Abstract
Objectives
We explored how experience of arthrography affects treatment preferences for Legg-Calvé-Perthes disease (LCPD) patients. We also examined changes in surgical procedure preferences after examining arthrography images. In addition, we analysed the effect of experience with arthrography on treatment and surgical modality preferences.
Methods
A case-based questionnaire was completed by 26 participants. Information on age, symptoms, hip range of motion (ROM), and extremity length differences were provided for eight LCPD cases. Based on these data and roentgenography images of the cases, the respondents were questioned regarding diagnostic, treatment, and surgical preferences. A slide was shown of arthrography images of each case and the same questions were asked to determine any changes in treatment preferences. The participants were divided into arthrography-experienced (Group 1, n = 16) and -inexperienced (Group 2, n = 10) groups to determine differences in treatment preferences in association with experience.
Results
After the participants had examined the arthrography images, a significant decrease in the number of additional examination requests was observed (p < 0.001). A significant group difference was also found in the rate of change of preference in diagnostic modality (p < 0.001).
After arthrography images were examined, the tendency towards a preference for surgery increased in all participants. However, no significant difference between the experience groups was observed (p = 0.193). In addition, after arthrography images were examined, there was an increased tendency towards a preference for femoral valgisation and Salter osteotomy among participants who chose surgical treatments (p = 0.408). The treatment preferences difference between the two experience groups were not significant, and nor was the preference regarding surgical procedures (p = 0.999).
Conclusions
Previous studies have shown that arthrography is useful for planning treatment and informing decisions regarding surgical modality for LCPD. However, no study has explored changes in treatment preferences after viewing arthrography images. This study explored such changes in choices regarding the diagnostic method and treatment modality. Our study showed that experience with arthrography decreased the preference for additional diagnostic tests (p < 0.001). Experience of arthrography increased the preference for surgery, though not significantly (p = 0.193).
Keywords: Perthes disease, Arthrography, Treatment
1. Introduction
Legg-Calvé-Perthes disease (LCPD) is characterised by osteonecrosis of the femoral head, epiphysis, chondronecrosis, and growth arrest of the ossification nucleus.1 The incidence of LCPD in the USA was reported to be 5.1–5.7/100,000.2 Although LCPD typically affects children aged 4–8 years, it can occur in children at any time between 18 months and skeletal maturity. LCPD is four-fold more common in males than females.1
Radiological methods that can be used for diagnosis of LCPD include X-ray, ultrasonography, magnetic resonance imaging (MRI), scintigraphy, computed tomography (CT), and arthrography.1,3, 4, 5, 6, 7, 8, 9 Hip arthrography is a very useful diagnostic modality for LCPD, showing the femoral head and acetabular cartilage.8,9 Another important advantage of arthrography is the ability to dynamically evaluate joint compliance in many different positions. In 1992, Laredo analysed 105 hips and devised arthrographic classifications based on the position, shape and size of the femoral head and acetabular labrum.
The primary role of arthrography is to evaluate containment of the femoral head. In the earliest stage of LCPD, arthrography is rarely useful and findings may be normal.10 It is more reasonable to use arthrography in cases with severe collapse or flattening of the femoral head. The optimal position for femoral head containment and hinge abduction can be verified by arthrography.11 In 2007, Devalia et al. explored the role of arthrography for diagnosing LCPD. They showed that arthrography is useful in cases of late LCPD where valgus osteotomy may be appropriate, and in unusual cases where clinical findings are inconclusive and the optimal treatment modality is thus uncertain.12
We explored how preoperative experience of arthrography affects treatment decisions and choice of surgical procedure among surgeons. We also explored changes in the desired diagnostic method based on viewing arthrography images. In addition, we analysed the effect of experience with arthrography on treatment preferences.
2. Methods
A total of 26 participants were included in this study; 16 of the participants had experience with paediatric orthopaedic surgery (Group 1) and 10 did not (Group 2). The experienced group included professors in university hospitals with at least ten year experience in paediatric orthopaedics. The inexperienced group interacted with general orthopaedic surgeons and worked in government hospitals at least for ten years.
