Abstract
This short-term observational study of infection control practice was performed in the medical emergency outpatient department (EMOPD) of a tertiary-care hospital in India when threatened by an outbreak of severe acute respiratory syndrome (SARS). An investigator attended the lobby daily to screen patients with symptoms for SARS. Patient/attendant load, patient flow, medical staff working practices and position in the EMOPD were observed. Infection control measures such as fumigation and cleaning were noted, as was the EMOPD laboratory function, use of personnel protection and display of information on infectious diseases. A total of 162 (7.4%) of the 2165 patients surveyed had respiratory symptoms but no cases of SARS were found. The flow of patients and their attendants was not systematic. No laboratory tests for SARS were available, and no educational material on SARS was displayed. The EMOPDs in key hospitals need be able to screen for infectious diseases, especially in view of the threats from SARS and Avian influenza.
Keywords: Infection control practice, SARS, Hospital, Emergency outpatient department
Introduction
The Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarrh was conceived in 1960 as a centre of excellence for medical care in North India, and includes the Nehru hospital, a centre of national importance with 1369 beds ( Table I). It caters for 1.2 million outpatients, 50 000 inpatients and 40 000 emergencies per year. Infectious diseases are a common reason for medical consultations, and the threats posed by them have been receiving considerable attention at national levels.1
Table I.
Hospital statisticsa from Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh
| Variable (Service) | N |
|---|---|
| Total no. of hospital beds | 1369 |
| Indoor | 1279 |
| Observational | 90 |
| Total no. of doctors in hospital | 1051 |
| Doctors in EMOPD at one time | 5 (12-hourly shift) |
| Total no. of nurses in hospital | 1352 |
| Nurses in EMOPD at one time | 4 (6-hourly shift, 12-hourly at night) |
| Total no. of monthly admissions | 4585 |
| Average daily admissions | 148 |
| Daily census of indoor patients | |
| Maximum on any one day | 1267 |
| Minimum on any one day | 1176 |
| Average length of stay (days) | 6.5 |
| Communicable disease ward (days) | 6.4 |
| Medical emergency (days) | 2.8 |
| Bed occupancy ratio (%) | 95.3 |
| Communicable disease ward (%) | 46.4 |
| Medical emergency (%) | 99.1 |
| Average daily OPD | 4149 |
| Total monthly emergency OPD | 2783 (11.1% of new patients in hospital) |
| Total monthly deaths | 452 |
| Emergency OPD deaths | 148 |
| Indoor deaths | 304 |
EMOPD, medical emergency outpatient department.
Monthly Statistical Report (August 2005), Department of Biostatistics, PGIMER Chandigarh, India.
In February 2002 a few cases of a mysterious plague-like disease were admitted to PGIMER. The diagnosis was initially missed, and the patients were not isolated until a formal diagnosis was made. By that time, infection had been transmitted to a visitor to another patient in the ward; a 28-year-old man, who later died. The need to screen all patients with suspected infectious disease in the medical emergency outpatient department (EMOPD), and for control and prevention of infection, was recognized. Two community physicians were deputed to assess the situation, and an outbreak control committee was formed. This arrangement lapsed when the plague situation was controlled.
Shortly afterwards, cases of suspected severe acute respiratory syndrome (SARS) were reported in India. Twenty persons were found to be serologically positive, although none fell within the World Health Organization (WHO) definition of SARS.2 A national alert was sounded and patient screening in the EMOPD was recommenced. A ‘control room’ was established near the reception to screen all patients with respiratory symptoms for SARS. This study was performed to analyse infection control in the EMOPD and to examine the patient flow system.
Materials and methods
This was a short-term study (April–May 2003). Consent was obtained from the senior medial officer, the patients and their attendants. The physical space, entry and exit system, location, registration area, lobby/corridor, waiting area, triage area, examination rooms, observational beds, emergency X-ray room and laboratory, treatment rooms, nurse's station, staff rest rooms, stores, police post and public relations office were observed. In addition, the patient/attendant load, patient flow, and medical staff practice were observed, and information displayed on SARS or other infectious diseases was noted.
