Summary
Background
Healthcare workers (HCWs) face specific challenges in infectious disease outbreaks, which provide unusual, new events with exposure risk. The fear of infection or new, unknown tasks in an unfamiliar setting, for example, may complicate outbreak management.
Aim
To gain insight into how healthcare organizations can prepare to meet the needs of their HCWs by capturing the experiences of HCWs with patients with suspected Ebola virus disease.
Methods
We conducted 23 in-depth interviews with HCWs, of whom 20 worked in a Dutch university hospital and three worked in a regional ambulance service. We invited HCWs who cared for patients with suspected Ebola or who were on the team preparing for admission of such patients in the period 2014–2015.
Findings
The HCWs were stressed and anxious, but most rated their overall experience as positive. We categorized the reported experiences in three main themes, namely, experiences related to: (i) the novelty of the threat, (ii) the risk of infection and fear of transmission, and (iii) the excessive attention. Our results underline the importance of a supportive working environment suitable for crises.
Conclusion
The experiences of HCWs dealing with patients with suspected Ebola can direct improvements in generic preparedness for highly transmissible diseases.
Keywords: Health and safety, Hospital management, Infectious disease, Outbreaks, Ebola virus, Workforce, Healthcare worker
Introduction
Healthcare workers (HCWs) may experience stress when managing infectious disease outbreaks [1]. They may have to work extra shifts and perform tasks that do not belong to their daily routine in a different department, and they may have to work in a multidisciplinary team they are not accustomed to [2]. They must also deal with the unpredictability of their working schedule, which requires them to adjust their private and social life [3]. Most importantly, HCWs are at risk of exposure to highly infectious pathogens while they care for the patients. This may cause fear of being infected or being a source of infection for close contacts such as family members [2], [3], [4]. Such stressful events may have negative effects. For example, HCWs exposed to severe acute respiratory syndrome or Marburg haemorrhagic fever experienced high levels of psychological distress as a result of temperature monitoring and reporting, and of quarantine [4], [5]. The consequences of distress may persist long after the outbreak and may result in depression or post-traumatic stress disorder [2], [6], [7], [8], [9], [10].
Fortunately, not all outbreaks trigger distress in HCWs, but, in order to have the team of HCWs ready to perform optimally while the outbreak unfolds, organizations should prepare to address potential stressors. Little is known about how healthcare organizations can prepare for stress-related experiences that may affect HCWs [11].
The aim of this study was to gain insight into how healthcare organizations can prepare for meeting the needs of their healthcare personnel. We did this by studying the experiences of HCWs who dealt with patients with suspected Ebola virus disease.
Methods
Design
We conducted in-depth interviews with HCWs in the Netherlands dealing with patients with suspected Ebola during the 2014–2015 Ebola outbreak. These interviews took place from May to October in 2016.
Setting
The outbreak of Ebola virus disease in 2014 enforced hospitals to prepare for the admission of patients with suspected Ebola virus. In the Netherlands, such patients were referred to one of the five appointed university hospitals, following initial assessment by a general practitioner or a local hospital department. The regional ambulance services were responsible for transporting the patients. Of the 99 patients assessed for risk of Ebola, 14 were admitted in strict isolation. All Ebola laboratory tests proved negative [12]. Upon request of the United Nations, one patient with a confirmed case was admitted to the Major Incident Hospital in the University Medical Centre Utrecht in a Medevac procedure [13].
Study participants
We invited HCWs who had cared for a patient with suspected Ebola or were part of the team that had prepared for admission of such patients in several university hospitals in the Netherlands. We also invited HCWs from regional ambulance services who had transported a patient with suspected Ebola.
Data collection
A researcher (E.B.) trained in qualitative research interviewed the participants. Before enrolment, each participant received an information letter regarding the purpose of the interview, the voluntariness of participation, and how the data would be used. The participants were asked to sign an informed consent form. The interviews lasted 25 min to 1 h. Each interview started with a short explanation about the goal of the study. The interviews were semi-structured. We used an interview guide that included a topic list about HCWs' potential needs from a systematic literature review of outbreak preparedness (A. Huis et al., unpublished data).
