Summary
The epidemics of severe acute respiratory syndrome (SARS) in 2003 highlighted both short- and long-range transmission routes, i.e. between infected patients and healthcare workers, and between distant locations. With other infections such as tuberculosis, measles and chickenpox, the concept of aerosol transmission is so well accepted that isolation of such patients is the norm. With current concerns about a possible approaching influenza pandemic, the control of transmission via infectious air has become more important. Therefore, the aim of this review is to describe the factors involved in: (1) the generation of an infectious aerosol, (2) the transmission of infectious droplets or droplet nuclei from this aerosol, and (3) the potential for inhalation of such droplets or droplet nuclei by a susceptible host. On this basis, recommendations are made to improve the control of aerosol-transmitted infections in hospitals as well as in the design and construction of future isolation facilities.
Keywords: Aerosol, Transmission, SARS, Influenza, Droplets, Control, Infection
Introduction
The experience in 2003 with severe acute respiratory syndrome (SARS) highlighted the issue of aerosol transmission, both short range between healthcare workers and their patients,1, 2, 3 and long range amongst the residents of the Amoy Gardens estate.4, 5 Aerosol or airborne transmission is already well recognized for many human pathogens. Much work has been performed using air-sampling techniques together with culture and molecular detection methods for viruses6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 [particularly varicella zoster virus (VZV)],17, 18, 19, 20, 21, 22, 23, 24 bacteria25, 26, 27, 28, 29, 30, 31, 32, 33 [particularly tuberculosis (Mycobacterium tuberculosis, TB) and other mycobacteria],34, 35, 36, 37, 38, 39, 40, 41, 42 and fungi (particularly Aspergillus spp.).43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56 Beggs reviewed the importance of airborne transmission of infection in hospitals, focusing mainly on bacteria that are well known to cause nosocomial infections, i.e. Staphylococcus aureus and meticillin-resistant S. aureus (MRSA), M. tuberculosis, Acinetobacter spp., Aspergillus spp., Pseudomonas spp. and Legionella spp.57 He concluded that, for these infections, although contact spread was still the main route of infection, infections via the airborne route, both direct and indirect (via the settling of airborne pathogens on fomites), were probably underestimated.
The generation of such infectious aerosols of infectious human pathogens can occur in many ways, and in many settings, although some have been studied more extensively than others due to their greater clinical significance. The literature on the risks of aerosol transmission of infection in hospital operating theatres is extensive.58, 59, 60, 61, 62, 63, 64, 65 Over 40 studies on the relationship between ventilation systems and the transmission of infection in hospitals, offices, aeroplanes and ships were reviewed recently by Li et al. 66 Studies have also been conducted on how infectious aerosols generated by various procedures in hospital environments can lead to infection in burns care facilities67, 68, 69 and medical intensive care units.70, 71 In particular, the use of oxygen masks,72, 73 and power tools in dental practice74, 75, 76, 77 and orthopaedics77, 78, 79, 80, 81, 82, 83, 84 may pose a risk of aerosol infection. Aerosol dispersal of infectious agents has also been demonstrated in wastewater spray sites,85 surface waves on the sea,86 the flushing of the household toilet,87 and even just opening a standard hinged door.88
Definitions
True long-range aerosol transmission becomes possible when the droplets of infectious material are sufficiently small to remain almost indefinitely airborne and to be transmitted over long distances. One set of infection control guidelines for healthcare settings suggested that only TB, measles (rubeola virus) and chickenpox (VZV) should be considered as ‘true’ airborne infectious diseases.89 However, it is likely that other infectious agents may also behave as ‘airborne’, given a favourable environment, e.g. whooping cough (Bordetella pertussis), influenza virus, adenovirus, rhinovirus, Mycoplasma pneumoniae, SARS coronavirus (SARS-CoV), group A streptococcus and Neisseria meningitidis. Many more organisms fall into this category, as it probably includes virtually all pathogens where replication and/or colonization occur in the respiratory tract. Table I lists organisms associated with varying degrees of aerosol transmission.90 Each organism can also be transmitted through direct contact with infected body fluids.
Table I.