The EMOPD has four entrances manned by security guards. These open into a spacious, well-lit lobby. There are separate emergency wards for medicine and surgery (total 110 beds), and 28 observational beds. On average, 80–100 patients are admitted daily and almost twice that number of attendants accompany them. A computed tomography (CT) scan/radiology department, seven operating theatres, a blood bank, an attendant waiting room, laboratory, and a public relation officer's room are attached to the EMOPD. No isolation facility is available. At any one time, there is a consultant, two senior residents, three junior residents, four nursing staff and a sanitary staff member present.
The principal investigator was a senior resident (MD) in community medicine with six years' experience. He sat with a public health nurse in a lobby near an EMOPD entrance from 08:00 to 17:00 and was on call for the rest of the day. The security guards directed patients with respiratory symptoms to the principal investigator, who asked them and their relatives the SARS screening questions specified in the WHO protocol, i.e. Do you have a fever? Do you have one or more of the following symptoms: cough, shortness of breath, difficult breathing? Have you been in contact with a person with respiratory symptoms in the last 10 days? They were also asked to provide their travel history over the past 10 days. There was no objective assessment of temperature. Patients with at least two of the three symptoms had chest radiographs. The WHO protocol was used to classify the patients as having suspected or probable SARS.3
Results
On 25 April 2003, EMOPD began screening all febrile patients with respiratory complaints for SARS. A 30-year-old male suspect case of SARS was admitted on 1 May 2003 with fever (39°C), chills and breathlessness. He developed respiratory failure and was transferred to the respiratory intensive care unit on 2 May. One day later he was put into the isolation ward as a suspected SARS case along with six contacts. A senior resident in pulmonary medicine and the principal investigator examined any contacts in the ward. After five days of isolation, he was moved into a general ward. Facemasks were provided for him and his family but standard procedures for handling samples from SARS cases were not followed. A blood sample taken on admission was sent to the National Institute of Communicable Diseases, Delhi and proved to be negative for SARS. No convalescent sample was sent, nor were any other respiratory samples examined. The case and the contacts were then discharged. They were asked to report immediately if any sign/symptom appeared in next fortnight.
A total of 2165 patients were screened in 28 days, 162 (7.4%) of whom had a history of respiratory complaints. An average of six or seven patients with respiratory complaints were screened for SARS daily. No confirmed case of SARS was found.
The flow of patients and their attendants was not systematic and their movement was uncontrolled. Two or three or even more attendants usually accompanied one patient. At the entrance, there was no sign showing the direction to the patient reception area. The corridor was overcrowded, leaving little space for movement of patients, nurses and doctors. There is a central air-conditioning system with different airflow control units, but no negative-pressure isolation room or other isolation facility. The floors were wet mopped two or three times per day and once a day with cresol. The emergency operation theatres were fumigated monthly.
Initially the principal investigator was only provided with standard facemasks. He wore two at a time for protection. An N-95 mask was made available for the final 10 days. The suspected SARS case and his contacts were also given standard facemasks. Laboratory investigations for SARS were not available in the EMOPD. Attendants crowded around the place of collection for laboratory reports, which they searched for themselves.
No information on SARS was displayed, and the staff told the patients/attendants about the symptoms of SARS only when asked. Most of the attendants/patients targeted the principal investigator for information. In the EMOPD there was no online access to information on recent outbreaks of communicable diseases. Journals such as CD Alert are not taken by the EMOPD and none of the resident doctors had heard of CD Alert or the WHO Weekly Epidemiological Report. They were unaware of the notifiable diseases or SARS management protocols.