We asked the participants to tell us about their experiences during the Ebola outbreak, starting with their first Ebola training session or allocation to the Ebola team and ending with the final evaluation. We asked them to reflect on their experiences during each step, from preparation to caring for the patient. We asked them to share their feelings and worries, and those of their friends and family. New themes that emerged during the interviews were intuitively added to the interview guide, to be verified in the next interviews. Inclusions took place until saturation was reached and no new concepts or themes emerged.
Analysis
The interviews were recorded with a digital voice recorder and transcribed verbatim by an independent transcriber. The main researcher (E.B.) and a member of the research team (A.T. or J.S.) coded 10 interviews, and they discussed the codes until consensus was reached. The main researcher (E.B.) coded the remaining interviews.
Synthesis
A thematic analysis was applied and the main themes extracted from the data. Patterns in the data were identified with an iterative process in research group meetings (E.B., J.S., A.T., A.H., and M.H.). The qualitative software program Atlas.ti was used for the coding.
Ethical review
The Medical Ethics Committee of the University Medical Center Utrecht assessed the study and concluded that it was exempt from their approval; reference number 16/192.
Results
Twenty-three in-depth interviews were conducted. Twenty HCWs were employed by five separate university hospitals (13 nurses, six physicians, and one person in charge of logistics). Three interviewees worked as ambulance nurses in three different regional ambulance services. Two of these interviewees had additional tasks: one was a team leader, and the other was a regional manager of acute medical incidents. All except five HCWs had children and each of them had a partner when they were involved in caring for a patient with suspected Ebola. They had four to 38 years of experience in their current profession.
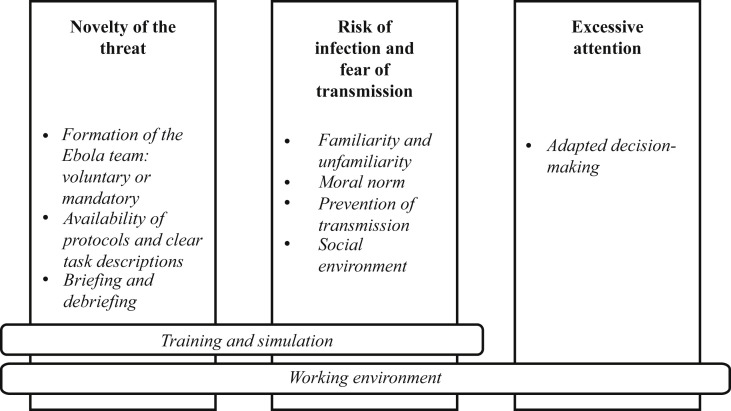
The experiences of HCWs dealing with a patient with suspected Ebola were categorized into three themes, which were experiences related to: (i) the novelty of the threat, (ii) the risk of infection and the fear of transmission, and (iii) the excessive attention (Figure 1 ). Experiences related to the ‘working environment’ were relevant for all three themes. The responses of the various types of healthcare professionals were similar with very few differences.
Figure 1.
Categorization of the experiences of healthcare workers dealing with a patient with suspected Ebola virus disease.
Overall experience
Despite their fears and anxiety, almost all the HCWs felt positive about the experience of caring for a patient with suspected Ebola. It gave them a chance to test their protocols, it was motivating, and they felt special and proud that they had been selected for this work. Afterwards, they were more motivated for further training and simulation exercises for similar outbreaks. Table I shows the corresponding quotes.
Table I.
Quotes related to the overall experience
| Interview | Quote |
|---|---|
| Male nurse in university hospital | ‘Everyone had the feeling they were doing something good for this world.’ |
| Female physician in university hospital | ‘But then the tension diminishes, and it's very nice to do something this exciting, which is actually not that exciting, but everything around it makes it very interesting.’ |
Novelty of the threat
The experiences in this domain are related to Ebola being a new situation in this part of the world. Organizations and HCWs were faced with a situation that deviated from the norm and required immediate preparations and action. Table II shows the corresponding quotes.
Table II.