The questionnaire included roentgenogram and arthrogram images of eight LCPD cases differing in LCPD severity according to the Catterall classification (stage 2, n = 3; stage 3, n = 4; stage 4, n = 1). Incomplete questionnaires were returned by five participants; these were excluded from the analysis.
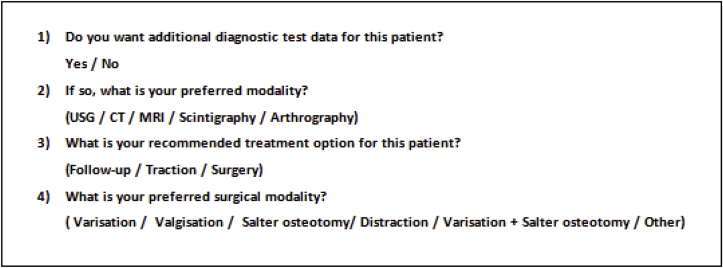
Information on age, symptoms, hip range of motion (ROM), and extremity length differences was provided on the first of a series of slides. On the second slide, anteroposterior (AP) and frog leg views of the pelvis were shown (Fig. 1). On slide 3, participants were asked specific questions including preferences regarding diagnostic, treatment, and surgical modalities (the latter only for those who preferred surgical treatment) (Fig. 2). We showed the participants arthrography images after the questionnaires were completed (Fig. 3), following which the same questions were asked again. Among the arthrography images, the best evaluating images of hinge abduction were presented to the participants. A computer programmer wrote a Representational State Transfer (RESTful) program. We removed the session information and JavaScript answers on/to all questions to prevent participants from moving back through the slide deck. A link to the questionnaire was sent to each participant by e-mail.
Fig. 1.
Example roentgenography image. (A: neutral AP view; B: frog leg view).
Fig. 2.
Questions asked before viewing the arthrography images.
Fig. 3.
Example arthrography images. (A: neutral AP view; B: frog leg view).
Questionnaire responses before and after experience of arthrography were also compared. We examined the effect of experience with arthrography on additional diagnostic modality preferences and medical decision-making. In addition, changes in preferences between the arthrography-experienced and -inexperienced groups were examined.
SPSS software (ver. 24.0; IBM Corp., Armonk, NY, USA) was used to analyse the data. Fisher's exact test was used to analyse categorical variables; 95% confidence levels were calculated and p < 0.05 was considered significant. All statistical analyses were performed by a biostatistics expert.
3. Results
A total of 208 responses (26 participants x 8 cases) to questionnaire items (before and after viewing arthrography images of eight LCPD cases), and changes in answers after viewing the images, were examined; the effect of experience with arthrography on the responses was also assessed (Table 1).
Table 1.
Questionnaire responses before and after viewing the arthrography images.
| Questions | Experience level |
p-value | ||
|---|---|---|---|---|
| Experienced |
Inexperienced |
Total |
||
| n (%) | n (%) | n (%) | ||
| Do you want additional diagnostic test data for this patient? | ||||
| Unchanged | 77 | 46 | 123 (59.1) | 0.772 a |
| Changed |
51 |
34 |
85 (40.9) |
|
|
Total |
128 (61.5) |
80 (38.5) |
208 (100.0) |
|
| If so, what is your preferred modality? | ||||
| Unchanged | 19 | 2 | 21 (70.0) | 0.999 b |
| Changed |
8 |
1 |
9 (30.0) |
|
|
Total |
27 (90.0) |
3 (10.0) |
30 (100.0) |
|
| What is your recommended treatment option for this patient? | ||||
| Unchanged | 110 | 68 | 178 (85.6) | 0.999 a |
| Changed |
18 |
12 |
30 (14.4) |
|
|
Total |
128 (61.5) |
80 (38.5) |
208 (100.0) |
|
| What is your preferred surgical modality? | ||||
| Unchanged | 57 | 25 | 82 (85.4) | 0.999 b |
| Changed |
10 |
4 |
14 (14.6) |
|
| Total | 67 (69.8) | 29 (30.2) | 96 (100.0) | |
Pearson's chi-squared test.
