Abstract
Bacterial pneumonia is a common clinical diagnosis in dogs but seems to occur less commonly in cats. Underlying causes include viral infection, aspiration injury, and foreign body inhalation. Identification of the organisms involved in disease, appropriate use of antibiotics and adjunct therapy, and control of risk factors for pneumonia improve management.
Keywords: Bacterial pneumonia, Lower respiratory tract infection, Canine, Feline, Lower airway disease
Key points
-
•
Bacterial pneumonia is recognized much more commonly in dogs than in cats.
-
•
Viral infection followed by bacterial invasion is common in young dogs, whereas aspiration pneumonia and foreign body pneumonia seem to be more common in older dogs.
-
•
Clinical signs can be acute or chronic and do not always reflect a primary respiratory condition.
-
•
Definitive diagnosis requires detection of intracellular bacteria in airway cytology or clinically significant bacterial growth from an airway sample, although relevant clinical findings are often used.
-
•
Treatment requires identification of underlying diseases associated with pneumonia, appropriate antibiotic therapy, and control of airway secretions.
Introduction
Bacterial pneumonia remains one of the most common clinical diagnoses in dogs with either acute or chronic respiratory disease. New research suggests a complex relationship between viral respiratory diseases and development of bacterial pneumonia in dogs. Over the past decade, much has been discovered about the convoluted interplay between host and environmental factors that leads to this complex of diseases. In cats, bacterial pneumonia is less commonly identified than inflammatory feline bronchial disease.
Classification of bacterial pneumonia
Aspiration
Aspiration pneumonia results from the inadvertent inhalation of gastric acid and/or ingesta and remains a common cause of bacterial pneumonia, accounting for roughly 23% of clinical diagnoses in a study of human patients admitted to the intensive care unit.1 Although inhalation of gastroesophageal material is a common theme, different factors lead to the development of this phenomenon. Risk factors that have been identified for the development of aspiration pneumonia include esophageal disease, refractory vomiting, seizures, prolonged anesthesia, and laryngeal dysfunction (Table 1 ).2
Table 1.
Factors associated with aspiration pneumonia
|
|
|
|
|
|
In a healthy animal, physiologic and anatomic features reduce the chance of aspiration. During a normal swallow, fluid and food are propelled caudally in the oropharynx and through the upper esophageal sphincter by contraction of the oral cavity and tongue. At the same time, the epiglottis retracts to cover the laryngeal aditus and protect the trachea from particulate inhalation. Adduction of the arytenoid cartilages then contributes to further occlusion of the upper airways. Any process impeding these primary defenses or inhibiting the normal swallowing reflexes increases the likelihood of aspiration.
Aspiration injury results from inhalation of either sterile, acidic gastric contents (resulting from vomiting or gastric regurgitation) or of septic material from gastric or oral secretions. Irritation induced by acid inhalation promotes a local environment in which bacterial colonization can develop and lead to bacterial pneumonia. The severity of disease varies depending on the quantity and nature of the material aspirated as well as the length of time between the event and its diagnosis. Conscious patients with intact airway reflexes tend to cough and prevent massive aspiration injury. Animals under anesthesia or with reduced airway reflexes because of neurologic disorders are less likely to cough in response to the aspiration event and are, therefore, more likely to develop diffuse pulmonary infiltrates and acute lung injury. In many instances aspiration injuries occur under general anesthesia and the presence of a cuffed endotracheal tube does not prevent inadvertent aspiration.
Canine Infectious Pneumonia
Infectious, or community-acquired, pneumonias in dogs commonly begin with viral colonization and infection of the upper respiratory tract (canine respiratory coronavirus, herpesvirus, pneumovirus, and parainfluenza virus, among others).3 Often, such diseases are acute and self-limiting, but in a subset of dogs inflammation associated with these organisms immobilizes the host's immune defenses and predisposes infection with other (often bacterial) respiratory pathogens.4 Many bacteria have been implicated in canine infectious respiratory disease (CIRD), although special focus has been directed toward Streptococcus (specifically Streptococcus equi subsp zooepidemicus and S canis), Mycoplasma cynos, and Bordetella bronchiseptica.
CIRD is especially prevalent in dogs naive to the pathogens and exposed in overcrowded, stressful environments such as animal shelters, boarding kennels, and treatment facilities. The pathophysiology associated with this disease and infectious lower respiratory tract disease in cats is discussed later in this article (Boxes 1 and 2 ).
Box 1. CIRD complex: changing the nature of kennel cough.
CIRD complex (formerly known as kennel cough) is a syndrome in which multiple pathogens, both viral and bacterial, coinfect either naive, immunocompromised dogs or previously vaccinated dogs. This complex is multifactorial and it is likely that both host and environmental factors play a role in the development of illness.27 Organisms associated with this disease are ubiquitous, especially in overcrowded housing facilities such as animal shelters and training facilities. It is likely that stress induced by the new environment and exposure to novel pathogens both play a role in development of disease.
In most cases, respiratory signs are present for days to weeks and most animals show mild to moderate clinical signs. Viral infections typically cause either a bronchopneumonia or bronchointerstitial pneumonia because of their propensity to infect and damage type I pneumocytes.28 As the condition progresses, desquamation of the respiratory epithelium and aggregation of inflammatory cells further reduce the lungs' natural defenses, increasing the potential for secondary bacterial colonization and infection.
Previous studies have implicated viral organisms such as canine adenovirus or canine parainfluenza29 as major participants in CIRD, although recent studies have proposed novel respiratory pathogens such as canine respiratory coronavirus,3, 20, 30, 31 canine influenza virus,20 and canine herpesvirus32 as additional important pathogens associated with CIRD. B bronchiseptica,33 Streptococcus canis, S equi subsp zooepidemicus,29 and M cynos 3, 34 have been implicated as secondary bacterial infections associated with CIRD. S equi subsp zooepidemicus infections, in particular, have been associated with a rapidly progressive and often fatal hemorrhagic pneumonia.27, 35 Some strains identified in outbreaks of this pathogen have been identified as resistant to tetracycline antibiotics, which are often the drug of choice prescribed for other bacterial pathogens associated with this complex.
