Abstract
The use of transmission precautions such as contact isolation in patients known to be colonised or infected with multidrug-resistant organisms is recommended in healthcare institutions. Although essential for infection control, contact isolation has recently been associated with adverse effects in patients. We undertook a systematic review to determine whether contact isolation leads to psychological or physical problems for patients. Studies were included if (1) hospitalised patients were placed under isolation precautions for an underlying medical indication, and (2) any adverse events related to the isolation were evaluated. We found 16 studies that reported data regarding the impact of isolation on patient mental well-being, patient satisfaction, patient safety or time spent by healthcare workers in direct patient care. The majority showed a negative impact on patient mental well-being and behaviour, including higher scores for depression, anxiety and anger among isolated patients. A few studies also found that healthcare workers spent less time with patients in isolation. Patient satisfaction was adversely affected by isolation if patients were kept uninformed of their healthcare. Patient safety was also negatively affected, leading to an eight-fold increase in adverse events related to supportive care failures. We found that contact isolation may negatively impact several dimensions of patient care. Well-validated tools are necessary to investigate these results further. Large studies examining a number of safety indicators to assess the adverse effects of isolation are needed. Patient education may be an important step to mitigate the adverse psychological effects of isolation and is recommended.
Keywords: Isolation, Patient psychology, Patient safety
Introduction
Antimicrobial resistance has reached near epidemic proportions in US hospitals, leading to establishment of mandatory infection control programmes. Multiple modalities to prevent transmission of resistant organisms have included the development of antimicrobial stewardship programmes, promotion of hand hygiene products, heightened education, and use of strict barrier and isolation precautions.1
Since 1996 the Centers for Disease Control and Prevention (Atlanta, GA, USA) have recommended the use of Standard and Contact Precautions for multidrug-resistant organisms (MDRO) such as meticillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococcus (VRE) and certain Gram-negative bacilli (GNB) that are ‘judged by an infection control program … to be of special clinical and epidemiologic significance.’2
To prevent transmission of these MDRO, use of contact isolation in patients known to be colonised or infected with these MDRO is recommended and widely used in healthcare institutions. Although essential for preventing transmission of multidrug-resistant pathogens in healthcare institutions, patient isolation has recently been associated with adverse effects in patients, including the possibility of less than optimal care.3 For example, some have mentioned that the requirement to wear gown and gloves before patient examination may impede the physician’s ability to perform adequate physical examination, or provide a disincentive for healthcare workers to enter patient rooms.4, 5 Similarly, other studies have pointed out the concern that isolation may negatively affect patients’ mental health.6, 7, 8, 9, 10
We undertook a systematic review of the literature to determine whether or not there are physical and psychological adverse effects that are associated with patient isolation.
Methods
Literature search and selection
We searched the Medline and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases by using the search term ‘isolation’ plus ‘adverse effect’, ‘psychological impact’ or ‘safety’. The search was limited to articles written in the English language, involving either children or adults from 1966 to 30 April 2009. Studies were included if (1) hospitalised patients were placed under isolation precautions for an underlying medical indication (i.e. MDRO infection or immune suppression) and (2) any adverse events related to the isolation were evaluated. A list of trials that did not meet inclusion criteria and the reasons for exclusion are available from the authors.
Data extraction and validity assessment
Data were extracted independently and corroborated by all authors using a standard data collection form. We extracted data on setting, study design, methodologic quality, type of intervention, and outcomes.
Statistical analysis
The studies were descriptive and heterogeneous, and a formal statistical analysis could not be performed.
