Abstract
Background
Randomized trials have shown that optimal adherence to antihypertensive agents could protect against cardiovascular diseases, but whether adherence reduces cardiovascular deaths in community settings has not been explored so fully. This study evaluates the association between antihypertensive adherence and cardiovascular (coronary heart disease and stroke) mortality in the primary care settings.
Methods
From a territory-wide database in Hong Kong, we included all patients who were prescribed their first-ever antihypertensive agents in the years between 2001 and 2005 from the public healthcare sector. All patients were followed up for five years, and assigned as having poor (Proportion of Days Covered [PDC] < 40%), intermediate (40–79%), and high (≥ 80%) adherence to antihypertensive agents. The association between antihypertensive adherence and cardiovascular mortality was evaluated by using the Cox proportional hazard models.
Results
From a total of 218,047 eligible patients, 3825 patients (1.75%) died of cardiovascular disease within five years after having received their first-ever antihypertensive agents. The proportions of patients having poor, intermediate, and high medication adherence were 32.9%, 12.1%, and 55.0%, respectively. Higher adherence levels at PDC 40%–79% (HR = 0.46, 95% C.I. 0.41–0.52, p < 0.001) and ≥ 80% (HR = 0.91, 95% C.I. 0.85–0.98, p = 0.012) were significantly less likely to be associated with mortality than the poor adherence (PDC0.040) group.
Conclusions
Better antihypertensive adherence was associated with lower cardiovascular mortality. This highlights the need to promote adherence through strategies which have been proved to be effective in clinical settings.
Keywords: Antihypertensive agents, Adherence, Cardiovascular mortality, Associated factors
1. Introduction
Antihypertensive pharmacotherapies are effective in reducing hypertension-induced complications, including death. In trial settings, reductions of blood pressure lowered the incidence of heart failure by 50%, stroke by 40–45%, and myocardial infarction by 20–25% [1], [2]. However, it is widely recognized that a large proportion of hypertensive patients do not take antihypertensive therapies as prescribed [3], and persistence with prescriptions decreased with time especially in the first year of treatment [4], [5], [6], [7]. Higher morbidity rates, mortality, hospitalization rates and healthcare costs have been attributed to poor medication adherence [8], [9], [10], [11].
A recent study conducted by Mazzaglia and colleagues [12], which included more than 18,800 newly diagnosed hypertensive patients, showed that higher antihypertensive adherence was associated with a significantly lower risk of acute cardiovascular events (hazard ratio [HR] 0.62, 95% C.I. 0.40–0.96). It shows that even among those who had not experienced any such events, maintenance of optimal antihypertensive adherence confers primary prevention to a substantial extent. An accompanying editorial by Chobanian [13] argued for the importance of investigating this in greater depth because suboptimal adherence is likely to be multi-factorial. One of the major determinants includes the patients' race and ethnicity, which in turn introduces cultural and attitudinal differences [14].
Owing to this ethnic heterogeneity, more data from patients of different ethnic groups is needed to further generalize the above findings in a global context. Thus far, the impact of antihypertensive persistence on cardiovascular mortality has not been adequately studied among patients in general non-experimental clinical settings nor more specifically in Chinese populations. Most studies on the impact of antihypertensive compliance on health outcomes have been conducted on higher-risk individuals or have used a cardiovascular (CVS) event alone as an outcome measure [15], [16], [17], [18]. Thus, to establish the effectiveness of adherence on primary prevention of CVS mortality an even larger cohort of hypertensive patients is needed. The clinical management system (CMS) in Hong Kong hospitals allows the opportunity for just such a study.
The objectives of this study were to test the a priori hypothesis that better medication adherence leads to lower mortality from coronary heart disease and stroke in a large Chinese population, based on a recent study showing that such a relationship exists on cardiovascular events among a Caucasian population [12].
2. Methods
2.1. Data source
A detailed description of a comprehensive, territorywide database in Hong Kong has been reported previously [19], [20], [21], [22], [23], [24], [25]. Briefly, the clinical management system consists of patients' demographic profiles, prescription details, and clinical information, including diagnoses in the forms of the International Classification of Diseases (ICD-9) or the International Classification of Primary Care (ICPC-2). It is the sole portal for information used in all public clinical settings. This allows linkage of information when patients visit clinics in different districts. All physician prescriptions were checked by dispensers or pharmacists using standardized procedures, and any amendments in the prescriptions were captured in the database. A previous evaluation which assessed this database reported that socio-demographic and prescription details were 100% and 99.8% complete, respectively [19]. The sampling frame for this study included the entire population of Hong Kong, which is more than 7,000,000 as of 2012. Hong Kong has three distinct regions; these are Hong Kong Island (most urbanized); Kowloon; and the New Territories (most rural). Ethics clearance was obtained from the Clinical Ethics Research Committee of the Hospital Authority, and the Surveys and Behavioral Research Ethics Committee of the Chinese University of Hong Kong. No informed consent was required; this is because all subjects were anonymized with a unique identity number.
