Abstract
Background
Several reports have shown that enhanced recovery or fast-track (FT) regime introduction in patients undergoing total knee replacement (TKR) and total hip replacement (THR) results in significant reduction in length of stay (LOS) with no associated increase of complications or readmission rate. Despite that, FT programs for arthroplasty have has not been uniformly recognized or accepted by many orthopaedic surgeons and there is still no consensus on the best implementation process. The aim of this study was to report the results of a stepwise implementation of a FT regime in TKR and THR patients in a general orthopaedic department.
Material and methods
This was a retrospective study of prospectively collected data (from 2014 to 2017) concerning all consecutive unselected patients who underwent TKR or THR on Monday morning. At stage 1 the rehabilitation and physiotherapy component was changed, at stage 2 and 3 a patient's blood management program and a pain management program were prospectively recorded (i.e. respectively Patients’ demographics, ASA classification, Charlson index, LOS, blood loss, transfusion rate, complications and 30 – day readmissions).
Results
Four hundred and thirty four patients underwent either TKR (n: 302) or THR (n:132) and were included in this study. A gradual reduction of mean LOS was found in THR patients from 5.7 days to 3.0 days and in TKR patients from 5.6 days to 3.4 days. Furthermore, no significant difference was found in complications or regarding the 30-day readmission rate at the different stages of implementation of the different FT components (i.e. at the final stage 96.7% of THR and 86.7% of TKR patients were discharged to home by the fourth post-operative day).
Conclusion
The stepwise implementation of a FT program in an unelected population of THR and TKR patients was effective and safe, reducing the post-surgical recovery time and patients’ LOS with no major complications and no increase of 30-day re-admissions.
Keywords: Total hip arthroplasty, Total knee arthroplasty, Fast-track, Enhanced recovery after surgery
1. Introduction
Total hip replacement (THR) and total knee replacement (TKR) is the final solution for end-stage hip and knee osteoarthritis (i.e. advanced degenerative changes and osteonecrosis) respectively. Both procedures successfully address patients' pain and functional disability and improve health-related quality of life.1 Nevertheless THR and TKR are operations followed by a risk of morbidity and mortality, especially in preoperative high-risk patients.2
According to the literature the frequency of THA and TKA has increased over the last 2-3 decades and this is predicted to continue for the next several decades.3,4
The postoperative recovery and the patients’ length of hospital stay (LOS) after THR and TKR in European countries traditionally has been 6–11 days, but the implementation of fast-track (FT) or enhanced recovery after surgery (ERAS) regimes has resulted in a significant reduction of LOS to less than 4 days.5,6
The target of the FT program is not the reduction of the LOS itself but the enhancement of recovery and the reduction of morbidity that will lead to reduction of LOS, convalescence, and costs.6, 7, 8
Fast Track protocols were first introduced by Kehlet in colorectal surgery 1997.9 Subsequently similar protocols were successfully implemented in different hospitals and countries in THR and TKR patients.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20
Prospective comparative studies have shown that FT protocols resulting in reduced LOS are feasible and safe with no adverse effects and without increasing the risk of complications.12,14,16,17,19, 20, 21, 22, 23, 24 Furthermore in some studies apart from reduced LOS other beneficial effects were also found such as lower readmission rate,22 better quality of life,12 significant reduction in 30day and 90-day death rate14 and cardiac ischemic events,17 significant reduction in death rate at 2 years,16 and reduced cost overall.20,24
The implementation of such protocols in large areas resulted in clinical benefits to patients and reduced length of hospital stay in THR and TKR patients.25,26 A recent meta-analysis also found that FT significantly reduces length of stay with no increase of complications and 30-day readmission rate in patients undergoing THR or TKR.27
However, it seems that the effectiveness of FT on arthroplasty has not been uniformly recognized or accepted by orthopaedic surgeons. Elaborating on these issues may express the need for the stepwise implementation of a FT program.6,27,28
The aim of this study is to report the results of a stepwise implementation of fast-track regime in THR and TKR patients in a tertiary hospital.
2. Material and methods
This is a retrospective study of a prospectively collected data (from 2014 to 2017) concerning all consecutive unselected patients underwent TKR or THR early in the week (on Monday) in a tertiary hospital. During this time, three steps in succession have been implemented, which are discussed below. The time frame of each step is completed within 9 months. The patients were contributed by two senior orthopaedic surgeons (G.D. and A.V) using similar surgical approaches and techniques. The surgical techniques used included the middle parapatellar approach for TKR and the lateral approach (Hardinge approach) for THR.
The traditional (T) peri-operative regime in our department (before commencing the implementation of the FT regime) included, (a) pre-admission clinic at five days before the operation, (b) peri-operative antibiotic prophylaxis with a second generation cephalosporin (cefoxitin sodium), (c) spinal or general anesthesia, (d) post-operation pain management based on opioids (e) anticoagulation protocol with low-weight molecular heparin, (f) transfusion trigger of Hemoglobin was 10 g/dL, (g) patients' mobilization at the second post-operative day and (h) LOS for at least 5–6 days.
The implementation of the different components of the FT program utilized in three stages.
At the first step (P), the existing rehabilitation and physiotherapy component was changed. Patients were instructed to commence specific exercises during the pre-admission clinic, and performed these exercises post-operatively as soon as they were able to move their legs. All patients were mobilized out of bed the morning after surgery and before the 24-h after the operation.
At the second step (P + BMP), a blood management program (BMP) was introduced. The preoperative hemoglobin (Hb) was tested one month before the operation and in case of anaemia (preoperative Hb value lower than 12 gr/dL) the appropriate investigation and treatment was applied. Furthermore we introduced the use of tranexamic acid (intra-operatively used 2gr dissolved in 100 ml of normal saline) locally applied and a transfusion trigger of 9 g/dL.
Finally (i.e., at the third step (P + BMP + PMP)), a pain management program (PMP) and a standard protocol of orthopaedic nursing were introduced. The PMP includes a multimodal opioid-sparing analgesia regimen using gabapentinoids, local infiltration analgesia (ropivacaine 1% in a maximum dose of 3 mg/kg), paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs).
Peri-operative antibiotic prophylaxis with a second generation cephalosporin (cefoxitin sodium) for 24 h and anticoagulation protocol with low-weight molecular heparin, was the same for all patients, while the type of anesthesia (spinal or general anesthesia) was chosen by the attending anesthesiologists.
All patients were discharged to their homes, with regular follow-ups in the outpatient's clinic.