Results
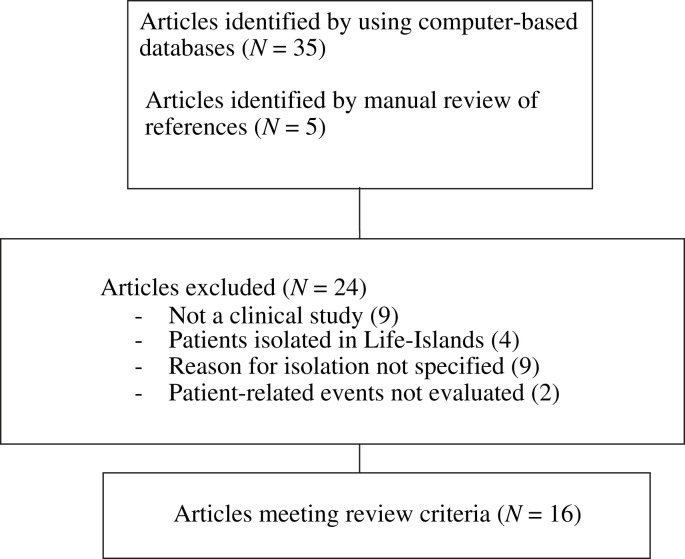
We identified a total of 40 studies that described the use of hospital isolation precautions for a medical indication.1, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 Of these, 16 met our inclusion criteria.1, 4, 5, 9, 10, 26, 27, 28, 31, 32, 34, 36, 37, 39, 40, 42 Two of these articles formed a two-part study series and will be combined in this review henceforth.37, 42 The remainder were excluded due to the following reasons: there was no clinical assessment involved,7, 11, 14, 15, 19, 20, 21, 22, 24 patients were isolated in Life-Islands (germ-free isolation units),16, 18, 23, 25 which are no longer in use, the reason for or specific type of isolation was not specified,6, 8, 12, 29, 30, 33, 35, 38, 41 or patient-related events were not evaluated.13, 17 The details of the literature search leading to final selection are shown in Figure 1 .
Figure 1.
Literature search process.
Of the 15 studies included in the review, seven were case/control studies.1, 5, 10, 26, 27, 28, 39 The rest were prospective cohorts except one which was retrospective.34 There was a single randomised controlled trial.32 Most studies had small sample sizes, of which the smallest was N = 19.34, 36 The largest study comprised a total of 234 patients.39
The majority of the studies included adults.1, 4, 5, 9, 10, 27, 28, 31, 34, 36, 37, 39, 40, 42 There were two studies that included children.2, 26 Most of the studies were located in the general ward; two were undertaken in the intensive care unit,5, 32 and two involved both sites.1, 34 For all included studies, the reason for isolation was infection. Of these, five exclusively identified VRE or MRSA infection.10, 31, 36, 39, 40 Three reported infection with either hospital-acquired or multidrug-resistant organisms.1, 5, 26 One used protective isolation for severe acute respiratory syndrome (SARS),34 and the remaining studies used isolation for infections by several different organisms including Salmonella spp., Clostridium difficile, Scabies spp., and Mycobacterium tuberculosis. 27, 28, 37, 42 Three did not identify the specific type of infections.4, 9, 32 In 11 studies, patients were placed exclusively under contact isolation.4, 5, 9, 10, 27, 28, 31, 32, 36, 39, 40 In the remaining four studies, a combination of either airborne, contact, or droplet precautions was used.1, 26, 34, 37, 42 A summary of study demographics is shown in Table I .
Table I.
Study demographics
| Study | Study design | Controls | Target population | No. of patients (N) cases/controls | Setting | Reason for isolation | Type of isolation |
|---|---|---|---|---|---|---|---|
| Catalano et al.10 | Case–control | Non-isolated patients with infection | Adults | 27/24 | Infectious disease ward | VRE, MRSA | C |
| Cohen et al.26 | Case–control | Patients on standard precautions | Children | 24/41 | Medical ward | HAI | C, A, D |
| Evans et al.1 | Case–control | Non-isolated matched controls in SICU/ward | Adults | 48/48 | Surgical ward/ICU | HAI | C, D |
| Gammon27 | Case–control | Non-isolated patients in the ward for at least 7 days | Adults | 20/20 | Medical ward | Mixed infection | C |
| Gasink et al.28 | Case–control | Non-isolated patients in the ward for at least 3 days | Adults | 43/43 | Medical/surgical ward | Mixed infection | C |
| Kennedy and Hamilton31 | Prospective cohort | – | Adults | 16/16 | Medical ward | MRSA | C |
| Klein et al.32 | Randomised controlled trial | Patients randomised to standard hospital care | Children | 32/38 | ICU | Infection, NS | C |
| Kirkland and Weinstein5 | Case–control | Non-isolated patients in the ICU | Adults | 29/88 | MICU | MDRO | C |
| Maunder et al.34 | Retrospective cohort | – | Adults | 19 | ICU, medical ward | SARS | A, C |
| Newton et al.36 | Prospective cohort | – | Adults | 19 | Medical ward | MRSA | C |
| Rees et al.37, 42 | Prospective cohort | – | Adults | 21 | Rehabilitation ward | Mixed infection | A, C |
| Saint et al.4 | Prospective cohort | – | Adults | 31/108 | Medical ward | Infection, NS | C |
| Stelfox et al.39 | Case–control with two matched cohorts: a general cohort plus a CHF cohort | Non-isolated patient who occupied the same bed, and was admitted immediately before, or after the patient in isolation | Adults | 78/156 (72/144) | Medical ward | MRSA | C |
| Tarzi et al.40 | Prospective cohort | – | Adults | 22/20 | Rehabilitation ward | MRSA | C |
| Wilkins et al.9 | Prospective cohort | – | Adults | 41 | Infectious disease ward | Infection, NS | C |
VRE, vancomycin-resistant enterococcus; MRSA, meticillin-resistant Staphylococcus aureus; HAI, hospital-acquired infection; SICU, surgical intensive care unit; SARS, severe acute respiratory syndrome; NS, not specified; C, contact; A, airborne; D, droplet; CHF, congestive heart failure.