2.2. Patients
We included all patients who attended any consultations in the public sector and who were prescribed their first-ever antihypertensive medications between the calendar years 2001 to 2003 and in 2005 (the index date); the details from 2004 were excluded because the clinical services' utilization was substantially disrupted due to Severe Acute Respiratory Syndrome. We excluded patients who were prescribed any antihypertensive drugs before the index date, and treated patients who died due to conditions other than cardiovascular diseases within the observation period as being censored. We allocated each patient according to the initial prescription of antihypertensive drugs, namely, α-blockers, β-blockers, thiazide diuretics, calcium channel blockers (CCBs) and angiotensin converting enzyme inhibitors (ACEIs). Those prescribed angiotensin receptor blockers (ARBs) and combination therapy were not included in our analysis as the number was relatively few. Concomitant comorbidities include cardiovascular risk factors and diseases which could potentially influence the choice of antihypertensive drug class, as indicated by the respective ICPC-2 or ICD-9 codes. Patients were followed up until the occurrence of cardiovascular mortality during the study or at the end of five years.
2.3. Outcome variables and covariates
The outcome variables included mortality due to coronary heart disease (ICD-9 I20 to I25.1) and cerebrovascular disease (ICD-9 I60–I66.9). Among all deaths in Hong Kong, the vast majority occurred in hospitals, and this allows accurate case ascertainment [26]. Deaths in hospital have been utilized in previous studies as a valid measure of patient mortality, and it is usual in Chinese populations that death occurs in hospital [26], [27], [28]. The predictor variable in this study was the interval-based PDC, defined as the number of days when medication is supplied in a specified period divided by the total number of days within the period. Interval-based PDC is an internationally accepted metric for the assessment of medication adherence in large database analysis [29], [30], [31]. A PDC ≥ 80% indicates that the patient is medication-adherent [29], [30]. In this study we used a five-year interval for the estimation of PDC, or we used the time period between the index date and mortality if the subject died. We adopted an approach similar to Mazzaglia and colleagues [12], namely, that of classifying drug adherence into three levels: high (PDC ≥ 80%); intermediate (PDC = 40–70%); or low (PDC < 40%) [18], [31].
The potential covariates we controlled for consist of the patients' age, gender, fee payment status (recipients vs non-recipients of public assistance; each consultation in a primary care setting including investigation and prescription fees costs approximately US$5.77), type of clinic visits (in- and day-patient clinics, specialist outpatient clinics [SOPCs], accident and emergency departments [AEDs], general outpatient clinic [GOPC], and other clinic types), region of residence (Hong Kong Island vs Kowloon vs the New Territories; from the most urbanized to the most rural, respectively), number of concomitant comorbidities, and the levels of systolic blood pressure and diastolic blood pressure averaged over all clinic visits. We used the same list of comorbidities by their ICD-9 and ICPC-2 coding as published elsewhere [25], categorized under “diabetes or impaired glucose tolerance” (23.0%), “cardiovascular diseases” (24.3%), “respiratory diseases” (14.6%) and “renal diseases” (11.0%).
2.4. Statistical analysis
Student's t-tests and Chi-square tests of heterogeneity were used to compare continuous and categorical variables, respectively. To evaluate the association between medication adherence (high vs intermediate vs low), initial antihypertensive drug class and mortality, we entered all the variables listed above into one Cox-proportional hazard model with combined coronary heart disease- and stroke-specific mortality as the outcome variable. In addition, because of the observational nature of the study, treatment indication bias might exist. Therefore, an additional analysis was conducted including adjustment of propensity scores in the Cox proportion hazard models in accordance with standard statistical methodology [32], [33]. Two propensity score models were developed to estimate weightings for adherence selection, namely high vs low and intermediate vs low adherence. The absence of multicollinearity was evaluated to ensure the robustness of the regression model. The Statistical Package for Social Sciences (SPSS) version 16.0 was used for all data analyses. All p < 0.05 were regarded as statistically significant.