Fisher's exact test.
The distribution of answers to the question "Would you request additional diagnostic tests for this patient?" is shown in Table 2. A total of 55.3% respondents requested additional diagnostic tests before viewing the arthrography images and this decreased to 13.9% after viewing the images (p < 0.001).
Table 2.
Responses to the question: “Would you request additional diagnostic tests for this patient?”
| Would you request additional diagnostic tests for this patient? |
After viewing the images |
Total |
p-value (K) | ||
|---|---|---|---|---|---|
| Yes |
No |
||||
| Before viewing the images | N (%) | N (%) | N (%) | ||
| Total | Yes | 29 (100.0) | 86 (48.1) | 115 (55.3) | <0.001 |
|
No |
0 (0.0) |
93 (51.9) |
93 (44.7) |
||
| Total | 29 (13,9) | 179 (86.1) | 208 (100.0) | ||
Data were compared using the McNemar test.
The variation in additional test preferences is summarised in Table 3. None of the participants requested ultrasonography (USG) before or after arthrography, after examining the X-ray images. A total of 72 participants asked to see the arthrography images before deciding upon the treatment method. Before seeing the arthrography images, 36 participants requested MRI, but after seeing the images this number decreased to 22 (p < 0.001).
Table 3.
Participant responses to the question: “If so, what is your preferred modality?”
| Before viewing the arthrography images | |||||||
|---|---|---|---|---|---|---|---|
| After viewing the arthrography images | USG | CT | MRI | Scintigraphy | Arthrography | Total | |
| USG | 0 | 0 | 0 | 0 | 0 | 0 | |
| CT | 0 | 6 | 0 | 0 | 0 | 6 | |
| MRI | 0 | 0 | 14 | 0 | 8 | 22 | |
| Scintigraphy | 0 | 0 | 0 | 1 | 1 | 2 | |
| Arthrography | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | 0 | 6 | 14 | 1 | 9 | ||
USG, ultrasonography; CT, computed tomography; MRI, magnetic resonance imaging.
Data are the numbers of responses.
The decrease in the number of requests for additional examinations, and the change in type of examination requested, were significant when evaluating all participants (p < 0.001) (Table 2) However, no significant group difference was found in either parameter (p = 0.772) (Table 1).
Before viewing the arthrography images, there were 95 responses (45.7%) of “follow-up” to the question of "What is your recommended treatment option for this patient?"; this number decreased to 89 (42.8%) after viewing the arthrography images. For the same question, 103 (49.5%) responses were of “surgery”, and this number increased to 111 (53.4%) after viewing the arthrography images (Table 4). Thus, viewing the arthrography images increased the preference for surgical treatment, albeit not significantly (p = 0.193). There a significant group difference in the extent of the increase in preference for surgery for case 3 only (p = 0.008) (Fig. 4).
Table 4.
Participant responses to the question: “What is your recommended treatment option for this patient?”
| What is your recommended treatment option for this patient? | Experience of arthrography |
Inexperienced |
Total |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before viewing the arthrography images |
Before viewing the arthrography images |
Before viewing the arthrography images |
||||||||||
| Follow-up |
Traction |
Surgery |
Total |
Follow-up |
Traction |
Surgery |
Total |
Follow-up |
Traction |
Surgery |
Total |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| After viewing the arthrography images | ||||||||||||
| Follow-up | 44 | 0 | 6 | 50 (39.1) | 35 | 0 | 4 | 39 (48.8) | 79 | 0 | 10 | 89 (42.8) |
| Traction | 0 | 3 | 1 | 4 (3.1) | 0 | 4 | 0 | 4 (5.0) | 0 | 7 | 1 | 8 (3.8) |
| Surgery |
9 |
2 |
63 |
74 (57.8) |
7 |
1 |
29 |
37 (46.3) |
16 |
3 |
92 |
111 (53.4) |
|
Total |
53 (41.4) |
5 (3.9) |
70 (54.7) |
128 (100) |
42 (52.5) |
5 (6.3) |
33 (41.3) |
80 (100) |
95 (45.7) |
10 (4.8) |
103 (49.5) |
208 (100) |
| p-value | 0.445 | 0.376 | 0.193 | |||||||||
Data were compared using the marginal homogeneity test.