Seven studies used a standardised scoring scale to assess the psychological impact of isolation.9, 10, 27, 28, 31, 37, 40, 42 These included Hamilton Anxiety/Depression Rating Scale (HAM-D or HAM-A), Hospital Anxiety and Depression Scale (HADS), Health Illness Questionnaire (HIQ), Self-Esteem Scale (SES), Consumer Assessment of Healthcare Providers and Systems (CAHPS), Beck Depression Inventory (BDI), State Anxiety Inventory (STAI), Profile of Mood States (POMS), Abbreviated Mental Test Score (AMTS), Barthel Index, Geriatric Depression Scale (GDS), and Crown–Crisp Experiential Index (CCEI). Two studies developed their own questionnaire or patient survey to evaluate their primary outcomes.1, 26 Three other studies used direct observation,4, 5, 32 and two used the interview method.34, 36 A number of studies used one or more of these methods in combination (Table II ).1, 26, 39
Table II.
Summary of study methodology and outcomes
| Study | Methodology | Psychometric tools | Main outcome | Time of assessment | Results |
|---|---|---|---|---|---|
| Catalano et al.10 | Psychometric tools | Hamilton Depression Rating Scale (HAM-D), Hamilton Anxiety Rating Scale (HAM-A) | Psychological impact | At day 7 and day 14 | HAM-D and HAM-A scores were higher for cases than controls (P < 0.0001) |
| Cohen et al.26 | Direct observation by a single worker not part of the healthcare team during morning rounds. Questionnaire |
Pediatric Family Satisfaction Questionnaire (PFSQ) | Time spent in direct patient care. Quality of care |
At 48 h | No difference in either direct patient care or quality of care |
| Evans et al.1 | Direct observation by a healthcare worker. Questionnaire |
16 item questionnaire | Time spent in direct patient care | 2 h daily for 5 weeks | No. of encounters/h and contact time/h was higher for non-isolated than for isolated (P < 0.001, and P = 0.0078) |
| Gammon27 | Multiple psychometric tools | Hospital Anxiety and Depression Scale (HADS), Health Illness Questionnaire (HIQ), Self-Esteem Scale (SES) | Psychological impact | At day 7 | Mean Anxiety and Depression scores higher in isolated patients (P < 0.001, and P < 0.001). Mean self-esteem scores lower in isolated patients (P < 0.005) |
| Gasink et al.28 | Questionnaire | Consumer Assessment of Healthcare Providers and Systems (CAHPS) | Patient care satisfaction | At day 3 | No difference in patient care satisfaction |
| Kennedy and Hamilton31 | Multiple psychometric tools | Beck Depression Inventory (BDI), State Anxiety Inventory (STAI –Form), Profile of Mood States (POMS) | Psychological impact | In isolation for at least 2 weeks | Isolated patients with higher POMS Anger–Hostility scores |
| Klein et al.32 | Direct observation by investigator | – | Incidence of nosocomial infection | For 1 h on days 1, 3 and 7 | Isolation reduced nosocomial infection rates. Patient care was not compromised, and isolation was well-tolerated |
| Kirkland and Weinstein5 | Direct observation (not specified by whom) | – | Frequency of patient encounters | 35 observation periods lasting 1 h each, over 7 months | Patients in isolation: fewer room entries/h (P = 0.06), contacts/h (P = 0.03). No difference in duration of interaction (P = 0.6) |
| Maunder et al.34 | Interview of patients with and without SARS by mental health professionals and consultation–liaison psychiatrists | – | Psychological impact | 4 weeks | Isolated patients reported fear, loneliness, anxiety, depression |
| Newton et al.36 | Interview by infection control nurse | – | Psychological impact | During isolation | Mixed patient experiences during isolation |
| Rees et al.37, 42 | Psychometric tools | HADS | Psychological impact and patient satisfaction | During isolation | 12/21 had depression, based on HADS. Satisfaction was related to information/education |
| Saint et al.4 | Direct observation by study investigator | – | Time spent in direct patient care | On several days/month for 6 months, during morning rounds | Attending physicians spent less time examining patients in isolation (RR = 0.49, P < 0.001) |