Quotes related to the novelty of the threat
| Factor | Interview | Quote |
|---|---|---|
| Formation of the Ebola team: voluntary or mandatory | Male ambulance nurse | ‘I think that refusing to transport a patient with suspected Ebola would have resulted in a service request. Refusing a service request has consequences or has consequences in the future. And I definitely considered: am I willing to accept the consequences?’ |
| Availability of protocols and clear task descriptions | Male nurse in university hospital | ‘Everything was in protocols. We had task cards and protocols of everything so there was no discussion how something should be done. That was simply pre-defined.’ |
| Male ambulance nurse | ‘First they say, “This is sufficient”. And two weeks later it is completely different. Then you think: are the current equipment and the current procedures for donning PPE good enough?’ | |
| Briefing and debriefing | Male ambulance nurse | ‘Well, we had the team ready and the team came here, and the team was briefed. Whatever you do – Well, this is how we are going to do it. This is the plan, this can be expected, you should do this and you shouldn't do that; this is what we have practised.’ |
| Training and information | Female nurse in university hospital | ‘Well, we are well-trained. Bring it on!’ |
| Working environment | Female nurse in university hospital | ‘If you are in the Ebola group, then food and drink are taken care of. You can rest; there are beds. And people walk in all the time and ask, “How are you?”, “Is everything okay?” and “How are you feeling?” In that respect it is a reassuring experience.’ |
Formation of the Ebola team: voluntary or mandatory
Some healthcare organizations allowed for voluntary participation in the Ebola treatment team. Other organizations appointed employees for the team. The HCWs who voluntarily applied for the Ebola team more often reported positive experiences – less stress and anxiety – than HCWs who were mandatorily appointed. The latter said that being a team member should not be taken for granted. These HCWs wondered whether they could be fired if they refused to provide care for a patient with Ebola. One interviewee reported that she refused to be part of the Ebola team and had the feeling that her colleagues disapproved. The HCWs who volunteered were also fearful and anxious, but were nonetheless excited about doing something that really matters.
Availability of protocols and clear task descriptions
Healthcare organizations had to develop new protocols and train their HCWs to handle patients with Ebola. The HCWs described how clear and simple protocols helped them remain calm by using the instructions provided. Interviewees who worked in a healthcare organization that did not have clear and unambiguous protocols said that this caused stress and uncertainty. These HCWs felt confused because of undefined roles and tasks.
The HCWs felt safe seeing their organization continuously reviewing and improving procedures, securing the availability of all necessary materials, and taking steps to obtain the safest personal protective equipment (PPE) possible. However, a small minority saw the continuous adjustments as a weakness, mainly when PPE was involved.
Briefing and debriefing
The HCWs perceived anticipating the arrival of a patient with suspected Ebola positively. Some organizations only admitted the patient after they had completed all the preparatory work and after the isolation room had been fully prepared. By contrast, when HCWs had to rush because the patient had already arrived, they found the preparation very stressful.
Most organizations had an Ebola team meeting before the patient arrived to talk through all steps in the patient admission and treatment. This pre-arrival briefing helped the HCWs to prepare mentally.
Most healthcare organizations had a debriefing after the dismissal of each patient, which the HCWs appreciated because it served as an outlet, and protocols could be adjusted if necessary.
Training and simulation
In all the interviews, the HCWs referred to the influence of the training and preparation they had received. Most reported that training had helped them feel prepared for their tasks. However, some HCWs were unsure whether and how their healthcare organization was fully prepared. They reported that information about the disease helped them stay calm. Some HCWs said they needed more information on treatment options or disease progression.
Working environment
Most healthcare organizations put much effort into the comfort of their HCWs, and the HCWs valued these efforts. Almost all the HCWs felt that preparing for and taking care of a patient with suspected Ebola greatly increased the team spirit. After leaving the isolation room, the HCWs turned to team members as an outlet for emotions and feelings, which helped reduce their stress levels. It was very reassuring to share this experience and to talk about it with colleagues. Team members were very receptive to social talks and meetings. Nonetheless, HCWs also pointed out the importance of keeping in touch with the HCWs who were not on the Ebola team and who performed all the regular tasks. The HCWs mentioned that protocols were often developed with the entire team, which made them feel that their opinion was important. They also felt that their supervisors valued their opinions. Most organizations did an evaluation. The HCWs stated that this evaluation should be done with the entire team and not only the designated Ebola team. However, this did not happen in every organization.