3. Results
3.1. Patient characteristics
A total of 218,047 eligible patients were included, 3825 patients (1.75%) died of coronary heart disease or stroke within five years after being prescribed their first-ever antihypertensive agents (Table 1 ). Among these 3825 patients, 1371 deaths were due to coronary heart disease and 2454 deaths were due to stroke. The distribution of mortality within 5 years from different causes was shown in Fig. 1 . The proportions of patients having poor, intermediate, and good medication adherence were 32.9%, 12.1%, and 55.0%, respectively. Among all the patients, the majority were females (54.9%) and aged 60 years or above (52.6%). Most (84.8%) did not receive any public assistance, and the majority attended in- or day-patient clinics (30.2%), general outpatient clinics (29.7%) or specialized outpatient clinics (29.7%). Significantly more patients lived in the most rural region (the New Territories: 48.6%) than in other more urbanized districts. Beta-blockers (45.2%) and CCBs (30.1%) were the most commonly prescribed medications, followed by ACEIs (10.5%), thiazide diuretics (8.0%), and alpha-blockers (6.2%). The majority did not suffer from any comorbidities (60.1%); with 32.5% and 7.4% having one or at least two comorbidities, respectively.
Table 1.
Baseline characteristics of patients (N = 218,047).
| Na | % | p | |
|---|---|---|---|
| Proportion Days Covered in 5 years' follow-up | |||
| < 40% | 71,734 | 32.9 | |
| 40–79% | 26,478 | 12.1 | < 0.001 |
| ≥ 80% | 119,834 | 55.0 | |
| Gender | |||
| Male | 98,270 | 45.1 | < 0.001 |
| Female | 119,775 | 54.9 | |
| Age | |||
| < 50 | 61,362 | 28.1 | < 0.001 |
| 50–59 | 42,027 | 19.3 | |
| 60–69 | 41,627 | 19.1 | |
| ≥ 70 | 73,011 | 33.5 | |
| Public assistance | |||
| Yes | 32,827 | 15.2 | < 0.001 |
| No | 183,151 | 84.8 | |
| Service type on first visit | |||
| In-/day-patient clinic | 65,860 | 30.2 | < 0.001 |
| Special out-patient clinic | 64,680 | 29.7 | |
| Accident and emergency department | 16,898 | 7.8 | |
| General outpatient clinics | 64,715 | 29.7 | |
| Others | 5885 | 2.7 | |
| District of residence | |||
| Hong Kong | 38,327 | 17.6 | < 0.001 |
| Kowloon | 73,817 | 33.9 | |
| New Territories | 105,902 | 48.6 | |
| First prescription | |||
| ACEIs | 22,985 | 10.5 | < 0.001 |
| Alpha blockers | 13,455 | 6.2 | |
| Beta blockers | 98,626 | 45.2 | |
| CCBs | 65,535 | 30.1 | |
| Thiazide diuretics | 17,445 | 8.0 | |
| Co-morbidity | |||
| 0 | 131,088 | 60.1 | < 0.001 |
| 1 | 70,915 | 32.5 | |
| 2 | 14,585 | 6.7 | |
| ≥ 3 | 1458 | 0.7 |
Cardiovascular disease refers to a composite outcome of coronary heart disease and stroke combined.
Fig. 1.
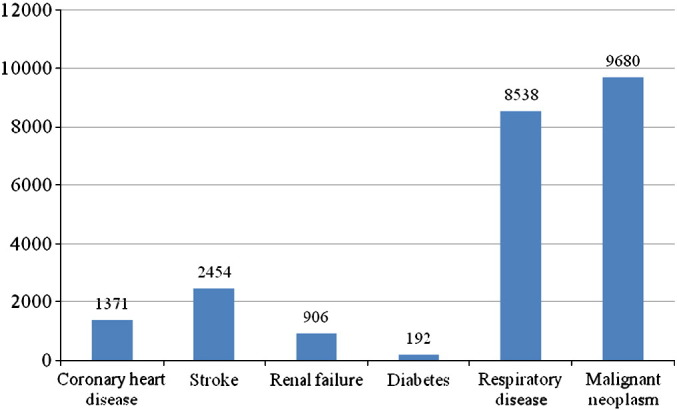
The distribution of mortality from different causes within 5 years among the study participants.