Pathogens and diseases that have the potential to be transmitted via the airborne route
| Pathogen | Aerosol route of transmission |
|---|---|
| Anthrax | Inhalation of spores |
| Arenaviruses | Inhalation of small particle aerosols from rodent excreta |
| Aspergillosis | Inhalation of airborne conidia (spores) |
| Blastomycosis | Conidia, inhaled in spore-laden dust |
| Brucellosis | Inhalation of airborne bacteria |
| Chickenpox/shingles (varicella zoster virus) | Droplet or airborne spread of vesicle fluid or respiratory tract secretions |
| Coccidioidomycosis | Inhalation of infective arthroconidia |
| Adenovirus | Transmitted through respiratory droplets |
| Enteroviruses (coxsackie virus) | Aerosol droplet spread |
| Cryptococcosis | Presumably by inhalation |
| Human parvovirus | Contact with infected respiratory secretions |
| Rotavirus | Possible respiratory spread |
| Norwalk virus | Airborne transmission from fomites |
| Hantavirus | Presumed aerosol transmission from rodent excreta |
| Histoplasmosis | Inhalation of airborne conidia |
| Influenza | Airborne spread predominates |
| Lassa virus | Aerosol contact with excreta of infected rodents |
| Legionellosis | Epidemiological evidence supports airborne transmission |
| Lymphocytic choriomeningitis | Oral or respiratory contact with virus-contaminated excreta, food or dust |
| Measles | Airborne by droplet spread |
| Melioidosis | Inhalation of soil dust |
| Meningitis (Neisseria meningitidis) | Respiratory droplets from nose and throat |
| Meningitis (Haemophilus influenzae) | Droplet infection and discharges from nose and throat |
| Meningitis (Streptococcus pneumoniae) | Droplet spread and contact with respiratory secretions |
| Mumps | Airborne transmission or droplet spread |
| Nocardia | Acquired through inhalation |
| Paracoccidioidomycosis | Presumably through inhalation of contaminated soil or dust |
| Whooping cough (Bordetella pertussis) | Direct contact with discharges from respiratory mucous membranes of infected persons by the airborne route |
| Plague (Yersinia pestis) | Rarely airborne droplets from human patients. In the case of deliberate use, plague bacilli would possibly be transmitted as an aerosol |
| Pneumonia (S. pneumoniae) | Droplet spread |
| Pneumonia (Mycoplasma pneumoniae) | Probably droplet inhalation |
| Pneumonia (Chlamydia pneumoniaea) | Possibilities include airborne spread |
| Psittacosis (Chlamydia psittacia) | By inhaling the agent from desiccated droppings, secretions and dust from feathers of infected birds |
| Q fever (Coxiella burnetti) | Commonly through airborne dissemination of coxiellae in dust |
| Rabies | Airborne spread has been demonstrated in a cave where bats were roosting, and in laboratory settings, but this occurs very rarely |
| Rhinitis/common cold (rhinovirus, coronavirus, parainfluenza, respiratory syncytial virus) | Presumably inhalation of airborne droplets |
| Rubella | Droplet spread |
| Smallpox (Variola major) | Via respiratory tract (droplet spread) |
| Sporotrichosis | Pulmonary sporotrichosis presumably arises through inhalation of conidia |
| Staphylococcal diseases | Airborne spread is rare but has been demonstrated in patients with associated viral respiratory disease |
| Streptococcal diseases | Large respiratory droplets. Individuals with acute upper respiratory tract (especially nasal) infections are particularly likely to transmit infection |
| Toxoplasmosis | Inhalation of sporulated oocysts was associated with one outbreak |
| Tuberculosis | Exposure to tubercle bacilli in airborne droplet nuclei |
| Tularaemia (Francisella tularensis) | By inhalation of dust from contaminated soil, grain or hay |
Virtually all of these pathogens are also transmissible by direct contact. Pathogens in bold are those which are considered to have the potential to be transmitted by the long-range airborne route.89 The original wording of the reference text90 concerning aerosol transmission routes has been retained as much as possible.
Now known as Chlamydophila psittaci and Chlamydophila pneumoniae, but the original classification has been retained here as in the original reference text.90
A recent systematic review demonstrated that adequate or inadequate ventilation has an effect on the risk of infection via infectious aerosols.66 This interdisciplinary review, authored by a large group of engineers, microbiologists and epidemiologists, defined the following terms.
-
–
Airborne transmission refers to the passage of micro-organisms from a source to a person through aerosols, resulting in infection of the person with or without consequent disease.
-
–
Aerosols are a suspension of solid or liquid particles in a gas, with particle size from 0.001 to over 100 μm.91 Infectious aerosols contain pathogens.
-
–
A droplet nucleus is the airborne residue of a potentially infectious (micro-organism-bearing) aerosol from which most of the liquid has evaporated.92
On the basis of these definitions, the following clinically applicable distinctions are made between short-range airborne infection routes (between individuals, generally less than 1-m apart) and long-range routes (within a room, between rooms or between distant locations, generally greater than 1-m distances):
-
–
The short-range airborne infection route depends on the close proximity of the infected source and susceptible host. A study was performed recently (Xie et al., unpublished observations) to define more clearly the size of the droplets originally referred to by Wells.92 These terms are also in common current use. This study proposes the following size definitions: ‘large-droplet’ diameter >60 μm, ‘small droplet’ diameter ≤60 μm and ‘droplet nuclei’ diameter <10 μm. Note that small droplets may also participate in short-range transmission, but they are more likely than larger droplets to evaporate to become droplet nuclei and then be considered as having the potential for long-range airborne transmission (see below).93 Exhaled air from both nose and mouth is able to enter and mix with air in the breathing zone of another person standing nearby (e.g. patients and doctors on a ward round at the bedside). Thus, short-range transmission implies that air flows between individuals may interact to infect one another.94 In addition, it has been shown that the use of a simple oxygen mask may also generate a short-range (<1 m) infectious aerosol, with a potential risk to nearby healthcare workers and other patients.72, 73 Together with nebulizers, oxygen masks fall into this classification of potential short-range aerosol transmission sources, but some droplets generated by such masks can evaporate to become droplet nuclei that can also transmit infection over larger distances.57
-
–
Long-range aerosol transmission refers to the potential for agents to be carried long distances by air flows to cause infection, and includes the traditional terms ‘small-droplet’ or ‘droplet nuclei’ and ‘airborne’. Virtually all infectious agents that can cause infection at long range can also cause infection at short range as well as by direct contact. Therefore, use of the term ‘long range’ refers to the greatest distance from their source at which these agents have the potential to cause infection.
