Summary
The Middle East Respiratory Coronavirus (MERS-CoV) was first isolated from a patient who died with severe pneumonia in June 2012. As of 19 June 2015, a total of 1,338 MERS-CoV infections have been notified to the World Health Organization (WHO). Clinical illness associated with MERS-CoV ranges from mild upper respiratory symptoms to rapidly progressive pneumonia and multi-organ failure. A significant proportion of patients present with non-respiratory symptoms such as headache, myalgia, vomiting and diarrhoea. A few potential therapeutic agents have been identified but none have been conclusively shown to be clinically effective. Human to human transmission is well documented, but the epidemic potential of MERS-CoV remains limited at present. Healthcare-associated clusters of MERS-CoV have been responsible for the majority of reported cases. The largest outbreaks have been driven by delayed diagnosis, overcrowding and poor infection control practices. However, chains of MERS-CoV transmission can be readily interrupted with implementation of appropriate control measures. As with any emerging infectious disease, guidelines for MERS-CoV case identification and surveillance evolved as new data became available. Sound clinical judgment is required to identify unusual presentations and trigger appropriate control precautions.
Evidence from multiple sources implicates dromedary camels as natural hosts of MERS-CoV. Camel to human transmission has been demonstrated, but the exact mechanism of infection remains uncertain. The ubiquitously available social media have facilitated communication and networking amongst healthcare professionals and eventually proved to be important channels for presenting the public with factual material, timely updates and relevant advice.
Introduction
The Middle East Respiratory Syndrome Coronavirus (MERS-CoV) was first identified in September 2012. As of 19 June 2015, a total of 1,338 MERS-CoV infections have been reported to the World Health Organization (WHO).1 Despite an accumulation of clinical experience and scientific knowledge, new MERS-CoV infections continue to be reported almost on daily basis. What lessons can we learn after three years of clinical experience and scientific research?
Lesson one: no substitute for continuous vigilance
A 60-year-old man was admitted on June 13th, 2012, to a hospital in Jeddah, Saudi Arabia, with severe pneumonia and multi-organ failure. The patient died after 11 days of hospitalization.2 Indirect immunofluorescence assays and real-time polymerase chain reaction (PCR) for widely occurring respiratory viruses failed to identify an infective aetiology. Interestingly, cytopathic changes consistent with viral replication were noted in LLC-MK2 and Vero cell cultures of the patient’s respiratory samples. Slides of the infected cell cultures reacted strongly with the patient’s serum but not with any of 2400 control sera stored in the same hospital. However, pan-coronavirus PCR yielded positive results. The PCR fragments were sequenced at the Erasmus Medical Centre in Rotterdam, The Netherlands, and phylogenetic analysis showed that the novel coronavirus belonged to lineage C of the genus betacoronavirus.2, 3 On 20 September 2012, an email was posted on Program for Monitoring Emerging Diseases Mail (ProMED-mail) announcing the discovery of a novel human coronavirus.4
Meanwhile, a critically ill 49-year-old Qatari man was transferred by air ambulance on September 11th, 2012, to a hospital in England.5 He had developed respiratory symptoms on September 3rd followed by multi-organ failure. His upper and lower respiratory tract samples were negative for influenza A/B, parainfluenza 1–4, RSV A/B, human metapneumovirus, enterovirus, rhinovirus, adenovirus, human bocavirus, and the human coronaviruses (NL63, 229E, OC43, HKU1). On September 21st, 2012, one day after the above ProMED-mail posting, the patient’s respiratory samples tested positive by pan-coronavirus PCR. Once sequenced, a 250 base-pair fragment from this isolate showed 99.5% homology with the Erasmus Medical Centre’s isolate.5 The third patient was a 45-year-old man who presented to a hospital in Riyadh, Saudi Arabia, on October 10th, 2012, with severe pneumonia and renal failure. MERS-CoV was detected in samples from the patient's upper and lower respiratory tract.6
Prior to all of this, an outbreak of respiratory illness was reported in April 2012 from an intensive care unit in a hospital in Zarqa, Jordan.7 A retrospective epidemiological investigation in November 2012 identified 13 probable cases, two of whom had died. MERS-CoV was detected by reverse transcription (RT)–PCR in stored samples from the two deceased patients.8 Seven more were subsequently confirmed by serological testing.9
A pattern began to emerge, characterized by severe pneumonia, multi-organ failure, and an epidemiological link to a country in the Middle East. In May 2013, the virus, which had been initially known as human coronavirus–Erasmus Medical Centre (hCoV-EMC), was named the Middle East respiratory syndrome coronavirus (MERS-CoV).10
Notably, phylogenetic analysis of the first five available MERS-CoV sequences suggested a common ancestor dating back to mid-2011.11 Furthermore, anti-MERS-CoV antibodies were detected in 15 out of 10,009 serum samples [0.15%; 95% confidence interval (CI): 0.09–0.24%] obtained between December 2012 and December 2013 from 13 provinces in Saudi Arabia.12 The authors extrapolated that just fewer than 45,000 individuals (44,951; 95% CI: 26,971–71,922) in Saudi Arabia could be seropositive for MERS-CoV.12 It is therefore reasonable to assume that human MERS-CoV infections had taken place in the region for some considerable time before it was identified. It is possible that the identification of the virus might have been delayed even more, had it not been for the meticulous investigation by a single virologist, Dr A.M. Zaki, of the first reported case of MERS-CoV.2 The first lesson one has to learn from MERS-CoV and its discovery is that continuous vigilance and perseverance with diagnostic investigation of undiagnosed infectious diseases are essential to identify emerging pathogens.
Lesson two: yet again, prevention is better than cure
Clinically, MERS-CoV infection may range from an asymptomatic or mild upper respiratory illness to a rapidly progressive and fatal disease.13, 14, 15 The majority of hospitalized patients with MERS-CoV infection present with fever and respiratory symptoms including cough and shortness of breath with clinical and radiological evidence of pneumonia.16, 17 Fatigue, myalgia, headache, and gastrointestinal symptoms such as vomiting and diarrhoea are also frequent.16, 17 Respiratory and renal failure are frequent complications of severe MERS-CoV infection, in addition to acute liver injury, cardiac dysrhythmias, and coagulopathy.16, 17, 18, 19, 20 Overall mortality is around 35.6%, but exceeds 70% in critically ill patients and in those with significant comorbidities.1, 18, 19, 20, 21, 22 For reasons yet to be understood, MERS-CoV infection is rare in children.23, 24
In-vitro studies have identified numerous agents with anti-MERS-CoV activity including interferon, ribavirin, mycophenolate, cyclosporine and lopinavir.25 The combination of interferon and ribavirin showed promising results in experimentally infected macaques.26 However, in retrospective clinical studies the combination was not associated with significantly improved overall survival.21, 22 Treatment of patients with MERS-CoV infections remains largely dependent on supportive measures.27
Diagnosis is confirmed by detection of MERS-CoV RNA in respiratory samples by real-time PCR targeting the upE and ORF 1b genes.28 Samples obtained from the lower respiratory tract have higher viral loads and better diagnostic yield than those obtained from the throat or nasopharynx.11, 29, 30 Moreover, viral shedding is considerably prolonged in symptomatic and severely ill MERS-CoV patients compared with asymptomatic infected contacts.31 Interestingly, detection of MERS-CoV in blood has been associated with worse clinical outcome.22, 32 MERS-CoV may also be detected in stool for up 16 days and in urine for up to 13 days from disease onset.11 Under certain conditions, MERS-CoV can survive on plastic and steel surfaces for up to 30 h.33 In the absence of appropriate precautions, the environment surrounding a symptomatic MERS-CoV patient can therefore become extensively contaminated with viable, potentially infectious virus.