Box 2. Feline lower respiratory tract infections.
Organisms that have been reported as lower respiratory pathogens of cats include Pasteurella spp, Escherichia coli, Staphylococcus spp, Streptococcus spp, Pseudomonas spp, B bronchiseptica, and Mycoplasma spp,36 and specific attention has been paid to Mycoplasma spp because of a possible association with the induction and exacerbation of asthma in adult and pediatric human patients.37 However, the association between lower respiratory infection and chronic inflammatory lower airway disease in cats is unclear and is a topic of ongoing interest.
Mycoplasma species are considered normal flora in the upper respiratory tract and their role is controversial in lower respiratory tract infection. Because they are rarely identified cytologically, and specific culture or polymerase chain reaction is needed to document the presence of these organisms, the role of Mycoplasma in cats (as well as in dogs) remains difficult to define.
Foreign Body
Inhaled foreign bodies carry mixed bacterial and fungal organisms into the lung and are associated with focal pneumonias that are often initially responsive to antimicrobial medications but relapse shortly after discontinuation of therapy.5, 6 Foreign bodies reported in the veterinary literature include grass awns, plant materials, or plastic materials.6 Organisms associated with grass awn inhalation include Pasteurella, Streptococcus, Nocardia, Actinomyces, and anaerobic bacteria.6, 7 Most often, foreign material remains at the carina or enters caudodorsal principal bronchi (accessory, right and left caudal lobar bronchi).
Features associated with pulmonary foreign bodies include:
-
•
Young, sporting breeds
-
•
Environmental exposure to grass awns
-
•
Focal, recurrent radiographic alveolar pattern
-
•
History of other cutaneous or visceral foreign bodies
-
•
Spontaneous pneumothorax or pyothorax
Normal thoracic radiographs do not rule out the possibility of an airway foreign body8 and even computed tomography (CT) can fail to identify an affected bronchus. Chronic pulmonary foreign bodies are associated with marked inflammation that can lead to massive airway remodeling and bronchiectasis that, when seen on radiographs, should raise the degree of suspicion for foreign body.5
Nosocomial
Ventilator-associated pneumonia (VAP) is a common cause of hospital-acquired pneumonia in people, although there are few veterinary reports in the literature. Colonization of the oropharynx by pathogenic and multidrug-resistant bacteria occurs and the endotracheal tube acts as a conduit to transmit pathogens into the airways, which leads to tracheobronchitis and potentially pneumonia. In addition, any animal with a compromised respiratory tract or serious systemic disease is particularly prone to development of infectious airway disease while hospitalized.
The use of mechanical ventilation in human patients raises the risk of nosocomial infection by 6-fold to 20-fold.9 No published studies assess the risk in ventilated veterinary patients, although a study investigating differences in bacterial sensitivity between ventilated and nonventilated patients suggested that patients requiring mechanical ventilation were more likely to be infected with bacteria resistant to the antimicrobials most commonly used in veterinary practice.8 This finding parallels the increase in incidence of multidrug-resistant VAP in human medicine.9
Immune Dysfunction
Both the innate and adaptive immune systems protect against the development of infectious airway disease, and a breakdown in either increases the likelihood of opportunistic infection (Table 2 ). Congenital immunodeficiencies have been recognized that make an animal particularly sensitive to infectious disease. Young animals are especially prone to the development of bacterial pneumonia because of their naive immune systems, and when coupled with alterations to the innate immune system, such as primary ciliary dyskinesia (PCD) or complement deficiency, the risk of life-threatening infection increases greatly (see Veterinary Clinics of North America 2007;37(5):845-60 for a comprehensive review of respiratory defenses in health and disease).
Table 2.
Conditions leading to impaired immune function and resulting in increased risk of pneumonia
| Congenital | Acquired | |
|---|---|---|
| Innate | Primary ciliary dyskinesia Complement deficiency Leukocyte adhesion deficiency |
Bronchiectasis Secondary ciliary dyskinesia |
| Adaptive | Immunoglobulin deficiency Severe combined immunodeficiency |
Retrovirus infection (eg, FIV, FeLV) Endocrine or metabolic disease (eg, DM or HAC) Chemotherapy and other immunosuppressive therapy Splenectomy |
Any cause of systemic immunocompromise increases the risk for bacterial pneumonia, and any additional alterations to the body's natural defense mechanisms increase the risk. Medications such as chemotherapy, immunosuppressive therapy, or antitussive therapy significantly increase the likelihood of bacterial pneumonia. Underlying respiratory viruses or systemic viruses such as feline leukemia virus and feline immunodeficiency virus have the potential to enhance the severity of respiratory illness.
Clinical signs
Clinical signs of bacterial pneumonia vary depending on its cause, severity, and chronicity of disease. They can be acute or peracute in onset or can display an insidious onset, resulting in chronic illness. Early in disease, mild signs such as an intermittent, soft cough might be the only evidence of disease. As infection spreads, clinical signs worsen and often include a refractory, productive cough, exercise intolerance, anorexia, and severe lethargy. Owners can note a change in the respiratory pattern, with increased panting or rapid breathing and, in cases of severe infection, cyanosis and orthopnea can be observed. In general, these systemic signs are more obviously displayed in dogs than in cats.
Cats with pneumonia can display similar clinical signs, although the cough can be misinterpreted as a wretch or vomit by owners. Clinical signs and radiographic findings can also be considered consistent with inflammatory airway disease. As disease worsens, cats can become tachypneic with short, shallow breaths and nasal flaring.10 Owners rarely notice exercise intolerance associated with bacterial pneumonia.