Infectious agents transmissible by aerosols
If the pathogen has some part of its life cycle in the respiratory tract, it is more likely to be present in aerosols generated and projected into the surrounding air by breathing, talking, coughing, sneezing and singing. For truly airborne pathogens (TB, measles and VZV), the routes of acquisition and dissemination of the infectious particles are well recognized to be via the respiratory tract. In the other pathogens listed in Table I, acquisition of the infection is also via the respiratory tract, which is the primary site of infection and replication. Therefore, these other pathogens, such as parvovirus B19, enteroviruses and the organisms of atypical pneumonias [M. pneumoniae, Chlamydophila psittaci (previously Chlamydia psittaci), Chlamydophila pneumoniae (previously Chlamydia pneumoniae), Coxiella burnetti and Legionella pneumophila], have the potential to be transmitted via aerosols as their life cycle involves replication at some point in the respiratory tract. Regarding L. pneumophila, replication also occurs in water systems, and human infection can occur via infected water aerosols, such as showerheads and fountains. With SARS-CoV, viral RNA as well as viable (culturable) virus has been found in air samples.95, 96 Therefore, SARS-CoV can potentially be transmitted by short- and long-range aerosols to cause disease, as has been strongly implicated by several studies.1, 2, 3, 4, 5
With influenza, there is ongoing debate about the nature of transmission between people. A recent review suggested that ‘aerosol-generating procedures…should be performed with proper infection control precautions’, but the authors do not elaborate on exactly what these precautions should be.97 Recent guidelines from the UK review the evidence for aerosol transmission of influenza more comprehensively.98 The report concluded that whilst close contact with infected individuals seems to be responsible for the vast majority of transmission, most reports of influenza transmission do not provide enough temporal-spatial data to determine whether transmission is mainly due to droplet, contact or airborne spread. This is probably the most realistic assessment, and this uncertainty is reflected in the large range of values for the basic reproductive number (R0, the number of secondary cases arising from a single index case in an otherwise totally susceptible population), ranging from 1–299 to 2–7100 to <21.101 However, there are reports to suggest that in pandemic or large, explosive outbreak situations, influenza can become truly airborne.12, 13 For comparison, the R0 values of other commonly encountered infections are shown in Table II.
Table II.
The basic reproductive number (R0) of some human infectious agents (adapted from Reference102 with additional references as indicated)
| Infectious disease | Basic reproductive number (R0) |
|---|---|
| Measles | 15–17 |
| Whooping cough | 15–17 |
| Chickenpox103 | 10–12 |
| Mumps | 10–12 |
| Rubella | 7–8 |
| Diphtheria | 5–6 |
| Poliomyelitis | 5–6 |
| Smallpox103 | 4–7 |
| Influenza99, 100, 101 | 1.68–20 |
| SARS104, 105 | 2–3 |
SARS, severe acute respiratory syndrome.
In contrast, other pathogens, such as human immunodeficiency virus and hepatitis B and C viruses, replicate mainly outside the respiratory tract and are not naturally transmitted via aerosols. With other organisms that can replicate on many surfaces either inside or outside the body, e.g. S. aureus, the picture is not so clear-cut. Although mainly spread by direct contact, there is a suggestion that patients that carry S. aureus in the respiratory tract can spread the bacteria by short-range aerosols.57, 106 S. aureus on skin epithelial cells on fomites, such as bed sheets, can also be spread during bed making.57, 106 This becomes more important when considering resistant strains such as MRSA.57
Sources of infectious agents
A commonly encountered source is the patient with flu-like symptoms who is coughing, sneezing and dispersing the organism ( Figure 1).107, 108 In the diagnostic laboratory, it may be an inoculated culture medium that is dropped or spilt, as has been reported for laboratory-acquired SARS infection.109 A more worrying possibility is the deliberate release of a biological agent, such as during the US terrorist anthrax attacks of 2001–2002,32, 33 or an accidental release, such as the anthrax incident in the Russian city of Sverdlovsk of 1979.110
Figure 1.