Human-to-human transmission of MERS-CoV has been well documented in family clusters, community settings and more often in healthcare settings.13, 14, 15, 17, 20, 34 Common denominators in the largest hospital outbreaks have been overcrowding, especially in emergency departments, and poor adherence to infection control standards.15, 17, 35, 36 However, MERS-CoV continues to have relatively limited infectiousness. For example, screening identified secondary MERS-CoV infections in only 4% of 280 close family contacts and 2% of 5065 healthcare contacts.37, 38 Moreover, no secondary cases were identified following extensive epidemiological investigations of imported cases in the UK, Germany, France, Greece, The Netherlands, and the USA.39, 40, 41, 42, 43, 44, 45, 46
It has been phylogenetically demonstrated that MERS-CoV transmission chains have not extended beyond two to three months and that the virus has remained genetically stable over the past three years.47, 48 Given an effective reproduction number (R0) of less than one, human-to-human MERS-CoV could be readily interrupted with effective preventive interventions.49, 50 Indeed, even the most explosive hospital outbreaks of MERS-CoV infection, such those that occurred in Jeddah and Riyadh in April to May 2014, were brought under control through a strategy based on early case detection and implementation of appropriate infection prevention and control measures; namely contact and droplet precautions for general care in addition to airborne precautions for aerosol-generating procedures such as intubation and respiratory tract suctioning.51, 52, 53
The poor prognosis associated with MERS-CoV, especially in patients with multiple comorbidities, and the lack of effective anti-viral therapy make appropriate infection prevention and control all-important. Just as is true for most infectious diseases, MERS-CoV reminds us again that prevention is better than cure.
Lesson three: guidelines should not prevail over sound clinical judgement
The initial case definitions for MERS-CoV case finding and reporting focused on patients who are hospitalized, had evidence of acute pulmonary disease with an epidemiological link to confirmed cases or to countries in the Middle East.54, 55 As more clinical experience and epidemiological data became available, updated definitions removed the requirement for hospitalization.56 The reporting of several community and hospital clusters during the first half of the year 2013, often without identifiable human or animal sources, led to speculation that individuals with no or only mild respiratory symptoms might have a role in MERS-CoV transmissions.13, 14, 20 This was reflected in the WHO revised interim definition published in July 2013 where patients with acute febrile illness of any severity were included; in addition to a recommendation to proactively test asymptomatic close contacts of confirmed MERS-CoV infections.57 Memish et al. later showed that MERS-CoV was detectable for up to 12 days in 30% of 12 asymptomatic contacts.31 In another report, an asymptomatic healthcare worker had detectable MERS-CoV for more than five weeks.58 Although MERS-CoV transmission from an asymptomatic individual remains a strong probability, this has never been documented.37, 38
In the meantime, clinicians were becoming increasingly aware that MERS-CoV infections were being diagnosed in patients whose clinical presentations did not conform to those definitions, including the absence of fever, lack of respiratory involvement and the predominance of gastrointestinal or non-specific generalized symptoms.17, 22, 59 In the aftermath of the surge of MERS-CoV infection in Jeddah and Riyadh in April and May 2014, the Ministry of Health in Saudi Arabia revised its case definition and surveillance guidance to recommend MERS-CoV testing in any of four patient categories:
-
–
patients with clinical or radiological evidence of community-acquired pneumonia;
-
–
patients with clinical or radiological evidence of healthcare-associated pneumonia;
-
–
patients with acute febrile illness and myalgia, headache, diarrhoea, nausea, or vomiting, and unexplained leucopenia or thrombocytopenia;
-
–
contacts of individuals with confirmed or probable MERS-CoV infection who develop upper or lower respiratory symptoms within two weeks of exposure.60
As better understanding of the epidemiology of MERS-CoV developed, it became obvious that a considerable proportion of cases were probably missed.12, 50 During the steep learning curve of an emerging infectious disease, regularly updated guidelines are important. Such guidelines are inevitably based on incomplete evidence and hence may not be comprehensive or applicable in all situations. Clinical acumen and heightened medical awareness are essential for early detection of unusual MERS-CoV cases and to prevent delays in diagnosis and to mitigate additional exposures.61
Lesson four: MERS-CoV is another zoonotic infection
A zoonotic origin was suspected soon after the identification of MERS-CoV.6 Bats are known natural hosts for several coronaviruses and hence were the initial target for investigation.62, 63 More than 1000 faecal samples were collected from wild bats in the area around where the first MERS-CoV patient lived. A 190-nucleotide fragment of MERS-CoV RNA was detected in one faecal pellet from an Egyptian tomb bat. The sequenced amplification product was genetically identical to the MERS-CoV sequence obtained from the index human case.64 More recently, a closely related coronavirus was isolated from bats in South Africa, suggesting that MERS-CoV ancestors might exist in Old World bats.65, 66 To date, no further evidence is available to confirm the role of bats as natural hosts or reservoirs for MERS-CoV.
