholar]
- Sander A.M., High W.M.J., Hannay H.J., Sherer M. Predictors of psycho-logical health in caregivers of patients with closed head injury. Brain Injury. 1997;11:235–249. doi: 10.1080/026990597123548. [DOI] [PubMed] [Google Scholar]
- Savard J., Lebel P., Béland F., Bergman H. Caregiver satisfaction with support services. J. Aging Health. 2006;18:3–27. doi: 10.1177/0898264305280979. [DOI] [PubMed] [Google Scholar]
- Sawatzky J.E., Fowler-Kerry S. Impact of caregiving: listening to the voice of informal caregivers. J. Psychiatr. Ment. Health Nurs. 2003;10:277–286. doi: 10.1046/j.1365-2850.2003.00601.x. [DOI] [PubMed] [Google Scholar]
- Schulz R., Vistainer P., Williamson G.M. Psychiatric and physical morbidity effects of caregiving. J. Gerontol. B: Psychol. Sci. Soc. Sci. 1990;45:P181–P191. doi: 10.1093/geronj/45.5.p181. [DOI] [PubMed] [Google Scholar]
- Schulz R., Beach S.R. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. J. Am. Med. Assoc. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Song L., Biegel D.E., Milligan S.E. Predictors of depressive symptomatology among lower social class caregivers of persons with chronic mental illness. Commun. Mental Health J. 1997;33:269–286. doi: 10.1023/a:1025090906696. [DOI] [PubMed] [Google Scholar]
- Song L.Y. The development and validation of a caregiver burden scale- a focus on practice applicability. Soc. Policy Soc. Work. 2002;6:61–100. (in Chinese, with English abstract) [Google Scholar]
- Stommel M., Given C.W., Given B. Depression as an overriding variable explaining caregiver burdens. J. Aging Health. 1999;2:80–103. [Google Scholar]
- Thompson E.H., Futterman A.M., Gallagher-Thompson D., Rose J.M., Lovett S.B. Social support and caregiving burden in family caregivers of frail elders. J. Gerontol. B: Psychol. Sci. Soc. Sci. 1993;28:S245–S254. doi: 10.1093/geronj/48.5.s245. [DOI] [PubMed] [Google Scholar]
- Waite A., Bebbington P., Skelton-Robinson M., Orrell M. Social factors and depression in caregivers of people with dementia. Int. J. Geriatric Psychiatry. 2004;19:582–587. doi: 10.1002/gps.1136. [DOI] [PubMed] [Google Scholar]
- Ward-Griffin C., McKeever P. Relationships between nurses and family caregivers: partners in care? Adv. Nurs. Sci. 2000;22:89–103. doi: 10.1097/00012272-200003000-00008. [DOI] [PubMed] [Google Scholar]
- Ware J.E., Gandek B., The International Quality of Life Assessment Project Group The SF-36 health survey: development and use in mental health research and IQOLA project. Int. J. Ment. Health. 1994;23:49–73. [Google Scholar]
- White C.L., Mayo N., Hanley J.A.S., Wood-Dauphines S. Evolution of the caregiving experience in the initial 2 years following stroke. Res. Nurs. Health. 2003;26:177–189. doi: 10.1002/nur.10084. [DOI] [PubMed] [Google Scholar]