Risk of infection and fear of transmission
The experiences in this domain are related to Ebola being a highly infectious pathogen, which causes fear and anxiety among HCWs and their families. Most HCWs were fearful and anxious when they had to care for a patient with suspected Ebola, although some felt safe and protected. Table III shows the corresponding quotes.
Table III.
Quotes related to the risk of infection and fear of transmission
| Factor | Interview | Quote |
|---|---|---|
| Female nurse in university hospital | ‘Will I get infected? That is your biggest fear.’ | |
| Familiarity and unfamiliarity | Female nurse in university hospital | ‘After some time it becomes more normal. After a few nights, when I was changing my clothes, my new buddy said, “Huh, aren't you nervous?” But it just becomes sort of a routine.’ |
| Moral norm | Female nurse in university hospital | ‘You get instructions like: “If the patient is dying and it is not safe for you, then we let the patient die.” But that is new to us, that is the opposite of normal. We are used to doing everything we can to keep someone alive. So I think you need to discuss the psychological effect of this. “Yes we make this choice, but we do it for your own good.” That is difficult to accept. Witnessing such an event can be very dramatic.’ |
| Prevention of transmission | Female nurse in university hospital | About personal protective equipment (PPE): ‘It demands a lot from your body and you perspire underneath it [the PPE]. Because it is really layer on layer on layer. You do have a cotton T-shirt underneath it, but that is not enough. Your body temperature will really rise, so to speak. Yes, and then you are very happy when you can take the PPE off.’ |
| Social environment | Female nurse in university hospital | ‘I think that especially my husband, and my son the most … were more concerned. Like, be careful, if anything happens, let me know.’ |
| Female physician in university hospital | ‘My partner asked me, “Shouldn't you be sleeping on the couch?” It was sort of a joke. But the undertone suggested there was more to it.’ | |
| Training and simulation | Female nurse in university hospital | ‘More like, I missed the entire psychosocial aspect around it. I thought that was a shortcoming. … At least to sit around the table and listen to what the needs are.’ |
| Working environment | Female nurse in university hospital | About the buddy: ‘It was very clear what was expected from you and what you should do. There was no question about that. And also, how you should do it. You didn't have to figure that out yourself.’ |
| Male nurse in university hospital | ‘Yes … some supervisors stayed at night … so we could discuss things with them if we wanted.’ |
Familiarity and unfamiliarity
The HCWs said that they were nervous about entering the patient's room because they did not know what to expect. They were anxious about how seriously ill the patient would be; they were relieved when they found that the patient was mildly ill. They reported that, when entering the patient's room, they were extremely alert about their own actions and were afraid of making mistakes. Once they had entered the room and had seen a patient who needed their help, they felt comfortable in the role of care provider. In addition, HCWs who had to enter the patient's room repeatedly reported that their fear and anxiety diminished at each entrance. Some HCWs were afraid that, without wearing any PPE, they had been in contact with a supposedly non-infectious patient who would later be diagnosed with Ebola.
Moral norm
Most healthcare organizations propagated the ‘one's own safety first’ principle. This means, for example, that lifesaving invasive procedures might have to be delayed or cancelled if a staff member with inadequate PPE is in the room. It was difficult for some HCWs to accept the fact that their own safety was given preference over the patient's health.
Prevention of transmission
Wearing PPE was reported to be a significant physical burden. Working in full PPE makes the body temperature rise and moving around is difficult. Physicians could sometimes provide care at a physical distance from the patients (for example, by using the intercom), whereas direct nursing care can never take place at a distance.
Social environment
The HCWs feared for the safety of their family and vice versa. Most interviewees reported that their family members were anxious. Some HCWs kept in touch with their family members, mostly by telephone, and updated them regularly on their tasks and well-being. Family members also feared transmission; some asked the HCW to keep a distance at home or to take an extra shower before joining the family, sit in a separate chair, or sleep on the couch. Most healthcare organizations had information available for family members (sometimes written, and some organizations had a meeting), but this information was generally not used. If the organization did not have information available for family members, HCWs reported that they had missed it. Most HCWs reassured their family members themselves and provided information about disease and control measures.