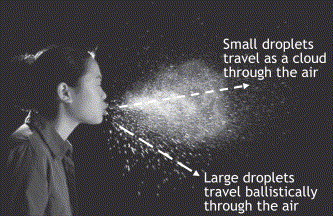
Droplet generation. A flash photo of a human sneeze, showing the expulsion of droplets that may be laden with infectious pathogens. Sneezing can produce as many as 40 000 droplets of 0.5–12 μm.107 These particles can be expelled at a velocity of 100 m/s,108 reaching distances of several metres. Smaller droplets with less mass are less influenced by gravity, and can be transported as a ‘cloud’ over greater distances by air flows. Larger droplets with more mass are more strongly influenced by gravity and less so by air flows, and move more ‘ballistically’, falling to the ground more quickly. Reproduced with the kind permission of Prof. Andrew Davidhazy, School of Photographic Arts and Sciences, Rochester Institute of Technology Rochester, NY, USA.
A sneeze can generate up to 40 000 droplets (Figure 1),107, 108 which can evaporate to produce droplets of 0.5–12 μm in diameter.107 A cough can generate about 3000 droplet nuclei, the same number as talking for 5 minutes.111 During normal breathing, exhalation can project droplets up to 1 m in room air, which may be inhaled by another person nearby ( Figure 2),94 whereas sneezing can project droplets several metres (Figure 1).107, 108 In addition, a recent study has shown that some individuals may exhale more particles during quiet breathing than others, suggesting that some people may be more infectious than others when infected with the same organism.112 The way that an infectious aerosol is generated should be considered when assessing the probable distance of spread. As noted earlier, large droplets can evaporate to become small droplets that can evaporate further to become droplet nuclei and hence become truly airborne if this evaporation process can occur before the droplet lands on the ground. The 2003 SARS epidemics also revealed iatrogenic and environmental factors that might contribute to producing virus-laden aerosols, such as those produced by nebulizers, tracheostomies, bronchoscopies,113, 114, 115, 116 and, in the Amoy Gardens outbreak, a defective sewage system.4, 5
Figure 2.
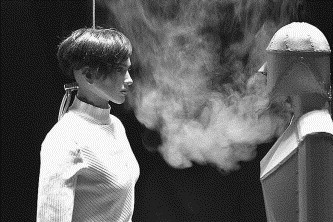
Smoke visualization of exhalation flow from nose of the right mannequin penetrating into the breathing zone of the left mannequin, which are 0.4 m apart.94 Reproduced from Figure 12 in Reference94 with the kind permission of Blackwell Publishing.
Mechanics of aerosol transmission of infectious agents
Once infectious droplets are released, the main factors that determine how they move are their size and the airflow patterns that carry them around ( Figure 3). The droplet size changes with time, depending on the environmental conditions. Humidity in the air alters the rate of droplet evaporation and therefore its size. Droplets in dry air evaporate quickly, reduce in size and fall to the ground more slowly.57 The changing size of a droplet affects how it will respond to airflow patterns and how quickly it will settle. Movement in air is determined by Stokes' settling law, which governs how quickly a sphere falls under the opposing forces of gravity downwards and air friction upwards (Figure 3).92 Knight estimated the times taken for particles of various diameters to fall 3 m (corresponding to the height of a room).10 Particles of diameters 1–3 μm remained suspended almost indefinitely, 10 μm took 17 min, 20 μm took 4 min, and 100 μm took 10 s to fall to the floor. ‘Naked’ viruses, bacteria and fungal spores (i.e. without associated water, mucus or pus droplets) range in approximate size from 0.02 to 0.3 μm, from 5 to 100 μm and from 1 to 10 μm, respectively. Infectious agents from patients can be expelled as individual or clusters of ‘naked’ organisms, or disseminated on skin cells, mucus or saliva.107 The amount of solid matter in a droplet ultimately determines its minimal size limit.
Figure 3.
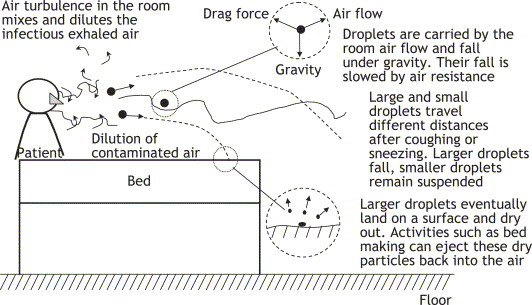
Droplet suspension. Illustration of the mechanics of suspension of droplet nuclei produced by an infected patient due to the effects of air friction and gravity.