3.2. Profiles of cardiovascular mortality
Patients with higher medication adherence at PDC 40–79% (1.2%) had a lower incidence of cardiovascular mortality than those with low adherence levels (PDC < 40%) [1.8%], and the latter group had similar incidence than those having PDC ≥ 80% [1.8%]. Older patients, male subjects, those receiving public assistance and attending in- or day-patient clinics as their first visit setting had higher proportions who died from cardiovascular diseases. Residents in the most rural regions had the lowest incidence of CVS mortality (1.5% vs up to 1.7–2.1% in the more urbanized regions). Higher proportions of patients prescribed ACEIs (2.7%) and CCBs (2.7%) as their first-ever prescriptions died, followed by thiazide (1.6%), alpha-blockers (1.2%), and beta-blockers (1.0%). As the number of comorbidities increased, the cumulative incidence of cardiovascular mortality increased progressively (Table 2 ).
Table 2.
Number and percentages of deaths due to cardiovascular diseases 5 years within the cohort.
| N (%) | p | |
|---|---|---|
| Proportion Days Covered in 5 years' follow-up | ||
| < 40% | 1290 (1.8%) | < 0.001 |
| 40–79% | 305 (1.2%) | |
| ≥ 80% | 2230 (1.8%) | |
| Gender | ||
| Male | 1924 (2.0%) | < 0.001 |
| Female | 1901 (1.6%) | |
| Age | ||
| < 50 | 140 (0.23%) | < 0.001 |
| 50–59 | 200 (0.48%) | |
| 60–69 | 521 (1.25%) | |
| ≥ 70 | 2964 (4.06%) | |
| Public assistance | ||
| Yes | 1033 (3.1%) | < 0.001 |
| No | 2727 (1.5%) | |
| Service type on first visit | ||
| In-/day-patient clinic | 2627 (4.0%) | < 0.001 |
| Special out-patient clinic | 513 (0.8%) | |
| Accident and emergency department | 132 (0.8%) | |
| General Outpatient Clinics | 439 (0.7%) | |
| Others | 114 (1.9%) | |
| District of residence | ||
| Hong Kong | 657 (1.7%) | < 0.001 |
| Kowloon | 1571 (2.1%) | |
| New Territories | 1597 (1.5%) | |
| First prescription | ||
| ACEIs | 630 (2.7%) | < 0.001 |
| Alpha blockers | 168 (1.2%) | |
| Beta blockers | 1012 (1.0%) | |
| CCBs | 1744 (2.7%) | |
| Thiazide diuretics | 271 (1.6%) | |
| Co-morbidity | ||
| 0 | 1851 (1.4%) | < 0.001 |
| 1 | 1537 (2.2%) | |
| 2 | 388 (2.7%) | |
| ≥ 3 | 49 (3.4%) |
3.3. Factors associated with cardiovascular mortality
When controlled for potential confounders by Cox proportional hazard regression models, older patients (HR = 2.28 to 15.79, p < 0.001 in age groups ≥ 50 years), male subjects (HR = 0.79, 95% C.I. 0.74–0.85, p < 0.001 among females), and people receiving public assistance (HR = 1.15, 95% C.I. 1.07–1.24, p < 0.001) were more likely to suffer from cardiovascular deaths (Table 3 ). When thiazide diuretics was used as a reference group, initial prescriptions of ACEIs (HR = 1.31, 95% C.I. 1.13–1.52, p < 0.001) and CCBs (HR = 1.21, 95% C.I. 1.06–1.38, p = 0.005) were associated with higher CVS mortality, whereas patients given β-blockers (HR = 1.02, 95% C.I. 0.89–1.18, p = 0.738) were similarly likely to suffer from cardiovascular deaths.
Table 3.
Association between medication persistence and cardiovascular mortality 5 years within cohort entry.
| Hazard ratio (95% C.I.) | p | |
|---|---|---|
| Age | ||
| < 50 | 1.00 (reference) | < 0.001 |
| 50–59 | 2.28 (1.83–2.84) | |
| 60–69 | 5.65 (4.67–6.83) | |
| ≥ 70 | 15.79 (13.24–18.82) | |
| Gender | ||
| Male | 1.00 (reference) | < 0.001 |
| Female | 0.79 (0.74–0.85) | |
| Public assistance | ||
| No | 1.00 (reference) | < 0.001 |
| Yes | 1.15 (1.07–1.24) | |
| Proportion of Days Covered (PDC) | ||
| < 40% | 1.00 (reference) | |
| 40–79% | 0.46 (0.41–0.52) | < 0.001 |
| ≥ 80% | 0.91 (0.85–0.98) | 0.012 |
| First prescription | ||
| Thiazide diuretics | 1.00 (reference) | |
| ACEIs | 1.31 (1.13, 1.52) | < 0.001 |
| β-Blockers | 1.02 (0.89–1.18) | 0.738 |
| CCBs | 1.21 (1.06–1.38) | 0.005 |
ACEIs: angiotensin converting enzyme inhibitors; CCBs: calcium channel blocker.
