Highlights
-
•
COC enables healthcare more effectively and improves clinical outcomes.
-
•
COC is also important for elderly ACO patients.
-
•
Increasing COC is beneficial for elderly patients with ACO in disease management.
Keywords: Elderly adults, Asthma-chronic obstructive pulmonary disease overlap, Continuity of care, Emergency department, Hospitalization
Abstract
Objective
To investigate associations between continuity of care (COC) and emergency department (ED) visits and hospitalization for chronic obstructive pulmonary disease (COPD) or asthma among elderly adults with asthma-COPD overlap (ACO).
Methods
A retrospective cohort study was performed using the Taiwan National Health Insurance research database. A total of 1141 ACO patients aged ≥65 years during 2005–2011 were observed and followed for 2 years. The Bice and Boxerman COC index (COCI) was used to evaluate COC by considering ambulatory care visits duo to COPD or asthma in the first year; ED visits and hospitalization for COPD or asthma were identified in the subsequent year, respectively. The COCI was divided into three levels (COCI < 0.3= low, 0.3 ≤ COCI<1=medium, COCI = 1=high). The Cox model was used to estimate the hazard ratio (HR) for ED visits and hospital admissions due to COPD or asthma.
Results
The average COCI was 0.55. 21.3% patients received outpatient care from a single physician. Compared to patients with high COC, those with low and medium COC had a higher risk of ED visits (aHR = 2.80 and 2.69, P < .01) and admissions (aHR = 1.80 and 1.72, P < .05).
Conclusion
Increasing COC is beneficial for elderly patients with ACO in disease management. Policymakers could create effective pay-for-performance programs for the elderly ACO population to enhance COC and improve care outcomes.
1. Introduction
Asthma–chronic obstructive pulmonary disease (COPD) overlap (ACO) is characterized by persistent airflow limitation with several similar features associated with asthma and COPD [1]. Global Initiative for Asthma (GINA) and Global Initiative for Chronic Obstructive Lung Disease (GOLD) recognized ACO to notice clinicians, researchers and regulators being aware of these patients because of complex conditions [2]. Studies of ACO reported the prevalence ranges from 0.9% to 11.1% among general population around the world [3]. The disease burden and healthcare utilization such as emergency department (ED) visits and hospital admissions for patients with ACO has been found to be higher than those with asthma or COPD alone [[4], [5], [6], [7], [8], [9]]. While the importance of caring for patients with ACO has become a critical issue, there is limited information regarding treatment in ACO patients to reduce the resulting healthcare utilization. Additionally, there was a greater increase in the proportion of patients with ACO with increasing age [7,8,10]. Hence, an investigation of elderly patients with ACO is necessary because our society is aging.
Previous literature demonstrated that appropriate asthma or COPD control leads to high quality of life and lower healthcare utilization [11]. Therefore, the Agency of Healthcare Research and Quality (AHRQ) [12] and the Centers for Medicare and Medicaid Services (CMS) [13] have identified admissions for COPD or asthma in older adults as a prevention quality indicator (PQI), which may be avoided under more effective treatment in outpatient care. In regard with disease management especially for chronic diseases, continuity of care (COC), is a crucial element of primary care [14] to improve clinical outcomes by consistent and seamless treatment between patients and physicians over time [15]. Previous studies revealed COC is associated with healthcare outcomes in elderly patients with asthma or COPD, respecitively [[16], [17], [18], [19], [20], [21], [22], [23]]. These studies supported higher COC is associated with fewer ED visits [[16], [17], [18]] and hospitalizations [16, [18], [19], [20], [21], [22], [23], and lower healthcare cost [16,18]. However, the potential impact of COC and the therapeutic relationship between physician and patient, in which improvements in healthcare outcomes such as ED visits or hospital admissions due to asthma or COPD for elderly adults with ACO, is not sufficiently understood. Therefore, to examine the association between COC and care outcomes among ACO population is worthwhile for patients, clinicians and policy regulators in disease management and policy development.
The Taiwanese government implemented a single-payer National Health Insurance (NHI) program in March 1995 and approximately 99% of Taiwan’s 23 million residents are enrolled in this program [24]. The NHI program provides universal and compulsory health insurance to strengthen accessibility of health care services and to reduce patients’ financial barriers. Under the NHI program, patients can freely visit any health care provider at any level without referral [25]. Due to features of this healthcare system, patients with ACO may seek out one or more physicians to care for their health, which leads increase outpatient care visits. However, there is no evidence reporting the relationship between COC and healthcare outcomes for these elderly patients. Therefore, exploration of the COC and its effects on healthcare outcomes among elderly ACO patients may offer new contributions to extend current literature regarding healthcare outcomes. For this reason, the aim of this study is to investigate whether high COC reduces the risk of ED visits and hospital admissions for COPD or asthma among elderly patients with ACO under a national insurance system.
2. Methods
2.1. Study data and design
This retrospective cohort study is based on claim data collected from 2004 to 2013 from the longitudinal Health Insurance Database for 2010 (LHID2010) and consists of a million randomized beneficiaries in 2010 from the entire National Health Insurance (NHI) enrollee maintained by the National Health Research Institute. All selected beneficiaries were retrospected to 1996 and followed to 2013. The claim data contain comprehensive personal and healthcare care records, such as cryptographic identification for each patient and physician, patient’s gender, date of birth, and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for primary and secondary diseases. There were no significant differences in the distributions of age or gender between patients in the LHID2010 and the nationwide databases [26]. Therefore, the LHID2010 database is representative of the entire population. The years between 2004 and 2013 were selected in this study because of Severe Acute Respiratory Syndrome (SARS) outbreak in Taiwan from March 14 to May 22 in 2003 [27]. The institutional review board at National Yang-Ming University of Taiwan approved this study (IRB Approval Number: YM103047E).