Temperature differences can set up large exchange flows between rooms, in a similar way to leaving a front door open on a cold day ( Figure 4). Opening a hinged door leads to a sweeping action, which can also move a considerable volume of infectious air across the open doorway (Figure 4). A typical hinged door (about 1 m wide) opening relatively slowly from closed to 45° sweeps out one-eighth of a circle of circumference (C) 2π = 6.3 m (C = 2πr). Therefore, the door edge travels about 6.3/8 = about 0.8 m in about 2 s, generating an air flow with speed of approximately 0.8/2 = 0.4 m/s. In practice, doors may be opened faster and wider than this. As the door opens, air inside the room is dragged (or ‘entrained’) into the region swept by the door, leading to a large exchange of air across the doorway.117, 118 At least one case report has described a secondary case of chickenpox arising from infectious air being transported out of an isolation room containing a patient with severe chickenpox via the opening of a hinged door.88 Closing a door does not seem to lead to any significant air exchange between rooms. Such problems with hinged doors may be reduced by the use of sliding doors.
Figure 4.
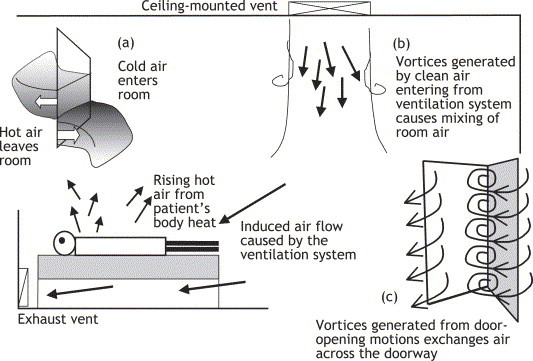
Droplet transport. The dispersion of the droplet nuclei is affected by the air flows from an open window, the ventilation system and door opening. (a) The air flow from an open window is affected by temperature differences between the inside and outside. In this figure, inside the room is warm and outside is cold. (b) The ceiling-mounted ventilation vent injects clean air into the room, which is removed by the exhaust vent near the patient's head, diluting the total amount of contaminated air. This also generates a downward flow pattern. (c) The action of opening a door generates a large vortex that sweeps clean air into the room and ejects contaminated air. When there are temperature differences between inside and outside, this also leads to a buoyancy exchange flow indicated in (a).
The effect of movement of people on air flow produces a similar effect to door opening, but is more complex and difficult to calculate. The velocity of the layer of air closest to the body is comparable to a person's walking speed. As a person moves at speed U, there is a volume flux, F, of air volume of approximately F = CAU/2, where C is the drag coefficient for a body (approximately equal to 1 in this example), A is the cross-sectional area of the body (for a person about 1.7 m tall, 0.3 m wide and 0.15 m deep, A = 1.7 × 0.3 = 0.51 m2) and U is velocity. In addition, there is a wake bubble of volume ɛV, where V is the volume of the body. In this example, V = 1.7 × 0.3×0.15 = 0.0765 m3 (i.e. a person of 76.5 kg, since 1 m3 = 100 × 100 × 100 cm3 = 1000 L water, assuming human body density has an average density equal to that of water) and ɛ = 1–3.119 For a person walking at speed U = 1 m/s, this corresponds to F = 1 × 0.51 × 1/2 = 0.255 m3 = 255 L/s, with an attached wake of ɛV = 0.0765–0.2295 m3 = 76–230 L/s. Thus, movement of people in a room plays a significant part in disturbing the flow and also in transporting infected air from one place to another ( Figure 5).
Figure 5.
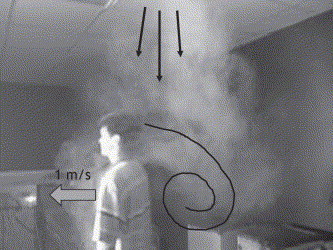
A snapshot of the movement of one person in the corridor of a full-scale test room for a six-bed general hospital ward. The ward was ventilated by a downward supply system with exhaust at floor level. At the time of the experiment, the supply air stream was marked by smoke. A person walking forward at about 1 m/s would push a front layer of air creating a volume flux, F, of about 255 L/s, with an attached wake of 76–230 L behind (see main text for calculations). This introduces a significant mixing air flow into the room.
Thus, room air flow is governed by a combination of air movements caused by differences in temperature/humidity and moving bodies/equipment. These complex air movements make the route and suspension time of an infectious particle very difficult to determine once it has left the infectious host. The infectivity of the droplet nuclei will also change with time, as the infectious organism will also be affected by the air temperature and humidity.