All patients’ data including demographics, American Society of Anesthesiology physical status classification system (ASA),29 Charlson index,30 perioperative data including operation time, blood loss, transfusion rate, LOS, 30 - day re-admissions, and complications were prospectively recorded.
Complications were categorized according to Parvizi et al. (2007)31 as systemic (major or minor) and local (major or local).
2.1. Statistical analysis
Statistical analysis of the data was performed by using the Statistical Package for the Social Sciences (SPSS), version 19.0 software (SPSS, Chicago, IL). The normality of quantitative variables was tested with Kolmogorov-Smirnov test. All quantitative variables were expressed as the mean ± standard deviation (SD). Categorical variables were expressed as frequencies (and percentage). Oneway analysis of variance (ANOVA) and chi-square test were used to determine differences in demographic and clinical characteristics between the four groups of patients.
One-way analysis of covariance (ANCOVA) was performed to investigate the effect of different steps on LOS, adjusting for all potential confounders. Pearson's r correlation coefficient was used to examine the linear association between two quantitative variables. To assess the independent effect of demographic and clinical characteristics on the POS (probability of success) multivariate stepwise linear regression models was constructed. All tests were two tailed and statistical significance was considered for p - values less than 0.05.
3. Results
Four hundred and forty three consecutive patients underwent TKR (n:302) and THR (n:141). No patient was excluded or missed from the follow-up.
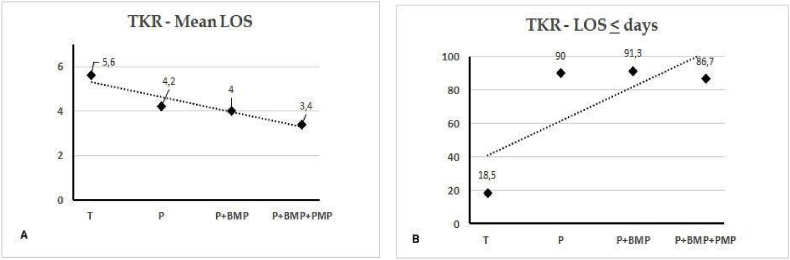
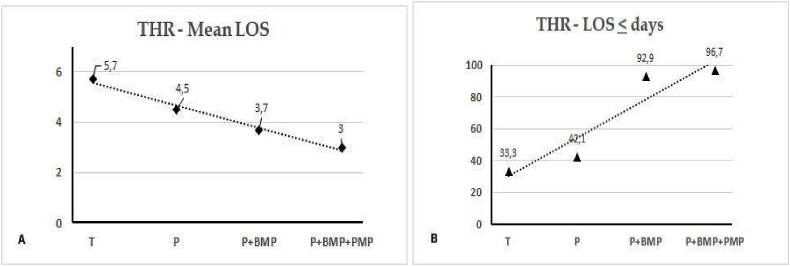
A gradual reduction of mean LOS was found in TKR patients from 5.6 days to 3.4 days and at the final step 86.7% of TKR patients were discharged by the fourth post-operative day (Fig. 1). Similarly a gradual reduction of mean LOS was found in THR patients from 5.7 days to 3 days and at the final step 96.7% of THR were discharged up to the fourth post-operative day (Fig. 3).
Fig. 1.
Mean length of stay (LOS) (A) and LOS up to four days (B) in Total Knee Replacement (TKR) patients. Step T: Traditionl, P: Physiotherapy, P+BMP: Physiotherapy + Blood Management Program, P+BMP+PMR: Physiotherapy + Blood Management Program + Pain Management Program.
Fig. 3.
Mean length of stay (LOS) (A) and LOS up to four days (B) in Total Hip Replacement (THR) patients. Step T: Traditionl, P: Physiotherapy, P+BMP: Physiotherapy + Blood Management Program, P+BMP+PMR: Physiotherapy + Blood Management Program + Pain Management Program.
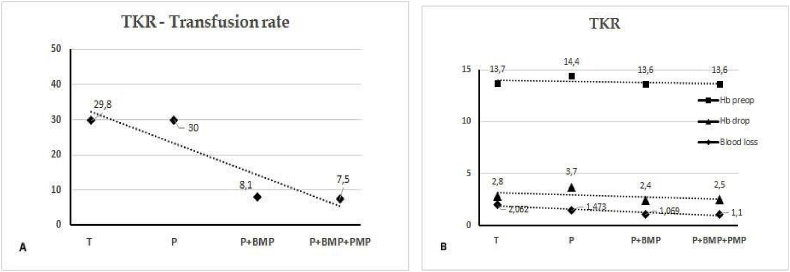
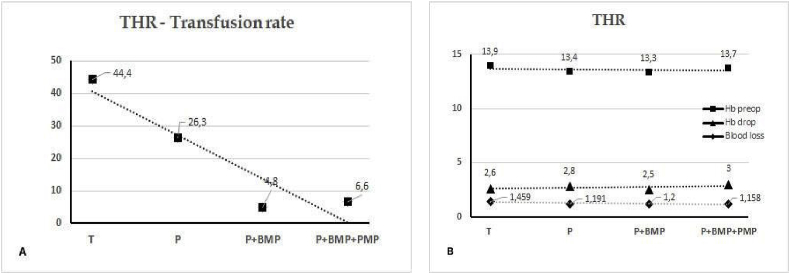
The introduction of BMP resulted in gradual reduction of the transfusion rate and the blood loss despite the similar other hematological parameters in both TKR (Fig. 2) and THR (Fig. 4) patients.
Fig. 2.
Transfusion rate (A) and hematological parameters (B) in Total Knee Replacement (TKR) patients. Step T: Traditionl, P: Physiotherapy, P+BMP: Physiotherapy + Blood Management Program, P+BMP+PMR: Physiotherapy + Blood Management Program + Pain Management Program.
Fig. 4.
Transfusion rate (A) and hematological parameters (B) in Total Hip. Step T: Traditionl, P: Physiotherapy, P+BMP: Physiotherapy + Blood Management Program, P+BMP+PMR: Physiotherapy + Blood Management Program + Pain Management Program.
The mean LOS was reduced.
3.1. TKR patients
3.1.1. Patients’ characteristics
Patients were categorized into the following groups, according to the step in T (47 patients), P (40 patients), P + BMP (148 patients) and P + BMP + PMP (67 patients).