| Stelfox et al.39 | Medical chart review | – | Patient adverse events, described as injuries caused by medical management | During isolation | Cases had fewer vital sign recordings (P = 0.02), less nursing narrative (P < 0.001) and physician notes (P < 0.001) in the chart, and were twice as likely to experience adverse events (20 vs 3/1000 days, P < 0.001). Cases had more complaints and were less satisfied with their care (30 vs 8, P < 0.001) |
| Tarzi et al.40 | Multiple psychometric tools | Abbreviated Mental Test Score (AMTS), Barthel Index (BI), Geriatric Depression Scale (GDS), POMS | Psychological impact | – | GDS scores were higher in isolated patients (P < 0.01) |
| Wilkins et al.9 | Psychometric tools | Crown–Crisp Experiential Index (CCEI) | Psychological impact | On admission | Admission scores for hysteria, anxiety and total scores were increased for patients in isolation |
Study results and outcome
Impact of isolation on patient psychological well-being
The main outcome for most of the studies was assessment of the impact of isolation on patient psychology and behaviour.9, 10, 27, 31, 34, 36, 40 A few studies focused on the effect of isolation on patient safety,39 satisfaction,28 or time spent in direct patient care.1, 4, 5, 26 Rees et al. focused on the impact of isolation on both patient psychology and satisfaction.37, 42 The primary outcome of the study by Klein et al. was incidence of nosocomial infection, but it also examined the influence of isolation on quality of care.32
Among the studies that focused on the psychological impact of isolation, the majority showed a negative impact on patient psychology and behaviour, including higher scores for depression and anxiety,9, 10, 27, 40 higher anger–hostility scores,31 and reports of fear and loneliness.34, 36
In the study by Catalano et al., for example, the HADS scores of patients in isolation increased in proportion to their length of isolation, from 7.25 at baseline to 8.83 at week 1 and 11.5 at week 2.10 By contrast, the scores of controls decreased from 9.78 at baseline to 5.44 at week 1, and finally 4.22 at week 2 (P < 0.001). Similarly, Gammon found that patients on day 7 of isolation also had higher mean scores for anxiety (12.75 vs 8.15) and depression (12.45 vs 7.3), and lower self-esteem scores (14.35 vs 16.1) compared to controls.27 Tarzi et al. also found that patients in isolation had significantly higher rates of depression (P < 0.01) and anxiety (P < 0.02) than non-isolated patients.40 There was no significant difference in anger scores. By contrast, Kennedy and Hamilton did not find any statistically significant difference in terms of depression and anxiety between isolated and non-isolated patients, but found higher anger–hostility mean scores for patients in isolation (12.4 vs 4.9, P = 0.037).31
Maunder et al. focused on the psychosocial response of both patients and healthcare staff to a SARS outbreak.34 Although no quantitative analysis was performed, the authors found that in patients isolated for SARS, the most prominent emotional effects included fear, loneliness, boredom and anger. In Rees et al.’s cohort where patients were isolated for different types of infections, they found that 12 of 21 patients had mood disturbances as evidenced by high HADS scores.37, 42 In Newton et al.’s study, among a total of 19 patients, seven felt isolated and complained about lack of attention from nursing staff. Nevertheless 10 patients identified the positive impact of isolation including greater freedom and privacy. Interestingly, most of the patients did not have a clear understanding for the reason for isolation.36 Wilkins et al. had a cohort of 41 isolated patients.9 Their CCEI scores for anxiety and hysteria were found to be higher than that in the general population. Scores were also higher on admission than on discharge. Not surprisingly, history of mental illness was associated with higher scores for anxiety.