Environmental survival of infectious agents
To transmit from the respiratory tract of one person to another, the organisms in such droplets must remain airborne for a sufficient amount of time and must remain viable in a sufficient quantity to be inhaled by a susceptible host. Many environmental factors affect the viability of an infectious agent, e.g. temperature, humidity and air flows that might lead to dehydration,120 ultraviolet (UV) radiation,121, 122, 123 chemical hazards such as exhaust fumes from road transport or air pollution,120 and possibly cigarette smoke and air fresheners inside houses. Some organisms resist environmental degradation better than others. M. tuberculosis is a hardy organism with a thick cell wall, and can survive for long periods in the environment.111
Measles and VZV are both lipid enveloped and are sensitive to changes in temperature, relative humidity (RH) and UV radiation.124 Viruses without a lipid envelope generally survive longer at high RH (>50%), e.g. poliovirus,6, 120 but lipid-enveloped viruses survive longer in low RH (<50%), e.g. influenza,6, 110 Lassa fever virus125 and human coronavirus (hCV) 229E.126 Data on hCV 229E from Ijaz et al. showed that, when airborne, this virus had a survival half-life of about 3 h at an RH of 80%, 67 h at an RH of 50% and 27 h at an RH of 30%, at 20 °C, suggesting that high RH above 80% is most detrimental to survival of this coronavirus.126 Influenza has been shown to survive for 24–48 h on hard, non-porous surfaces such as stainless steel and plastic, but for less than 8–12 h on cloth, paper and tissues.127 In addition, influenza virus survived for up to 5 min on hands, and could be transferred to hands from these non-porous surfaces for 24 h and from tissues for 15 min.127 More recently, it has been shown that SARS-CoV can survive in alkaline diarrhoea stools for up to four days, and remain infectious in respiratory specimens for more than seven days at room temperature.128 Similarities with other viruses of nosocomial importance, i.e. other RNA, lipid-enveloped, respiratory viruses such as influenza, suggest that such organisms can survive for long enough in aerosols to cause disease, especially when associated with biological fluids such as mucus, faeces and blood. This sensitivity to environmental conditions may also partially explain the seasonality of some viral infections.
The situation is more complex in airborne bacteria. Gram-negative bacteria such as Escherichia coli and Klebsiella pneumoniae tend to behave like enveloped viruses, i.e. are less stable at high RH.120 In contrast, a study on another airborne Gram-negative bacterium, Salmonella seftenberg, found the opposite, i.e. that survival or ‘tenacity’ was highest at high RH.129 Cox suggested that a temperature of 10 °C offers optimal survival to most infectious pathogens.120 Hence, it is difficult to predict the survivability of infectious organisms from their structural characteristics alone.
Infectious doses of aerosol-transmitted agents
The infectious dose of a pathogen is the number of organisms required to cause infection. Theoretically, a single organism in a favourable environment may replicate sufficiently to cause disease. Guidelines for commissioning operating theatres recommend that the bioload in an empty theatre should not exceed 35 bacteria-carrying particles (e.g. skin scales)/m3 air.130, 131 During an operation, the bioload in the same theatre should not exceed 180 colony-forming units per cubic metre (CFU/m3, where 1 CFU represents the progeny from one viable bacterium).132 Such guidelines are developed in an attempt to minimize the risks of surgical nosocomial transmission.
Data from research performed on biological warfare agents suggest that both bacteria and viruses can produce disease with as few as 1–100 organisms (e.g. brucellosis 10–100, Q fever 1–10, tularaemia 10–50, smallpox 10–100, viral haemorrhagic fevers 1–10 organisms).132 M. tuberculosis may need only a single organism to cause disease, and as many as 3000 organisms can be produced by a cough or talking for 5 min, with sneezing producing many more.111 For many common agents, the infectious dose almost certainly varies between individual pathogens and their hosts, e.g. immunocompromised hosts may not only be more susceptible to infection with a lower infectious dose, but may also be a more infectious source, as the pathogen is poorly controlled by the defective immune system. This may allow higher pathogen loads to be disseminated into the surrounding environment in some cases, possibly leading to super-spreading events, such as described in some SARS outbreaks.1, 2, 3, 4, 5 Knowledge of the infectious dose of airborne pathogens may allow an estimate of the number of air changes required in an indoor environment to reduce the concentration of such pathogens below the level that can cause disease.
Methods of control of infectious aerosols
Li et al. reviewed the evidence for the effects of ventilation on the transmission of infectious diseases.66 They concluded that there was good evidence (as demonstrated by the contemporary technology available at the time of the studies) for aerosol transmission influenced by ventilation factors in outbreaks involving measles,133 chickenpox,134 the pneumococcus (Streptococcus pneumoniae),135 SARS-CoV,1, 2, 3, 4, 5 tuberculosis,136, 137 influenza138, 139 and smallpox.140 Therefore, from this and other studies reviewed here, it should be possible to reduce the risk of aerosol transmission by altering ventilation parameters in healthcare environments.