Turning to medication adherence, higher levels at PDC 40%–79% (HR = 0.46, 95% C.I. 0.41–0.52, p < 0.001) and ≥ 80% (HR = 0.91, 95% C.I. 0.85–0.98, p = 0.012) were significantly less likely to be associated with mortality when poor adherence (PDC < 0.040) was used as a reference (Table 3). The proportions of patients with low, medium and high medication adherence who died from coronary heart disease (CHD) and stroke, respectively, were presented in Fig. 2 . When compared between coronary heart disease and stroke mortality, there was no significant difference in these proportions (p = 0.692). When propensity scores for different adherence groups were applied to the regression model, similar findings were reported (HR = 0.46, 95% C.I. 0.40–0.42 for PDC 40–79%; HR = 0.91, 95% C.I. 0.85–0.98 for PDC ≥ 80%).
Fig. 2.
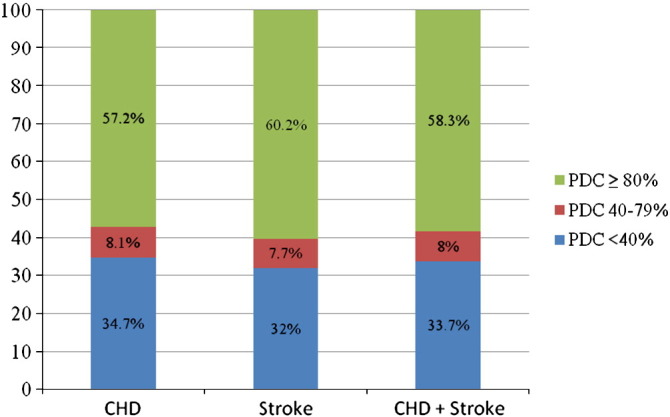
The distribution of the proportions of patients in different medication adherence groups according to coronary heart disease (CHD) and stroke mortality.
PDC: Proportion of Days Covered.
4. Discussion
4.1. Major findings
From this large database study of over 218,000 Chinese patients, it can be seen that higher medication adherence to antihypertensive agents is associated with lower cardiovascular mortality. In addition, the initial prescription of beta-blockers was independently related to a lower incidence of CVS deaths. Other at-risk factors for CVS mortality identified included advanced age, male gender, and poorer socio-economic status (using receipt of public assistance as a proxy measure).
4.2. Relationship with literature and interpretation
Corrao and colleagues utilized the health service databases of Lombardy, Italy, and followed up newly treated hypertensive patients for six years. They reported that compared to patients having PDC ≤ 25%, those with intermediate (PDC 51–75%), and high levels (PDC > 75%) of adherence had 20% and 25% of CVS risk reductions, respectively [34]. Many other studies demonstrating the positive relationship between medication compliance and clinical outcome also reflected the importance of maintaining optimal medication adherence [11], [12], [15], [16], [17], [18], [35], [36], [37], [38], [39], [40]. Our study differs from these studies in a number of respects, including the fact that they included different patient groups such as diabetics [16], patients with pre-existing myocardial infarction [18], or coronary heart disease [17]; different medications under study like cardiovascular drugs other than antihypertensive agents [15]; different clinical outcomes measured like cardiovascular events or heart failure instead of CVS mortality [12], [27], [33], [37], [38], hospitalization risk or healthcare cost [11]; and the use of self-reported data to measure adherence [36]. Furthermore, all of these studies were predominantly based on patients of Caucasian ethnicity, which group has a higher incidence of coronary heart disease and a lower risk of stroke than Chinese subjects. The prevalence of hypertension is rising rapidly in different urban and rural regions of China, and the adherence to antihypertensive medications among Chinese remains poor. For instance, recent studies found that the prevalence of hypertension in Southern China has increased to 25% in urbanized regions [41], [42], and the rates of awareness, treatment and control are as low as 17.59%, 10.39%, and 3.42%, respectively, in rural regions of China [42]. The adherence rate to antihypertensive treatment was found to be 52% among elderly Chinese Americans, and this similarly poor adherence level was also observed in other Chinese populations [43].
The other factors identified as being associated with higher CVS risks, namely, advanced age, male gender, and poorer socio-economic status have been extensively supported in previous literature [44]. The finding that the prescriptions of ACEIs and CCBs were associated with higher CVS mortality could be explained by the fact that these newer antihypertensive agents were commonly prescribed in patients with concomitant comorbidities. For instance, patients with diabetes or chronic kidney diseases were more likely to receive ACEIs, while physicians might avoid prescribing thiazide diuretics and β-blockers to patients with existing dyslipidemia and used CCBs or ACEIs as first-line agents instead.