2.2. Study subjects
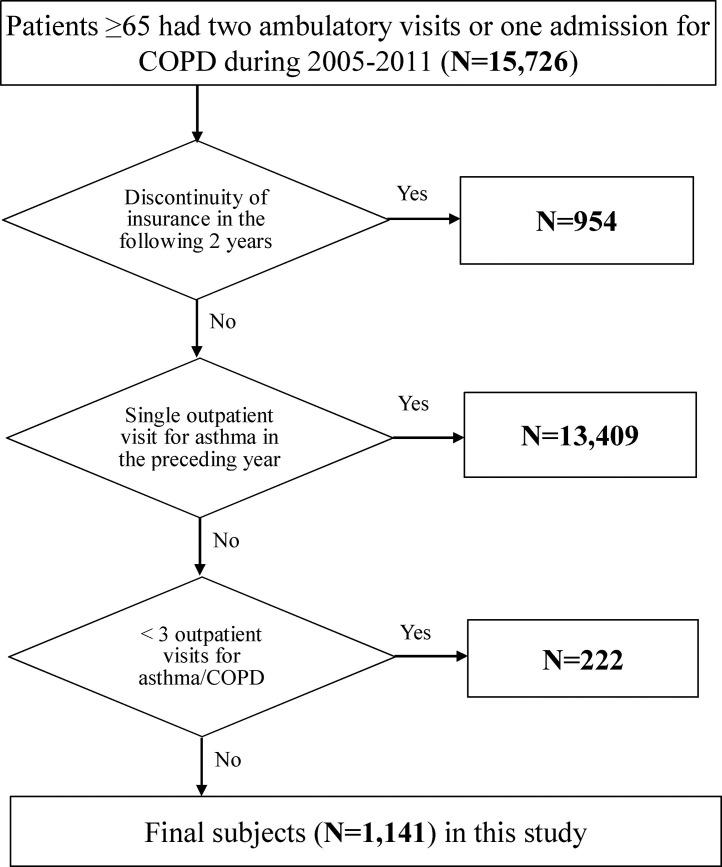
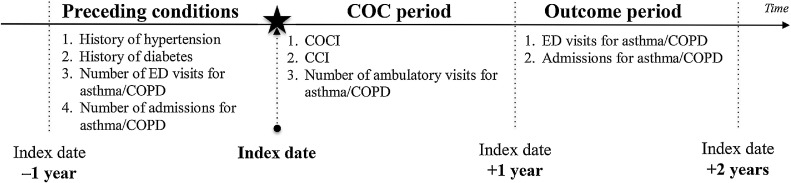
There were 15,762 patients aged ≥65 years who either had at least 2 outpatient visits or 1 inpatient admission for COPD as a primary diagnosis (ICD-9-CM codes: 491.xx, 492.xx, 496.xx) [5,6,28,29] identified during the period from January 1, 2005, to December 31, 2011. The index date was set as the earliest date for patients who had a record during this period. Patients who were not continuously enrolled in the NHI program (n = 954) until the end of study period were excluded. To identify ACO patients, patients without ≥2 outpatient visit claims or 1 inpatient admission for asthma (ICD-9-CM code 493.xx) in a prior year of index date [29,30] were excluded (n = 13,409). In order to calculate a stable COC value that requires ≥3 outpatient visits; therefore, patients had <3 outpatient visits during the COC period were excluded (n = 222). In total, 1141 patients were included (Fig. 1 ). To avoid time-dependent bias and incorrect conclusions [31], we followed each patient for 2 years after the index date. The first year was the COC period, and the subsequent year was the outcome period (Fig. 2 ).
Fig. 1.
A flow chart demonstrating study subject selection. COPD = Chronic Obstructive Pulmonary Disease.
Fig. 2.
A framework for this study. COPD = Chronic Obstructive Pulmonary Disease, COC = continuity of care, COCI = continuity of care index, CCI = Charlson comorbidity index, ED = emergency department.
2.3. ED visits and hospital admissions
Two interesting outcomes in our study concerned ED visits and hospital admissions for either COPD or asthma. According to the PQI for COPD or asthma in older adults proposed by AHRQ and CMS, a certain number of ED visits and hospital admissions for asthma (ICD-9-CM codes: 493.xx in the primary diagnosis) or COPD ((1) ICD-9-CM codes: 4910, 4911, 49120, 49121, 4918, 4919, 4920, 4928, 494, 4940, 4941, and 496 in the primary diagnosis; (2) ICD-9-CM codes: 4660 and 490 must combined with a secondary diagnosis code of COPD) were identified [12,13]. ED visits and hospital admissions were separately defined as an independent event that occurred during the outcome period for each patient. The follow-up duration was defined as the number of days from the date of the end of the COC period to the date of the first ED visit or hospitalization for COPD or asthma, respectively. If a patient had no ED visits or hospital admissions in this period, then that the patient was censored at the end of the outcome period.
2.4. Continuity of care index
We applied the Bice and Boxerman COC index (COCI) [32] as our primary dependent variable. COCI represents the concentration of visits to individual physicians and has been widely employed in studies using claim data sets [[16], [17], [18], [19], [20]]. In addition, the index is suitable for a higher number of outpatient visits [33] because it is less sensitive to the number of physician visits [34]. The COCI score, ranging from 0 to 1, measures the dispersion of contact between patient and physician, and the value close to 1 that represents greater COC. The general formula is
Where N is the total number of physician visits, ni is the number of visits to the physician, and k is the total number of physicians. The total number of physician visits (N) and the number of visits to a given physician (ni) included ambulatory claims (clinic or hospital physician visits) due to asthma or COPD as the principal diagnosis. COCI was categorized into three level (low (COCI < 0.3), medium (0.3 ≤ COCI<1) and high (COCI = 1)) [16,35].