Fig. 4.
Legg-Calvé-Perthes disease (LCPD): roentgenography and arthrography images for case 3.
(A: neutral AP view roentgenography; B: arthrographic neutral AP view; C: arthrographic frog leg view).
Surgical preferences are detailed in Table 5. Varisation was the preferred choice in 42 cases before examining the arthrography images, and in 37 after viewing the images; the difference was not significant (p = 0.408). The preference for valgisation increased after viewing the images (25 responses vs. 20 pre-image viewing), as did the preference for Salter osteotomy (from 9 to 12 responses), but not significantly (p = 0.408).
Table 5.
Participant responses to the question: “What is your preferred surgical modality?”
| What is your preferred surgical modality? | Conservative | Before viewing the arthrography images |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Varisation | Valgisation | Salter | Distraction | Varisation + Salter osteotomy | Other | Total | |||
| After viewing the arthrography images | Conservative | 83 | 5 | 4 | 0 | 0 | 1 | 2 | 95 |
| Varisation | 3 | 32 | 0 | 0 | 0 | 0 | 2 | 37 | |
| Valgisation | 6 | 3 | 15 | 0 | 0 | 0 | 1 | 25 | |
| Salter | 2 | 1 | 0 | 7 | 0 | 1 | 1 | 12 | |
| Distraction | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 2 | |
| Varisation + Salter osteotomy | 4 | 1 | 0 | 1 | 0 | 9 | 1 | 16 | |
| Others | 2 | 0 | 1 | 0 | 0 | 0 | 18 | 21 | |
| Total | 100 | 42 | 20 | 9 | 1 | 11 | 25 | 208 | |
Data are the numbers of responses.
4. Discussion
LCPD onsets in childhood and causes hip pain and arthrosis in adults. Early diagnosis and appropriate treatment are important when interventions are required in adulthood. Spherity and coverage of the femoral head are important in terms of disease prognosis.9 Treatment is based on the concept of "containment". Therefore, dynamic visualisation of containment is important.13, 14, 15 Although ultrasound, scintigraphy, CT, and MRI are viable imaging modalities, Milan et al. emphasised that arthrography is the most useful method, especially in countries where equipment availability tends to be limited.9
In 2008, Kamegaya et al. studied patients who underwent femoral varus osteotomy. They concluded that preoperative arthrography was the most effective modality for predicting osteotomy results.16 Devalia et al. emphasised that preoperative arthrography is a cheap and easily applicable method; they used arthrography in patients for whom valgus osteotomy was planned but the indications were unclear.12
In a study by Kotnis et al., interobserver and intraobserver agreement among three consultants regarding arthrography was assessed for 21 paediatric cases with developmental dysplasia of the hip (DDH) and 19 of LCPD. In 6 of the 19 LCPD cases, the treatment plan was changed after arthrography. Intraobserver agreement was high but interobserver agreement was moderate; the authors emphasised that arthrography is a useful method for facilitating decision-making in the treatment of developmental hip dysplasia and LCPD.15
Our results showed some similarities to those of Kotnis et al.,15 but we included more participants, and also grouped them by arthrography experience. Also, the same questionnaire was completed before and after viewing arthrography images to investigate the effect of viewing arthrography images on treatment decisions. A total of 208 responses to images of eight cases were examined, in addition to changes in treatment decisions post- versus pre-image viewing. However, the validity of the treatment options and surgical methods have not yet been determined. Changes in treatment decisions by our participants and their association with arthrography experience are detailed in Table 1.