Physical examination
As with the history and clinical signs of bacterial pneumonia, physical examination findings vary with the state and severity of disease. Dogs or cats with mild disease can have no abnormalities detected on physical examination. An early clue to the diagnosis might be a change in the respiratory pattern, with an increase in rate and effort. The clinician needs to pay close attention to thoracic auscultation because adventitious lung sounds (crackles and wheezes) can be subtle, focal, or intermittent. In many cases, only harsh or increased lung sounds are detected rather than crackles.5 The examination should also include a thorough auscultation of the trachea and upper airway for evidence of upper airway signs (eg, nasal congestion or discharge) that can result from lower airway infection, either as an extension of epithelial infection or from nasopharyngeal regurgitation of lower airway secretions.
Animals with bacterial pneumonia generally present with mixed inspiratory and expiratory signs, similar to those seen with other diseases of the pulmonary parenchyma. Fever is detected in 16% to 50% of cases, so it is not a reliable indicator of disease.4, 11, 12, 13
Diagnosis
Bacterial pneumonia implies sepsis of the lower airway and lungs, so the diagnosis is confirmed by showing septic suppurative inflammation on airway cytology obtained through bronchoalveolar lavage (BAL) or tracheal wash, along with a positive microbiology culture. In some cases, this is completed easily and yields results consistent with clinical suspicion. However, financial limitations or patient concerns can inhibit the ability to collect samples needed to document specifically a bacterial infection, and in those cases a clinical diagnosis of bacterial pneumonia might be presumed based on available information.
A clinical diagnosis of bacterial pneumonia should be reached after obtaining compelling evidence to suggest a bacterial cause for the animal's clinical signs (after excluding other causes), with appropriate resolution of signs following suitable antimicrobial therapy. Acute bacterial pneumonia is a common diagnosis in the small animal clinic and can often be easily identified; however, early and chronic pneumonias are more challenging to recognize because clinical signs can be subtle.
Hematology
The complete blood count is a useful diagnostic test in animals with respiratory signs. Bacterial pneumonias are typically associated with an inflammatory leukogram, characterized primarily by a neutrophilia, with or without a left shift and variable evidence of toxic changes,7, 14 although the absence of inflammatory change does not exclude the possibility of pneumonia.4, 11 Furthermore, the leukogram and differential can provide clues to suggest that bacterial pneumonia is less likely. For example, eosinophilia in an animal with respiratory signs would suggest eosinophilic bronchopneumopathy or parasitic lung diseases as an underlying cause rather than a bacterial cause. The erythrogram and platelet evaluation are generally not helpful in determining a bacterial cause of respiratory disease.
A biochemistry panel, urinalysis, and fecal flotation do not always contribute to the diagnosis of bacterial pneumonia but can provide clues to the presence of metabolic or endocrine diseases that could make the development of bacterial pneumonia more likely.
Thoracic Radiography
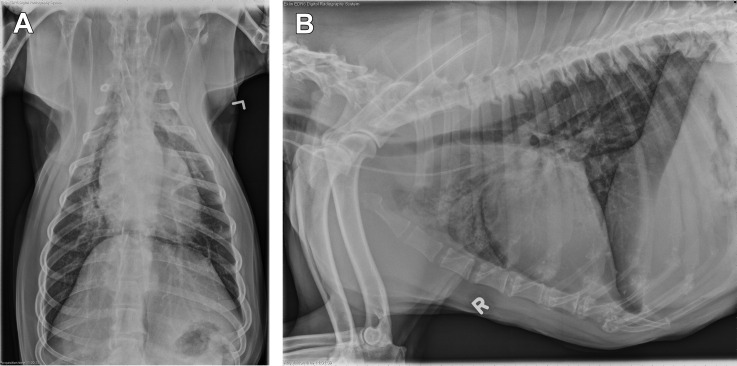
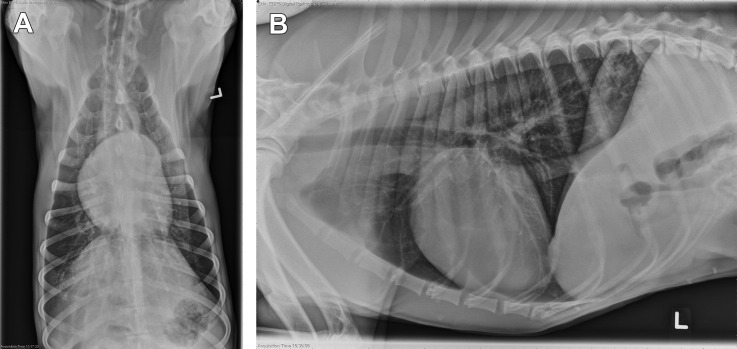
Thoracic radiographs are crucial diagnostic tests in the evaluation of lower airway and pulmonary parenchymal disease. Radiographic evidence of bacterial pneumonia can appear as a focal, multifocal, or diffuse alveolar pattern, although early in the disease process infiltrates might be primarily interstitial (Figs. 1 and 2 ). Ventral lung lobes are most commonly affected in aspiration pneumonia, and a caudodorsal pattern is expected with inhaled foreign bodies or hematogenous bacterial spread. A lobar sign can be seen in cases of aspiration pneumonia in which the right middle lung lobe is most often affected (Table 3 ).
Fig. 1.
Dorsoventral (A) and right lateral (B) thoracic radiographs from a dog with an alveolar pattern in the cranioventral lung lobes, suggesting aspiration. In this case, the left cranial lobes were most affected which are most easily examined on the right lateral view. In many cases the right middle lung lobe is most affected, necessitating a left lateral orthogonal view.
Fig. 2.
Dorsoventral (A) and right lateral (B) thoracic radiographs of a dog with a focal, patchy, interstitial to alveolar pattern in the left cranial lung lobe. This dog was diagnosed with a foxtail foreign body, which was removed thoracoscopically via lung lobectomy.
Table 3.