For short-range aerosol transmission exposures, personal protective equipment (PPE; i.e. gowns, gloves and facemasks) is recommended in addition to the usual contact-transmission prevention precautions (i.e. handwashing, avoiding touching mucous membranes of the eyes, nose and mouth) to protect susceptible healthcare workers. Seto et al. performed a study on the effectiveness of masks in reducing infection during the SARS outbreak, and found that surgical masks were effective in reducing infection from SARS to a certain extent.141 However, with more infectious diseases such as TB, measles or chickenpox, a surgical mask alone may be insufficient aerosol protection, and masks with built-in filters, i.e. filtered face piece masks, may be required. Droplet nuclei produced during respiration, talking, coughing and sneezing from such patients are very small, less than 5 μm in diameter, and behave similarly to smoke particles in air.142 Where susceptible hosts are widely separated in an indoor space, the potential for airborne transmission depends partially on the ventilation system present. In the community, some studies during the SARS outbreak in Hong Kong suggested that the use of facemasks and covering the mouth when sneezing may have contributed to an overall reduction in the incidence of viral respiratory infections at this time.143, 144
For the control of long-range aerosol transmission, the architecture of the healthcare facilities requires consideration. Hospital rooms are connected by doorways, corridors, stairwells and lift shafts. Small pressure differences, induced by natural forces such as thermal buoyancy due to air temperature differences, the wind or mechanical fans, can generate air flows that move air from one room to another. These air flows are very sensitive to doors or windows being kept open, e.g. although opening a window can enhance natural ventilation, this can change the air pressure in neighbouring rooms and corridors, reducing, or even reversing, airflow directions (Figure 4). This highlights the importance of keeping isolation room windows and doors closed.
The use of air filtration aims to reduce airborne concentrations to well below their infectious dose. Besides simply increasing the number of air changes per hour, there are other ways in which manipulation of air flows can be used to reduce the spread of airborne infection in an indoor environment such as a hospital. One main difficulty in designing ventilation systems for removing airborne pathogens is due to the fact that air flow is generally turbulent. In a hospital environment, if a ventilation system can ensure that the inhaled air for each individual mainly consists of fresh outdoor air, the system would be considered effective as the purpose of ventilation is to protect individuals from inhaling hazardous, infectious air.145 This principle can be broken down into three approaches, as follows.
-
–
Mixing of the contaminated air with uncontaminated air in the room, reducing the peak concentrations of droplet nuclei in the contaminated air. Over time, the average concentration of the droplet nuclei in the room will increase, unless the air is filtered.
-
–
Diluting contaminated air using ‘fresh’ (uninfected) air. Current recommendations of ventilation flow rate in various different guidelines for hospital ventilation and isolation room designs are based on the principle of dilution.146 A ventilation flow rate of at least 12 air changes (of a room)/h is suggested for new isolation rooms (constructed since 2001). Existing isolation rooms (constructed before 2001) may still use six air changes/h.89, 147
-
–
Controlling the air flow so that it moves from healthcare workers to patient. This requires putting patients and exhaust vents in close proximity.
Practically, there are at least two commonly used air distribution systems in general hospital wards. These are the mixing ventilation and displacement ventilation systems ( Figure 6).
Figure 6.
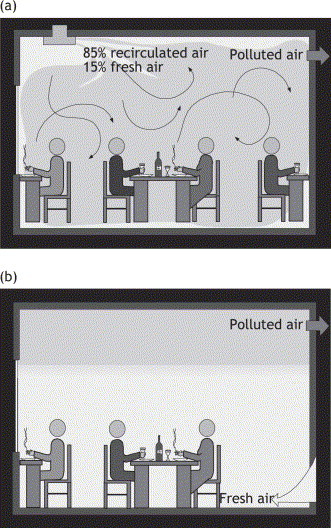
Illustration of the two commonly used air distribution methods in rooms. (a) Mixing ventilation: the cool air is supplied at ceiling level at high velocity and returned at either ceiling or floor level. The air in the room is generally fully mixed due to the strong mixing created by the overall air recirculation in the room, governed by the strong supply momentum. (b) Displacement ventilation: the cool air is supplied at floor level at low velocity and returned at ceiling level. The air in the room is divided into two parts: the upper part with ‘polluted’ air and the lower part with ‘clean’ air. Both parts of figure reproduced with the kind permission of CSIRO Australia. © CSIRO.
Mixing ventilation
The idea is to create a uniform low concentration of infected air in the room air that is subsequently extracted. The air is supplied along the ceiling or directed upwards along the window or wall surface, as shown in Figure 6(a).
Displacement ventilation
This refers to ‘fresh’ air sweeping in one direction across a room, carrying the pollutants with it and exhausting the polluted air. The flow is driven by large temperature differences in the room.145, 148 The vertical downward displacement ventilation system would be the ideal ventilation system for operating theatres, but there is a need for further study in the effectiveness of removing large particles with the upward vertical displacement system shown in Figure 6(b). However, a recent study demonstrated that the exhaled air plumes from a patient lying on his/her side on a bed could be spread over long distances, assisted by differences in air temperature and density, on a ward using displacement ventilation.149 This suggests that displacement ventilation should be used with caution in hospital wards, where such a risk of aerosol transmission is present.