On the other hand, the evidence implicating dromedary camels in MERS-CoV epidemiology is more consistent. A role for dromedary camels is supported by the following observations:
-
−
Neutralizing MERS-CoV antibodies are highly prevalent in dromedary camels from across the Arabian Peninsula, North Africa, and Eastern Africa.67, 68, 69, 70, 71, 72, 73 MERS-CoV antibodies were detected in stored camel sera dating as far back as the early 1990s.73, 74, 75 The prevalence of MERS-CoV seropositivity is significantly higher in camels aged more than two years than in juvenile camels.68, 74, 76
-
−
Several groups have reported the detection of MERS-CoV by RT–PCR in nasal and faecal samples from dromedary camels in the Arabian Peninsula.72, 74, 76, 77, 78, 79 One study reported MERS-CoV positivity in more than 60% of lung tissue samples obtained from dromedary camel carcasses.79 RT–PCR was positive in camels that had prior evidence of MERS-CoV seropositivity, indicating that animal reinfection is possible.76 Interestingly, the prevalence of MERS-CoV RNA is significantly higher in juvenile than in adult camels.74, 76, 79 Furthermore, all MERS-CoV strains obtained from dromedary camels are phylogenetically clustered within human isolates, supporting possible animal–human intertransmission.72, 76, 77, 78, 79, 80, 81
-
−
Viable MERS-CoV was isolated from nasal and faecal samples from dromedary camels.76, 82 MERS-CoV recovered from dromedary camels is capable of causing ex-vivo infection in human respiratory cells.83
-
−
Acute infection in dromedary camels has been demonstrated by documented rises in anti-MERS-CoV antibody titres, and by RT–PCR in symptomatic animals.76, 81, 82
-
−
Experimental MERS-CoV infection of dromedary camels resulted in clinical infection manifesting as fever and rhinorrhoea.84 Viable MERS-CoV was recovered in cultures of nasal samples for up to seven days post-inoculation; a period during which infectiousness is theoretically possible. MERS-CoV seroconversion was documented within 14 days of inoculation.84
-
−
Almost identical MERS-CoV strains were recovered from epidemiologically linked human cases and camels with which they had close contact in Qatar, and in Saudi Arabia.80, 81, 85
It is important to note, however, that MERS-CoV seroprevalence studies in individuals with close contact with camels have yielded inconsistent results. A national serosurvey in Saudi Arabia found prevalence of MERS-CoV antibodies that was 15 times higher in camel shepherds (P = 0.0004) and 23 times higher in slaughterhouse workers (P < 0.0001), compared with the general population.12 Similarly, MERS-CoV serology was positive in individuals who had occupational exposure to dromedary camels in Qatar but not in those without such exposure.86 On the other hand, MERS-CoV antibodies were not detected in sera obtained from individuals who had close contact with camels that had documented MERS-CoV infection two to three months earlier.87 Likewise, screened slaughterhouse workers and other animal workers in Western and Southern Saudi Arabia were all seronegative for MERS-CoV antibodies.88, 89
Collectively, the available data strongly suggest that MERS-CoV is highly prevalent in dromedary camels in the Arabian Peninsula and that transmission of infection from camels to humans, although inefficient, does occur. However, the exact mechanism and route of infection it is still unclear. Even less clear is the role of bats as possible natural reservoirs for MERS-CoV. Moreover, only a small proportion of patients with confirmed MERS-CoV infection report close contact with camels.17 Even though camels are probably important in the transmission cycle of sporadic MERS-CoV infection, human-to-human transmission remains the likely source of the majority of reported MERS-CoV infections.
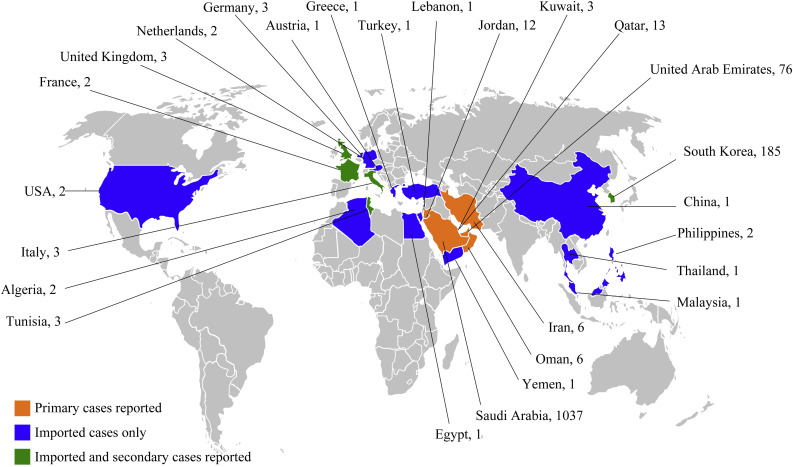
Lesson five: the world is getting smaller
MERS-CoV infections have been reported from a total of 26 countries around the world (Figure 1 ). Cases outside the Middle East include individuals who travelled to Europe or the Far East for medical care, expatriates returning home from countries in the Middle East or short-term visitors to the region.5, 11, 30, 35, 44, 90, 91, 92, 93, 94, 95, 96 On some occasions, travel-related MERS-CoV infections resulted in small clusters of secondary infections.30, 94, 95, 97 One pertinent cause for concern has been the potential global spread of MERS-CoV during the annual Hajj pilgrimage when millions of Muslims from around the world gather in Mecca, Saudi Arabia.98, 99, 100, 101, 102 Though those concerns are well founded, several surveillance studies over the past three years have not identified any MERS-CoV infections among Hajj pilgrims while they are in Saudi Arabia or after their return to their home countries.103, 104, 105, 106, 107, 108
Figure 1.
Countries and numbers of Middle East respiratory syndrome coronavirus (MERS-CoV) cases reported as of July 7th, 2015.
The situation was entirely different in the recent outbreak in South Korea where a single imported case resulted in a total of 186 laboratory-confirmed cases of MERS-CoV infection, including 36 deaths.109 The index patient was a 68-year-old man who developed respiratory symptoms seven days after returning to Seoul from a two-week visit to Bahrain, Saudi Arabia, United Arab Emirates, and Qatar.35 He sought medical care in several hospitals before he was diagnosed with MERS-CoV infection.35, 110 A combination of late recognition, overcrowding in emergency departments and hospital wards, multiple incidents of patient movement between different healthcare facilities, and delayed implementation of adequate infection control precautions culminated in the largest single outbreak of MERS-CoV infection.35, 36, 110, 111, 112 The outbreak involved patients, visitors, care-givers and healthcare workers, and spanned across six different hospitals in three South Korean cities.110, 113 Notably, phylogenetic analysis of MERS-CoV strains from South Korea revealed no significant biological changes compared to previously sequenced viruses.114
The outbreak in South Korea was eventually controlled through a series of measures including aggressive contact identification, screening and strict isolation, and rigorous infection control precautions.111, 115, 116 Within a few weeks, South Korea went from a country with no reported MERS-CoV cases to one that has the second largest number in the world.116, 117
With air travel becoming readily accessible and affordable, the South Korean experience demonstrates vividly that in the context of an infectious respiratory illness, there is simply no room for complacency. Adequate assessment of patients presenting with febrile illness must include their recent travel history to enable early application of proper control measures and to expedite laboratory confirmation and appropriate clinical management.