Differential diagnoses for specific radiographic patterns
| Lobar Alveolar Consolidation | Focal Alveolar Consolidation |
|---|---|
| Aspiration pneumonia (cranioventral, right middle) Lung lobe torsion (cranial) Atelectasis secondary to mucus plugging (right middle most commonly) |
Airway foreign body Primary pulmonary neoplasia (caudal) Metastatic neoplasia Noncardiogenic pulmonary edema |
| Diffuse Alveolar Pattern | Diffuse or Focal Interstitial Pattern |
|---|---|
| Acute respiratory distress syndrome Congestive heart failure (perihilar in dogs) Fluid overload Eosinophilic bronchopneumopathy Coagulopathy Metastatic neoplasia |
Early bacterial pneumonia Imminent congestive heart failure Pneumocystis carinii infection Inhalant toxicity (eg, paraquat) Viral pneumonia |
Three-view thoracic radiographs (left lateral, right lateral, and either dorsoventral or ventrodorsal views) should be obtained when screening for pneumonia because differential aeration associated with positional atelectasis can either mask or highlight pulmonary changes. For example, a radiograph taken in left lateral recumbency is preferred when aspiration is suspected because it increases aeration of the right middle lung lobe, the most commonly affected lobe.
Diffuse radiographic involvement is expected to suggest more severe disease, although radiographic changes lag behind clinical disease. Consequently, bacterial pneumonia cannot be ruled out in patients with acute onset of clinical signs and unremarkable radiographs.7
Advanced Imaging
Advanced imaging is rarely necessary in the diagnosis of uncomplicated bacterial pneumonia, although it can be helpful in more complicated cases. Thoracic ultrasound can be used to characterize peripheral areas of consolidation and to obtain fine-needle aspirates for cytology. Cytology is often helpful in distinguishing inflammation from neoplastic infiltration. In addition, sonographic evaluation is particularly useful in the detection of superficial foxtail foreign bodies when they remain in the periphery of the lobe (Fig. 3 ).10
Fig. 3.
A foxtail foreign body retrieved bronchoscopically from the left principal bronchus of a dog with chronic respiratory signs. Foxtails are endemic to the Western and Midwestern United States and are often associated with mixed aerobic, anaerobic, and fungal infections.
CT provides greater detail and resolution of lesions within the pulmonary parenchyma and gives the clinician better spatial information regarding the severity and extent of pulmonary involvement (Fig. 4 ). In some cases, CT can be useful to identify migration tracts associated with inhaled foreign bodies.7 However, in most cases, general anesthesia is required for CT acquisition and prolonged recumbency can lead to atelectasis, which is difficult to differentiate radiographically from infiltrates. Repeating the CT in a different position after providing several maximal inspirations can alleviate atelectasis. Nuclear scintigraphy can be useful for the evaluation of ciliary dyskinesia, although secondary causes of mucociliary stasis (ie, infection with Mycoplasma or Bordetella, as well as exposure to smoke) must be excluded before assuming the diagnosis of PCD. Because of the time necessary for image acquisition, magnetic resonance imaging is not commonly used for the diagnosis of most respiratory diseases.
Fig. 4.

CT image of a dog with severe, diffuse pneumonia resulting from a chronic foxtail foreign body (see Fig. 3). The foreign body was not visible on thoracic radiographs, but is clearly evident in the left principal bronchus on this image.
Bronchoscopic Evaluation
Examination of the trachea and bronchial tree should be performed systematically. The endoscopist should note the color and character of the mucosa and any airway sections, making sure to evaluate all branches of the lower airways for evidence of foreign bodies, bronchiectasis, or collapse (diffuse or focal changes). Airway mucosa in a normal animal should be pale pink with visible mucosal and pulmonary vessels. Airway bifurcations should appear as narrow, crisp mucosal margins.
Animals with pneumonia can have hyperemia of the epithelium, prominent mucosal vessels, and evidence of airway inflammation, appearing as rounded, thickened airway bifurcations and airway nodules. Airway secretions are usually opaque, viscous, and discolored (brown, yellow-green, or red tinged).
Airway Sampling
When available, BAL is preferred for collection of a lower airway sample rather than tracheal wash because the trachea and carina are not sterile, even in healthy dogs.15 In addition, the sensitivity for detecting cytologic features of sepsis is greater with BAL than tracheal wash.12 However, when only a tracheal wash specimen can be obtained, because of the lack of equipment for BAL or because of patient instability, collection of a lower airway sample is desirable to identify infecting bacteria and to determine appropriate antibiotic therapy through susceptibility testing.
BAL cell counts in animals with bacterial pneumonia are markedly higher than in patients with chronic bronchitis or other respiratory disease.14 Septic, suppurative inflammation is a reliable indicator of bacterial pneumonia in dogs14 and is likely to indicate bacterial pneumonia in cats. In those cases that lack evidence of airway sepsis (intracellular bacteria), BAL cytology generally reveals suppurative or mixed inflammation.13
In animals with suspected or confirmed foreign bodies, a BAL sample should always be obtained from the affected airway and submitted individually for cytologic analysis. Airway bacteria are more likely to be found in the cytologic sample from the site of the foreign body than from an alternate site.8 Furthermore, cytology of BAL samples obtained from multiple lobes can reveal different findings, even in cases of sterile inflammatory diseases like feline bronchial disease, thus reliance on a single-segment BAL cytology could lessen the chance of yielding diagnostic results.16
Microbiology
Diagnosis of bacterial pneumonia relies on identification of septic inflammation in conjunction with a positive bacterial culture. Aerobic and Mycoplasma culture and sensitivity are typically requested, and, in cases with markedly purulent secretions or a history of known aspiration or foreign bodies, anaerobic cultures should also be requested. Samples should be refrigerated in sterile containers until submitted. If multiple alveolar segments are sampled during BAL, these are usually are pooled for culture submission.