Impact of isolation on patient contact, satisfaction and safety
Four studies focused on the difference in time spent in direct patient contact.1, 4, 5, 26 In the study by Evans et al., there was a total of 485 patient–provider encounters spent with patients in isolation over a period of 91.6 h (5.3 encounters/h), compared with 1002 encounters in non-isolated patient rooms observed for 91.2 h (10.9 encounters/h).1 In addition, they found that providers spent less time with isolated versus non-isolated patients regardless of whether it was in the ward (29 ± 5 vs 37 ± 3, P = 0.008) or ICU setting (42 ± 10 vs 47 ± 5 min/h, P = 0.03). Similarly, Kirkland and Weinstein also found that healthcare workers were about two times less likely to enter the room of patients in contact isolation, with mean room entry/h of 3.9 vs 7.9 (P = 0.06).5 Contact was also two-fold less in isolated patients, with mean contacts/h of 2.1 vs 4.2 (P = 0.03). The duration of interaction was not significantly different between isolated patients and controls (4.5 vs 2.8, P = 0.6). By contrast, Saint et al. found no difference in the number of examinations by senior medical residents among patients in isolation and controls [risk ratio (RR) = 0.96, P = 0.58].4 However, attending physicians examined patients in isolation less frequently than their non-isolated counterparts (RR = 0.49, P < 0.001).
Two studies showed no difference in either direct patient care or quality of care between isolated patients and controls.26, 32 In the study by Cohen et al., attending physicians were found to spend an average of 9 min in the patients’ rooms, regardless of whether they were in isolation or not (516 vs 480, P = 0.503). Overall PFSQ scores, to assess quality of care were also similar in both groups (4.7 vs 4.8, P = 0.209).26 Similarly Klein et al. found that frequency of contact between patients in isolation and between those under standard precautions was comparable. Patients in isolation also tolerated this well, without apparent adverse effects.32
Gasink et al. evaluated patient satisfaction by using the CAHPS survey.28 Among a cohort of 86 patients, of whom half were isolated, they did not find any statistical difference between the responses of patients in isolation and patients not in isolation, regarding inpatient care. Of the 39 patients in isolation, only 3 (7.7%) thought that isolation worsened their care, whereas 24 (61.5%) thought that it improved theirs. In the second part of the two-part study by Rees et al., patient satisfaction was greatest in the patients who were kept informed regarding their care.37 Among the 21 patients, 66.7% felt that they were given enough information, and 85.7% felt that they knew someone they could ask regarding healthcare issues.
In a study that assessed patient safety, the authors found that compared with patients not in isolation, isolated patients had more errors in processes of care, and had increased likelihood for adverse events.39 For example, isolated patients were more likely to have either incomplete recordings of vital signs (14 vs 9%, P < 0.001), or to have days with no vital sign recordings at all (5 vs 1%, P = 0.02). In addition, they had more days with either no nursing narrative notes (14 vs 10%, P < 0.001), or physician progress notes (26 vs 13%, P < 0.001) recorded in the chart. Isolated patients were twice as likely as control patients to experience adverse events per 1000 days (31 vs 15, P < 0.001). This reflected preventable (20 vs 3, P < 0.001) as opposed to non-preventable events (11 vs 12, P = 0.98). Specifically, patients in isolation were as much as eight times more likely to experience supportive care failures such as falls, ulcers, and fluid and electrolyte abnormalities. There were no significant differences in terms of severity of adverse event or death. Not surprisingly, patients in isolation expressed greater dissatisfaction regarding their care, as reflected by both formal and informal complaints (30 vs 8%, P < 0.001). A summary of these findings is shown in Table II.
Discussion
Our systematic review examines the impact of isolation precautions on patients’ psychological well-being, provider contact with patient, patient satisfaction and patient safety. The majority of the literature we reviewed suggests that adverse psychological consequences of isolation exist. Our results update, and are in keeping with, a recent systematic review published on this subject.43
Most of the studies that focused on patient psychology used standardised scoring scales to assess patient mood and behaviour. However, the use of several different scoring scales makes comparison among studies challenging. In addition, the timing of assessment during isolation was also highly varied. This may have impacted the overall results because of recall bias. Nevertheless, the majority of studies found that the physical process of isolation has a negative impact on patients’ moods, including increased rates of depression, anxiety, fear, and hostility.