Lesson six: we live in the era of social media
The past decade has witnessed an exponential rise in internet-based social media sites such as Facebook, Twitter, and YouTube.118 Healthcare professionals are increasingly using social media applications to follow medical developments and emerging scientific literature and to share their own research findings, observations, and opinion.119 The general public often uses these tools as news outlets to seek and share medical and scientific information.120 However, in the context of MERS-CoV, social media have been a double-edged sword. For example, social media were at some point rife with inaccurate information that included rumours of hospitals closed due to MERS-CoV outbreaks and certain social events being nodes for MERS-CoV transmission. The authors are aware of examples of information and photos shared on social media resulting in patients losing their right to privacy and confidentiality. Patients often cancelled their clinic appointments or scheduled surgical procedures for fear of acquiring MERS-CoV while in hospital. Some avoided attending emergency departments despite having acute problems that required medical attention. Some individuals posted videos and messages challenging the suggestion that camels may be a source of MERS-CoV infection. Scepticism and mistrust in governmental agencies and the medical community were sometimes promoted and propagated.
On the other hand, various government agencies, scientific organizations and healthcare professionals used social media to enhance networking and facilitate communication of epidemiological, medical and scientific developments; in addition to presenting the public with factual material, timely updates, and relevant advice.121 The Saudi Ministry of Health, for example, posts daily updates on its website and through social media outlining details of current MERS-CoV cases. The Korean Ministry of Health and Welfare did the same during their MERS-CoV outbreak. Such steps are important to gain the public’s trust and to remove barriers to appropriate sources of information. Taking on board the surging role of social media and using them effectively to disseminate appropriate information turns them into invaluable tools for controlling an emerging infectious disease such as MERS-CoV.
Conclusion
MERS-CoV is an emerging infectious disease of probable animal origin. Sustained human-to-human infection has not occurred and its potential for causing widespread epidemic remains limited. Vigilance, early recognition, and institution of appropriate protective measures are the most effective control measures.
Conflict of interest
None declared.
Funding sources
None.
References
- 1.World Health Organization . WHO; Geneva: 2015. Middle East respiratory syndrome coronavirus (MERS-CoV); Summary of current situation, literature update and risk assessment 7 July 2015.http://apps.who.int/iris/bitstream/10665/179184/2/WHO_MERS_RA_15.1_eng.pdf?ua=1 Available at: [last accessed August 2015] [Google Scholar]
- 2.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D.M.E., Fouchier R.A.M. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Eng J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 3.van Boheemen S., de Graaf M., Lauber C. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio. 2012;3:e00473–00412. doi: 10.1128/mBio.00473-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ProMED-mail . International Society for Infectious Diseases; Washington DC: 2012. Novel coronavirus – Saudi Arabia: human isolate. Archive Number: 20120920.1302733; 20 September 2012 21:51:30 CEST.http://www.promedmail.org/direct.php?id=20120920.1302733 Available at: [last accessed August 2015] [Google Scholar]
- 5.Bermingham A., Chand M.A., Brown C.S. Severe respiratory illness caused by a novel coronavirus, in a patient transferred to the United Kingdom from the Middle East, September 2012. Euro Surveill. 2012;17:20290. [PubMed] [Google Scholar]
- 6.Albarrak A.M., Stephens G.M., Hewson R., Memish Z.A. Recovery from severe novel coronavirus infection. Saudi Med J. 2012;33:1265–1269. [PubMed] [Google Scholar]
- 7.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2012. Communicable Disease Threats Report, Week 18, 29 April–5 May 2012. Severe respiratory disease of unknown origin – Jordan – outbreak in ICU.http://www.ecdc.europa.eu/en/publications/Publications/CDTR.pdf Available at: online version 4 May 2012 [last accessed August 2015] [Google Scholar]
- 8.Hijawi B., Abdallat M., Sayaydeh A. Novel coronavirus infections in Jordan, April 2012. East Mediterr Health J. 2013;19:S12–18. [PubMed] [Google Scholar]
- 9.Al-Abdallat M.M., Payne D.C., Alqasrawi S. Hospital-associated outbreak of Middle East respiratory syndrome coronavirus: a serologic, epidemiologic, and clinical description. Clin Infect Dis. 2014;59:1225–1233. doi: 10.1093/cid/ciu359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Groot R.J., Baker S.C., Baric R.S. Middle East respiratory syndrome coronavirus (MERS-CoV): announcement of the Coronavirus Study Group. J Virol. 2013;87:7790–7792. doi: 10.1128/JVI.01244-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drosten C., Seilmaier M., Corman V.M. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2013;13:745–751. doi: 10.1016/S1473-3099(13)70154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muller M.A., Meyer B., Corman V.M. Presence of Middle East respiratory syndrome coronavirus antibodies in Saudi Arabia: a nationwide, cross-sectional, serological study. Lancet Infect Dis. 2015;15:559–564. doi: 10.1016/S1473-3099(15)70090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Memish Z.A., Zumla A.I., Al-Hakeem R.F., Al-Rabeeah A.A., Stephens G.M. Family cluster of Middle East respiratory syndrome coronavirus infections. N Eng J Med. 2013;368:2487–2494. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 14.Omrani A.S., Matin M.A., Haddad Q., Al-Nakhli D., Memish Z.A., Albarrak A.M. A family cluster of Middle East respiratory syndrome coronavirus infections related to a likely unrecognised asymptomatic or mild case. Int J Infect Dis. 2013;17:e668–672. doi: 10.1016/j.ijid.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oboho I.K., Tomczyk S.M., Al-Asmari A.M. 2014 MERS-CoV outbreak in Jeddah – a link to health care facilities. N Engl J Med. 2015;372:846–854. doi: 10.1056/NEJMoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assiri A., Al-Tawfiq J.A., Al-Rabeeah A.A. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13:752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saad M., Omrani A.S., Baig K. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–306. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Hameed F., Wahla A.S., Siddiqui S. Characteristics and outcomes of Middle East respiratory syndrome coronavirus patients admitted to an intensive care unit in Jeddah, Saudi Arabia. J Intensive Care Med. 2015 doi: 10.1177/0885066615579858. [DOI] [PubMed] [Google Scholar]