Cultures should always be performed when possible in order to guide appropriate antimicrobial therapy. With the liberal use of antibiotics, increasing populations of resistant microbes are being identified, particularly in patients with hospital-acquired pneumonia.17, 18 However, airway samples cannot be collected in all animals and, in those instances, judicious use of antibiotics must be followed.
Common bacteria cultured from lung washes of cats or dogs with bacterial pneumonia include enteric organisms (Escherichia coli, Klebsiella spp), Pasteurella spp, coagulase-positive Staphylococcus spp, beta-hemolytic Streptococcus spp, Mycoplasma spp, and B bronchiseptica (Table 4 ).4, 13, 27
Table 4.
Bacteria commonly isolated from airway samples of canine patients with pneumonia
| Organism | Percentage of Isolates |
|---|---|
| B bronchiseptica | 22-49 |
| E coli | 11-17 |
| Klebsiella pneumoniae | 2-6 |
| Pasteurella spp | 3-21 |
| Mycoplasma spp | 30-70 |
| Streptococcus spp | 6-13 |
| Staphylococcus spp | 14 |
| Anaerobes | 5-17 |
Pulmonary Function Testing
Arterial blood gas analysis is a useful test to measure the lung's ability to oxygenate. For patients with significant respiratory compromise, arterial blood samples ideally should be collected and analyzed to determine the severity of pulmonary disease. Furthermore, trends in arterial oxygen partial pressures can be used to track progression or resolution of disease. In many cases, blood gas analysis is not available or patient factors preclude the acquisition of samples. Pulse oximetry is a quick, noninvasive evaluation of oxygen delivery to body tissues that measures percentage of hemoglobin saturation with oxygen. It provides only a crude assessment of oxygenation and is subject to variability; however, trends in hemoglobin saturation can provide additional clinical support to progression or resolution of disease.
Treatment
Treatment of bacterial pneumonia varies considerably with the severity of disease, and appropriate antibiotic therapy is essential. The International Society for Companion Animal Disease is currently constructing guidelines for antibiotic therapy for respiratory infections. Pending those guidelines, antibiotic recommendations from previous literature should be considered (Table 5 ). For stable animals with mild disease, outpatient therapy consisting of administration of a single, oral antibiotic is often all that is necessary. Antimicrobial choices should ideally be based on culture and sensitivity results from airway lavage samples, although sometimes empiric therapy is more practical. Regardless, in cases of severe pneumonia, initial empiric therapy should be instituted while awaiting culture results. Antibiotics are typically administered for 3 to 6 weeks, and at least 1 to 2 weeks beyond the resolution of clinical and/or radiographs signs of disease.
Table 5.
Empiric antibiotic choice for patients with pneumonia
| Stable patient, mild clinical signs |
|
| Moderate clinical signs |
|
| Critical patient, severe clinical signs |
|
Abbreviations: IV, intravenous; PO, by mouth; SQ, subcutaneous.
Animals with more advanced disease require more intensive care, including hospitalization with intravenous fluids to maintain hydration. Adequate hydration is essential to facilitate clearance of respiratory exudates. Nebulization to create particles that enter the lower airways (<5 μm) can also enhance clearance of secretions. Nebulizer types include ultrasonic devices, compressed air nebulizers, and mesh nebulizers. Nebulization with sterile saline can be achieved by directing the hosing from the nebulizer into a cage or animal carrier covered in plastic. Depending on how viscous secretions are, therapy can be provided for 15 to 20 minutes 2 to 4 times daily. In many cases, nebulization coupled with coupage helps the animal expectorate airway secretions. Coupage is performed by cupping the hands and gently and rhythmically pounding on the lateral thoracic walls in dorsal to ventral and caudal to cranial directions. Coupage should not be performed in animals with regurgitation because any increase in intrathoracic pressure could exacerbate regurgitation and subsequent reaspiration.
Supplemental oxygen is necessary for animals with moderate to marked hypoxemia (documented by a Pao 2 less than 80 mm Hg or oxygen saturation via pulse oximetry less than 94% on room air) in conjunction with increased respiratory effort. Oxygen supplementation at 40% to 60% is provided until respiratory difficulty lessens and the animal can be weaned to room air. Animals with refractory pneumonia that fail to improve on supplemental oxygen can succumb to ventilatory fatigue and need to be referred to an intensive care facility for mechanical ventilation.
Administration of an oral mucolytic agent such as N-acetylcysteine can be useful for animals with moderate to severe bronchiectasis that are prone to recurrent pneumonia. Decreasing the viscosity of airway secretions might improve expectoration of fluid and debris that accumulates in dependent airways, although no published information is available on use of mucolytics in animals. N-acetylcysteine is typically not used via nebulization because of the risk of bronchoconstriction and epithelial toxicity. Under no circumstances are cough suppressants (such as butorphanol or hydrocodone) appropriate for use in the management of bacterial pneumonia, particularly when it is complicated by bronchiectasis. By decreasing the cough reflex, these drugs perpetuate retention of mucus, debris, and other material in the airways and therefore hinder clearance of infection. Also, furosemide should not be used because drying of secretions traps material in the lower airway and perpetuates infection.
In cases in which aspiration pneumonia is suspected, strategies should be used to reduce the chance of reaspirating through appropriate treatment of the underlying condition. With disorders of esophageal motility, upright feedings of either slurry or meatballs can enhance esophageal transit. Furthermore, diets low in fat can increase gastric emptying. In patients with refractory vomiting, antiemetic and prokinetic agents can be used to reduce the episodes of vomiting. Drugs like maropitant (Cerenia; 1 mg/kg subcutaneously once daily) or ondansetron (Zofran; 0.3-1 mg/kg intravenously or subcutaneously once to twice daily) act peripherally and centrally to decrease the urge to vomit and are safe to use in both cats and dogs.