There is one finding worthy of note — patients with high levels of adherence (PDC ≥ 80%) had hazard ratios closer to one as compared to patients having PDC in the range of 40–79%, despite the use of propensity scores to control for treatment indication bias. We believe that this could be caused by the presence of residual confounding — a possible condition might be that sicker patients at higher risk for CVS mortality were under more intensive drug-taking monitoring.
4.3. Study limitations
This is hitherto the largest observational study which has evaluated the relationship between antihypertensive adherence and clinical outcome in Asians. We report a clear inverse relationship between medication adherence and CVS mortality in real-life clinical practice. The large sample size followed up for five years, and the comprehensive computerized systems with complete clinical information are among some of the study strengths. In addition, the good dispensation practice captured by the computer further enhanced the robustness of our study findings. Nevertheless, some limitations should be discussed. Firstly, there exists an inherent limitation in database analysis, namely, the assumption that patients were actually taking the medications prescribed. In addition, the healthcare system of Hong Kong consists both of a public and a private sector, and this study cannot capture data if patients visit clinical settings in the private market — although more than 90% of hypertensive patients were followed up in the public sector for medication refill. Also, we were able to study cardiovascular outcomes for only up to five years, and not all confounders could be controlled for in this study. There exists a possibility of residual confounding despite regression analysis, and the issue of treatment indication bias could still remain despite the introduction of propensity scores. It could be argued that those who adhered better to medications could also be sicker — and hence at a significantly higher risk for cardiovascular diseases.
4.4. Implications for clinical practice and future research
This study strengthened the notion that better medication adherence would not only protect against cardiovascular mortality in interventional settings, but also in actual clinical practice. It fills the knowledge gap in existing literature which has scarcely addressed this association in non-interventional settings. As a result, we have more concrete evidence to support more intensive counseling on medication adherence initiated by physicians and allied health professionals with hypertensive patients during clinical consultations. At a health-policy level, a greater need for community-based programs and strategies to enhance compliance is justified by these findings. Many innovative approaches to enhance medication adherence, including comprehensive, multimodal pharmacy care initiatives, have been demonstrated as being effective in improving drug adherence [45]. In addition, those at higher risks of medication non-adherence [25], namely, younger patients, female subjects, people with lower socio-economic status, and patients without concomitant comorbidities should receive particular attention. Future research should focus on evaluating this association in other ethnic groups and in patients with different cardiovascular risks, as well as identifying patient subgroups where the impact of enhancing medication adherence is the strongest.
4.5. Conclusion
In summary, this study extends the understanding of the positive impact of antihypertensive medication adherence to cardiovascular mortality, in addition to cardiovascular events [12]. It also strengthens the use of medication adherence as an outcome variable on the proxy of cardiovascular outcomes in studies where mortality data cannot easily be collected. This study concurs with the recommendation by Mazzaglia et al. [12] that systematic efforts to improve medication adherence would provide even more concrete clinical benefits.
Acknowledgment
We would like to thank the Health Informatics Section of the Hospital Authority Information Technology Services for their permission to utilize the computer dataset. The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology.