Participant preferences regarding treatment options and surgical modality, post- versus pre-image viewing, changed by 14.42% and 14.58%, respectively; the change was not significant in either case (both p = 0.99). There was also no relationship between rate of decisional change and experience with arthrography.
The additional diagnostic tests requested by the participants are shown in Table 2. Before viewing the arthrography images, 55.3% of the participants requested additional diagnostic tests, which decreased to 13.9% after viewing the arthrography images (p < 0.001). These results suggest that arthrography can guide the choice of treatment method.
When the additional examination requests were evaluated (n = 115), MRI was found to be requested most frequently (31.3% of all requests). However, the number of MRI requests showed the most significant decrease after viewing arthrography images, from the pre-image viewing total of 36 to 22 (p < 0.001; Table 3).
Treatment preferences before and after arthrography image-viewing are detailed in Table 4 according to arthrography experience. Among all participants, the "follow-up" answer option decreased to 42.8% after viewing arthrography images, from, 45.7%, whereas the preference for the “surgery” increased from 49.5% to 53.4%. Thus, after viewing the arthrography images, the preference for a surgical treatment approach increased, albeit not significantly (p = 0.193).
Both before and after viewing the arthrography images, the preference for surgery was greater in the arthrography-experienced group versus the -inexperienced group. However, the preference for surgery increased by the same amount in both groups after viewing the images.
We observed a significant group difference in the preference for surgery in case 3 only. In this case, there was incongruence in the X-ray images and in the arthrography images for the abduction position; after viewing the images, the preference for surgery of the participants changed significantly (Fig. 4). There was a similar situation for case two, albeit that the change in preference for surgery was not significant. This highlighted a difference between observers in the decision for LCPD treatment; even for a small number of cases, there was no consensus in treatment decisions.
The most preferred method of surgery, both before and after viewing arthrography images, was varisation (Table 5). After viewing the images, there was an increase in preference for other surgical techniques, although this was not significant (i.e., valgisation, Salter osteotomy, and varisation + Salter osteotomy) (p = 0.408). Thus, viewing arthrography images can influence the preference regarding surgical modality.
The limitations of this study included an unequal number of participants in the two groups, and the small number of cases covered by the questionnaire; however, a long questionnaire can negatively affect participant compliance and thus data reliability. Nevertheless, the inclusion of cases in different stages of LCPD, and the fact that our participants included surgeons with at least 10 years of experience in paediatric orthopaedics, improves the power of our study.
Based on our results, arthrography is an important diagnostic modality for LCPD. We observed a significant decrease in the number of requests for additional diagnostic tests after viewing arthrography images. In addition, we observed changes in treatment choice post-image viewing, although the rate of change was not significant. Among all participants, the preference for surgery increased after viewing the arthrography images. However, there was no significant difference in preferences between the arthrography-experienced and -inexperienced groups.
Declaration of competing interest
No conflicts of interest are declared by the authors. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributor Information
Ismail Eralp Kacmaz, Email: kacmazeralp@gmail.com.
Ali Reisoglu, Email: drreisoglu@gmail.com.
Can Doruk Basa, Email: candorukb@hotmail.com.
Vadym Zhamilov, Email: vadpenim@hotmail.com.
Haluk Agus, Email: halukagus@gmail.com.