The role of antacids in management of aspiration pneumonia remains controversial. By neutralizing the pH of gastric secretions, animals with refractory vomiting or regurgitation are less likely to succumb to chemical injury related to aspiration. However, in cases treated with acid suppression, the aspirant is likely to contain a greater concentration of bacteria that can colonize the lower airways and lead to bacterial pneumonia. No controlled studies have assessed the severity of aspiration pneumonia or the relative risk of using antacid therapy in dogs or cats.
Because radiographic findings lag behind clinical disease, recheck radiographs are not helpful early into the disease process, although they are useful to document resolution of disease and should be obtained within a week of discontinuation of antimicrobial therapy. In cases of refractory pneumonia, recheck radiographs midway through therapy can be used to assess resolution or progression of disease and help to guide further therapy.
In animals suspected of having contagious or multidrug-resistant pathogens, appropriate contact precautions should be used. Isolation gowns, examination gloves, and good hand washing technique along with appropriate quarantine facilities are essential to preventing transmission of disease to other patients or members of the health care team.
Prognosis
Prognosis for animals with bacterial pneumonia varies depending on the severity of disease, the animal's immunocompetence, and the virulence of the infectious agent. In general, between 77% and 94% of patients diagnosed with pneumonia are discharged from the hospital.4, 19 No long-term studies assess the overall prognosis of patients with multidrug-resistant bacteria or recurrent pneumonia. The outcome associated with these cases presumably will be worse.
Case studies
Case Study 1
An 8-year-old female spayed Chihuahua mix presented for a wet cough.
History
Cough had been present for 4 months and there had been minimal response to antibiotics combined with a cough suppressant and no response to heart failure medication (furosemide, enalapril, and pimobendan).
Physical examination
Temperature (38.9°C [102°F]), pulse (140 beats per minute [bpm]), and respiratory rate (30 breaths per minute) were normal. No murmur was auscultated and lung sounds were normal.
Diagnostic evaluation
Chronic cough in a small-breed dog is often associated with airway collapse or chronic bronchitis; however, infectious and neoplastic disease must remain on the differential list. Congestive heart failure is unlikely given the lack of a heart murmur and the lack of response to diuretic therapy.
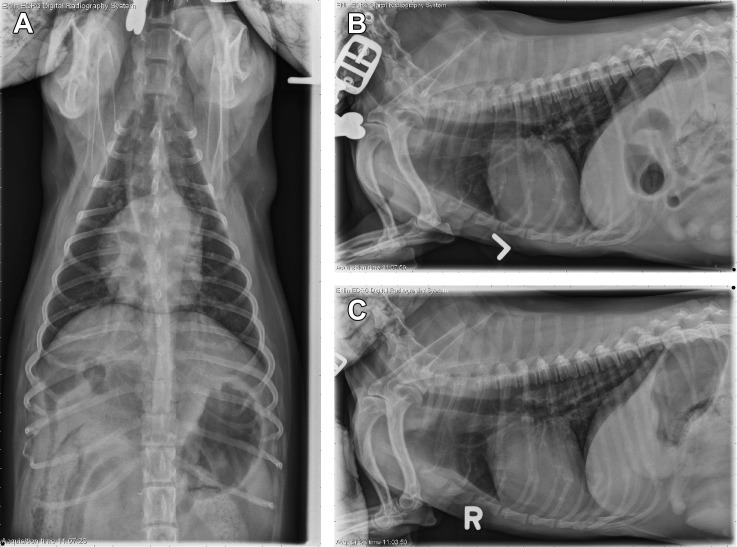
A white blood cell count was normal (5800 cells/μL) with 4400 neutrophils. Thoracic radiographs revealed scattered bronchial markings in the caudal thorax (Fig. 5 ). Fluoroscopic examination did not reveal evidence of tracheal or airway collapse. Laryngoscopy indicated lack of abduction of the arytenoid cartilages consistent with bilateral laryngeal paralysis. Secretions were evident throughout the upper and lower airways. Diffuse airway hyperemia and irregularities of the mucosa were apparent. BAL cytology was remarkable for septic suppurative inflammation, and bacterial cultures were positive for Pasteurella, Mycoplasma spp, and anaerobic bacteria, consistent with an aspiration cause.
Fig. 5.
Thoracic radiographs from case study 1 demonstrate a multifocal bronchial pattern throughout the caudal lung fields and a noticeable lack of alveolar infiltrates.
Case Study 2
A 5-year-old male castrated domestic medium hair cat was presented for evaluation of acute respiratory distress.
History
Lethargy and anorexia had been noted 3 days before the onset of respiratory signs.
Physical examination
Temperature (38.7°C [101.6°F]) and pulse (210 bpm) were normal. Tachypnea was noted (respiratory rate, 60 breaths per minute) with increased respiratory effort on inspiration and expiration. Diffuse expiratory wheezes were auscultated.
Diagnostic evaluation
Acute onset of respiratory difficulty in a cat is most commonly related to inflammatory airway disease. The physical examination is consistent with this diagnosis, although it is uncommon for affected cats to show lethargy and anorexia. Infectious and neoplastic diseases were also on the differential diagnosis list, along with aspiration and foreign body pneumonia.
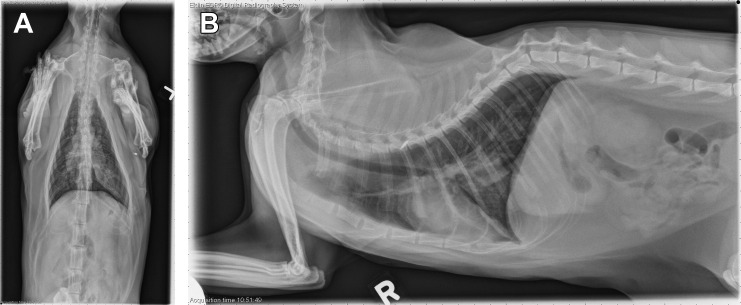
Thoracic radiographs revealed a focal opacity in the left caudal lung lobe and a diffuse bronchial pattern (Fig. 6 ). Complete blood count revealed a normal white blood cell count (8500/μL) with a left shift (6800/μL neutrophils, 1000/μL bands). Bronchoscopy with lavage was performed. A moderate amount of airway hyperemia and edema was noted along with purulent material obstructing several airways. BAL cytology showed increased cellularity (1500, normal 500 cells/μL) with neutrophilic inflammation (84%, normal 5%-8%). Neutrophils contained dark blue granular debris, suspicious for sepsis. Aerobic and anaerobic cultures were negative but a pure culture of Mycoplasma was isolated on special medium. A diagnosis of mycoplasma bronchopneumonia was made.