Training and simulation
Almost all the interviewees were very positive about the training and simulation exercises. Because of the training and simulation exercises, the HCWs had information about the pathogen and knew how to prevent transmission. Some HCWs regretted that they were unprepared for the fear and anxiety that they experienced. They said that training and simulation exercises focused mainly on technical guidance related to the pathogen and the transmission routes only. They focused on preventing transmission, whereas no attention was paid to mental well-being in the preparation phase or during training sessions. The HCWs felt the need to talk about their worries with their colleagues and team managers in this phase.
Working environment
Almost all the interviewees said that having a buddy who helped them put on and take off the PPE was useful and comforting. The buddy instructed the HCW, who then felt more at ease during high-risk procedures without having to think about what they should do and only had to carry out the task. By contrast, some HCWs found it difficult to carry out the buddy's instructions without being allowed any personal initiative.
Some HCWs positively valued the fact that their supervisors and medical specialists were more easily accessible than in normal situations. Most HCWs said that, in this exceptional situation, there was always someone available to answer all their questions. They also appreciated the fact that, when they were caring for a patient with suspected Ebola, they had much more time for the patient than in their regular work because they could care only for this one patient. However, since there was not much work to do, they were sometimes bored. Further, the efforts of their employers to do everything possible to protect their safety made the HCWs feel safe.
Excessive attention
The suspected Ebola led to media frenzy and attracted a lot of curiosity from other healthcare staff and from the media. Table IV shows the corresponding quotes.
Table IV.
Quotes related to excessive attention
| Factor | Interview | Quote |
|---|---|---|
| Adapted decision-making | Female physician in university hospital | ‘Well … I think it's a bit tricky … I was focused on the entire patient process, but what I ran into is that, while working, my activities were somewhat determined by the board of directors. They decided when the patient was to be dismissed from the isolation room, while this is a medical decision.’ |
| Working environment | Female physician in university hospital | ‘Yes, you are just doing your job and the first time with the first patient and the first moments in the isolation room …. If there are a lot of people nearby, you think: just let us do our jobs. Because when you get out of the isolation room you are sweating like crazy and just want to recover.’ |
Adapted decision-making
Some doctors reported that the board of directors took over the medical decision-making because the board wanted to ensure that the right decisions were made. Physicians from one hospital reported that, in their opinion, the visibility of the team taking care of the patients with suspected Ebola was underexposed. Some nurses said they were not allowed to follow up on the patient's condition at home. They reported that sometimes they were concerned about the patient's condition when they were at home. They sometimes kept thinking about the patient while they were off duty because they had no access to the patient's record and colleagues were not allowed to give them any information. However, physicians could often follow up on the patient while they were at home. They found this very comforting and reassuring.
Working environment
Most HCWs were bothered by the unnecessary presence of colleagues in the patient's room. Because of media attention and the interest of colleagues, the HCWs felt that they were being watched. In some cases, colleagues from other departments in the hospital were anxious and insecure about a patient with suspected Ebola being in their hospital. Nonetheless, there was a lot of positive and supportive interest from colleagues and supervisors. The HCWs felt that their supervisors, doctors, and team members supported them. The supervisors were generally more easily accessible than in normal situations. However, if the supervisor was stressed or unsupportive, this reflected on the HCWs. The HCWs considered the presence of security guards in the department to be good because they kept intruders out of the department.
Discussion
We studied the experiences of HCWs dealing with patients with suspected Ebola in the industrialized western world to gain insight into how healthcare organizations can prepare for meeting the specific needs of their healthcare personnel in future crises. Such insight may improve generic preparedness regarding highly transmissible diseases. Our results show that, overall, most HCWs felt positive about the total experience despite their fears and anxiety. On the basis of the reported experiences, we constructed a framework for preparedness that included crisis-specific themes. The interviews clearly showed the importance of a supportive working environment. Training and simulation were also seen as helpful for dealing with this new situation with a high risk of infection. When preparing for outbreaks, healthcare organizations focus mainly on the medical, hygienic, and organizational aspects, whereas the human factors are ignored [14]. Our study shows that, while preparing for outbreaks, a general working environment that meets the needs of the individual and ensures the support of the team and the managers is crucial.