Demographics and disease characteristics of the 302 patients included that underwent TKR, in relation to the step are presented in Table 1. There were no statistically significant differences in age (p = 0.683), gender (p = 0.765), BMI (p = 0.560), ASA (p = 0.276), Charlson index (p = 0.123), and preoperative Hb values (p = 0.239). On the contrary, patients in step T and P presented greater Hb change (p = 0.001), more blood loss (p < 0.001) and more need of transfusion (p < 0.001) compared to patients in step P + BMP and P + BMP + PMP. Moreover, patients in step P + BMP + PMP had longer surgical time (p = 0.033) and more frequently underwent general anesthesia (p < 0.001).
Table 1.
Details concerning the TKR patients.
| T | P | P + BMP | P + BMP + PMP | p | |
|---|---|---|---|---|---|
| Patients | 47 | 40 | 148 | 67 | |
| Age | 70.62 ± 7.28 | 71.78 ± 6.52 | 71.07 ± 6.40 | 70.25 ± 6.92 | 0.683 |
| Gender [n (%)] | 0.765 | ||||
| M | 9 (19.1) | 11 (27.5) | 31 (20.9) | 16 (23.9) | |
| F | 38 (80.9) | 29 (72.5) | 117 (79.1) | 51 (76.1) | |
| BMI | 32.75 ± 4.38 | 31.60 ± 4.59 | 32.74 ± 5.05 | 32.30 ± 4.44 | 0.560 |
| ASA [n (%)] | 0.276 | ||||
| I | 4 (8.5) | 6 (15.0) | 6 (4.1) | 5 (7.5) | |
| II | 33 (70.2) | 27 (67.5) | 114 (77.0) | 53 (79.1) | |
| III | 10 (21.3) | 7 (17.5) | 28 (18.9) | 9 (13.4) | |
| Charlson index[n (%)] | 0.123 | ||||
| 1 | 27 (58.7) | 21 (52.5) | 95 (64.2) | 40 (59.7) | |
| 2 | 15 (32.6) | 18 (45.0) | 52 (35.1) | 24 (35.8) | |
| 3 | 4 (8.7) | 1 (2.5) | 1 (0.7) | 3 (4.5) | |
| Surgical time (min) | 86.36 ± 16.18 | 88.81 ± 16.29 | 89.46 ± 14.97 | 92.12 ± 14.32 | <0.001** |
| Anesthesia [n (%)] | <0.001** | ||||
| Spinal | 45 (95.7) | 40 (100.0) | 145 (98.0) | 57 (85.1) | |
| General | 2 (4.3) | 0 (0.0) | 3 (2.0) | 10 (14.9) | |
| Pre-operative Hb | 13.52 ± 1.32 | 13.83 ± 1.46 | 13.38 ± 1.22 | 13.58 ± 1.25 | 0.239 |
| Hb change | 2.56 ± 1.30 | 3.08 ± 1.22 | 2.22 ± 1.27 | 2.29 ± 1.02 | 0.001 |
| Blood loss (in litters) | 2.06 ± 0.68 | 1.49 ± 0.48 | 1.07 ± 0.23 | 1.12 ± 0.34 | <0.001** |
| Transfusion [n (%)] | 14 (29.8) | 19 (47.5) | 12 (8.2) | 5 (7.5) | <0.001** |
| LOS (days) | 5.57 ± 1.08 | 4.15 ± 0.83 | 3.92 ± 0.86 | 3.34 ± 1.18 | <0.001** |
T: Traditional stage, P: Physiotherapy and mobilization stage, P + BMP: Plus Blood management program, P + BMP + PMP: Plus Pain management program.
BMI: Body Mass Index.
ASA: American Society of Anesthesiology physical status classification system LOS: Length of stay.
3.1.2. LOS in relation to the step
Mean LOS values in relation to the steps are shown in Table 1. One-way ANOVA showed statistically significant differences of LOS values between the four steps (F3,139 = 43.295, p < 0.001); post hoc analysis showed that all pair-wise differences were statistically significant (all p < 0.05), with the exception of P and P + BMP (p = 0.184).
There were no statistically significant differences in age (p = 0.683), gender (p = 0.765), BMI (p = 0.560), ASA (p = 0.276), Charlson index (p = 0.123), and preoperative Hb values (p = 0.239). Analysis of covariance (ANCOVA) was performed to investigate the effect of the step on LOS, controlling for the effect of all possible confounders. The adjusted mean LOS ± standard errors (SE) are shown in Table 2. Post hoc analyses revealed of mean LOS are shown in Table 3.
Table 2.
LOS in relation the characteristics of the TKR patients.
| Patients’ characteristics | LOS | p |
|---|---|---|
| Age | 0.066 | 0.252 |
| Gender | 0.314 | |
| M | 4.21 ± 1.41 | |
| F | 4.04 ± 1.12 | |
| BMI | −0.035 | 0.543 |
| ASA | 0.063 | 0.274 |
| Charlson index | 0.065 | 0.259 |
| Surgical time (min) | 0.139 | 0.016* |
| Anesthesia | 0.836 | |
| Spinal | 4.08 ± 1.18 | |
| General | 4.00 ± 1.51 | |
| Pre-operative Hb | −0.086 | 0.136 |
| Hb change | 0.136 | 0.018* |
| Blood loss | 0.365 | <0.001** |
| Transfusion | <0.001** | |
| No | 3.96 ± 1.14 | |
| Yes | 4.72 ± 1.28 | |
| Step | <0.001** | |
| T | 5.57 ± 1.08 | |
| P | 4.15 ± 0.83 | |
| P + BMP | 3.92 ± 0.86 | |
| P + BMP + PMP | 3.34 ± 1.18 | |
Table 3.
Multivariate analysis for LOS. Independent factors related to LOS.
| Unstandardized b Coefficient | Standard error | Unstandardized beta coefficient | t | P value | |
|---|---|---|---|---|---|
| Constant | 5.446 | 0.149 | 36.622 | <0.001 | |
| Stage | |||||
| T | Ref. | ||||
| P | −1.501 | 0.209 | −0.428 | −7.166 | <0.001** |
| P + BMP | −1.556 | 0.165 | −0.653 | −9.411 | <0.001** |
| P + BMP + PMP | −2.135 | 0.187 | −0.746 | −11.416 | <0.001** |
| Male gender | 0.540 | 0.159 | 0.187 | 3.399 | 0.001* |
| Transfusion | 0.431 | 0.162 | 0.135 | 2.663 | 0.008* |
3.1.3. LOS in relation to patients’ characteristics
Table 2 demonstrates LOS in relation to demographic and clinical characteristics TKR patients.
