Abstract
Purpose
Reverse shoulder arthroplasty (RSA) as an alternative to hemiarthroplasty (HA) as treatment for proximal humerus fractures has prompted a re-evaluation of utilization trends.
Methods
Operative treatment for proximal humeral fractures were analyzed using a New York State database.
Results
After introduction as an ICD-9 code, RSA increased to 39.3% (m = +5.2%/year, r = 0.984). When stratifying by age ≥65, HA decreased to 7.7% (m = −2.8%/year, r = 0.962) while RSA increased to 50.6% (m = +6.4%/year, r = 0.985).
Conclusion
RSA overtook HA as the arthroplasty procedure of choice for proximal humerus fractures. In patients ≥65, RSA passed ORIF as the most prevalent procedure in 2017.
Level of evidence
III, Descriptive Epidemiology Study, Large Database Analysis.
Keywords: Proximal humerus fractures, Reverse shoulder arthroplasty, Shoulder hemiarthroplasty, Elderly, Open reduction and internal fixation, Trauma
1. Introduction
Proximal humerus fractures account for approximately 4–6% of all fractures.1 In the elderly population, only hip fractures and distal radius fractures are more common.1,2 There is a growing incidence of these fractures, which is attributed to an increasingly elderly population and a higher prevalence of osteoporosis.2, 3, 4, 5 If current trends continue, the proximal humerus fracture rate will triple over the next three decades.6
Although the majority of proximal humerus fractures are treated non-operatively, options for surgical treatment include closed reduction-internal fixation (CRIF), open reduction-internal fixation (ORIF), hemiarthroplasty (HA), and reverse shoulder arthroplasty (RSA). HA has been considered the historical treatment of choice for arthroplasty in the elderly with poor bone quality and complex fracture patterns that are not suitable for internal fixation.7 Studies, however, have reported poor functional outcomes and no clear benefit towards quality of life with the use of HA compared to non-operative management.1,8, 9, 10, 11
Recent literature has demonstrated an increased utilization of RSA and a decreased utilization of HA, particularly in the elderly population.4,5,12,13 A recent systematic review suggests that RSA results in better clinical outcomes, improved range of motion, decreased re-operation rates, and equivocal infection rates compared to HA.14 The emergence of reverse shoulder arthroplasty as a more clinically reliable alternative to hemiarthroplasty has prompted a re-evaluation of utilization trends. The purpose of this study was to assess trends in the management of proximal humerus fractures during a 13-year period using a healthcare data reporting system. Our hypothesis was that RSA has become the procedure of choice for the management of complex proximal humerus fractures.
2. Materials and methods
2.1. Database
The New York Statewide Planning and Research Cooperative System (SPARCS) is a healthcare data reporting system established by the New York State Department of Health (https://www.health.ny.gov/statistics/sparcs/). The SPARCS database collects data annually on all admissions in New York State. Each patient record includes data on demographics and clinical course, including medical diagnoses and surgical procedures. Data aggregated prior to October 2015 use International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes for diagnoses and procedures while data aggregated after October 2015 use 10th Revision codes (ICD-10-CM). A unique identification code for each patient allows researchers to track a patient across multiple inpatient encounters. Since our version of the SPARCS database did not contain any protected health information, this study was determined to be exempt by our institutional review board.
2.2. Cases
We initially identified 46,719 inpatient admissions for proximal humerus fractures (ICD-9-CM: 812.0X and 812.1X, ICD-10-CM: S42.2XXX) between January 2005 and June 2017.
2.3. Covariates
We extracted demographic variables for each admission, including age (years), sex (male or female), race (white or nonwhite), insurance (government, private), and year of admission. Comorbidities were assessed using the Charlson/Deyo scoring method for ICD-9 coding. The 17 comorbidities with point value in parenthesis included: congestive heart failure (1), cerebrovascular disease (1), chronic pulmonary disease (1), dementia (1), peripheral vascular disease (1), rheumatologic disease (1), peptic ulcer disease (1), mild liver disease (1), past myocardial infarct (1), uncomplicated diabetes (1), hemiplegia or paraplegia (2), renal disease (2), malignancy including leukemia and lymphoma (2), diabetes with end organ damage (2), moderate or severe liver disease (3), metastatic solid tumor (6), and HIV infection (6). Patients with none of these comorbidities received a score of zero. The Charlson/Deyo score was then made into a categorical variable with score categories 0, 1 or 2 or more.
2.4. Outcomes
Operative management of proximal humerus fractures was considered if the patient had ICD-9 or ICD-10 procedural codes for open reduction internal fixation (ORIF: ICD-9: 79.31; ICD-10: 0PSC04Z, 0PSD04Z, 0PSF04Z, 0PSG04Z), closed reduction internal fixation (CRIF: 79.11; ICD-10: 0PSC43Z, 0PSC44Z, 0PSD43Z, 0PSD44Z, 0PSF44Z, 0PSG34Z), HA (ICD-9: 81.81; ICD-10: 0RRJ0J6, 0RRJ0J7, 0RRJ0JZ, 0RRK0JZ, 0RRK0J6, RRK0J7; or RSA (ICD-9: 81.88; ICD-10: 0RRJ00Z, 0RRK00Z).