One must bear in mind that in this study we interviewed professionals who worked in a well-organized and well-prepared healthcare system while caring for patients potentially infected by a highly contagious disease. Even in this well-controlled and relatively safe situation, we found many aspects that affect HCWs. The impact on HCWs working in less well-organized or less prepared organizations will likely be different. Healthcare organizations should plan and put mechanisms in place to capture the experiences of HCWs and channel them in order to improve the resilience of the HCWs, and, if need be, their families. There are many studies and guidelines that describe mental care in other contexts of major emergency situations, mass trauma events, or disasters [11], [15], [16]. In line with our findings, these documents acknowledge the importance of creating feelings of safety and connectedness, providing reliable information, and showing organizational involvement and facilitation of the exchange of experiences between those involved. However, they lack recommendations about the risk of infection and excessive attention that may arise during outbreaks. The results of these studies and guidelines are, however, difficult to translate to HCWs dealing with highly infectious patients for three reasons. First, most of the literature describes care for victims or patients but not for HCWs who are exposed to the pathogen because of their obligation to attend work [11], [16], [17], [18]. Second, infectious disease outbreaks have a unique feature among mass trauma events: transferability of pathogens from person to person that may result in fear of containment. Third, an outbreak is not a sudden disaster; the severity may gradually increase, and infectious disease outbreaks may eventually last for months. This means that HCWs must work in a stressful environment for a long period. One other study took a step to gain insight into the experiences of HCWs regarding their mental state when they were working during the Ebola outbreak in a western country [19]. The reported experiences are similar to our findings. Our study, in addition, provides a systematic framework that may be helpful to healthcare organizations when they are preparing for outbreaks. The experiences related to the factor ‘working environment’ apply to all outbreaks, irrespective of whether they are new or highly infectious, or whether they create excessive attention. Healthcare organizations should first focus on these experiences when they begin preparing for outbreaks.
There are several limitations to this study. First, there was only one confirmed Ebola case in the Netherlands. The 14 suspected cases were negative. The experiences of the HCWs in our study should therefore be considered a best-case scenario. Second, there was a delay between the HCW caring for a patient with suspected Ebola and the interview that may have caused recall bias. This study can nevertheless be used as a basis for further research into this topic and gives enough items and opportunities for improving preparedness in the industrialized western world. Because we identified experiences, and not necessarily needs or shortcomings of healthcare organizations, it is difficult to provide extensive advice for healthcare organizations. One of the strengths of this study is the data synthesis. We used an iterative group process that led to the identification of patterns and themes across our data. Another strength is the diversity of the HCWs who participated in the interviews. All the relevant types of HCW were included from different hospitals and different ambulance services in the Netherlands. We interviewed more than 20 HCWs, ensuring that different perspectives were taken into account.
In conclusion, it is important that the experiences of HCWs in settings such as the Ebola outbreak are not forgotten, but are translated into a set of recommendations for healthcare organizations preparing for, or responding to, outbreaks of serious infections.
Conflict of interest statement
None declared.
Funding sources
This work was carried out with financial support from the Dutch Ministry of Health, Welfare and Sport (VWS).