Longer LOS was associated with longer surgical time (p = 0.016), greater Hb change (p = 0.018) blood loss (p < 0.001), transfusion (p < 0.001) and the step (p < 0.001).
No statistically significant effect of age (p = 0.252), gender (p = 0.314), BMI (p = 0.543), ASA (p = 0.274), Charlson index (p = 0.259), type of anesthesia (p = 0.836) and pre-operative Hb values.
(p = 0.136) on LOS was found.
Multivariate linear regression analysis disclosed that the step (p < 0.001), transfusion (p = 0.008) and gender (p = 0.001) were the statistically significant independent determinants of LOS in TKR patients (Table 3).
The P, the P + BMP and the P + BMP + PMP were associated with shorter LOS compared to T (by 1.5 days, 1.56 days and 2.1 days, respectively), while transfusion and male gender were associated with longer LOS (by about 0.5 days) in TKR patients.
3.2. THR patients
3.2.1. Patients’ characteristics
The study population consisted of 141 consecutive THR patients (51 males, 90 females) with a mean age of 65.86 ± 11.68 years (range, 25–85 years; median age, 68 years), mean height of 165.60 ± 9.15 cm (range, 154–192 cm), mean weight of 83.61 ± 13.30 kg (range, 52–122 kg) and mean BMI of 30.48 ± 3.91 kg/m2 (range, 20–40 kg/m2).
Patients were categorized into the following groups, according to the step in T (19 patients), P (19 patients), P + BMP (42 patients) and P + BMP + PMP (61 patients).
Demographics and disease characteristics of the patients in relation to the step are presented in Table 4. There were no statistically significant differences in gender (p = 0.530), BMI (p = 0.405), ASA (p = 0.371), pre-operative Hb values (p = 0.271) and Hb change (p = 0.525) between the four groups of patients. On the contrary, patients in step T and P were significantly older (p = 0.001), had higher Charlson index (p < 0.001) and more frequent underwent general anesthesia (p = 0.004) compared to patients in step P + BMP and P + BMP + PMP. Moreover, patients in step T had longer surgical time (p = 0.033), greater blood loss (p = 0.031) and more need of transfusion (p < 0.001).
Table 4.
Details concerning the THR patients.
| T | P | P + BMP | P + BMP + PMP | p | |
|---|---|---|---|---|---|
| Patients | 19 | 19 | 42 | 61 | |
| Age | 70.53 ± 4.68 | 70.26 ± 12.05 | 61.76 ± 12.35 | 65.85 ± 11.70 | 0.001* |
| Gender [n (%)] | 0.530 | ||||
| M | 9 (47.4) | 6 (31.6) | 17 (40.5) | 19 (31.1) | |
| F | 10 (52.6) | 13 (68.4) | 25 (59.5) | 42 (52.6) | |
| BMI | 31.26 ± 3.24 | 31.25 ± 2.89 | 30.63 ± 4.27 | 29.90 ± 4.09 | 0.405 |
| ASA [n (%)] | 0.371 | ||||
| I | 0 (0.0) | 3 (15.8) | 6 (14.3) | 10 (16.4) | |
| II | 19 (100.0) | 15 (78.9) | 32 (76.2) | 45 (73.8) | |
| III | 0 (0.0) | 1 (5.3) | 4 (9.5) | 6 (9.8) | |
| Charlson index [n(%)] | <0.001** | ||||
| 1 | 0 (0.0) | 0 (0.0) | 1 (2.4) | 1 (1.7) | |
| 2 | 4 (21.1) | 8 (42.1) | 30 (71.4) | 47 (78.3) | |
| 3 | 12 (63.2) | 10 (52.6) | 10 (23.8) | 11 (18.3) | |
| 4 | 3 (15.8) | 1 (5.3) | 1 (2.4) | 1 (1.7) | |
| Surgical time (min) | 122.63 ± 46.35 | 106.58 ± 17.24 | 98.95 ± 18.42 | 95.49 ± 23.22 | 0.033 |
| Anesthesia [n (%)] | 0.004* | ||||
| Spinal | 4 (21.1) | 4 (21.1) | 23 (54.8) | 34 (55.7) | |
| General | 15 (78.9) | 15 (78.9) | 19 (45.2) | 27 (44.3) | |
| Pre-operative Hb | 13.99 ± 1.55 | 13.44 ± 1.42 | 13.30 ± 1.43 | 13.73 ± 1.45 | 0.271 |
| Hb change | 2.60 ± 1.07 | 2.82 ± 0.78 | 2.46 ± 1.04 | 2.94 ± 2.28 | 0.525 |
| Blood loss (in litters) | 1.45 ± 0.36 | 1.19 ± 0.26 | 1.20 ± 0.43 | 1.16 ± 0.37 | 0.031 |
| Transfusion [n (%)] | 8 (41.1) | 5 (26.3) | 2 (4.8) | 4 (6.6) | <0.001* |
| LOS (days) | 5.68 ± 1.33 | 4.47 ± 1.02 | 3.66 ± 0.91 | 3.03 ± 0.75 | <0.001* |
3.2.2. LOS in relation to the step
Mean LOS values in relation to the step are shown in Table 4. One-way ANOVA showed statistically significant differences of LOS values between the four groups of patients (F3,139 = 43.295, p < 0.001); post hoc analysis showed that all pair-wise differences were statistically significant (all p < 0.05).
Since there were some significant differences in demographic and clinical characteristics among groups, analysis of covariance (ANCOVA) was performed to investigate the effect of the step on LOS, controlling for the effect of all possible confounders. The adjusted mean LOS ± standard errors (SE) and post hoc analysis revealed that mean LOS in steps are shown in Table 5.
Table 5.
LOS in relation the characteristics of the THR patients.
| Patients' characteristics | LOS | p |
|---|---|---|
| Age | 0.292 | <0.001** |
| Gender | 0.226 | |
| M | 3.94 ± 1.54 | |
| F | 3.67 ± 1.12 | |
| BMI | 0.053 | 0.536 |
| ASA | 0.116 | 0.174 |
| Charlson index | 0.348 | <0.001** |
| Surgical time (min) | 0.357 | <0.001** |
| Anesthesia | <0.001** | |
| Spinal | 3.37 ± 1.08 | |
| General | 4.12 ± 1.35 | |
| Pre-operative Hb | −0.066 | 0.442 |
| Hb change | −0.089 | 0.294 |
| Blood loss | 0.219 | 0.009* |
| Transfusion | 0.002* | |
| No | 3.56 ± 1.05 | |
| Yes | 5.11 ± 1.82 | |
| Step | <0.001** | |
| T | 5.68 ± 1.33 | |
| P | 4.47 ± 1.02 | |
| P + BMP | 3.66 ± 0.91 | |
| P + BMP + PMP | 3.03 ± 0.75 | |
3.2.3. LOS in relation to patients’ characteristics
Table 5 demonstrates LOS in relation to demographic and clinical characteristics THR patients. Longer LOS was associated with older ages (p < 0.001), higher Charlson index (p < 0.001), longer surgical time (p < 0.001), general anesthesia (p = 0.009), greater blood loss (p = 0.009), transfusion (p = 0.002) and the step (p < 0.001). No statistically significant effect of gender (p = 0.226), BMI (p = 0.536), ASA (p = 0.174), pre-operative Hb (p = 0.442) and Hb change (p = 0.294) on LOS was found.