Grant support: None; all authors take the responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
References
- 1.Chobanian A.V., Bakris G.L., Black H.R. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Blood Pressure Lowering Treatment Trialists' Collaboration Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362:1527–1535. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 3.Sabate E. World Health Organization; Geneva: 2003. Evidence for action. [Google Scholar]
- 4.Vrijens B., Vincze G., Kristanto P., Urquhart J., Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114–1117. doi: 10.1136/bmj.39553.670231.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Wijk B.L., Shrank W.H., Klungel O.H., Schneeweiss S., Brookhart M.A., Avorn J. A cross-national study of the persistence of antihypertensive medication use in the elderly. J Hypertens. 2008;26:145–153. doi: 10.1097/HJH.0b013e32826308b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caro J.J., Salas M., Speckman J.L., Raggio G., Jackson J.D. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160:31–37. [PMC free article] [PubMed] [Google Scholar]
- 7.Bourgault C., Sénécal M., Brisson M., Marentette M.A., Grégoire J.P. Persistence and discontinuation patterns of antihypertensive therapy among newly treated patients: a population-based study. J Hum Hypertens. 2005;19:607–613. doi: 10.1038/sj.jhh.1001873. [DOI] [PubMed] [Google Scholar]
- 8.Hughes D.A., Bagust A., Haycox A., Walley T. The impact of non-compliance on the cost-effectiveness of pharmaceuticals: a review of the literature. Health Econ. 2001;10:601–615. doi: 10.1002/hec.609. [DOI] [PubMed] [Google Scholar]
- 9.Mar J., Rodríguez-Artalejo F. Which is more important for the efficiency of hypertension treatment: hypertension stage, type of drug or therapeutic compliance? J Hypertens. 2001;19:149–155. doi: 10.1097/00004872-200101000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Mancia G., De Backer G., Dominiczak A. The ESH-ESC Task Force on the Management of Arterial Hypertension. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens. 2007;25:1751–1762. doi: 10.1097/HJH.0b013e3282f0580f. [DOI] [PubMed] [Google Scholar]
- 11.Sokol M.C., McGuigan K.A., Verbrugge R.R., Epstein R.S. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 12.Mazzaglia G., Ambrosioni E., Alacqua M. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120:1598–1605. doi: 10.1161/CIRCULATIONAHA.108.830299. [DOI] [PubMed] [Google Scholar]
- 13.Chobanian A.V. Impact of nonadherence to antihypertensive therapy. Circulation. 2009;120:1558–1560. doi: 10.1161/CIRCULATIONAHA.109.906164. [DOI] [PubMed] [Google Scholar]
- 14.Hajjar I., Kotchen T.A. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 15.Newby L.K., LaPointe N.M., Chen A.Y. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation. 2006;113:203–212. doi: 10.1161/CIRCULATIONAHA.105.505636. [DOI] [PubMed] [Google Scholar]
- 16.Ho P.M., Rumsfeld J.S., Masoudi F.A. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Int Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 17.Ho P.M., Magid D.J., Shetterly S.M. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155:772–779. doi: 10.1016/j.ahj.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Rasmussen J.N., Chong A., Alter D.A. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 19.Wong M.C.S., Jiang Y., Tang J.L., Lam A., Fung H., Mercer S.W. Health services research in the public healthcare system in Hong Kong: an analysis of over 1 million antihypertensive prescriptions between 2004–2007 as an example of the potential and pitfalls of using routinely collected electronic patient data. BMC Health Serv Res. 2008;8:138. doi: 10.1186/1472-6963-8-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong M.C.S., Jiang J.Y., Griffiths S.M. Factors associated with compliance to thiazide diuretics among 8551 Chinese patients. J Clin Pharm Ther. 2011;36:179–186. doi: 10.1111/j.1365-2710.2010.01174.x. [DOI] [PubMed] [Google Scholar]
- 21.Wong M.C.S., Jiang J.Y., Griffiths S.M. Adherence to combination therapy among ethnic Chinese patients: a cohort study. Hypertens Res. 2010;33:416–421. doi: 10.1038/hr.2009.229. [DOI] [PubMed] [Google Scholar]
- 22.Wong M.C.S., Jiang J.Y., Griffiths S.M. Short-term adherence to beta-blocker therapy among ethnic Chinese patients with hypertension: a cohort study. Clin Ther. 2009;31:2170–2177. doi: 10.1016/j.clinthera.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Wong M.C.S., Jiang J.Y., Griffiths S.M. Antihypertensive drug adherence among 6408 Chinese patients on angiotensin-converting enzyme inhibitors in Hong Kong: a cohort study. J Clin Pharmacol. 2010;50:598–605. doi: 10.1177/0091270009346058. [DOI] [PubMed] [Google Scholar]