Total utilization rates for ORIF, HA, RSA and CRIF were analyzed. Utilization rates were further compared with age subgroup analyses, dividing age into two categories - those older than or equal to 65, and those younger than 65.
2.5. Statistical analysis
Statistical analyses were descriptive to define the utilization rate of each procedure throughout the study period. We performed all statistical analyses using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Figures were generated using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA, USA). All rates were considered linear functions, with slope and coefficient of determination calculated using trendlines. All p-values were two-tailed, and p less than 0.05 was considered statistically significant.
3. Results
Between January 2005 and June 2017, there were 46,719 proximal humeral fracture admissions in New York State, with 31.9% treated operatively. The majority of operative patients were represented by: females, age greater than or equal to 65, whites, government insured, and no comorbidities. ORIF was the most prevalent procedure at 63.0%, followed by HA at 22.2%, RSA at 10.5% and CRIF at 4.3% (Table 1).
Table 1.
Demographics of study cohort.
| Characteristic |
Operative |
|---|---|
| Proximal Humeral Fractures, N | 14,889 (31.9%) |
| Age category, % | |
| ≤65 | 40.4 |
| ≥65 | 59.6 |
| Sex | |
| Male | 30.2 |
| Female | 69.8 |
| Race, % | |
| White | 83.0 |
| Non-White | 17.0 |
| Insurance, % | |
| Government | 54.1 |
| Private | 45.9 |
| Deyo Comorbidity Score, % | |
| 0 | 58.4 |
| 1 | 25.6 |
| 2+ | 16.0 |
| Treatment | |
| CRIF | 4.3 |
| ORIF | 63.0 |
| Hemi | 22.2 |
| RSA | 10.5 |
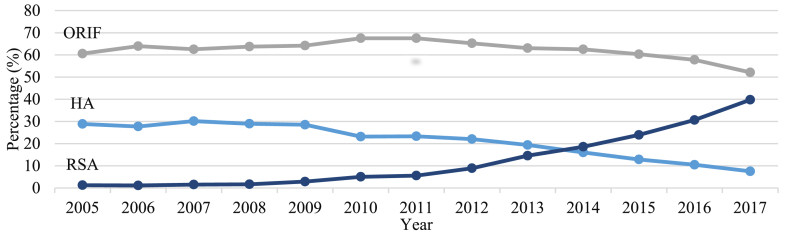
Over the course of the study duration, the annual utilization rate for ORIF did not significantly change (m = −0.5% per year, r = 0.514, p = 0.07), and ORIF remained the most prevalent procedure annually. Hemiarthroplasty utilization significantly decreased from 28.9% in 2005 to 7.5% in 2017 (m = −1.9% per year, r = 0.954, p < 0.001). After being introduced in 2010 as an ICD-9 code, RSA for operative fractures significantly increased from 1.7% in 2010 to 39.3% in 2017 (m = +5.2% per year, r = 0.984, p < 0.001). CRIF utilization decreased from 9.3% in 2005 to 0.5% in 2017 (m = −0.6% per year, r = 0.954, p < 0.001) (Fig. 1).
Fig. 1.
Trends in operative management of proximal humerus fractures, all ages. HA, hemiarthroplasty; ORIF, open reduction and internal fixation; RSA, reverse shoulder arthroplasty.
When stratifying by age less than 65, ORIF utilization did not significantly change (m = −0.1% per year, r = 0.14, p = 0.627) and remained the most prevalent procedure annually. However, HA significantly decreased from 16.0% in 2005 to 7.2% in 2017 (m = −0.6% per year, r = 0.852, p < 0.001) while RSA significantly increased from 0.2% in 2010 to 20.9% in 2017 (m = +2.6% per year, r = 0.829, p < 0.001). CRIF utilization decreased from 9.1% in 2005 to 1.0% in 2017 (m = −0.6% per year, r = 0.948, p < 0.001) (Fig. 2).
Fig. 2.
Trends in operative management of proximal humerus fractures, age <65. HA, hemiarthroplasty; ORIF, open reduction and internal fixation; RSA, reverse shoulder arthroplasty.
When stratifying by age 65 years and older, ORIF utilization was on the borderline of a statistical significant decrease (m = −0.1% per year, r = 0.14, p = 0.627), and no longer remained the most prevalent procedure in 2017. RSA significantly increased from 2.8% in 2010 to 50.6% in 2017 (m = +6.4% per year, r = 0.985, p < 0.001), becoming the most prevalent procedure in 2017. HA significantly decreased from 38.0% in 2005 to 7.7% in 2017 (m = −2.8% per year, r = 0.962, p < 0.001). CRIF utilization decreased from 9.4% in 2005 to 0.3% in 2017 (m = −0.6% per year, r = 0.924, p < 0.001) (Fig. 3).