Multivariate linear regression analysis disclosed that the step (p < 0.001), patients’ age (p = 0.005), transfusion (p = 0.006) and surgical time (p = 0.025) remained statistically significant independent determinants of LOS in THR patients (Table 6).
Table 6.
Multivariate analysis for LOS – Independent factors related to LOS.
| Unstandardized beta Coefficient | Standard error | Unstandardized beta coefficient | t | P value | |
|---|---|---|---|---|---|
| Constant | 3.234 | 0.615 | 5.262 | <0.001 | |
| Step | |||||
| T | Ref. | ||||
| P | −1.020 | 0.288 | −0.272 | −3.537 | 0.001 |
| P + BMP | −1.493 | 0.270 | −0.525 | −5.536 | <0.001 |
| P + BMP + PMP | −2.176 | 0.255 | −0.835 | −8.534 | <0.001 |
| Age | 0.020 | 0.007 | 0.173 | 2.881 | 0.005 |
| Transfusion | 0.653 | 0.235 | 0.174 | 2.784 | 0.006 |
| Surgical time | 0.007 | 0.003 | 0.141 | 2.264 | 0.025 |
The P, the P + BMP and the P + BMP + PMP were associated with shorter LOS compared to T (by 1.0 days, 1.5 days and 2.2 days, respectively), while older age, transfusion and longer surgical time were associated with longer LOS in THR patients.
3.3. 30-Day readmission and complications
No patients were re-admitted during the first 30 post-operative days. There were no deaths or acute deep wound infections (Table 7). In TKR patients there were more minor local complications, while in THR patients there were more minor systemic complications.
Table 7.
30-day complication rate per catergory as categorized by Parvizi et al. (2007).
| T | P | P + BMP | P + BMP + P | ||
| n (%) | n (%) | n (%) | n (%) | ||
| TKR patients | |||||
| Major systemic | |||||
| Tachyarrhythmia | 1 (0.7) | ||||
| Heparin induced thrombocytopenia (HIT) | 1(1.5) | ||||
| Minor systemic | |||||
| Mental status change | 1 (2.1) | ||||
| Deep venous thrombosis | 1 (0.7) | ||||
| Others | Allergic reaction n:1 (0.7) | Diarroia n:1(1.5) | |||
| Minor local | Hematoma | 1 (1.4) | 1 (1.5) | ||
| Persistent wound drainage | 1 (2.1) | 2 (5) | 2 (1.4) | 1 (1.5) | |
| Superficial wound | 1 (0.7) | 1 (1.5) | |||
| THR patients | |||||
| Major systemic | |||||
| Bowel obstruction | 1 (2.4) | ||||
| Minor systemic | |||||
| Mental status change | 1 (1.6) | ||||
| Deep venous thrombosis | 1 (2.4) | 1 (1.6) | |||
| Others (Allergic reaction) | 1 (2.4) | 1 (1.6) | |||
| Minor local | |||||
| Persistent wound drainage | 1 (5.3) | 1 (2.4) | |||
4. Discussion
The stepwise implementation of the different components of a FT program in our department resulted in gradual reduction of LOS in THR and TKR patients, with no major complications and no 30-day re-admissions. These results are in agreement with the current literature that supports the significant reduction of LOS with no increase of complications or re-admissions after the introduction FT protocols in THR and TKR patients.
The different FT programs include evidence-based interventions pre-operatively, intra-operatively and post-operatively, as well as pre-defined discharged criteria. Despite the differences amongst them.
32, 33, 34, 35, 36, 37, 38, they are characterized by the basic principles of FT programs. These include multidisciplinary collaboration (surgeons, anesthesiologists, nurses, and physiotherapists), the implementation of evidence-based perioperative care principles, monitoring of data, and adjustment of the program on the basis of scientific evidence.34
Several factors that related to the LOS in THR and TKR patients have been recognized and these include patients’ characteristics (age, comorbidities), peri-operative factors (type of anesthesia, blood loss) and post-operative regimes (analgesia, rehabilitation and physiotherapy).10,11,13,39,40
In our study factors related to increased LOS in both TKR and THR patients were the step, blood loss and transfusion and surgical time. Furthermore in THR patients age (older), Charlson index (comorbidities), and type of anesthesia (general) were also related to increased LOS. Multivariate analysis showed that the most important factors related to increased LOS in both TKR and THR patients were step and transfusion. Furthermore in TKR patients another factor was gender (male) and in THR patients both age (older) and surgical time were key factors.
4.1. Early mobilization and physiotherapy
Early mobilization is the gold standard for achieving functional mobility after arthroplasty41 and combined with early physiotherapy is a key component of FT programs.42,43
A recent meta-analysis shows a significant reduction in length of LOS when patients ambulate within 24 h of THR or TKR surgery.44 Furthermore there is evidence that mobilization of patients on the day of surgery after THR or TKR, is associated with reduced LOS.45, 46, 47
In our study patients commenced the instructed exercises soon after the operation and were mobilized and commenced physiotherapy (strengthening exercises) the first morning following surgery due to the lack of afternoon physiotherapy services. This change itself significantly reduced the LOS compared to the previous regime of mobilization the second postoperative day (Fig. 1, Fig. 3).