2.5. Covariates
A number of control variables were considered in our study. Patients’ characteristics at baseline were age, gender and insurance premiums (low: <US$667, medium: US$667-1333, high: ≥US$1333). The average monthly minimum wage in Taiwan was around 20,000 N T dollars in this study period ($US667, one US dollar was equal to 30 New Taiwan dollars in 2012) [36]. Therefore, we used US$667 and doubled this amount (US$1333) to categorize three levels of insurance premiums [37]. Due to the relationship between socioeconomic status (SES) and health care outcomes [38,39], insurance premiums were used as a proxy for SES because the NHI claims data set does not provide patients’ educational levels or household incomes. In addition, health status and disease severity may affect the measurement of health outcomes [6,9,16,39]; therefore, any history of hypertension (ICD-9-CM codes 401.xx-405.xx), and diabetes (ICD-9-CM codes 250.xx) [4,6,9], whether a patient had ED visits for COPD or asthma and whether a patient was hospitalized for COPD or asthma were included in the previous year of the index date. The Charlson comorbidity index (CCI) [4,5,7,40] that was calculated for each patient according to outpatient or inpatient care by using the Quan adaptation of the Elixhauser comorbidities [41] and the number of outpatient visits for COPD or asthma (3–12, 13–24, and ≥25 times) [16] was measured during the COC period.
2.6. Statistical analysis
This study used descriptive statistical analyses to present the distribution of subjects’ characteristics and performed χ 2 tests and one-way analyses of variance to analyze the associations between subjects’ characteristics and COC. The Cochran-Armitage trend test was used to evaluate the association of both ED visit and hospital admission for COPD or asthma with the level of COC. Furthermore, with the valid proportional hazard assumption for ED visit and hospital admission [42], Cox regression models were used to examine the association between COC levels and the risk of ED visits and hospital admission for COPD or asthma in elderly patients with ACO. In the adjusted model, we calculated the adjusted hazard ratio (aHR) after adjusting for sex, age, insurance premium, history of hypertension and diabetes, ED visits for COPD or asthma, hospital admissions for COPD or asthma, CCI and number of ambulatory visits for COPD or asthma. All variables had no multicollinearity in our model. All statistical analyses and data management were conducted using SAS software version 9.4 (SAS Institute, Cary, NC). All tests were 2-sided and P values of <0.05 were considered statistically significant.
3. Results
The average COCI of older ACO patients was 0.55 (standard deviation = 0.3). A total of 243 patients (21.3%) had index values of 1, indicating maximum or all outpatient care received from the same physician. There were 644 (56.4%) and 254 (22.3%) of 1141 patients in the medium (0.3 ≤ COCI<1) and low (COCI < 0.3) COC groups, respectively. The mean age was 74.4 years, and men comprised 61.3% of the patients. Furthermore, 38.2% of the patients had a low insurance premium level. Regarding medical conditions in a preceding year, the percentage of patients who had hypertension and diabetes was 33.6% and 10.4%. 11.4% and 12.2% of the patients had at least one ED visits and admissions, respectively. Regarding the number of ambulatory visits for COPD or asthma during the COC period, 59.8% of the patients had 3 to 12 ambulatory visits. The overall rate for ED visits was 12.6%, and a negative association was found across all levels of COCI (high: 4.9%, medium: 14.6%, and low: 15.0%; P for trend <0.001). The overall rate for hospital admissions was 13.0% and the rate of admissions increased when COCI decreased (high: 7.8%, medium: 14.0%, and low: 15.4%; P for trend = 0.013). The characteristics of all patients and of each COC group are shown in Table 1 .
Table 1.
Characteristics in subjects aged 65+ by continuity of care index group (N=1141).
| Characteristics | % | Level of COCI (%) |
P valuea | ||
|---|---|---|---|---|---|
| <0.3 (n=254) | 0.3-0.99 (n=644) | 1 (n=243) | |||
| Total | 100.0 | 22.3 | 56.4 | 21.3 | |
| Demographics at baseline | |||||
| Gender | 0.711 | ||||
| Female | 38.7 | 36.6 | 39.6 | 38.7 | |
| Male | 61.3 | 63.4 | 60.4 | 61.3 | |
| Age (mean ±SD) | 74.4(6.2) | 74.4(6.6) | 74.4(5.8) | 74.3(6.5) | 0.985b |
| Insurance premium (USD) | 0.767 | ||||
| < 667 | 38.2 | 40.2 | 38.0 | 36.6 | |
| 667-1333 | 44.5 | 44.8 | 44.6 | 44.0 | |
| ≥1333 | 17.3 | 15.0 | 17.4 | 19.4 | |
| Medical conditions | |||||
| In preceding year | |||||
| History of hypertension | 0.654 | ||||
| No | 66.4 | 64.2 | 67.4 | 66.3 | |
| Yes | 33.6 | 35.8 | 32.6 | 33.7 | |
| History of diabetes | 0.783 | ||||
| No | 89.6 | 89.4 | 90.1 | 88.5 | |
| Yes | 10.4 | 10.6 | 9.9 | 11.5 | |
| ED visits for asthma/COPD | 0.313 | ||||
| No | 88.6 | 86.6 | 88.5 | 91.0 | |
| Yes | 11.4 | 13.4 | 11.5 | 9.1 | |
| Admissions for asthma/COPD | 0.638 | ||||
| No | 87.8 | 86.2 | 88.5 | 87.7 | |
| Yes | 12.2 | 13.8 | 11.5 | 12.4 | |
| In the COC period | |||||
| CCI (mean ±SD) | 1.3(1.5) | 1.4(1.6) | 1.3(1.5) | 1.2(1.4) | 0.489b |
| No. of ambulatory visits | <.001 | ||||
| 3-12 | 59.8 | 62.2 | 53.6 | 73.7 | |
| 13-24 | 34.9 | 30.7 | 41.2 | 22.6 | |
| ≥25 | 5.4 | 7.1 | 5.3 | 3.7 | |
| Healthcare outcome | |||||
| ED visits for asthma/COPD | <.001 | ||||
| No | 87.4 | 85.0 | 85.4 | 95.1 | |
| Yes* | 12.6 | 15.0 | 14.6 | 4.9 | |
| Admissions for asthma/COPD | 0.023 | ||||
| No | 87.0 | 84.7 | 86.0 | 92.2 | |
| Yes** | 13.0 | 15.4 | 14.0 | 7.8 | |
COPD: Chronic Obstructive Pulmonary Disease; COCI: continuity of care index; CCI: Charlson Comorbidity Index; ED: emergency department.