Fig. 3.
Trends in operative management of proximal humerus fractures, age ≥65. HA, hemiarthroplasty; ORIF, open reduction and internal fixation; RSA, reverse shoulder arthroplasty.
4. Discussion
Although the majority of proximal humerus fractures are treated non-operatively, there is a role for operative management depending on the complexity of these fractures and certain patient characteristics. The introduction of RSA as a surgical option has evolved over the past decade. Our study aimed to better understand the trends in the management of proximal humerus fractures over the past 13 years in New York State.
RSA has gained popularity over the past decade amongst surgeons for the treatment of proximal humerus fractures when arthroplasty is indicated.15,16 Studies have shown that the use of RSA for these complex fractures is increasing, while the rate of HA is decreasing.4,5,12,13 Our results are consistent with these previous trends and have further shown that the rate of RSA surpassed HA in all comers, with an even more drastic change in the elderly population. To our knowledge, this finding has not been demonstrated before.
Our results may be explained by increased surgeon confidence in the reliability of RSA as newer generations of the implant have been developed as well as increased competence and comfort with RSA as the procedure has become more prevalent in training settings.17, 18, 19, 20, 21, 22 In contrast, inconsistent results and poor functional outcomes have been reported with HA,8, 9, 10, 11 as well as long-term complications.23 A randomized control study showed that RSA was superior to HA in that it resulted in less pain, improved function, and had lower revision rates in the elderly.21 Due to an aggregate of studies suggesting RSA as a surgical option over HA for complex proximal humerus fractures in the elderly,14 it is not surprising that RSA has overtaken HA as the gold standard treatment when arthroplasty is indicated.
When stratifying for ages 65 year and older, there was a borderline decrease in the use of ORIF and it was no longer the most prevalent in 2017, being surpassed by RSA. These results contradict a previously reported increase in the use of ORIF in the elderly due to the introduction of locking plate technology,2 which is probably attributed to the relatively recent introduction of RSA and the increasing confidence in its use amongst surgeons. The consistently increased prevalence of ORIF in patients younger than 65 years old is likely explained by better bone quality more amendable to this treatment. Lastly, it was noted that the use of CRIF decreased to near non-existent levels which is consistent with previously reported trends.4
The major strength of this study was that the healthcare database identified many patients of variable demographic factors over a near 13-year period, which includes the introduction of RSA as an ICD-9 code in 2010. This allowed for an accurate analysis of the utilization trends in the management of proximal humerus fractures in New York State. The major limitation of this study is that retrospective bias may exist, and the data collected relies on proper coding practices. Furthermore, the data is one year old due to reporting lag. Additionally, the results of this study are limited to a specific geographic region, and one can question the generalizability to a national or international level. Further areas of interest include stratifying the trends in management of proximal humerus fracture based on fellowship training, as well as the collection of outcomes relative to the procedure performed.
5. Conclusion
RSA has overtaken HA as the arthroplasty procedure of choice for complex proximal humerus fractures in New York State. Moreover, in patients 65 years and older in, RSA passed ORIF as the most prevalent procedure in 2017. Future database analysis should be performed to determine if these trends continue.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Court-Brown C.M., Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Bell J.E., Leung B.C., Spratt K.F. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Jt Surg Am. 2011;93(2):121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kannus P., Palvanen M., Niemi S., Parkkari J., Jarvinen M., Vuori I. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970-1998 and alarming projections for the new millennium. Acta Orthop Scand. 2000;71(5):465–470. doi: 10.1080/000164700317381144. [DOI] [PubMed] [Google Scholar]
- 4.Khatib O., Onyekwelu I., Zuckerman J.D. The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. J Shoulder Elbow Surg. 2014;23(9):1356–1362. doi: 10.1016/j.jse.2013.12.034. [DOI] [PubMed] [Google Scholar]