The reason behind the psychologically negative effects of isolation is probably linked to uncertainty and loss of control, which is derived from multiple sources, but ultimately stems from isolation itself.27 Some authors have suggested that preparing these patients emotionally, prior to isolation, may help decrease their anxiety.29 Similarly, patient education regarding the isolation may also be beneficial and may help patients understand the necessity for isolation and cope with it better.33 Rees et al.’s study corroborates this, as they found that a patient’s satisfaction, regardless of being in source isolation, was highly associated with keeping in good communication with their healthcare providers.37 The Joint Commission’s Patient Safety Goals for 2009 include a recommendation for patient education regarding MDRO and isolation.
We found that although patient isolation is an established and important aspect of infection control, it may also negatively influence direct patient care. Studies included in our review found that time spent by healthcare professionals in direct patient care is either less frequent or shorter with patients in isolation, than with patients not in isolation. Some have postulated that the requirement to don a gown and a pair of gloves has itself become a barrier for healthcare workers, as it provides an additional, occasionally cumbersome, step that needs to be performed prior to entering patients’ rooms. Whether the less frequent contact or shorter time spent with patients is associated with adverse clinical outcomes is unclear, but deserves further study.
Our review has several limitations. We only included studies in the English language. Several other studies done in laminar air-flow units, and which also looked at the impact of source isolation on patient psychology, were excluded due to the lack of information regarding the specific type of isolation. The studies were limited by sample size, were heterogeneous, and lacked adjustment for severity of illness.
In conclusion, we find that although studies have shown that isolation may negatively impact patient psychological well-being, patient safety and satisfaction, and patient care, well-validated tools and larger studies are needed to examine this further. Patient education at the time of isolation is a critical component of the process to reduce anxiety and distress. Future studies to assess the adverse impact of isolation precautions should examine a broader array of safety indicators, in addition to the psychological aspects. As the problem of antibiotic-resistant bacteria in healthcare institutions continues to grow, isolation will remain and increase in importance as a critical infection control intervention to reduce nosocomial transmission of MDRO. Attention must be paid to the possible collateral damage of isolation, and adverse effects should be monitored closely.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Evans H.L., Shaffer M.M., Hughes M.G. Contact isolation in surgical patients: a barrier to care? Surgery. 2003;134:180–188. doi: 10.1067/msy.2003.222. [DOI] [PubMed] [Google Scholar]
- 2.Siegel J., Rhinehart E., Jackson M., Chiarello L. Centers for Disease Control and Prevention; Atlanta: 2006. Management of multidrug-resistant organisms in healthcare settings. pp. 1–72. [Google Scholar]
- 3.Koss W.G., Khalili T.M., Lemus J.F., Chelly M.M., Margulies D.R., Shabot M.M. Nosocomial pneumonia is not prevented by protective contact isolation in the surgical intensive care unit. Am Surg. 2001;67:1140–1144. [PubMed] [Google Scholar]
- 4.Saint S., Higgins L.A., Nallamothu B.K., Chenoweth C. Do physicians examine patients in contact isolation less frequently? A brief report. Am J Infect Control. 2003;31:354–356. doi: 10.1016/s0196-6553(02)48250-8. [DOI] [PubMed] [Google Scholar]
- 5.Kirkland K.B., Weinstein J.M. Adverse effects of contact isolation. Lancet. 1999;354:1177–1178. doi: 10.1016/S0140-6736(99)04196-3. [DOI] [PubMed] [Google Scholar]