Overall COC mean=0.55(SD=0.3).
χ2 test for difference level of COCI.
One-way ANOVA test.
P for trend <0.001.
P for trend <0.013.
The results of Cox proportional regression are presented in Table 2 . After adjustment, the patients in either the low or medium COC group had a significantly higher risk of ED visits for COPD or asthma compared with the patients in the high COC group (aHR, 2.80; 95% confidence interval [CI], 1.45–5.38; aHR, 2.69; 95% CI, 1.47–4.93, respectively). In addition, the risk of ED visits was associated with a statistically significant increase of 4% for each additional year of age (aHR, 1.04; 95% CI, 1.01–1.07). Patients who had ED visits (aHR, 2.87; 95% CI, 1.93–4.26) or admissions (aHR, 1.63; 95% CI, 1.09–2.46) for COPD or asthma in the previous year had higher risks of ED visits for COPD or asthma than those who had no ED visits or admissions. Compared to the patients having 3–12 ambulatory visits, the patients having 13–24 or ≥25 ambulatory visits during the COC period were 100% (aHR, 2.00; 95% CI, 1.39–2.88) or 191% (aHR, 2.91; 95% CI, 1.67–5.08) more likely to have ED visits for COPD or asthma, respectively.
Table 2.
Factors associated with ED visits and hospital admissions for COPD or asthma among ACO patients aged 65+ using Cox models (N=1141).
| ED visits |
Hospital admissions |
|||||||
|---|---|---|---|---|---|---|---|---|
| Crude model |
Adjusted model |
Crude model |
Adjusted model |
|||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| COCI | ||||||||
| 1 (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 0.3-0.99 | 3.11 | 1.70-5.66 | 2.69 | 1.47-4.93 | 1.85 | 1.13-3.03 | 1.72 | 1.04-2.83 |
| <0.3 | 3.22 | 1.68-6.15 | 2.80 | 1.45-5.38 | 2.04 | 1.18-3.53 | 1.80 | 1.03-3.13 |
| Patient characteristics at baseline | ||||||||
| Gender | ||||||||
| Female (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Male | 1.33 | 0.94-1.88 | 1.21 | 0.84-1.74 | 1.49 | 1.05-2.11 | 1.49 | 1.03-2.13 |
| Age (years) | 1.04 | 1.01-1.06 | 1.04 | 1.01-1.07 | 1.03 | 1.00-1.05 | 1.02 | 0.99-1.05 |
| Insurance premium (USD) | ||||||||
| <667 (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 667-1333 | 1.14 | 0.80-1.61 | 1.24 | 0.86-1.77 | 0.91 | 0.65-1.29 | 0.98 | 0.69-1.40 |
| ≥1333 | 0.54 | 0.30-0.96 | 0.73 | 0.40-1.33 | 0.61 | 0.36-1.02 | 0.75 | 0.44-1.28 |
| Medical conditions | ||||||||
| In a previous year | ||||||||
| History of hypertension | ||||||||
| No (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.70 | 0.48-1.00 | 0.81 | 0.55-1.18 | 0.94 | 0.67-1.33 | 0.99 | 0.70-1.41 |
| History of diabetes | ||||||||
| No (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.70 | 0.38-1.30 | 1.05 | 0.55-1.99 | 0.98 | 0.57-1.67 | 1.12 | 0.64-1.96 |
| ED visits for asthma/COPD | ||||||||
| No (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 4.25 | 2.99-6.04 | 2.87 | 1.93-4.26 | 2.81 | 1.93-4.10 | 1.83 | 1.21-2.77 |
| Admissions for asthma/COPD | ||||||||
| No (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 2.56 | 1.75-3.75 | 1.63 | 1.09-2.46 | 3.01 | 2.09-4.32 | 2.39 | 1.62-3.51 |
| In the COC period | ||||||||
| CCI | 0.93 | 0.83-1.05 | 0.96 | 0.85-1.08 | 1.03 | 0.93-1.14 | 1.04 | 0.93-1.16 |
| No. of ambulatory visits | ||||||||
| 3-12 (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 13-24 | 2.56 | 1.79-3.65 | 2.00 | 1.39-2.88 | 1.65 | 1.17-2.31 | 1.39 | 0.98-1.97 |
| ≥25 | 4.96 | 2.93-8.39 | 2.91 | 1.67-5.08 | 2.69 | 1.54-4.71 | 1.85 | 1.03-3.31 |
COCI, continuity of care index; CCI, Charlsons' Comorbidity Index; COPD, Chronic Obstructive Pulmonary Disease; ED, emergency department.