4.2. Blood management program
The introduction of BMP decreased the blood loss and transfusion rates in THR and TKR patients, with improved outcomes.48,49
Important parts of a BMP include the preoperative evaluation and treatment of patients anaemia, reduction of blood loss and transfusion rate, in an effort to decrease the adverse reactions and complications related to allogeneic blood transfusion.50 The prevalence of anemia depends on the type of surgery, age, gender, greater symptoms of tissue hypoperfusion and comorbidies present. Normal Hb according to WHO definitions, which is considered value higher than 12 g/dL. Determination of hemoglobin levels, blood loss, lowering of hemoglobin levels and duration of this condition vary considerably between hospitals.48, 49, 50, 51
Preoperative evaluation and treatment of patients’ anaemia is an important element of the BMP since preoperative anemia is independently associated with transfusion requirement, increased LOS and postoperative morbidity.51
Tranexamic acid used either intravenously or topically in THR and TKR patients is associated with a decreased blood loss and transfusion rates without increasing the risk for adverse reactions.52,53 Clinical studies with large number of THR and TKR patients have found that TXA is not only effective but it also safe even in patients with severe medical comorbidities.54, 55, 56
In our department TXA was initial used in a comparative study of TKR patients57 and subsequently it was introduced as part of BMP in all THR and TKR patients in a standard dose of 2 gr in 100 ml normal saline for topical use.
4.3. Local infiltration analgesia
The LIA was introduced the previous decade in an effort to reduce the acute postoperative pain after THR and TKR.58,59 Ropivacaine is the most commonly used local anesthetic and is used alone or mixed with other drugs; ketorolac and adrenaline being the most popular.58 There are several reports concerning different regimes but the results of a recent systematic reviews are inconclusive as far as the most effective and safe regime.60,61
Nevertheless, LIA combined with a multimodal systemic analgesia provides effective analgesia in the initial postoperative period and up to 24 h after TKR, while its effectiveness may be limited in THR patients.60,61 Furthermore it seems that LIA provides at least the same if not better analgesia compared to regional nerve block, and is potentially safer and more beneficial to early functional recovery preserving the quadriceps function in the immediate postoperative period in TKR patients.60,61
In our study the combination of LIA and multimodal systemic analgesia provided effective analgesia in the initial postoperative period and up to 24 h for both THR and TKR patients. Only 5% of the TKR patients and none of THR patients required use of narcotics as rescue analgesia.
4.4. Implementation process
The aim of a FT program is to reduce in post-surgical recovery time and consequently in LOS with safety and it is characterized by a multimodal and multi-disciplinary approach.
There is still no consensus on the optimal implementation process, so implementation of an FT program can be done sequentially or gradually.27,28 The characteristics of each hospital or unit concerning personnel, services, traditions and expertise, influence the implementation process and therefore the FT program should be considered accordingly.28,64
The implementation process includes not only the application of evidence-based protocols, but also adjustment of the program as a result of continuous monitoring of the process (and audit) as well as the adoption of new evidence that allows improvement of the FT program.6,14,15,28,65
Therefore, the FT program should be considered as a project with a beginning and an end.28
The present study is a report of gradual introduction of different FT program components that resulted in a gradual reduction of LOS with safety. Our study should be considered as a pilot one as the reported findings only relate to THR and THR patients operated on Monday. Areas of improvement include the provision of regular physiotherapy services in the afternoon and the weekends.13
Furthermore, an ongoing study in our unit monitors the readiness for discharge, using specific criteria and the actual LOS. The aim is to identify the reasons for any discrepancy between readiness for discharge and the actual time of discharge from the hospital.
This study has some limitations; it is a retrospective one, with a relatively small number of cases. Furthermore the follow-up period was only 30-days and the number of complications was small making any statistical analysis difficult. Nevertheless there were no deaths, no re-admissions and no major systemic or local complications.
4.5. In conclusion
In major orthopeadic surgery, FT program was effective and safe in the THR and the TKR. The stepwise implementation reduced the post-surgical recovery time and patients LOS, with no identified major complications and no increase of 30-day re-admissions. There are many factors (i.e.
‘anesthesia, pain management, transfusion trigger, nursing care, rehabilitation and physiotherapy) involved in its normal or abnormal enhanced recovery. The combination of all the above mentioned factors, contributes to the successful outcome. Additional studies are required to compare additional factors and their implications.
Declaration of competing interest
Authors declare that they have no conflict of interest.
Acknowledgement
The authors acknowledge the significant contribution of the following staff of our hospital during the implementation of this FT program (a) Sister Nurse Theopoula Kisoudi and all nurses of our department and (b) the personnel of the physiotherapy department of our hospital.
Contributor Information
Georgios I. Drosos, Email: drosos@otenet.gr.
Ioannis E. Kougioumtzis, Email: siritea@yahoo.gr.
Stylianos Tottas, Email: stottasdoc@hotmail.com.
Athanasios Ververidis, Email: athanasios@ververidis.net.
Christos Chatzipapas, Email: hatzy@otenet.gr.
Grigorios Tripsianis, Email: gtryps@med.duth.gr.
Konstantinos Tilkeridis, Email: tilkerorth@gmail.com.