- 24.Wong M.C.S., Jiang J.Y., Griffiths S.M. Factors associated with compliance, discontinuation and switching of calcium channel blockers in 20,156 Chinese patients. Am J Hypertens. 2009;22:904–910. doi: 10.1038/ajh.2009.95. [DOI] [PubMed] [Google Scholar]
- 25.Wong M.C.S., Tam W.W.S., Cheung C.S.K. Medication adherence to first-line antihypertensive drug class in a large Chinese population. Int J Cardiol. 2013;167:1438–1442. doi: 10.1016/j.ijcard.2012.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sun W., Schooling M., Chan W.M., Ho K.S., Lam T.H. The association between depressive symptoms and mortality among Chinese elderly: a Hong Kong cohort study. J Gerontol A Biol Sci Med Sci. 2011;66A:459–466. doi: 10.1093/gerona/glq206. [DOI] [PubMed] [Google Scholar]
- 27.Schooling C.M., Lam T.H., Li Z.B. Obesity, physical activity, and mortality in a prospective Chinese elderly cohort. Arch Intern Med. 2006;166:1498–1504. doi: 10.1001/archinte.166.14.1498. [DOI] [PubMed] [Google Scholar]
- 28.Lam T.H., Ho S.Y., Hedley A.J., Mak K.H., Peto R. Mortality and smoking in Hong Kong: case–control study of all adult deaths in. BMJ. 1998;2001:323–361. doi: 10.1136/bmj.323.7309.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choudhry N.K., Shrank W.H., Levin R.L. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15:457–464. [PMC free article] [PubMed] [Google Scholar]
- 30.Martin B.C., Wiley-Exley E.K., Richards S., Domino M.E., Carey T.S., Sleath B.L. Contrasting measures of adherence with sampling drug use, medication switching and therapeutic duplication. Ann Pharmacother. 2009;43:36–44. doi: 10.1345/aph.1K671. [DOI] [PubMed] [Google Scholar]
- 31.Andrade S.E., Kahler K.H., Frech F., Chan K.A. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–574. doi: 10.1002/pds.1230. [DOI] [PubMed] [Google Scholar]
- 32.Curtis L.H., Hammill B.G., Eisenstein E.L., Kramer J.M., Anstrom K.J. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care. 2007;45:S103–S107. doi: 10.1097/MLR.0b013e31806518ac. [DOI] [PubMed] [Google Scholar]
- 33.D'Agostino R.B. Propensity scores in cardiovascular research. Circulation. 2007;115:2340–2343. doi: 10.1161/CIRCULATIONAHA.105.594952. [DOI] [PubMed] [Google Scholar]
- 34.Corrao G., Parodi A., Nicotra F. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011;29:610–618. doi: 10.1097/HJH.0b013e328342ca97. [DOI] [PubMed] [Google Scholar]
- 35.Breekveldt-Postma N.S., Penning-van Beest F.J., Siiskonen S.J. The effect of discontinuation of antihypertensives on the risk of acute myocardial infarction and stroke. Curr Med Res Opin. 2008;24:121–127. doi: 10.1185/030079908x253843. [DOI] [PubMed] [Google Scholar]
- 36.Nelson M.R., Reid C.M., Ryan P., Willson K., Yelland L. Self-reported adherence with medication and cardiovascular disease outcomes in the Second Australian National Blood Pressure Study (ANBP2) Med J Aust. 2006;185:487–489. doi: 10.5694/j.1326-5377.2006.tb00662.x. [DOI] [PubMed] [Google Scholar]
- 37.Kettani F.Z., Dragomir A., Coˆté R. Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke. 2009;40:213–220. doi: 10.1161/STROKEAHA.108.522193. [DOI] [PubMed] [Google Scholar]
- 38.Perreault S., Dragomir A., White M., Lalonde L., Blais L., Bérard A. Better adherence to antihypertensive agents and risk reduction of chronic heart failure. J Intern Med. 2009;266:207–218. doi: 10.1111/j.1365-2796.2009.02084.x. [DOI] [PubMed] [Google Scholar]
- 39.Perreault S., Dragomir A., White M., Lalonde L., Blais L., Bérard A. Adherence level of antihypertensive agents in coronary artery disease. Br J Clin Pharmacol. 2010;69:74–84. doi: 10.1111/j.1365-2125.2009.03547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dragomir A., Coˆ,té R., Roy L. Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Med Care. 2010;48:418–425. doi: 10.1097/MLR.0b013e3181d567bd. [DOI] [PubMed] [Google Scholar]
- 41.Wu Y., Huxley R., Li L. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 42.Ma W.J., Tang J.L., Zhang Y.H. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens. 2012;25:590–596. doi: 10.1038/ajh.2012.11. [DOI] [PubMed] [Google Scholar]
- 43.Hsu Y.H., Mao C.L., Wey M. Antihypertensive medication adherence among elderly Chinese Americans. J Transcult Nurs. 2010;21:287–305. doi: 10.1177/1043659609360707. [DOI] [PubMed] [Google Scholar]
- 44.Lynch J.W., Kaplan G.A., Cohen R.D., Tuomilehto J., Salonen J.T. Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all-cause mortality, cardiovascular mortality, and acute myocardial infarction? Am J Epidemiol. 1996;144:934–942. doi: 10.1093/oxfordjournals.aje.a008863. [DOI] [PubMed] [Google Scholar]
- 45.Lee J.K., Grace K.A., Taylor A.J. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]