- 5.Rosas S., Law T.Y., Kurowicki J., Formaini N., Kalandiak S.P., Levy J.C. Trends in surgical management of proximal humeral fractures in the Medicare population: a nationwide study of records from 2009 to 2012. J Shoulder Elbow Surg. 2016;25(4):608–613. doi: 10.1016/j.jse.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Palvanen M., Kannus P., Niemi S., Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 7.Robinson C.M., Page R.S., Hill R.M., Sanders D.L., Court-Brown C.M., Wakefield A.E. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Jt Surg Am. 2003;85-a(7):1215–1223. doi: 10.2106/00004623-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Boons H.W., Goosen J.H., van Grinsven S., van Susante J.L., van Loon C.J. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop Relat Res. 2012;470(12):3483–3491. doi: 10.1007/s11999-012-2531-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gronhagen C.M., Abbaszadegan H., Revay S.A., Adolphson P.Y. Medium-term results after primary hemiarthroplasty for comminute proximal humerus fractures: a study of 46 patients followed up for an average of 4.4 years. J Shoulder Elbow Surg. 2007;16(6):766–773. doi: 10.1016/j.jse.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 10.Olerud P., Ahrengart L., Ponzer S., Saving J., Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20(7):1025–1033. doi: 10.1016/j.jse.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 11.Park Y.K., Kim S.H., Oh J.H. Intermediate-term outcome of hemiarthroplasty for comminuted proximal humerus fractures. J Shoulder Elbow Surg. 2017;26(1):85–91. doi: 10.1016/j.jse.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Acevedo D.C., Mann T., Abboud J.A., Getz C., Baumhauer J.F., Voloshin I. Reverse total shoulder arthroplasty for the treatment of proximal humeral fractures: patterns of use among newly trained orthopedic surgeons. J Shoulder Elbow Surg. 2014;23(9):1363–1367. doi: 10.1016/j.jse.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Sabesan V.J., Lombardo D., Petersen-Fitts G., Weisman M., Ramthun K., Whaley J. National trends in proximal humerus fracture treatment patterns. Aging Clin Exp Res. 2017;29(6):1277–1283. doi: 10.1007/s40520-016-0695-2. [DOI] [PubMed] [Google Scholar]
- 14.Austin D.C., Torchia M.T., Cozzolino N.H., Jacobowitz L.E., Bell J.E. Decreased reoperations and improved outcomes with reverse total shoulder arthroplasty in comparison to hemiarthroplasty for geriatric proximal humerus fractures: a systematic review and meta-analysis. J Orthop Trauma. 2019;33(1):49–57. doi: 10.1097/BOT.0000000000001321. [DOI] [PubMed] [Google Scholar]
- 15.Acevedo D.C., Vanbeek C., Lazarus M.D., Williams G.R., Abboud J.A. Reverse shoulder arthroplasty for proximal humeral fractures: update on indications, technique, and results. J Shoulder Elbow Surg. 2014;23(2):279–289. doi: 10.1016/j.jse.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Cvetanovich G.L., Frank R.M., Chalmers P.N., Verma N.N., Nicholson G.P., Romeo A.A. Surgical management of proximal humeral fractures: the emerging role of reverse total shoulder arthroplasty. Orthopedics. 2016;39(3):e465–e473. doi: 10.3928/01477447-20160324-02. [DOI] [PubMed] [Google Scholar]
- 17.Baudi P., Campochiaro G., Serafini F. Hemiarthroplasty versus reverse shoulder arthroplasty: comparative study of functional and radiological outcomes in the treatment of acute proximal humerus fracture. Musculoskelet Surg. 2014;98(Suppl 1):19–25. doi: 10.1007/s12306-014-0322-3. [DOI] [PubMed] [Google Scholar]
- 18.Bonnevialle N., Tournier C., Clavert P., Ohl X., Sirveaux F., Saragaglia D. Hemiarthroplasty versus reverse shoulder arthroplasty in 4-part displaced fractures of the proximal humerus: multicenter retrospective study. Orthop Traumatol Surg Res. 2016;102(5):569–573. doi: 10.1016/j.otsr.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 19.Cuff D.J., Pupello D.R. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Jt Surg Am. 2013;95(22):2050–2055. doi: 10.2106/JBJS.L.01637. [DOI] [PubMed] [Google Scholar]
- 20.Gallinet D., Ohl X., Decroocq L., Dib C., Valenti P., Boileau P. Is reverse total shoulder arthroplasty more effective than hemiarthroplasty for treating displaced proximal humerus fractures in older adults? A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2018;104(6):759–766. doi: 10.1016/j.otsr.2018.04.025. [DOI] [PubMed] [Google Scholar]
- 21.Sebastia-Forcada E., Cebrian-Gomez R., Lizaur-Utrilla A., Gil-Guillen V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23(10):1419–1426. doi: 10.1016/j.jse.2014.06.035. [DOI] [PubMed] [Google Scholar]
- 22.van der Merwe M., Boyle M.J., Frampton C.M.A., Ball C.M. Reverse shoulder arthroplasty compared with hemiarthroplasty in the treatment of acute proximal humeral fractures. J Shoulder Elbow Surg. 2017;26(9):1539–1545. doi: 10.1016/j.jse.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Noyes M.P., Kleinhenz B., Markert R.J., Crosby L.A. Functional and radiographic long-term outcomes of hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2011;20(3):372–377. doi: 10.1016/j.jse.2010.06.009. [DOI] [PubMed] [Google Scholar]