- 6.Hollenbeck A.R., Susman E.J., Nannis E.D. Children with serious illness: behavioral correlates of separation and isolation. Child Psychiatry Hum Dev. 1980;11:3–11. doi: 10.1007/BF00705865. [DOI] [PubMed] [Google Scholar]
- 7.Peel R.K., Stolarek I., Elder A.T. Is it time to stop searching for MRSA? Isolating patients with MRSA can have long term implications. BMJ. 1997;315:58. [PMC free article] [PubMed] [Google Scholar]
- 8.Powazek M., Goff J.R., Schyving J., Paulson M.A. Emotional reactions of children to isolation in a cancer hospital. J Pediatr. 1978;92:834–837. doi: 10.1016/s0022-3476(78)80170-x. [DOI] [PubMed] [Google Scholar]
- 9.Wilkins E.G., Ellis M.E., Dunbar E.M., Gibbs A. Does isolation of patients with infections induce mental illness? J Infect. 1988;17:43–47. doi: 10.1016/s0163-4453(88)92308-0. [DOI] [PubMed] [Google Scholar]
- 10.Catalano G., Houston S.H., Catalano M.C. Anxiety and depression in hospitalized patients in resistant organism isolation. South Med J. 2003;96:141–145. doi: 10.1097/01.SMJ.0000050683.36014.2E. [DOI] [PubMed] [Google Scholar]
- 11.Lewis A.M., Gammon J., Hosein I. The pros and cons of isolation and containment. J Hosp Infect. 1999;43:19–23. doi: 10.1053/jhin.1999.0638. [DOI] [PubMed] [Google Scholar]
- 12.Meehan T., Bergen H., Fjeldsoe K. Staff and patient perceptions of seclusion: has anything changed? J Adv Nurs. 2004;47:33–38. doi: 10.1111/j.1365-2648.2004.03062.x. [DOI] [PubMed] [Google Scholar]
- 13.Bennett S.M. ‘Patient perspective’ – psychological effects of barrier nursing isolation. Aust Nurses J. 1983;12:36–37. 44. [PubMed] [Google Scholar]
- 14.Denton P.F. Psychological and physiological effects of isolation. Nursing (Lond) 1986;3:88–91. [PubMed] [Google Scholar]
- 15.Gammon J. The psychological consequences of source isolation: a review of the literature. J Clin Nurs. 1999;8:13–21. doi: 10.1046/j.1365-2702.1999.00201.x. [DOI] [PubMed] [Google Scholar]
- 16.Graubert D.M., Edmonson J.H. Psychologic adaptation of patients isolated in protected environments. N Y State J Med. 1972;72:227–228. [PubMed] [Google Scholar]
- 17.Khan F.A., Khakoo R.A., Hobbs G.R. Impact of contact isolation on health care workers at a tertiary care center. Am J Infect Control. 2006;34:408–413. doi: 10.1016/j.ajic.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 18.Kohle K., Simons C., Weidlich S., Dietrich M., Durner A. Psychological aspects in the treatment of leukemia patients in the isolated-bed system ‘life island’. Psychother Psychosom. 1971;19:85–91. doi: 10.1159/000286309. [DOI] [PubMed] [Google Scholar]
- 19.Lesko L.M., Kern J., Hawkins D.R. Psychological aspects of patients in germ-free isolation: a review of child, adult, and patient management literature. Med Pediatr Oncol. 1984;12:43–49. doi: 10.1002/mpo.2950120111. [DOI] [PubMed] [Google Scholar]
- 20.MacKellaig J.M. A study of the psychological effects of intensive care with particular emphasis on patients in isolation. Intensive Care Nurs. 1987;2:176–185. doi: 10.1016/0266-612x(87)90130-1. [DOI] [PubMed] [Google Scholar]
- 21.Madeo M. The psychological impact of isolation. Nurs Times. 2003;99:54–55. [PubMed] [Google Scholar]
- 22.Mirand E.A., Mirand A.A. Psychological response of patients to protective environments. Prog Clin Biol Res. 1983;132C:397–408. [PubMed] [Google Scholar]
- 23.Oldman T. Isolated cases. Nurs Times. 1998;94:67–70. [PubMed] [Google Scholar]
- 24.Rooymans H.G., Kraal-Dingjan C.G., Pluut R.A., Zwaan F.E. Psychological aspects of the treatment of patients with bone marrow insufficiency. Neth J Med. 1979;22:138–142. [PubMed] [Google Scholar]
- 25.Simons C., Kohle K., Genscher U., Dietrich M. The impact of reverse isolation on early childhood development. Two and a half years of treatment in plastic isolation systems. Psychother Psychosom. 1973;22:300–309. doi: 10.1159/000286535. [DOI] [PubMed] [Google Scholar]