A similar trend was found in hospital admissions (Table 2). The risk of hospital admissions for COPD or asthma for patients in the low and medium COC group was significantly higher than for those in the high COC group (aHR, 1.80; 95% CI, 1.03–3.13; aHR, 1.72; 95% CI, 1.04–2.83, respectively). Male patients had a higher risk of hospital admission than female (aHR, 1.49; 95% CI, 1.03–2.13). Compared to the patients without ED visits or admissions for COPD or asthma in the previous year, patients had higher risk of hospital admissions if they experienced ED visits (aHR, 1.83; 95% CI, 1.21–2.77) or admissions (aHR, 2.39; 95% CI, 1.62–3.51). The patients having ≥25 ambulatory visits (aHR, 1.85; 95% CI, 1.03–3.31) during the COC period had a higher risk of hospital admissions for COPD or asthma than those who had 3–12 ambulatory visits. No significant interactions were observed between the COC groups and other variables in all regression models.
4. Discussion
This study used the Taiwanese nationwide claims data to examine the association between COC and ED visits and hospitalization for COPD or asthma among the elderly ACO patients. The findings of this study revealed that 21.3% of older patients with ACO had the highest score of COCI (COCI = 1) during the first observational year, and the average COCI was 0.55 among the study population. Previous studies reported that the mean of COCI in elderly patients with COPD ranged 0.49–0.71 [16,18,21,23] and in elderly asthmatic patients the mean ranged from 0.66 to 0.73 [16,17,22]. On the other hand, studies revealed the mean of COCI was around 0.3 among senior population when COC was estimated by considering for any condition [35,43,44]. A high COC score for the elderly patients with ACO might be attributable to the asthma pay-for-performance (P4P) program. The Taiwan government launched the asthma P4P program in 2001 to encourage clinics and hospitals to provide patient-centered care and focus on disease management. This program proposed a guideline-based practice with financial incentives. Except for the regular reimbursement for health care services, physicians (internist, pediatrician, family physician, and otorhinolaryngologist) who acquire asthma care training at least eight hours can receive additional compensates including case management fees and enlarged physician fees if their patients have a high follow-up rate and a low rate of hospitalization and ED visits for asthma. Previous studies focusing on asthma care found that the asthma P4P program in Taiwan might ameliorate COC score for elderly patients [17] and children [45]. Additionally, the benefit of P4P programs in improving COC as well as health outcomes was found among patients with diabetes [46].
Our study demonstrates that COC plays a critical role in the reduction of ED visits and hospitalization for asthma or COPD among older ACO patients under a free access policy. The findings were also supported by the previous literature [43]. We also observed that 56%, 17% and 12% (unpublished data) of elderly ACO patients in the high COC group (COCI = 1) sought internist, pulmonary and critical care medicine specialist and family physician to take care of their overlapping problem. Unlike most citizens who seek care first through a primary care physician in the United States, patients in Taiwan enjoy easy access physicians either in a community clinic or in a hospital outpatient care without a referral when they seek care [25]. In this free access policy, these patients directly selected their principal outpatient care providers by themselves. In addition, the Taiwan NHI Administration launched the P4P program to enhance disease management from healthcare providers. Those could be the reason why these patients had a high COC.
Elderly ACO patients with lower COCI showed a significantly higher risk of ED visits and hospital admissions related to COPD or asthma than those with higher value of continuity. These findings support the prior literatures that associated superior COC with fewer ED visits and inpatient admissions in aging populations with different single chronic disease such as asthma or COPD alone [[16], [17], [18], [19], [20], [21]]. These findings might indicate that COC is important for older patients with ACO. They would receive timely and efficient care because their healthcare providers has obtained and become familiar with the details of their disease condition. Therefore, we suggest that these patients with low COC should attempt to increase COC in order to reduce the risk of either ED visits or hospital admissions for COPD or asthma because patients have a higher COC, which represents better interpersonal relationships between patients and their physicians and better care outcomes. This robust partnership between patient and physician can be favorable for both patients and the health care system.
Our data also suggests that elderly patients with ACO who had >12 outpatient visits for COPD or asthma in a calendar year should be more diligent regarding follow-up care. Those patients had a significant risk increase for ED visits and hospitalizations of COPD or asthma than those having 3–12 outpatient visits. The increased tendency in the rates of ED visit and admission for COPD or asthma in those patients with decreased COC levels further supports that COC might play a much more crucial role for those patients to reduce the risk of ED visits and admissions.
Many indices were developed to evaluate COC such as COCI, Herfindhal Index, usual provider of care index (UPC), and Sequential Continuity of Care Index (SECON) in claims data [47]. COCI reflects the dispersion of contact between patients and physicians [32]. This index identifies visit concentration of a patient with each physician. The UPC, a density measure, focuses on the number of visits to the most frequently visited physicians, which cannot recognize whether patients reduce their visits or change healthcare providers frequently [48]. SECON determines the sequences of change in healthcare process, but it is limited to the detection of non-sequential issues [49]. The COCI, a most useful and common index, is adopted to measure for COC [50]. Additionally, compared with UPC and SECON, the COCI is suitable for a higher number of outpatient visits [33] because it is less sensitive to the number of physician visits [34]. Therefore, COCI was selected as our primary dependent variable to measure COC.