Discussion
There were no confirmed cases of SARS in India despite initial concern but the recent threats of avian influenza and SARS have reinforced the need for a screening system for such infections in EMOPD. Infected patients can transmit their infection to others in EMOPD as happened in the plague outbreak. The role of hospitals in the spread of infectious diseases was emphasized by experiences with SARS, for example in Taiwan, where 31 cases occurred after exposure to the index case in the EMOPD itself.4 Therefore, the promptness and quality of emergency medical care may be crucial in preventing the spread of infection.
Surveillance is an essential part of hospital control of infectious diseases. Many countries have tried to incorporate surveillance in their emergency medical services, and the role of national government in strengthening infectious disease control in an emergency has been debated.5 In India an Integrated Disease Surveillance Project (IDSP) has been implemented in many states to focus on early detection and control of spread of infectious diseases. A draft contingency plan for avian influenza has been included in the IDSP training of medical officers, but the IDSP lacks the necessary focus for the EMOPD.5
In our study, the WHO protocol was used to classify the cases as having suspected or probable SARS. Suspect patients were straightaway shifted to the isolation room (in a different block, 300 m from the EMOPD). However, the chances of infection spreading to patients/attendants during transfer of the patient remained. Grouping infectious patients in a centralized location in an early stage of infection may reduce the extent of an epidemic.6 Lingappa et al. also suggested that the hospital setting was the primary amplifier of SARS transmission.7 Table II shows the SARS control measures that ought to have been taken and what was actually done during the survey period.8 The standard management protocol was not followed. The casual approach was evident by the fact that collection of a single blood sample was done on day 1 of onset of symptoms in a suspected SARS case – a procedure with no diagnostic value.
Table II.
Severe acute respiratory syndrome (SARS) prevention measures undertaken in the medical emergency outpatient department (EMOPD) of the Post Graduate Institute of Medical Education and Research (PGIMER) in comparison with the standard protocol8
| What should have been done | What was done in PGIMER EMOPD |
|---|---|
| Educating staff about hand hygiene and isolation using posters and instructional materials | No such measure was taken |
| Educating patient about respiratory hygiene and cough etiquette | No such policy was declared |
| If there is a high index of suspicion for SARS-associated coronavirus (SARS-CoV) disease, the patient should immediately be on SARS isolation precaution and all contacts of the ill patients should be identified, evaluated and monitored. Prompt SARS-CoV laboratory diagnosis should be arranged |
|
| Collection of appropriate samples and transport to reference laboratory following standard guidelines | Standard guidelines were not followed; a casual approach was taken |
| Disposal of wastes according to standard guidelines | No specific instruction was issued about waste disposal from suspected SARS case |
The resident doctors of medicine and surgery should be aware of the locally endemic diseases and impending outbreaks. Accordingly they should watch for the suggestive symptoms in every case. This should be included in their training/teaching. A set of standard protocols for screening and management of infectious disease patients should be framed and displayed prominently. These guidelines should be regularly updated whenever any new emerging or re-emerging disease is reported. The latest updates from CD Alert and Global Infectious Disease Alert should also be prominently displayed in the EMOPD.
The layout of an emergency department affects the chances of spread of infection. Open wards with many beds separated by curtains and no controlled ventilation have been regarded as contributory factors to the spread of the virus.9 In Singapore changed triage and infection control practices stopped nosocomial transmission of the virus.10
In our study, patient flow was not systematic and there was no regulation of numbers. Others have reported similar scenarios.11 The number of air exchanges, air filters and flow of air in the EMOPD were as per accredited international norms, but there was no negative-pressure isolation room.