Fig. 6.
Thoracic radiographs from case 2 highlight a focal soft tissue opacity in the left caudal lung fields along with a diffuse bronchial pattern and a scant pneumothorax. A left lateral radiograph was not obtained.
Footnotes
Disclosures: None.
References
- 1.Leroy O., Vandenbussche C., Coffinier C. Community-acquired aspiration pneumonia in intensive care units. Epidemiological and prognosis data. Am J Respir Crit Care Med. 1997;156(6):1922–1929. doi: 10.1164/ajrccm.156.6.9702069. [DOI] [PubMed] [Google Scholar]
- 2.Tart K.M., Babski D.M., Lee J.A. Potential risks, prognostic indicators, and diagnostic and treatment modalities affecting survival in dogs with presumptive aspiration pneumonia: 125 cases (2005-2008) J Vet Emerg Crit Care (San Antonio) 2010;20(3):319–329. doi: 10.1111/j.1476-4431.2010.00542.x. [DOI] [PubMed] [Google Scholar]
- 3.Brownlie J., Mitchell J., Walker C.A. Mycoplasmas and novel viral pathogens in canine infectious respiratory disease. J Vet Intern Med (Seattle) 2013 http://www.vin.com/doc/?id=5820275 Available at: [Google Scholar]
- 4.Radhakrishnan A., Drobatz K.J., Culp W.T. Community-acquired infectious pneumonia in puppies: 65 cases (1993-2002) J Am Vet Med Assoc. 2007;230(10):1493–1497. doi: 10.2460/javma.230.10.1493. [DOI] [PubMed] [Google Scholar]
- 5.Workman H.C., Bailiff N.L., Jang S.S. Capnocytophaga cynodegmi in a rottweiler dog with severe bronchitis and foreign-body pneumonia. J Clin Microbiol. 2008;46(12):4099–4103. doi: 10.1128/JCM.00173-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tenwolde A.C., Johnson L.R., Hunt G.B. The role of bronchoscopy in foreign body removal in dogs and cats: 37 cases (2000-2008) J Vet Intern Med. 2010;24(5):1063–1068. doi: 10.1111/j.1939-1676.2010.0580.x. [DOI] [PubMed] [Google Scholar]
- 7.Schultz R.M., Zwingenberger A. Radiographic, computed tomographic, and ultrasonographic findings with migrating intrathoracic grass awns in dogs and cats. Vet Radiol Ultrasound. 2008;49(3):249–255. doi: 10.1111/j.1740-8261.2008.00360.x. [DOI] [PubMed] [Google Scholar]
- 8.Epstein S.E., Mellema M.S., Hopper K. Airway microbial culture and susceptibility patterns in dogs and cats with respiratory disease of varying severity. J Vet Emerg Crit Care (San Antonio) 2010;20(6):587–594. doi: 10.1111/j.1476-4431.2010.00587.x. [DOI] [PubMed] [Google Scholar]
- 9.Craven D.E., Hjalmarson K.I. Ventilator-associated tracheobronchitis and pneumonia: thinking outside the box. Clin Infect Dis. 2010;51(Suppl 1):S59–S66. doi: 10.1086/653051. [DOI] [PubMed] [Google Scholar]
- 10.Egberink H., Addie D., Belak S. Bordetella bronchiseptica infection in cats. ABCD guidelines on prevention and management. J Feline Med Surg. 2009;11(7):610–614. doi: 10.1016/j.jfms.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kogan D.A., Johnson L.R., Jandrey K.E. Clinical, clinicopathologic, and radiographic findings in dogs with aspiration pneumonia: 88 cases (2004-2006) J Am Vet Med Assoc. 2008;233(11):1742–1747. doi: 10.2460/javma.233.11.1742. [DOI] [PubMed] [Google Scholar]
- 12.Hawkins E.C., DeNicola D.B., Plier M.L. Cytological analysis of bronchoalveolar lavage fluid in the diagnosis of spontaneous respiratory tract disease in dogs: a retrospective study. J Vet Intern Med. 1995;9(6):386–392. doi: 10.1111/j.1939-1676.1995.tb03298.x. [DOI] [PubMed] [Google Scholar]
- 13.Johnson L.R., Queen E.V., Vernau W. Microbiologic and cytologic assessment of bronchoalveolar lavage fluid from dogs with lower respiratory tract infection: 105 cases (2001-2011) J Vet Intern Med. 2013;27(2):259–267. doi: 10.1111/jvim.12037. [DOI] [PubMed] [Google Scholar]
- 14.Peeters D.E., McKiernan B.C., Weisiger R.M. Quantitative bacterial cultures and cytological examination of bronchoalveolar lavage specimens in dogs. J Vet Intern Med. 2000;14(5):534–541. doi: 10.1892/0891-6640(2000)014<0534:qbcace>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 15.McKiernan B.C., Smith A.R., Kissil M. Bacterial isolates from the lower trachea of clinically healthy dogs. J Am Anim Hosp Assoc. 1984;20:139–142. [Google Scholar]
- 16.Ybarra W.L., Johnson L.R., Drazenovich T.L. Interpretation of multisegment bronchoalveolar lavage in cats (1/2001-1/2011) J Vet Intern Med. 2012;26(6):1281–1287. doi: 10.1111/j.1939-1676.2012.01016.x. [DOI] [PubMed] [Google Scholar]
- 17.Chalker V.J., Waller A., Webb K. Genetic diversity of Streptococcus equi subsp. zooepidemicus and doxycycline resistance in kennelled dogs. J Clin Microbiol. 2012;50(6):2134–2136. doi: 10.1128/JCM.00719-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foley J.E., Rand C., Bannasch M.J. Molecular epidemiology of feline bordetellosis in two animal shelters in California, USA. Prev Vet Med. 2002;54(2):141–156. doi: 10.1016/s0167-5877(02)00022-3. [DOI] [PubMed] [Google Scholar]