- 26.Cohen E., Austin J., Weinstein M., Matlow A., Redelmeier D.A. Care of children isolated for infection control: a prospective observational cohort study. Pediatrics. 2008;122:e411–e415. doi: 10.1542/peds.2008-0181. [DOI] [PubMed] [Google Scholar]
- 27.Gammon J. Analysis of the stressful effects of hospitalisation and source isolation on coping and psychological constructs. Int J Nurs Pract. 1998;4:84–96. doi: 10.1046/j.1440-172x.1998.00084.x. [DOI] [PubMed] [Google Scholar]
- 28.Gasink L.B., Singer K., Fishman N.O. Contact isolation for infection control in hospitalized patients: is patient satisfaction affected? Infect Control Hosp Epidemiol. 2008;29:275–278. doi: 10.1086/527508. [DOI] [PubMed] [Google Scholar]
- 29.Holland J., Plumb M., Yates J. Psychological response of patients with acute leukemia to germ-free environments. Cancer. 1977;40:871–879. doi: 10.1002/1097-0142(197708)40:2<871::aid-cncr2820400241>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 30.Kellerman J., Rigler D., Siegel S.E. The psychological effects of isolation in protected environments. Am J Psychiatry. 1977;134:563–565. doi: 10.1176/ajp.134.5.563. [DOI] [PubMed] [Google Scholar]
- 31.Kennedy P., Hamilton L.R. Psychological impact of the management of methicillin-resistant Staphylococcus aureus (MRSA) in patients with spinal cord injury. Spinal Cord. 1997;35:617–619. doi: 10.1038/sj.sc.3100469. [DOI] [PubMed] [Google Scholar]
- 32.Klein B.S., Perloff W.H., Maki D.G. Reduction of nosocomial infection during pediatric intensive care by protective isolation. N Engl J Med. 1989;320:1714–1721. doi: 10.1056/NEJM198906293202603. [DOI] [PubMed] [Google Scholar]
- 33.Knowles H.E. The experience of infectious patients in isolation. Nurs Times. 1993;89:53–56. [PubMed] [Google Scholar]
- 34.Maunder R., Hunter J., Vincent L. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can Med Assoc J. 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 35.Meyers C.A., Weitzner M., Byrne K., Valentine A., Champlin R.E., Przepiorka D. Evaluation of the neurobehavioral functioning of patients before, during, and after bone marrow transplantation. J Clin Oncol. 1994;12:820–826. doi: 10.1200/JCO.1994.12.4.820. [DOI] [PubMed] [Google Scholar]
- 36.Newton J.T., Constable D., Senior V. Patients’ perceptions of methicillin-resistant Staphylococcus aureus and source isolation: a qualitative analysis of source-isolated patients. J Hosp Infect. 2001;48:275–280. doi: 10.1053/jhin.2001.1019. [DOI] [PubMed] [Google Scholar]
- 37.Rees J., Davies H.R., Birchall C., Price J. Psychological effects of source isolation nursing (2): patient satisfaction. Nurs Stand. 2000;14:32–36. doi: 10.7748/ns2000.04.14.29.32.c2805. [DOI] [PubMed] [Google Scholar]
- 38.Sasaki T., Akaho R., Sakamaki H. Mental disturbances during isolation in bone marrow transplant patients with leukemia. Bone Marrow Transplant. 2000;25:315–318. doi: 10.1038/sj.bmt.1702117. [DOI] [PubMed] [Google Scholar]
- 39.Stelfox H.T., Bates D.W., Redelmeier D.A. Safety of patients isolated for infection control. JAMA. 2003;290:1899–1905. doi: 10.1001/jama.290.14.1899. [DOI] [PubMed] [Google Scholar]
- 40.Tarzi S., Kennedy P., Stone S., Evans M. Methicillin-resistant Staphylococcus aureus: psychological impact of hospitalization and isolation in an older adult population. J Hosp Infect. 2001;49:250–254. doi: 10.1053/jhin.2001.1098. [DOI] [PubMed] [Google Scholar]
- 41.Ward D. Infection control: reducing the psychological effects of isolation. Br J Nurs. 2000;9:162–170. doi: 10.12968/bjon.2000.9.3.162. [DOI] [PubMed] [Google Scholar]
- 42.Rees J. Psychological effects of isolation nursing (1): mood disturbance. Nurs Stand. 2000;14:35–38. doi: 10.7748/ns2000.03.14.28.35.c2799. [DOI] [PubMed] [Google Scholar]
- 43.Morgan D.J., Diekema D.J., Sepkowitz K., Perencevich E.N. Adverse outcomes associated with contact precautions: a review of the literature. Am J Infect Control. 2009;37:85–93. doi: 10.1016/j.ajic.2008.04.257. [DOI] [PMC free article] [PubMed] [Google Scholar]