- 19.Arabi Y.M., Arifi A.A., Balkhy H.H. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Int Med. 2014;160:389–397. doi: 10.7326/M13-2486. [DOI] [PubMed] [Google Scholar]
- 20.Assiri A., McGeer A., Perl T.M. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Eng J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Omrani A.S., Saad M.M., Baig K. Ribavirin and interferon alfa-2a for severe Middle East respiratory syndrome coronavirus infection: a retrospective cohort study. Lancet Infect Dis. 2014;14:1090–1095. doi: 10.1016/S1473-3099(14)70920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shalhoub S., Farahat F., Al-Jiffri A. IFN-alpha2a or IFN-beta1a in combination with ribavirin to treat Middle East respiratory syndrome coronavirus pneumonia: a retrospective study. J Antimicrob Chemother. 2015;70:2129–2132. doi: 10.1093/jac/dkv085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khuri-Bulos N., Payne D.C., Lu X. Middle East respiratory syndrome coronavirus not detected in children hospitalised with acute respiratory illness in Amman, Jordan, March 2010 to September 2012. Clin Microbiol Infect. 2013;20:678–682. doi: 10.1111/1469-0691.12438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Memish Z.A., Al-Tawfiq J.A., Assiri A. Middle East respiratory syndrome coronavirus disease in children. Pediatr Infect Dis J. 2014;33:904–906. doi: 10.1097/INF.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 25.Omrani A.S., Memish Z.A. Therapeutic options for Middle East respiratory syndrome coronavirus (MERS-CoV) infection: how close are we? Curr Treat Options Infect Dis. 2015:1–15. doi: 10.1007/s40506-015-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Falzarano D., de Wit E., Rasmussen A.L. Treatment with interferon-alpha2b and ribavirin improves outcome in MERS-CoV-infected rhesus macaques. Nature Med. 2013;19:1313–1317. doi: 10.1038/nm.3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization . WHO; Geneva: 2015. Clinical management of severe acute respiratory infection when Middle East respiratory syndrome coronavirus (MERS-CoV) infection is suspected; interim guidance updated 2 July 2015.http://apps.who.int/iris/bitstream/10665/178529/1/WHO_MERS_Clinical_15.1_eng.pdf?ua=1 Available at: [last accessed August 2015] [Google Scholar]
- 28.Corman V.M., Muller M.A., Costabel U. Assays for laboratory confirmation of novel human coronavirus (hCoV-EMC) infections. Euro Surveill. 2012;17:20334. doi: 10.2807/ese.17.49.20334-en. [DOI] [PubMed] [Google Scholar]
- 29.Memish Z.A., Al-Tawfiq J.A., Makhdoom H.Q. Respiratory tract samples, viral load, and genome fraction yield in patients with Middle East respiratory syndrome. J Infect Dis. 2014;210:1590–1594. doi: 10.1093/infdis/jiu292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guery B., Poissy J., el Mansouf L. Clinical features and viral diagnosis of two cases of infection with Middle East respiratory syndrome coronavirus: a report of nosocomial transmission. Lancet. 2013;381:2265–2272. doi: 10.1016/S0140-6736(13)60982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Memish Z.A., Assiri A.M., Al-Tawfiq J.A. Middle East respiratory syndrome coronavirus (MERS-CoV) viral shedding in the respiratory tract: an observational analysis with infection control implications. Int J Infect Dis. 2014;29:307–308. doi: 10.1016/j.ijid.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faure E., Poissy J., Goffard A. Distinct immune response in two MERS-CoV-infected patients: can we go from bench to bedside? PloS One. 2014;9:e88716. doi: 10.1371/journal.pone.0088716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Doremalen N., Bushmaker T., Munster V.J. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18:20590. doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- 34.Memish Z.A., Cotten M., Watson S.J. Community case clusters of Middle East respiratory syndrome coronavirus in Hafr Al-Batin, Kingdom of Saudi Arabia: a descriptive genomic study. Int J Infect Dis. 2014;23:63–68. doi: 10.1016/j.ijid.2014.03.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park H.Y., Lee E.J., Ryu Y.W. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20:21169. doi: 10.2807/1560-7917.es2015.20.25.21169. [DOI] [PubMed] [Google Scholar]
- 36.Lee S.S., Wong N.S. Probable transmission chains of MERS-CoV and the multiple generations of secondary infections in South Korea. Int J Infect Dis. 2015 doi: 10.1016/j.ijid.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Drosten C., Meyer B., Muller M.A. Transmission of MERS-coronavirus in household contacts. N Engl J Med. 2014;371:828–835. doi: 10.1056/NEJMoa1405858. [DOI] [PubMed] [Google Scholar]
- 38.Memish Z.A., Al-Tawfiq J.A., Makhdoom H.Q. Screening for Middle East respiratory syndrome coronavirus infection in hospital patients and their healthcare worker and family contacts: a prospective descriptive study. Clin Microbiol Infect. 2014;20:469–474. doi: 10.1111/1469-0691.12562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pebody R.G., Chand M.A., Thomas H.L. The United Kingdom public health response to an imported laboratory confirmed case of a novel coronavirus in September 2012. Euro Surveill. 2012;17:20292. [PubMed] [Google Scholar]
- 40.Parry-Ford F., Boddington N., Pebody R., Phin N. Public health response to two incidents of confirmed MERS-CoV cases travelling on flights through London Heathrow Airport in 2014 – lessons learnt. Euro Surveill. 2015;20:21114. doi: 10.2807/1560-7917.es2015.20.18.21114. [DOI] [PubMed] [Google Scholar]
- 41.Reuss A., Litterst A., Drosten C. Contact investigation for imported case of Middle East respiratory syndrome, Germany. Emerg Infect Dis. 2014;20:620–625. doi: 10.3201/eid2004.131375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buchholz U., Muller M.A., Nitsche A. Contact investigation of a case of human novel coronavirus infection treated in a German hospital, October–November 2012. Euro Surveill. 2013;18:20406. [PubMed] [Google Scholar]
- 43.Mailles A., Blanckaert K., Chaud P. First cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infections in France, investigations and implications for the prevention of human-to-human transmission, France, May 2013. Euro Surveill. 2013;18:20502. [PubMed] [Google Scholar]
- 44.Tsiodras S., Baka A., Mentis A. A case of imported Middle East respiratory syndrome coronavirus infection and public health response, Greece, April 2014. Euro Surveill. 2014;19:20782. doi: 10.2807/1560-7917.es2014.19.16.20782. [DOI] [PubMed] [Google Scholar]