In light of the effect of the P4P program of asthma care and COC is vital for COPD patients from our previous studies [20,23], the Taiwan NHI Administration has launched the COPD P4P program in 2017. ACO, which does not describe a single disease entity, likely includes patients with several different forms of airways phenotypes caused by a range of different mechanisms. However, there is limited evidence to investigate in regard of treating ACO [2]. This study used comprehensive data from a health care system with free access policy to provide the evidence that better COC is related to lower risk of ED visits and hospitalization for COPD or asthma among elderly ACO patients. Therefore, we suggest that policymakers could consider designing a program that focused on ACO to improve COC and disease-controlling ability.
This study has some limitations. First, the claims data did not include clinical data such as peak expiratory flow or forced expiratory volume to identify ACO [40]. Therefore, we used ICD-9-CM codes to define ACO as done in previous studies [4,6,29]. Second, the claims data lacks personal anthropometric measurements such as body mass index [39,40] and smoking status [39,51,52] that may affect healthcare outcomes. Therefore, we adopted ED visits and admissions for COPD or asthma as well as the frequency of ambulatory visits for COPD or asthma in the COC period as proxies for disease severity [9,52]; also, we used patients’ history of hypertension and diabetes and CCI as proxy indicators to present each patient’s health status [5,40]. Third, we used insurance premiums as an indicator to represent patients’ socioeconomic status because the database could not provide patients’ educational level or household income, which may affect the measurement of COC and outcomes [8]. Forth, we excluded patients who had less than three outpatient visits during the COC period, which might limit the generalizability for elderly patients with ACO. Finally, claim-based COC measurements could offer only limited aspects of information regarding COC [33,53] and fails to incorporate the view of COC from patient-centered point of view [54,55] because measures are based on the patterns of patient encounters during a time period.
Although some limitations exist, the study has several strengths. First, this retrospective cohort study presents stronger evidence of the association between COC and healthcare outcomes than a cross-sectional study. Second, the dataset are highly representative of the entire population because 99% of Taiwanese residents enroll in the NHI program which may reduce selection bias. Third, using the nationwide electronic health records (EHR) databases can reduce the effect of recall bias and make our results more informative. Fourth, this study focuses on ACO instead of either COPD or asthma, and provides empirical evidence of an adverse association between COC and the risk of ED visit and hospital admission. Fifth, this study adopted COCI which is the most commonly used index to measure the degree of coordination required between different providers during a clinical episode. Finally, the COCI was measured by continuity relationship between patients and physician, which may provide information that is superior to that obtained from measurements between patients and institutions.
5. Conclusion
An adverse association exists between COC and the risk of ED visits and hospital admissions for COPD or asthma among elderly patients with ACO in Taiwan. Elderly ACO patients with higher COC were more likely to have lower risk of ED visits and hospital admissions for asthma or COPD. Therefore, elderly ACO patients should be encouraged to concentrate on few physicians they trust and to develop a long-term relationship with these physicians to enhance disease management. Policymakers could initiate P4P programs of ACO to motivate physicians and patients to enhance COC and disease control for reducing the ED visit and hospitalization.
Conflict of interest statement
None declared.
Funding source
This work was supported by grants from the Ministry of Science and Technology Taiwan (MOST 103-2410-H-010-011-MY2, MOST 105-2410-H-010–011-MY2, and MOST 106-2917-I-564-039).
Acknowledgements
The authors thank to the National Health Research Institutes for providing the National Health Insurance Research Database.
Contributor Information
Yu-Hsiang Kao, Email: ykao1@lsuhsc.edu.
Tung-Sung Tseng, Email: ttseng@lsuhsc.edu.
Yee-Yung Ng, Email: yyngscwu12@gmail.com.
Shiao-Chi Wu, Email: scwu@ym.edu.tw.
References
- 1.Postma D.S., Rabe K.F. The asthma–COPD overlap syndrome. The New England Journal of Medicine. 2015;373:1241–1249. doi: 10.1056/NEJMra1411863. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Asthma and Global Initiative for Chronic Obstructive Pulmonary Disease . 2017. Diagnosis and initial treatment of asthma, COPD, and asthma-COPD overlap.http://ginasthma.org/download/824/ [Accessed 13 September, 2018] [Google Scholar]
- 3.Uchida A., Sakaue K., Inoue H. Epidemiology of asthma-chronic obstructive pulmonary disease overlap (ACO) Allergology International. 2018;67:165–171. doi: 10.1016/j.alit.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Shantakumar S., Pwu R.F., D’Silva L., Wurst K., Kuo Y.W., Yang Y.Y. Burden of asthma and COPD overlap (ACO) in Taiwan: a nationwide population-based study. BMC Pulmonary Medicine. 2018;18:16. doi: 10.1186/s12890-017-0571-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaya F.T., Dongyi D., Akazawa M.O., Blanchette C.M., Wang J., Mapel D.W. Burden of concomitant asthma and COPD in a Medicaid population. Chest. 2008;134:14–19. doi: 10.1378/chest.07-2317. [DOI] [PubMed] [Google Scholar]
- 6.Wurst K.E., St. Laurent S., Hinds D., Davis K.J. Disease burden of patients with asthma/COPD overlap in a US claims database: impact of ICD-9 coding-based definitions. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2017;14:200–209. doi: 10.1080/15412555.2016.1257598. [DOI] [PubMed] [Google Scholar]