References
- 1.Ethgen O., Bruyere O., Richy F., Dardennes C., Reginster J.Y. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Jt Surg Am Vol. 2004;86-a(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Kehlet H., Mythen M. Why is the surgical high-risk patient still at risk? Br J Anaesth. 2011;106(3):289–291. doi: 10.1093/bja/aeq408. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am Vol. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 4.Singh J.A. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J. 2011;5:80–85. doi: 10.2174/1874325001105010080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Husted H., Jensen C.M., Solgaard S., Kehlet H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000-2009: from research to implementation. Arch Orthop Trauma Surg. 2012;132(1):101–104. doi: 10.1007/s00402-011-1396-0. [DOI] [PubMed] [Google Scholar]
- 6.Kehlet H. Fast-track hip and knee arthroplasty. Lancet. 2013;381(9878):1600–1602. doi: 10.1016/S0140-6736(13)61003-X. [DOI] [PubMed] [Google Scholar]
- 7.Kehlet H., Dahl J.B. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362(9399):1921–1928. doi: 10.1016/S0140-6736(03)14966-5. [DOI] [PubMed] [Google Scholar]
- 8.Antrobus J.D., Bryson G.L. Enhanced recovery for arthroplasty: good for the patient or good for the hospital? Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2011;58(10):891–894. doi: 10.1007/s12630-011-9564-9. 4-6. [DOI] [PubMed] [Google Scholar]
- 9.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–617. doi: 10.1093/bja/78.5.606. [DOI] [PubMed] [Google Scholar]
- 10.Husted H., Holm G. Fast track in total hip and knee arthroplasty--experiences from Hvidovre University Hospital, Denmark. Injury. 2006;37(Suppl 5):S31–S35. doi: 10.1016/S0020-1383(07)70009-8. [DOI] [PubMed] [Google Scholar]
- 11.Husted H., Holm G., Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79(2):168–173. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- 12.Larsen K., Sorensen O.G., Hansen T.B., Thomsen P.B., Soballe K. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop. 2008;79(2):149–159. doi: 10.1080/17453670710014923. [DOI] [PubMed] [Google Scholar]
- 13.Schneider M., Kawahara I., Ballantyne G. Predictive factors influencing fast track rehabilitation following primary total hip and knee arthroplasty. Arch Orthop Trauma Surg. 2009;129(12):1585–1591. doi: 10.1007/s00402-009-0825-9. [DOI] [PubMed] [Google Scholar]
- 14.Malviya A., Martin K., Harper I. Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop. 2011;82(5):577–581. doi: 10.3109/17453674.2011.618911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raphael M., Jaeger M., van Vlymen J. Easily adoptable total joint arthroplasty program allows discharge home in two days. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2011;58(10):902–910. doi: 10.1007/s12630-011-9565-8. [DOI] [PubMed] [Google Scholar]
- 16.Savaridas T., Serrano-Pedraza I., Khan S.K., Martin K., Malviya A., Reed M.R. Reduced medium-term mortality following primary total hip and knee arthroplasty with an enhanced recovery program. A study of 4,500 consecutive procedures. Acta Orthop. 2013;84(1):40–43. doi: 10.3109/17453674.2013.771298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan S.K., Malviya A., Muller S.D. Reduced short-term complications and mortality following Enhanced Recovery primary hip and knee arthroplasty: results from 6,000 consecutive procedures. Acta Orthop. 2014;85(1):26–31. doi: 10.3109/17453674.2013.874925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winther S.B., Foss O.A., Wik T.S. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop. 2015;86(1):78–85. doi: 10.3109/17453674.2014.957089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang G., Chen W., Chen W., Tang X., Huang Y., Zhang L. Feasibility and safety of 2-day discharge after fast-track total hip arthroplasty: a Chinese experience. J Arthroplasty. 2016;31(8):1686–1692. doi: 10.1016/j.arth.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Wilches C., Sulbaran J.D., Fernandez J.E., Gisbert J.M., Bausili J.M., Pelfort X. Fast-track recovery technique applied to primary total hip and knee replacement surgery. Analysis of costs and complications. Rev Española Cirugía Ortopédica Traumatol. 2017;61(2):111–116. doi: 10.1016/j.recot.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Christelis N., Wallace S., Sage C.E. An enhanced recovery after surgery program for hip and knee arthroplasty. Med J Aust. 2015;202(7):363–368. doi: 10.5694/mja14.00601. [DOI] [PubMed] [Google Scholar]
- 22.Dowsey M.M., Kilgour M.L., Santamaria N.M., Choong P.F. Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study. Med J Aust. 1999;170(2):59–62. doi: 10.5694/j.1326-5377.1999.tb126882.x. [DOI] [PubMed] [Google Scholar]
- 23.Maempel J.F., Clement N.D., Ballantyne J.A., Dunstan E. Enhanced recovery programmes after total hip arthroplasty can result in reduced length of hospital stay without compromising functional outcome. The bone & joint journal. 2016;98-b(4):475–482. doi: 10.1302/0301-620X.98B4.36243. [DOI] [PubMed] [Google Scholar]
- 24.Stowers M.D., Manuopangai L., Hill A.G., Gray J.R., Coleman B., Munro J.T. Enhanced Recovery after Surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J Surg. 2016;86(6):475–479. doi: 10.1111/ans.13538. [DOI] [PubMed] [Google Scholar]
- 25.Scott N.B., McDonald D., Campbell J. The use of enhanced recovery after surgery (ERAS) principles in Scottish orthopaedic units-an implementation and follow-up at 1 year, 2010-2011: a report from the Musculoskeletal Audit, Scotland. Arch Orthop Trauma Surg. 2013;133(1):117–124. doi: 10.1007/s00402-012-1619-z. [DOI] [PubMed] [Google Scholar]
- 26.Featherall J., Brigati D.P., Faour M., Messner W., Higuera C.A. Implementation of a total hip arthroplasty care pathway at a high-volume health system: effect on length of stay, discharge disposition, and 90-day complications. J Arthroplasty. 2018;33(6):1675–1680. doi: 10.1016/j.arth.2018.01.038. [DOI] [PubMed] [Google Scholar]
- 27.Zhu S., Qian W., Jiang C., Ye C., Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med. 2017;93(1106):736–742. doi: 10.1136/postgradmedj-2017-134991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Molko S., Combalia A. Rapid recovery programmes for hip and knee arthroplasty. An update. Rev Española Cirugía Ortopédica Traumatol. 2017;61(2):130–138. doi: 10.1016/j.recot.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 29.Owens W.D., Felts J.A., Spitznagel E.L., Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49(4):239–243. doi: 10.1097/00000542-197810000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 31.Parvizi J., Mui A., Purtill J.J., Sharkey P.F., Hozack W.J., Rothman R.H. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Jt Surg Am Vol. 2007;89(1):27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 32.Paxton E.W., Inacio M.C., Singh J.A., Love R., Bini S.A., Namba R.S. Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a US healthcare system? Clin Orthop Relat Res. 2015;473(11):3446–3455. doi: 10.1007/s11999-015-4278-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maheshwari A.V., Blum Y.C., Shekhar L., Ranawat A.S., Ranawat C.S. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009;467(6):1418–1423. doi: 10.1007/s11999-009-0728-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kehlet H., Wilmore D.W. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248(2):189–198. doi: 10.1097/SLA.0b013e31817f2c1a. [DOI] [PubMed] [Google Scholar]