- 45.Kraaij-Dirkzwager M., Timen A., Dirksen K. Middle East respiratory syndrome coronavirus (MERS-CoV) infections in two returning travellers in the Netherlands, May 2014. Euro Surveill. 2014;19:20817. doi: 10.2807/1560-7917.es2014.19.21.20817. [DOI] [PubMed] [Google Scholar]
- 46.Breakwell L., Pringle K., Chea N. Lack of transmission among close contacts of patient with case of Middle East respiratory syndrome imported into the United States, 2014. Emerg Infect Dis. 2015;21:1128–1134. doi: 10.3201/eid2107.150054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cotten M., Watson S.J., Zumla A.I. Spread, circulation, and evolution of the Middle East respiratory syndrome coronavirus. mBio. 2014;5:e01062–01013. doi: 10.1128/mBio.01062-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Drosten C., Muth D., Corman V.M. An observational, laboratory-based study of outbreaks of Middle East respiratory syndrome coronavirus in Jeddah and Riyadh, kingdom of Saudi Arabia, 2014. Clin Infect Dis. 2015;60:369–377. doi: 10.1093/cid/ciu812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Breban R., Riou J., Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013;382:694–699. doi: 10.1016/S0140-6736(13)61492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cauchemez S., Fraser C., Van Kerkhove M.D. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14:50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization . WHO; Geneva: 2013. Infection prevention and control during health care for probable or confirmed cases of novel coronavirus (nCoV) infection; interim guidance.http://www.who.int/csr/disease/coronavirus_infections/IPCnCoVguidance_06May13.pdf Available at: [last accessed August 2015] [Google Scholar]
- 52.Ministry of Health, Saudi Arabia . 2nd ed. Ministry of Health, Saudi Arabia; Riyadh: 2014. Infection prevention/control and management guidelines for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) infection.http://www.moh.gov.sa/en/CCC/StaffRegulations/Corona/Documents/GuidelinesforCoronaPatients.pdf Available at: [last accessed August 2015] [PubMed] [Google Scholar]
- 53.Madani T.A., Althaqafi A.O., Alraddadi B.M. Infection prevention and control guidelines for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) infection. Saudi Med J. 2014;35:897–913. [PubMed] [Google Scholar]
- 54.World Health Organization . WHO; Geneva: 2012. Case definition for case finding severe respiratory disease associated with novel coronavirus. Interim case definition as of 25 September 2012.http://www.who.int/csr/disease/coronavirus_infections/case_definition_25_09_2012/en/ Available at: [last accessed August 2015] [Google Scholar]
- 55.World Health Organization . WHO; Geneva: 2013. Revised interim case definition – novel coronavirus. Interim case definition as of 16 January 2013.http://www.who.int/csr/disease/coronavirus_infections/case_definition_16_01_2013/en/ Available at: [last accessed August 2015] [Google Scholar]
- 56.World Health Organization . WHO; Geneva: 2013. Revised interim case definition for reporting to WHO – Middle East respiratory syndrome coronavirus (MERS-CoV). Interim case definition as of 19 February 2013.http://www.who.int/csr/disease/coronavirus_infections/case_definition_19_02_2013/en/ Available at: [last accessed August 2015] [Google Scholar]
- 57.World Health Organization . WHO; Geneva: 2013. Revised interim case definition for reporting to WHO – Middle East respiratory syndrome coronavirus (MERS-CoV). Interim case definition as of 3 July 2013.http://www.who.int/csr/don/03-july-2015-mers-saudi-arabia/en/ Available at: [last accessed August 2015] [Google Scholar]
- 58.Al-Gethamy M., Corman V.M., Hussain R., Al-Tawfiq J.A., Drosten C., Memish Z.A. A case of long-term excretion and subclinical infection with Middle East respiratory syndrome coronavirus in a healthcare worker. Clin Infect Dis. 2015;60:973–974. doi: 10.1093/cid/ciu1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shalhoub S., AlZahrani A., Simhairi R., Mushtaq A. Successful recovery of MERS-CoV pneumonia in a patient with acquired immunodeficiency syndrome: a case report. J Clin Virol. 2015;62:69–71. doi: 10.1016/j.jcv.2014.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Madani T.A. Case definition and management of patients with MERS coronavirus in Saudi Arabia. Lancet Infect Dis. 2014;14:911–913. doi: 10.1016/S1473-3099(14)70918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.World Health Organization . WHO; Geneva: 2015. Investigation of cases of human infection with Middle East respiratory syndrome coronavirus (MERS-CoV); interim guidance updated 3 July 2015.http://apps.who.int/iris/bitstream/10665/178252/1/WHO_MERS_SUR_15.2_eng.pdf?ua=1 Available at: [last accessed August 2015] [Google Scholar]
- 62.Drexler J.F., Corman V.M., Drosten C. Ecology, evolution and classification of bat coronaviruses in the aftermath of SARS. Antiviral Res. 2014;101:45–56. doi: 10.1016/j.antiviral.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lelli D., Papetti A., Sabelli C., Rosti E., Moreno A., Boniotti M.B. Detection of coronaviruses in bats of various species in Italy. Viruses. 2013;5:2679–2689. doi: 10.3390/v5112679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Memish Z.A., Mishra N., Olival K.J. Middle East respiratory syndrome coronavirus in bats, Saudi Arabia. Emerg Infect Dis. 2013;19:1819–1823. doi: 10.3201/eid1911.131172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ithete N.L., Stoffberg S., Corman V.M. Close relative of human Middle East respiratory syndrome coronavirus in bat, South Africa. Emerg Infect Dis. 2013;19:1697–1699. doi: 10.3201/eid1910.130946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Corman V.M., Ithete N.L., Richards L.R. Rooting the phylogenetic tree of MERS-Coronavirus by characterization of a conspecific virus from an African Bat. J Virol. 2014;88:11297–11303. doi: 10.1128/JVI.01498-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reusken C.B., Haagmans B.L., Muller M.A. Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect Dis. 2013;13:859–866. doi: 10.1016/S1473-3099(13)70164-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hemida M.G., Perera R.A., Wang P. Middle East respiratory syndrome (MERS) coronavirus seroprevalence in domestic livestock in Saudi Arabia, 2010 to 2013. Euro Surveill. 2013;18:20659. doi: 10.2807/1560-7917.es2013.18.50.20659. [DOI] [PubMed] [Google Scholar]
- 69.Reusken C.B., Ababneh M., Raj V.S. Middle East respiratory syndrome coronavirus (MERS-CoV) serology in major livestock species in an affected region in Jordan, June to September 2013. Euro Surveill. 2013;18:20662. doi: 10.2807/1560-7917.es2013.18.50.20662. [DOI] [PubMed] [Google Scholar]