- 7.Blanchette C.M., Broder M., Ory C., Chang E., Akazawa M., Dalal A.A. Cost and utilization of COPD and asthma among insured adults in the US. Current Medical Research and Opinion. 2009;25:1385–1392. doi: 10.1185/03007990902875927. [DOI] [PubMed] [Google Scholar]
- 8.De Marco R., Pesce G., Marcon A., Accordini S., Antonicelli L., Bugiani M. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One. 2013;8 doi: 10.1371/journal.pone.0062985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhee C.K., Yoon H.K., Yoo K.H., Kim Y.S., Lee S.W., Park Y.B. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2014;11:163–170. doi: 10.3109/15412555.2013.831061. [DOI] [PubMed] [Google Scholar]
- 10.Zeki A.A., Schivo M., Chan A., Albertson T.E., Louie S. The asthma-COPD overlap syndrome: a common clinical problem in the elderly. Journal of Allergy (Cairo) 2011;2011 doi: 10.1155/2011/861926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vogelmeier C.F., Criner G.J., Martinez F.J., Anzueto A., Barnes P.J., Bourbeau J. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report. European Respiratory Journal. 2017;22:575–601. doi: 10.1111/resp.13012. [DOI] [PubMed] [Google Scholar]
- 12.Agency of Healthcare Research and Quality Prevention quality indicators technical specifications version 4.3. http://www.qualityindicators.ahrq.gov/Downloads/Modules/PQI/V43/TechSpecs/PQI%2005%20Chronic%20Obstructive%20Pulmonary%20Disease%20or%20Asthma%20in%20Older%20Adults%20Admission%20Rate.pdf [Accessed 20 December, 2017]
- 13.Centers for Medicare & Medicaid Services . 2012. ACO #9 – prevention quality Indicator (PQI): ambulatory sensitive conditions admissions for chronic obsructive pulmonary disease (COPD) or asthma in older adults.https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Measure-ACO-9-Asthma.pdf [Accessed 20 December, 2017] [Google Scholar]
- 14.Haggerty J.L., Reid R.J., Freeman G.K., Starfield B.H., Adair C.E., McKendry R. Continuity of care: a multidisciplinary review. British Medical Journal. 2003;327:1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dreiher J., Comaneshter D.S., Rosenbluth Y., Battat E., Bitterman H., Cohen A.D. The association between continuity of care in the community and health outcomes: a population-based study. Israel Journal of Health Policy Research. 2012;1:21. doi: 10.1186/2045-4015-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong J.S., Kang H.C., Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. Journal of Korean Medical Science. 2010;25:1259–1271. doi: 10.3346/jkms.2010.25.9.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kao Y.H., Wu S.C. Effect of continuity of care on emergency department visits in elderly patients with asthma in Taiwan. Journal of the American Board of Family Medicine. 2017;30:384–395. doi: 10.3122/jabfm.2017.03.160285. [DOI] [PubMed] [Google Scholar]
- 18.Hussey P.S., Schneider E.C., Rudin R.S., Fox D., Lai J., Pollack C. Continuity and the costs of care for chronic disease. JAMA Internal Medicine. 2014;174:742–748. doi: 10.1001/jamainternmed.2014.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sveréus S., Larsson K., Rehnberg C. Clinic continuity of care, clinical outcomes and direct costs for COPD in Sweden: a population based cohort study. European Clinical Resproy Journal. 2017;4 doi: 10.1080/20018525.2017.1290193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin I.P., Wu S.C. Effects of long-term high continuity of care on avoidable hospitalizations of chronic obstructive pulmonary disease patients. Health Policy. 2017;121:1001–1007. doi: 10.1016/j.healthpol.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 21.Swanson J.O., Vogt V., Sundmacher L., Hagen T.P., Moger T.A. Continuity of care and its effect on readmissions for COPD patients: a comparative study of Norway and Germany. Health Policy. 2018;122:737–745. doi: 10.1016/j.healthpol.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Kao Y.H., Wu S.C. STROBE-compliant article: is continuity of care associated with avoidable hospitalization among older asthmatic patients? Medicine (Baltimore) 2016;95:e4948. doi: 10.1097/MD.0000000000004948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin I.P., Wu S.C., Huang S.T. Continuity of care and avoidable hospitalizations for chronic obstructive pulmonary disease (COPD) Journal of the American Board of Family Medicine. 2015;28:222–230. doi: 10.3122/jabfm.2015.02.140141. [DOI] [PubMed] [Google Scholar]
- 24.National Health Insurance Administration . Taipei Taiwan Ministry of Health and Welfare; 2017. National Health Insurance annual report 2016–2017. [Google Scholar]
- 25.Cheng T.M. Reflections on the 20th anniversary of Taiwan’s single-payer National Health Insurance System. Health Affairs (Millwood) 2015;34:502–510. doi: 10.1377/hlthaff.2014.1332. [DOI] [PubMed] [Google Scholar]
- 26.2018. National health insurance research database Taiwan.http://nhird.nhri.org.tw/en/Data_Subsets.html [Accessed 20 January, 2018] [Google Scholar]
- 27.Centers for Disease Control and Prevention Severe acute respiratory syndrome-Taiwan, 2003. MMWR Morbidity and Mortality Weekly Report. 2003;52:461. [PubMed] [Google Scholar]
- 28.Gershon A., Wang C., Guan J., Vasilevska-Ristovska J., Cicutto L., To T. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2009;6:388–394. doi: 10.1080/15412550903140865. [DOI] [PubMed] [Google Scholar]
- 29.Yeh J.J., Wang Y.C., Kao C.H. Asthma–chronic obstructive pulmonary disease overlap syndrome associated with risk of pulmonary embolism. PLoS One. 2016;11 doi: 10.1371/journal.pone.0162483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wurst K.E., Kelly-Reif K., Bushnell G.A., Pascoe S., Barnes N. Understanding asthma-chronic obstructive pulmonary disease overlap syndrome. Respiratory Medicine. 2016;110:1–11. doi: 10.1016/j.rmed.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Van Walraven C., Oake N., Jennings A., Forster A.J. The association between continuity of care and outcomes: a systematic and critical review. Journal of Evaluation in Clinical Practice. 2010;16:947–956. doi: 10.1111/j.1365-2753.2009.01235.x. [DOI] [PubMed] [Google Scholar]