- 35.Handley A. Fast track to recovery. Nurs Stand. 1987;24(9):18–19. doi: 10.7748/ns.24.9.18.s25. 2009. [DOI] [PubMed] [Google Scholar]
- 36.Husted H., Hansen H.C., Holm G. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg. 2010;130(2):263–268. doi: 10.1007/s00402-009-0940-7. [DOI] [PubMed] [Google Scholar]
- 37.Kehlet H., Soballe K. Fast-track hip and knee replacement--what are the issues? Acta Orthop. 2010;81(3):271–272. doi: 10.3109/17453674.2010.487237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams J., Kester B.S., Bosco J.A., Slover J.D., Iorio R., Schwarzkopf R. The association between hospital length of stay and 90-day readmission risk within a total joint arthroplasty bundled payment initiative. J Arthroplasty. 2017;32(3):714–718. doi: 10.1016/j.arth.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 39.Husted H., Solgaard S., Hansen T.B., Soballe K., Kehlet H. Care principles at four fast-track arthroplasty departments in Denmark. Dan Med Bull. 2010;57(7):A4166. [PubMed] [Google Scholar]
- 40.Mathijssen N.M., Verburg H., van Leeuwen C.C., Molenaar T.L., Hannink G. Factors influencing length of hospital stay after primary total knee arthroplasty in a fast-track setting. Knee Surg Sports Traumatol Arthrosc : official journal of the ESSKA. 2016;24(8):2692–2696. doi: 10.1007/s00167-015-3932-x. [DOI] [PubMed] [Google Scholar]
- 41.Roos E.M. Effectiveness and practice variation of rehabilitation after joint replacement. Curr Opin Rheumatol. 2003;15(2):160–162. doi: 10.1097/00002281-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 42.Bandholm T., Kehlet H. Physiotherapy exercise after fast-track total hip and knee arthroplasty: time for reconsideration? Arch Phys Med Rehabil. 2012;93(7):1292–1294. doi: 10.1016/j.apmr.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 43.Soffin E.M., YaDeau J.T. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117(suppl 3) doi: 10.1093/bja/aew362. iii62-iii72. [DOI] [PubMed] [Google Scholar]
- 44.Guerra M.L., Singh P.J., Taylor N.F. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil. 2015;29(9):844–854. doi: 10.1177/0269215514558641. [DOI] [PubMed] [Google Scholar]
- 45.Smith T.O., McCabe C., Lister S., Christie S.P., Cross J. Rehabilitation implications during the development of the Norwich Enhanced Recovery Programme (NERP) for patients following total knee and total hip arthroplasty. Orthopaedics & traumatology, surgery & research : OTSR. 2012;98(5):499–505. doi: 10.1016/j.otsr.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 46.Tayrose G., Newman D., Slover J., Jaffe F., Hunter T., Bosco J., 3rd Rapid mobilization decreases length-of-stay in joint replacement patients. Bull Hosp Jt Dis. 2013;71(3):222–226. 2013. [PubMed] [Google Scholar]
- 47.Okamoto T., Ridley R.J., Edmondston S.J., Visser M., Headford J., Yates P.J. Day-of-Surgery mobilization reduces the length of stay after elective hip arthroplasty. J Arthroplasty. 2016;31(10):2227–2230. doi: 10.1016/j.arth.2016.03.066. [DOI] [PubMed] [Google Scholar]
- 48.Marson B.A., Shah J., Deglurkar M. Blood transfusion in hip and knee arthroplasties: the end of the pre-operative group and save? Eur J Orthop Surg Traumatol : Orthop Traumatol. 2015;25(5):871–875. doi: 10.1007/s00590-015-1597-2. [DOI] [PubMed] [Google Scholar]
- 49.Loftus T.J., Spratling L., Stone B.A., Xiao L., Jacofsky D.J. A patient blood management program in prosthetic joint arthroplasty decreases blood use and improves outcomes. J Arthroplasty. 2016;31(1):11–14. doi: 10.1016/j.arth.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 50.Friedman R., Homering M., Holberg G., Berkowitz S.D. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. The Journal of bone and joint surgery American. 2014;96(4):272–278. doi: 10.2106/JBJS.L.01268. [DOI] [PubMed] [Google Scholar]
- 51.Jans O., Jorgensen C., Kehlet H., Johansson P.I. Role of preoperative anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion. 2014;54(3):717–726. doi: 10.1111/trf.12332. [DOI] [PubMed] [Google Scholar]
- 52.Li J., Zhang Z., Chen J. Comparison of efficacy and safety of topical versus intravenous tranexamic acid in total hip arthroplasty: a meta-analysis. Medicine. 2016;95(36) doi: 10.1097/MD.0000000000004689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shin Y.S., Yoon J.R., Lee H.N., Park S.H., Lee D.H. Intravenous versus topical tranexamic acid administration in primary total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc : official journal of the ESSKA. 2017;25(11):3585–3595. doi: 10.1007/s00167-016-4235-6. [DOI] [PubMed] [Google Scholar]
- 54.Poeran J., Rasul R., Suzuki S. Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasty in the United States: retrospective analysis of effectiveness and safety. Br Med J. 2014;349:g4829. doi: 10.1136/bmj.g4829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Whiting D.R., Gillette B.P., Duncan C., Smith H., Pagnano M.W., Sierra R.J. Preliminary results suggest tranexamic acid is safe and effective in arthroplasty patients with severe comorbidities. Clin Orthop Relat Res. 2014;472(1):66–72. doi: 10.1007/s11999-013-3134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Duncan C.M., Gillette B.P., Jacob A.K., Sierra R.J., Sanchez-Sotelo J., Smith H.M. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty. 2015;30(2):272–276. doi: 10.1016/j.arth.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 57.Drosos G.I., Ververidis A., Valkanis C. A randomized comparative study of topical versus intravenous tranexamic acid administration in enhanced recovery after surgery (ERAS) total knee replacement. J Orthop. 2016;13(3):127–131. doi: 10.1016/j.jor.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bianconi M., Ferraro L., Traina G.C. Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth. 2003;91(6):830–835. doi: 10.1093/bja/aeg277. [DOI] [PubMed] [Google Scholar]
- 59.Kerr D.R., Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop. 2008;79(2):174–183. doi: 10.1080/17453670710014950. [DOI] [PubMed] [Google Scholar]
- 60.Andersen L.O., Kehlet H. Analgesic efficacy of local infiltration analgesia in hip and knee arthroplasty: a systematic review. Br J Anaesth. 2014;113(3):360–374. doi: 10.1093/bja/aeu155. [DOI] [PubMed] [Google Scholar]
- 61.Seangleulur A., Vanasbodeekul P., Prapaitrakool S. The efficacy of local infiltration analgesia in the early postoperative period after total knee arthroplasty: a systematic review and metaanalysis. Eur J Anaesthesiol. 2016;33(11):816–831. doi: 10.1097/EJA.0000000000000516. [DOI] [PubMed] [Google Scholar]
- 64.Ibrahim M.S., Khan M.A., Nizam I., Haddad F.S. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med. 2013;11:37. doi: 10.1186/1741-7015-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Husted H., Lunn T.H., Troelsen A., Gaarn-Larsen L., Kristensen B.B., Kehlet H. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop. 2011;82(6):679–684. doi: 10.3109/17453674.2011.636682. [DOI] [PMC free article] [PubMed] [Google Scholar]