- 70.Reusken C.B., Messadi L., Feyisa A. Geographic distribution of MERS coronavirus among dromedary camels, Africa. Emerg Infect Dis. 2014;20:1370–1374. doi: 10.3201/eid2008.140590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alexandersen S., Kobinger G.P., Soule G., Wernery U. Middle East respiratory syndrome coronavirus antibody reactors among camels in Dubai, United Arab Emirates, in 2005. Transbound Emerg Dis. 2014;61:105–108. doi: 10.1111/tbed.12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nowotny N., Kolodziejek J. Middle East respiratory syndrome coronavirus (MERS-CoV) in dromedary camels, Oman, 2013. Euro Surveill. 2014;19:20781. doi: 10.2807/1560-7917.es2014.19.16.20781. [DOI] [PubMed] [Google Scholar]
- 73.Corman V.M., Jores J., Meyer B. Antibodies against MERS coronavirus in dromedary camels, Kenya, 1992–2013. Emerg Infect Dis. 2014;20:1319–1322. doi: 10.3201/eid2008.140596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alagaili A.N., Briese T., Mishra N. Middle East respiratory syndrome coronavirus infection in dromedary camels in Saudi Arabia. mBio. 2014;5:e00884–00814. doi: 10.1128/mBio.00884-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hemida M.G., Perera R.A., Al Jassim R.A. Seroepidemiology of Middle East respiratory syndrome (MERS) coronavirus in Saudi Arabia (1993) and Australia (2014) and characterisation of assay specificity. Euro Surveill. 2014;19:20828. doi: 10.2807/1560-7917.es2014.19.23.20828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hemida M.G., Chu D.K., Poon L.L. MERS coronavirus in dromedary camel herd, Saudi Arabia. Emerg Infect Dis. 2014;20:1231–1234. doi: 10.3201/eid2007.140571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chu D.K., Poon L.L., Gomaa M.M. MERS coronaviruses in dromedary camels, Egypt. Emerg Infect Dis. 2014;20:1049–1053. doi: 10.3201/eid2006.140299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Raj V.S., Farag E.A., Reusken C.B. Isolation of MERS coronavirus from a dromedary camel, Qatar, 2014. Emerg Infect Dis. 2014;20:1339–1342. doi: 10.3201/eid2008.140663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khalafalla A.I., Lu X., Al-Mubarak A.I., Dalab A.H., Al-Busadah K.A., Erdman D.D. MERS-CoV in upper respiratory tract and lungs of dromedary camels, Saudi Arabia, 2013–2014. Emerg Infect Dis. 2015;21:1153–1158. doi: 10.3201/eid2107.150070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Haagmans B.L., Al Dhahiry S.H., Reusken C.B. Middle East respiratory syndrome coronavirus in dromedary camels: an outbreak investigation. Lancet Infect Dis. 2014;14:140–145. doi: 10.1016/S1473-3099(13)70690-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Memish Z.A., Cotten M., Meyer B. Human infection with MERS coronavirus after exposure to infected camels, Saudi Arabia, 2013. Emerg Infect Dis. 2014;20:1012–1015. doi: 10.3201/eid2006.140402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wernery U., Corman V.M., Wong E.Y. Acute Middle East respiratory syndrome coronavirus infection in livestock dromedaries, Dubai, 2014. Emerg Infect Dis. 2015;21:1019–1022. doi: 10.3201/eid2106.150038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chan R.W., Hemida M.G., Kayali G. Tropism and replication of Middle East respiratory syndrome coronavirus from dromedary camels in the human respiratory tract: an in-vitro and ex-vivo study. Lancet Resp Med. 2014;2:813–822. doi: 10.1016/S2213-2600(14)70158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Adney D.R., van Doremalen N., Brown V.R. Replication and shedding of MERS-CoV in upper respiratory tract of inoculated dromedary camels. Emerg Infect Dis. 2014;20:1999–2005. doi: 10.3201/eid2012.141280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Madani T.A., Azhar E.I., Hashem A.M. Evidence for camel-to-human transmission of MERS coronavirus. N Engl J Med. 2014;371:1360. doi: 10.1056/NEJMc1409847. [DOI] [PubMed] [Google Scholar]
- 86.Reusken C.B., Farag E.A., Haagmans B.L. Occupational exposure to dromedaries and risk for MERS-CoV infection, Qatar, 2013–2014. Emerg Infect Dis. 2015;21:1422–1425. doi: 10.3201/eid2108.150481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hemida M.G., Al-Naeem A., Perera R.A., Chin A.W., Poon L.L., Peiris M. Lack of Middle East respiratory syndrome coronavirus transmission from infected camels. Emerg Infect Dis. 2015;21:699–701. doi: 10.3201/eid2104.141949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Aburizaiza A.S., Mattes F.M., Azhar E.I. Investigation of anti-Middle East respiratory syndrome antibodies in blood donors and slaughterhouse workers in Jeddah and Makkah, Saudi Arabia, fall 2012. J Infect Dis. 2014;209:243–246. doi: 10.1093/infdis/jit589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Memish Z.A., Alsahly A., Masri M.A. Sparse evidence of MERS-CoV infection among animal workers living in Southern Saudi Arabia during 2012. Influenza Other Respir Viruses. 2015;9:64–67. doi: 10.1111/irv.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.World Health Organization . WHO; Geneva: 2015. Middle East respiratory syndrome coronavirus (MERS-CoV) – Thailand. Disease Outbreak News 20 June 2015.http://www.who.int/csr/don/20-june-2015-mers-thailand/en/ Available at: [last accessed August 2015] [Google Scholar]
- 91.World Health Organization . WHO; Geneva: 2014. Middle East respiratory syndrome coronavirus (MERS-CoV) – Austria.http://www.who.int/csr/don/02-october-2014-mers-austria/en/ Available at: [last accessed August 2015] [Google Scholar]
- 92.Kapoor M., Pringle K., Kumar A. Clinical and laboratory findings of the first imported case of Middle East respiratory syndrome coronavirus to the United States. Clin Infect Dis. 2014;59:1511–1518. doi: 10.1093/cid/ciu635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.World Health Organization . WHO; Geneva: 2015. Middle East respiratory syndrome coronavirus (MERS-CoV) – The Philippines.http://www.who.int/csr/don/13-february-2015-mers/en/ Available at: [last accessed August 2015] [Google Scholar]
- 94.Puzelli S., Azzi A., Santini M.G. Investigation of an imported case of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in Florence, Italy, May to June 2013. Euro Surveill. 2013;18(34) doi: 10.2807/1560-7917.es2013.18.34.20564. [DOI] [PubMed] [Google Scholar]
- 95.Abroug F., Slim A., Ouanes-Besbes L. Family cluster of Middle East respiratory syndrome coronavirus infections, Tunisia, 2013. Emerg Infect Dis. 2014;20:1527–1530. doi: 10.3201/eid2009.140378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Premila Devi J., Noraini W., Norhayati R. Laboratory-confirmed case of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in Malaysia: preparedness and response, April 2014. Euro Surveill. 2014;19:20797. doi: 10.2807/1560-7917.es2014.19.18.20797. [DOI] [PubMed] [Google Scholar]