References
- 1.Hall R.C., Hall R.C., Chapman M.J. The 1995 Kikwit Ebola outbreak: lessons hospitals and physicians can apply to future viral epidemics. Gen Hosp Psychiatry. 2008;30:446–452. doi: 10.1016/j.genhosppsych.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koh D., Lim M.K., Chia S.E., Ko S.M., Qian F., Ng V. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Med Care. 2005;43:676–682. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- 3.Gershon R.R., Magda L.A., Qureshi K.A., Riley H.E., Scanlon E., Carney M.T. Factors associated with the ability and willingness of essential workers to report to duty during a pandemic. J Occup Environ Med. 2010;52:995–1003. doi: 10.1097/JOM.0b013e3181f43872. [DOI] [PubMed] [Google Scholar]
- 4.Timen A., Isken L.D., Willemse P., van den Berkmortel F., Koopmans M.P., van Oudheusden D.E. Retrospective evaluation of control measures for contacts of patient with Marburg hemorrhagic fever. Emerg Infect Dis. 2012;18:1107–1114. doi: 10.3201/eid1807.101638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mollers M., Jonges M., Pas S.D., van der Eijk A.A., Dirksen K., Jansen C. Follow-up of contacts of Middle East respiratory syndrome coronavirus-infected returning travelers, the Netherlands, 2014. Emerg Infect Dis. 2015;21:1667–1669. doi: 10.3201/eid2109.150560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan A.O., Huak C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond) 2004;54:190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Can Med Assoc J. 2004;170:793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin C.Y., Peng Y.C., Wu Y.H., Chang J., Chan C.H., Yang D.Y. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. 2007;24:12–17. doi: 10.1136/emj.2006.035089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Phil Trans R Soc Lond B Biol Sci. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsuishi K., Kawazoe A., Imai H., Ito A., Mouri K., Kitamura N. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci. 2012;66:353–360. doi: 10.1111/j.1440-1819.2012.02336.x. [DOI] [PubMed] [Google Scholar]
- 11.Bisson J.I., Tavakoly B., Witteveen A.B., Ajdukovic D., Jehel L., Johansen V.J. TENTS guidelines: development of post-disaster psychosocial care guidelines through a Delphi process. Br J Psychiatry. 2010;196:69–74. doi: 10.1192/bjp.bp.109.066266. [DOI] [PubMed] [Google Scholar]
- 12.Swaan C.M., Öry A.V., Schol L.G.C., Jacobi A., Richardus J.H., Timen A. Ebola preparedness in the Netherlands: the need for coordination between the public health and the curative sector. J Public Health Manag Pract. 2017 Mar 28 doi: 10.1097/PHH.0000000000000573. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haverkort J.J., Minderhoud A.L., Wind J.D., Leenen L.P., Hoepelman A.I., Ellerbroek P.M. Hospital preparations for viral hemorrhagic fever patients and experience gained from admission of an Ebola patient. Emerg Infect Dis. 2016;22:184–191. doi: 10.3201/eid2202.151393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belfroid E., Timen A., van Steenbergen J.E., Huis A., Hulscher M.E.J.L. Which recommendations are considered essential for outbreak preparedness by first responders? BMC Infect Dis. 2017;17:195. doi: 10.1186/s12879-017-2293-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hobfoll S.E., Watson P., Bell C.C., Bryant R.A., Brymer M.J., Friedman M.J. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70:283–315. doi: 10.1521/psyc.2007.70.4.283. discussion 316–69. [DOI] [PubMed] [Google Scholar]
- 16.Werkgroep multidisciplinaire richtlijnontwikkeling psychosociale hulp bij rampen en crises. Multidisciplinaire Richtlijn psychosociale hulp bij rampen en crises. 2014, Impact, Landelijk kennis- en adviescentrum psychosociale zorg en veiligheid bij schokkende gebeurtenissen. Partner in Arq Psychotrauma Expertgroep, Diemen; 2014.
- 17.Inter-Agency Standing Committee . IASC; Geneva: 2007. Guidelines on mental health and psychosocial support in emergency settings. [DOI] [PubMed] [Google Scholar]
- 18.De Vries M., Speets A.M., Kellert I.M., Smilde-van den Doel D.A. 2008. Inzet van geüniformeerde hulpverleners bij rampen en grootschalige calamiteiten: psychosociale gevolgen en de organisatie van preventie en nazorg in Nederland. Inventarisatie en beleidsaanbevelingen. [Google Scholar]
- 19.Smith M.W., Smith P.W., Kratochvil C.J., Schwedhelm S. The psychosocial challenges of caring for patients with Ebola virus disease. Health Secur. 2017;15:104–109. doi: 10.1089/hs.2016.0068. [DOI] [PubMed] [Google Scholar]