- 32.Bice T.W., Boxerman S.B. A quantitative measure of continuity of care. Medical Care. 1977;15:347–349. doi: 10.1097/00005650-197704000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Pollack C.E., Hussey P.S., Rudin R.S., Fox D.S., Lai J., Schneider E.C. Measuring care continuity: a comparison of claims-based methods. Medical Care. 2016;54:e30. doi: 10.1097/MLR.0000000000000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smedby Ö, Eklund G., Eriksson E.A., Smedby B. Measures of continuity of care: a register-based correlation study. Medical Care. 1986:511–518. doi: 10.1097/00005650-198606000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Cheng S.H., Hou Y.F., Chen C.C. Does continuity of care matter in a health care system that lacks referral arrangements? Health Policy and Planning. 2011;26:157–162. doi: 10.1093/heapol/czq035. [DOI] [PubMed] [Google Scholar]
- 36.Ministry of Labor Taiwan (R.O.C.) The history of enacting and adjusting the minimum wage policy. https://english.mol.gov.tw/6386/6394/6402/26387/ [Accessed 8 September, 2018]
- 37.Hsu C.H., Chou Y.J., Pu C. The effect of continuity of care on emergency room use for diabetic patients varies by disease severity. Journal of Epidemiology. 2016;26:413–419. doi: 10.2188/jea.JE20150045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cree M., Bell N., Johnson D., Carriere K. Increased continuity of care associated with decreased hospital care and emergency department visits for patients with asthma. Disease Management. 2006;9:63–71. doi: 10.1089/dis.2006.9.63. [DOI] [PubMed] [Google Scholar]
- 39.Kumbhare S., Pleasants R., Ohar J.A., Strange C. Characteristics and prevalence of asthma/chronic obstructive pulmonary disease overlap in the United States. The Annals of the American Thoracic Society. 2016;13:803–810. doi: 10.1513/AnnalsATS.201508-554OC. [DOI] [PubMed] [Google Scholar]
- 40.Miravitlles M., Soriano J.B., Ancochea J., Munoz L., Duran-Tauleria E., Sánchez G. Characterisation of the overlap COPD–asthma phenotype. Focus on physical activity and health status. Respiratory Medicine. 2013;107:1053–1060. doi: 10.1016/j.rmed.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 41.Quan H., Sundararajan V., Halfon P., Fong A., Burnand B., Luthi J.C. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 42.Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–241. [Google Scholar]
- 43.Cheng S.H., Chen C.C., Hou Y.F. A longitudinal examination of continuity of care and avoidable hospitalization: evidence from a universal coverage health care system. Archives of Internal Medicine. 2010;170:1671–1677. doi: 10.1001/archinternmed.2010.340. [DOI] [PubMed] [Google Scholar]
- 44.Nyweide D.J., Anthony D.L., Bynum J.P., Strawderman R.L., Weeks W.B., Casalino L.P. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Internal Medicine. 2013;173:1879–1885. doi: 10.1001/jamainternmed.2013.10059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang S.T., Wu S.C., Hung Y.N., Lin I.P. Effects of continuity of care on emergency department utilization in children with asthma. American Journal of Managed Care. 2016;22:e31–7. [PubMed] [Google Scholar]
- 46.Chen C.C., Cheng S.H. Does pay-for-performance benefit patients with multiple chronic conditions? Evidence from a universal coverage health care system. Health Policy and Planning. 2015;31:83–90. doi: 10.1093/heapol/czv024. [DOI] [PubMed] [Google Scholar]
- 47.Saultz J.W., Lochner J. Interpersonal continuity of care and care outcomes: a critical review. The Annals of Family Medicine. 2005;3:159–166. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Breslau N., Reeb K.G. Continuity of care in a university-based practice. Journal of Medical Education. 1975;50:965–969. doi: 10.1097/00001888-197510000-00006. [DOI] [PubMed] [Google Scholar]
- 49.Steinwachs D.M. Measuring provider continuity in ambulatory care: an assessment of alternative approaches. Medical Care. 1979;17:551–565. doi: 10.1097/00005650-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 50.Sudhakar-Krishnan V., Rudolf M.C. How important is continuity of care? Archives of Disease in Childhood. 2007;92:381–383. doi: 10.1136/adc.2006.099853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alshabanat A., Zafari Z., Albanyan O., Dairi M., FitzGerald J. Asthma and COPD overlap syndrome (ACOS): a systematic review and meta analysis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0136065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.van Boven J.F., Román-Rodríguez M., Palmer J.F., Toledo-Pons N., Cosío B.G., Soriano J.B. Comorbidome, pattern, and impact of asthma-COPD overlap syndrome in real life. Chest. 2016;149:1011–1020. doi: 10.1016/j.chest.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Salisbury C., Sampson F., Ridd M., Montgomery A.A. How should continuity of care in primary health care be assessed? British Journal of General Practice. 2009;59 doi: 10.3399/bjgp09X420257. e134-e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haggerty J.L., Roberge D., Freeman G.K., Beaulieu C., Bréton M. Validation of a generic measure of continuity of care: when patients encounter several clinicians. The Annals of Family Medicine. 2012;10:443–451. doi: 10.1370/afm.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Waibel S., Henao D., Aller M.B., Vargas I., Vázquez M.L. What do we know about patients’ perceptions of continuity of care? A meta-synthesis of qualitative studies. The International Journal for Quality in Health Care. 2011;24:39–48. doi: 10.1093/intqhc/mzr068. [DOI] [PubMed] [Google Scholar]