- 97.Health Protection Agency UK Novel Coronavirus Investigation Team Evidence of person-to-person transmission within a family cluster of novel coronavirus infections, United Kingdom, February 2013. Euro Surveill. 2013;18:20427. doi: 10.2807/ese.18.11.20427-en. [DOI] [PubMed] [Google Scholar]
- 98.Gardner L.M., Rey D., Heywood A.E. A scenario-based evaluation of the Middle East respiratory syndrome coronavirus and the Hajj. Risk Anal. 2014;34:1391–1400. doi: 10.1111/risa.12253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gautret P. Middle East respiratory syndrome (MERS) coronavirus. What travel health advice should be given to Hajj pilgrims? Travel Med Infect Dis. 2013;11:263–265. doi: 10.1016/j.tmaid.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gautret P., Benkouiten S., Salaheddine I., Parola P., Brouqui P. Preventive measures against MERS-CoV for Hajj pilgrims. Lancet Infect Dis. 2013;13:829–831. doi: 10.1016/S1473-3099(13)70259-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zumla A., Mwaba P., Bates M., Al-Tawfiq J.A., Maeurer M., Memish Z.A. The Hajj pilgrimage and surveillance for Middle East respiratory syndrome coronavirus in pilgrims from African countries. Trop Med Int Health. 2014;19:838–840. doi: 10.1111/tmi.12318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Khan K., Sears J., Hu V.W. Potential for the international spread of Middle East respiratory syndrome in association with mass gatherings in Saudi Arabia. PLoS Curr. 2013;5 doi: 10.1371/currents.outbreaks.a7b70897ac2fa4f79b59f90d24c860b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gautret P., Charrel R., Belhouchat K. Lack of nasal carriage of novel corona virus (HCoV-EMC) in French Hajj pilgrims returning from the Hajj 2012, despite a high rate of respiratory symptoms. Clin Microbiol Infect. 2013;19:e315–317. doi: 10.1111/1469-0691.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gautret P., Charrel R., Benkouiten S. Lack of MERS coronavirus but prevalence of influenza virus in French pilgrims after 2013 Hajj. Emerg Infect Dis. 2014;20:726–728. doi: 10.3201/eid2004.131708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Memish Z.A., Assiri A., Almasri M. Prevalence of MERS-CoV nasal carriage and compliance with the Saudi health recommendations among pilgrims attending the 2013 Hajj. J Infect Dis. 2014;210:1067–1072. doi: 10.1093/infdis/jiu150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Raoult D., Charrel R., Gautret P., Parola P. From the Hajj: it's the flu, idiot. Clin Microbiol Infect. 2014;20:O1. doi: 10.1111/1469-0691.12448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Annan A., Owusu M., Marfo K.S. High prevalence of common respiratory viruses and no evidence of Middle East respiratory syndrome coronavirus in Hajj pilgrims returning to Ghana, 2013. Trop Med Int Health. 2015;20:807–812. doi: 10.1111/tmi.12482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Benkouiten S., Charrel R., Belhouchat K. Circulation of respiratory viruses among pilgrims during the 2012 Hajj pilgrimage. Clin Infect Dis. 2013;57:992–1000. doi: 10.1093/cid/cit446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.ProMED-mail . International Society for Infectious Diseases; Washington DC: 2015. MERS-CoV (100): Saudi Arabia, South Korea. Archive Number: 20150804.3558326. 04-08-2015 21:27:59.http://www.promedmail.org/direct.php?id=3558326 Available at: [last accessed August 2015] [Google Scholar]
- 110.Cowling B.J., Park M., Fang V.J., Wu P., Leung G.M., Wu J.T. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015;20:21163. doi: 10.2807/1560-7917.es2015.20.25.21163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Khan A., Farooqui A., Guan Y., Kelvin D.J. Lessons to learn from MERS-CoV outbreak in South Korea. J Infect Dev Ctries. 2015;9:543–546. doi: 10.3855/jidc.7278. [DOI] [PubMed] [Google Scholar]
- 112.Hui D.S., Perlman S., Zumla A. Spread of MERS to South Korea and China. Lancet Resp Med. 2015;3:509–510. doi: 10.1016/S2213-2600(15)00238-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ministry of Health and Welfare (MOHW) and Korean Centers for Disease Control and Prevention (KCDC) MOHW and KCDC; Seoul: 2015. List of hospitals with known MERS exposure; 22 June 2015.http://cdc.go.kr/CDC/info/CdcKrHealth0298.jsp?menuIds=HOME001-MNU1132-MNU1013&fid=5767&q_type=&q_value=&cid=63640&pageNum Available at: [last accessed August 2015] [Google Scholar]
- 114.World Health Organization . WHO; Geneva: 2015. Preliminary data from sequencing of viruses in the Republic of Korea and the People's Republic of China. MERS-CoV situation assessment 9 June 2015.http://www.who.int/csr/disease/coronavirus_infections/mers-situation-assessment09-06.pdf?ua=1 Available at: [last accessed August 2015] [Google Scholar]
- 115.World Health Organization . WHO; Geneva: 2015. Managing contacts in the MERS-CoV outbreak in the Republic of Korea; briefing notes on MERS-CoV 1 July 2015.http://www.who.int/mediacentre/news/mers/briefing-notes/update-1-july-2015/en/ Available at: [last accessed August 2015] [Google Scholar]
- 116.World Health Organization . WHO; Geneva: 2015. Middle East respiratory syndrome coronavirus (MERS-CoV): Summary and risk assessment of current situation in the Republic of Korea and China – as of 19 June 2015.http://www.who.int/emergencies/mers-cov/mers-cov-republic-of-korea-and-china-risk-assessment-19-june-2015.pdf?ua=1 Available at: [last accessed August 2015] [Google Scholar]
- 117.Korean Society of Infectious Diseases Korean Society for Healthcare-associated Infection Control and Prevention. An unexpected outbreak of Middle East Respiratory syndrome coronavirus infection in the Republic of Korea, 2015. Infect Chemother. 2015;47:120–122. doi: 10.3947/ic.2015.47.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.George D.R., Rovniak L.S., Kraschnewski J.L. Dangers and opportunities for social media in medicine. Clin Obstet Gynecol. 2013;56:453–462. doi: 10.1097/GRF.0b013e318297dc38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ventola C.L. Social media and health care professionals: benefits, risks, and best practices. Pharm Therapeut (P T) 2014;39:491–520. [PMC free article] [PubMed] [Google Scholar]
- 120.Chretien K.C., Kind T. Social media and clinical care: ethical, professional, and social implications. Circulation. 2013;127:1413–1421. doi: 10.1161/CIRCULATIONAHA.112.128017. [DOI] [PubMed] [Google Scholar]
- 121.Mackay I.M., Arden K.E. Middle East respiratory syndrome: an emerging coronavirus infection tracked by the crowd. Virus Res. 2015;202:60–88. doi: 10.1016/j.virusres.2015.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]