- 19.Kogan D.A., Johnson L.R., Sturges B.K. Etiology and clinical outcome in dogs with aspiration pneumonia: 88 cases (2004-2006) J Am Vet Med Assoc. 2008;233(11):1748–1755. doi: 10.2460/javma.233.11.1748. [DOI] [PubMed] [Google Scholar]
- 20.An D.J., Jeoung H.Y., Jeong W. A serological survey of canine respiratory coronavirus and canine influenza virus in Korean dogs. J Vet Med Sci. 2010;72(9):1217–1219. doi: 10.1292/jvms.10-0067. [DOI] [PubMed] [Google Scholar]
- 21.McBrearty A., Ramsey I., Courcier E. Clinical factors associated with death before discharge and overall survival time in dogs with generalized megaesophagus. J Am Vet Med Assoc. 2011;238(12):1622–1628. doi: 10.2460/javma.238.12.1622. [DOI] [PubMed] [Google Scholar]
- 22.Bedu A.S., Labruyere J.J., Thibaud J.L. Age-related thoracic radiographic changes in golden and Labrador retriever muscular dystrophy. Vet Radiol Ultrasound. 2012;53(5):492–500. doi: 10.1111/j.1740-8261.2012.01948.x. [DOI] [PubMed] [Google Scholar]
- 23.Watson P.J., Herrtage M.E., Peacock M.A. Primary ciliary dyskinesia in Newfoundland dogs. Vet Rec. 1999;144(26):718–725. doi: 10.1136/vr.144.26.718. [DOI] [PubMed] [Google Scholar]
- 24.Watson P.J., Wotton P., Eastwood J. Immunoglobulin deficiency in Cavalier King Charles spaniels with Pneumocystis pneumonia. J Vet Intern Med. 2006;20(3):523–527. doi: 10.1892/0891-6640(2006)20[523:idickc]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 25.Jezyk P.F., Felsburg P.J., Haskins M.E. X-linked severe combined immunodeficiency in the dog. Clin Immunol Immunopathol. 1989;52(2):173–189. doi: 10.1016/0090-1229(89)90170-0. [DOI] [PubMed] [Google Scholar]
- 26.Jameson P.H., King L.A., Lappin M.R. Comparison of clinical signs, diagnostic findings, organisms isolated, and clinical outcome in dogs with bacterial pneumonia: 93 cases (1986-1991) J Am Vet Med Assoc. 1995;206(2):206–209. [PubMed] [Google Scholar]
- 27.Pesavento P.A., Hurley K.F., Bannasch M.J. A clonal outbreak of acute fatal hemorrhagic pneumonia in intensively housed (shelter) dogs caused by Streptococcus equi subsp. zooepidemicus. Vet Pathol. 2008;45(1):51–53. doi: 10.1354/vp.45-1-51. [DOI] [PubMed] [Google Scholar]
- 28.Mellema M. Viral pneumonia. In: King L.G., editor. Textbook of respiratory disease in dogs and cats. Saunders; St Louis (MI): 2004. pp. 431–445. [Google Scholar]
- 29.Chalker V.J., Brooks H.W., Brownlie J. The association of Streptococcus equi subsp zooepidemicus with canine infectious respiratory disease. Vet Microbiol. 2003;95(1-2):149–156. doi: 10.1016/S0378-1135(03)00155-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knesl O., Allan F.J., Shields S. The seroprevalence of canine respiratory coronavirus and canine influenza virus in dogs in New Zealand. N Z Vet J. 2009;57(5):295–298. doi: 10.1080/00480169.2009.58624. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell J.A., Brooks H.W., Szladovits B. Tropism and pathological findings associated with canine respiratory coronavirus (CRCoV) Vet Microbiol. 2013;162(2-4):582–594. doi: 10.1016/j.vetmic.2012.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kawakami K., Ogawa H., Maeda K. Nosocomial outbreak of serious canine infectious tracheobronchitis (kennel cough) caused by canine herpesvirus infection. J Clin Microbiol. 2010;48(4):1176–1181. doi: 10.1128/JCM.02128-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keil D.J., Fenwick B. Canine respiratory bordetellosis: keeping up with an evolving pathogen. In: Carmichael L.E., editor. Recent advances in canine infectious disease. International Veterinary Information Service; 2000. [Google Scholar]
- 34.Chalker V.J., Owen W.M., Paterson C. Mycoplasmas associated with canine infectious respiratory disease. Microbiology. 2004;150(Pt 10):3491–3497. doi: 10.1099/mic.0.26848-0. [DOI] [PubMed] [Google Scholar]
- 35.Priestnall S., Erles K. Streptococcus zooepidemicus: an emerging canine pathogen. Vet J. 2011;188(2):142–148. doi: 10.1016/j.tvjl.2010.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Foster S.F., Martin P., Allan G.S. Lower respiratory tract infections in cats: 21 cases (1995-2000) J Feline Med Surg. 2004;6(3):167–180. doi: 10.1016/j.jfms.2003.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wood P.R., Hill V.L., Burks M.L. Mycoplasma pneumoniae in children with acute and refractory asthma. Ann Allergy Asthma Immunol. 2013;110(5):328–334. doi: 10.1016/j.anai.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]