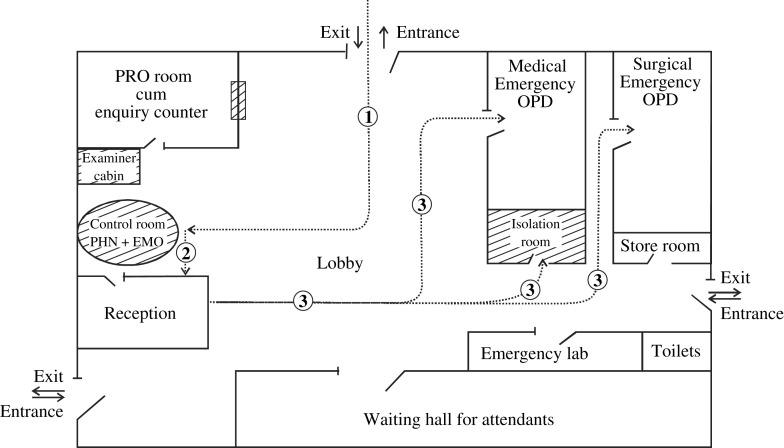
PGIMER EMOPD has a core type of design.11 Two kinds of change are possible:
-
(a)
Structure. The EMOPD initially contained 35–40 beds, but now has 110, leaving little scope for further expansion. To prevent spread of infection, a permanent ‘triage/control room’ should be established near reception for screening patients. This should include a cubicle for examination of critically ill infectious disease patients. If a doctor/nurse suspects that s/he is dealing with a highly infectious disease, s/he should have an option to isolate the suspected cases in an isolation room/ward located nearby.
-
(b)
Function. This could be changed without undue disturbance and cost, provided that the building has sufficient flexibility.12, 13 The flow of patients and visitors can be easily regulated. A sign should be placed at the entry of EMOPD instructing people where to report first. Proper directions to patients/attendants should be displayed inside the hall. A systematic patient flow control mechanism should be installed and a screening system for patients' attendants should also be initiated. Only one attendant (at the most two, in case of serious emergency) should be allowed into the EMOPD. A public health nurse (PHN) along with an emergency medical officer – surveillance and screening (EMO-S&S) should be posted permanently in the EMOPD.
The PHN should conduct a daily census of infectious and notifiable diseases. Patients arriving in EMOPD should first be examined thoroughly to rule out the chance of patients with acute infectious disease from mixing with the OPD crowd. Only the patients screened by the EMO-S&S should be allowed to enter along with one attendant. Restriction of patient movement is crucial for ensuring infection control. Until a larger EMOPD is constructed, overcrowding and lack of scope of flexibility for functional changes will continue to compromise infection control measures ( Figure 1).
Figure 1.
Design of emergency outpatient department (OPD) and patient flow (proposed changes are shown in shaded areas). PRO, public relation officer; PHN, public health nurse; EMO, emergency medical officer.
Medical personnel are also a recognized source of transmission of infectious diseases in hospitals.9, 13 Emergency department workers in large hospitals are generally more severely affected by an epidemic.6 Personal protection equipment (PPE), namely gloves, gowns and surgical masks, is important in preventing transmission of SARS.14 Failure to implement a policy of universal PPE use early in an outbreak enables the spread of infectious diseases. Use of fitness-tested personal protective equipment in all patient-care areas has been shown to prevent nosocomial spread of SARS.10 In our study, provision of the recommended N-95 masks was delayed due to late procurement. Such personal protective equipment should be permanently available in an EMOPD.
Availability of quick and reliable laboratory investigation facilities is vital for the early diagnosis of acute infectious diseases and allows initiation of prompt treatment and control measures. Standard protocols for specimen collection for infectious diseases should be used. In the present study, the standard protocol for specimen collection from a SARS case was not followed, which resulted in delayed confirmation of diagnosis. Streamlining of the laboratory reporting system was also required.
There is a definite need to make the EMOPD safer for immunocompromised and susceptible patients and their attendants. Our study highlights the vulnerability of EMOPDs in India for spread of infectious diseases even in centres of excellence. The situation in smaller hospitals can only be expected to be worse. A set of standard guidelines should be evolved for various levels of hospitals in India for handling infectious diseases and pasted in the EMOPD. Effective implementation of the IDSP would be another useful measure.