References
- 1.Kim H.K.W.H. 5 ed. Elsevier Saunders; Philadelphia: 2014. J.A. Legg-Calvé-Perthes Disease. Tachdjian's Pediatric Orthopedics; pp. 580–629. [Google Scholar]
- 2.Molloy M.K., MacMahon B. Incidence of Legg-Perthes disease (osteochondritis deformans) N Engl J Med. 1966;275(18):988–990. doi: 10.1056/NEJM196611032751804. [DOI] [PubMed] [Google Scholar]
- 3.Zilkens C., Miese F., Bittersohl B. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC), after slipped capital femoral epiphysis. Eur J Radiol. 2011;79(3):400–406. doi: 10.1016/j.ejrad.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 4.Holstein A., Zilkens C., Bittersohl B. Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) and morphologic MRI of cartilage in the long-term follow-up after Legg-Calve-Perthes disease (LCPD) J med imaging radiat oncolo. 2011;55(3):259–265. doi: 10.1111/j.1754-9485.2011.02262.x. [DOI] [PubMed] [Google Scholar]
- 5.Sutherland A.D., Savage J.P., Paterson D.C., Foster B.K. The nuclide bone-scan in the diagnosis and management of Perthes' disease. J bone joint surg Br. 1980;62(3):300–306. doi: 10.1302/0301-620X.62B3.7410461. [DOI] [PubMed] [Google Scholar]
- 6.Fasting O.J., Langeland N., Bjerkreim I., Hertzenberg L., Nakken K. Bone scintigraphy in early diagnosis of Perthes' disease. Acta Orthop Scand. 1978;49(2):169–174. doi: 10.3109/17453677809005746. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki S., Awaya G., Okada Y., Ikeda T., Tada H. Examination by ultrasound of Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1987;(220):130–136. [PubMed] [Google Scholar]
- 8.Catterall A. The natural history of Perthes' disease. J bone joint surg Br. 1971;53(1):37–53. [PubMed] [Google Scholar]
- 9.Milani C., Dobashi E.T. Arthrogram in legg-calve-perthes disease. J. Pediatr. Orthoped. 2011;31(2 Suppl):S156–S162. doi: 10.1097/BPO.0b013e318223b441. [DOI] [PubMed] [Google Scholar]
- 10.Kamegaya M., Moriya H., Tsuchiya K., Akita T., Ogata S., Someya M. Arthrography of early Perthes' disease. Swelling of the ligamentum teres as a cause of subluxation. J Bone Joint Surg. 1989;71(3):413–417. doi: 10.1302/0301-620X.71B3.2722932. [DOI] [PubMed] [Google Scholar]
- 11.Dimeglio A., Canavese F. Imaging in legg-calve-perthes disease. Orthop Clin N Am. 2011;42(3):297–302. doi: 10.1016/j.ocl.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Devalia K.L., Wright D., Sathyamurthy P., Prasad P., Bruce C. Role of preoperative arthrography in early Perthes disease as a decision-making tool. Is it really necessary? J. Pediatr. Orthoped.Part.B. 2007;16(3):196–200. doi: 10.1097/BPB.0b013e3280d9e8e1. [DOI] [PubMed] [Google Scholar]
- 13.Bennett J.T., Stuecker R., Smith E., Winder C., Rice J. Arthrographic findings in Legg-Calve-Perthes disease. J. Pediatr. Orthoped.Part.B. 2002;11(2):110–116. doi: 10.1097/00009957-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Ghanem I., Haddad E., Haidar R. Lateral shelf acetabuloplasty in the treatment of Legg-Calve-Perthes disease: improving mid-term outcome in severely deformed hips. J. Child. Orthop. 2010;4(1):13–20. doi: 10.1007/s11832-009-0216-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kotnis R., Spiteri V., Little C., Theologis T., Wainwright A., Benson M.K. Hip arthrography in the assessment of children with developmental dysplasia of the hip and Perthes' disease. J. Pediatr. Orthoped.Part.B. 2008;17(3):114–119. doi: 10.1097/BPB.0b013e3280103684. [DOI] [PubMed] [Google Scholar]
- 16.Kamegaya M., Saisu T., Takazawa M., Nakamura J. Arthrographic indicators for decision making about femoral varus osteotomy in Legg-Calve-Perthes disease. J. Child. Orthop. 2008;2(4):261–267. doi: 10.1007/s11832-008-0120-2. [DOI] [PMC free article] [PubMed] [Google Scholar]