Currently, there is a worldwide focus on improvement of quality of care in EMOPDs. The recent SARS epidemic showed that only healthcare systems that have been strengthened and can respond to events of this kind would be able to handle future contingencies. Under a new accreditation standard, EMOPDs and all departments must be prepared to handle an influx, or the risk of an influx, of infectious patients. They should collaborate with the infection control committee, disaster management committee, local board of health, and other providers to develop protocols and policies. They should hold disaster drills in which they must handle infectious patients. EMOPD staff, particularly the triage nurses, need training in the early recognition of presenting symptoms of infectious diseases.15 WHO has established a Global Alert and Response Network to monitor and track infectious diseases outbreaks, which should allow EMOPDs to anticipate future problems.16
References
- 1.Singhi S., Jain V., Gupta G. Pediatric emergencies at a tertiary care hospital in India. J Trop Pediatr. 2003;49:207–211. doi: 10.1093/tropej/49.4.207. [DOI] [PubMed] [Google Scholar]
- 2.Shaila M.S. Severe acute respiratory syndrome (SARS): an old virus jumping into a new host or a new creation? J Biosci. 2003;28:359–360. doi: 10.1007/BF02705108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Outbreak of severe acute respiratory syndrome – worldwide, 2003. MMWR Morb Mort Wkly Rep. 2003;52:226–228. [PubMed] [Google Scholar]
- 4.Chen Y.C., Huang L.M., Chan C.C. SARS in hospital emergency room. Emerg Infect Dis. 2004;10:782–788. doi: 10.3201/eid1005.030579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Directorate General of Health Services . New Delhi, DGHS, Ministry of Health and Family Welfare, Government of India; 2006. Contingency plan for management of human cases of avian influenza. [Google Scholar]
- 6.Chen W.K., Wu H.D., Lin C.C., Cheng Y.C. Emergency department response to SARK. Emerg Infect Dis. 2005;11:1067–1073. doi: 10.3201/eid1107.040917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lingappa J.R., McDonald L.C., Simone P., Parashar U.D. Wresting SARS from uncertainty. Emerg Infect Dis. 2004;10:167–170. doi: 10.3201/eid1002.031032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Srinivasan A., McDonald L.E., Jernigan D. Foundations of the severe acute respiratory syndrome preparedness and response plan for health care facilities. Infect Control Hosp Epidemiol. 2004;25:1020–1025. doi: 10.1086/502338. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Severe acute respiratory syndrome – Singapore. MMWR Morb Mortal Wkly Rep. 2003;52:405–412. [PubMed] [Google Scholar]
- 10.Li-Yang Hsu, Lee C.C., Green J.A. Severe acute respiratory syndrome in (SARS) Singapore: features of index patient and initial contacts. Emerg Infect Dis. 2003;9:713–717. doi: 10.3201/eid0906.030264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta S., Sharma R.K., Sharma Y.P. Planning and designing of accident and emergency department for a district hospital – 200–300 beds. J Acad Hosp Adm. 1998;10:63–72. [Google Scholar]
- 12.Kleczkowski B.M., Pibouleau R. World Health Organization; Geneva: 1976. Approaches to planning and design of health care facilities in developing areas, Vol. 1. (WHO Offset Publication No. 29) [Google Scholar]
- 13.Tsang K.W., Ho P.L., Ooi G.C. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1977–1985. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 14.Equipment for SARS control in patient care units and in units that process infected samples. Rev Panam Salud Publica. 2003;14:67–69. [PubMed] [Google Scholar]
- 15.Hospitals' preparation for surge of patients helps with new Joint Commission standards ED Manag. 2005;17 Suppl 1–3. [PubMed] [Google Scholar]
- 16.Marmagas S.W., King L.R., Chuk M.G. Public health's response to a changed world. September 11, biological terrorism and the development of an environmental health tracking network. Am J Public Health. 2003;93:1226–1230. doi: 10.2105/ajph.93.8.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]