In practice, ventilation usually consists of a combination of mixing and displacement ventilation. The fresh air stream mixes with convection currents, such as the heat plumes that arise above people and equipment. To remove infectious particles, existing guidelines recommend that the air flow should follow a path from the ceiling supply vents to the healthcare workers, then to the patients, then finally to the exhaust vents that are generally located at a lower level, near the floor.147
Ventilation and air flows also affect the thermal comfort of both healthcare workers and patients. The air speed in the occupied zone of a room is designed to be below 0.2 m/s for reasons of comfort.150 Due to differences in metabolic rate and clothing, the cooling or heating requirements of healthcare workers and patients can be different. Thermal discomfort such as sweating may also discourage the proper use of PPE by HCWs and thus limit its effectiveness.141
To reduce the spread of airborne contamination between rooms, it is common to fit ventilation systems with the capability to produce negative pressures, so that the direction of flow around closed leaky windows and doors can be controlled. For instance, in a negative pressure room, the supply flow rate to the room is less than the exhaust flow rate. Such ‘negative pressure’ isolation rooms are generally separately air-conditioned and temperature controlled, but there is likely to be a temperature difference between adjacent rooms. Current guidelines recommend a minimum negative pressure of 2.5 Pa (0.01 inch water gauge) in relation to corridors, although other guidelines recommend a negative pressure of 5–10 Pa.147, 151, 152, 153, 154 In practice, however, the negative pressure will fluctuate with time, depending on the control method and environmental factors. These systems need to be regularly maintained because it is commonly found that some air-supply vents do not supply the air at their specified rate, vents may be blocked and fail to deliver any air, and/or negative pressure rooms are being operated in a positive pressure mode.
Most recently, a study using computational fluid dynamical modelling confirmed that the air exchange rate and airflow patterns are important factors in the control of airborne virus diffusion.155 Also, despite the recommendations for ceiling to floor level ventilation air flows, this study suggested that this arrangement results in an ‘up-draft effect and poor infection control efficiency’.147, 155 There is an obvious need for further work to determine the optimal methods of ventilation control to reduce the risk of aerosol transmission in healthcare premises.
Conclusions
-
–
Droplets generated by talking, laughing, coughing and sneezing potentially lead to the generation of an infectious aerosol.
-
–
The survival of such aerosolized pathogens depends upon environmental conditions, such as temperature and RH, both of which can vary with the season and the indoor building environment.
-
–
Such aerosols can be transmitted over short and long distances. Short-range transmission occurs over a distance of <1 m between individuals and is mediated mainly by the interaction of breathing zones of individuals. Long-range transmission occurs between distant locations and is primarily governed by air flows driven by pressure differences generated by ventilation systems, open windows and doors, movement of people or temperature differences.
-
–
Agents able to transmit infection over long distances can almost always transmit infection over short ranges and through direct contact. In addition, large droplets may become small droplets then droplet nuclei via the process of evaporation. This may explain why some infectious agents, normally only associated with short-range transmission, may occasionally cause outbreaks over greater distances.
-
–
Whether an individual acquires an infection depends on the final inhaled pathogen dose and the host's immune response.
-
–The airborne transmission of diseases may be restricted in three ways:
-
–control the source of infection by quarantine and the use of isolation facilities;
-
–control airborne transmission routes by the use of negative pressure ventilation systems, sliding doors instead of hinged doors, and improving seals around doors and windows; and
-
–protect exposed susceptible individuals from both aerosol and contact transmission of infection by the use of PPE.
-
–
Search strategy and selection criteria
Data for this review were identified by searches of Medline, references from relevant articles and books, and the authors' own extensive archives. Search terms included: ‘aerosol transmission’, ‘airborne transmission’, ‘environmental survival’, ‘aerosol suspension’, ‘airborne suspension’, ‘aerosol dispersal’, ‘airborne dispersal’, ‘aerosol dispersion’, ‘airborne dispersion’, ‘infectious dose’, ‘nosocomial airborne infection’, ‘nosocomial airborne transmission’, ‘nosocomial aerosol infection’ and ‘nosocomial aerosol transmission’.
Acknowledgements
The authors wish to thank Prof. Andrew Davidhazy (School of Photographic Arts and Sciences, Rochester Institute of Technology Rochester, NY, USA) and Blackwell Publishing for their kind permission to reproduce the photographs in Figure 1, Figure 2, respectively, and CSIRO Australia for the use of the figures in Figure 6(a) and 6(b).
References
- 1.Wong T.W., Lee C.K., Tam W. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerg Infect Dis. 2004;10:269–276. doi: 10.3201/eid1002.030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu I.T., Wong T.W., Chiu Y.L. Temporal-spatial analysis of severe acute respiratory syndrome among hospital inpatients. Clin Infect Dis. 2005;40:1237–1243. doi: 10.1086/428735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y., Huang X., Yu I.T. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air. 2005;15:83–95. doi: 10.1111/j.1600-0668.2004.00317.x. [DOI] [PubMed] [Google Scholar]
- 4.Yu I.T.S., Li Y., Wong T.W. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med. 2004;350:1731–1739. doi: 10.1056/NEJMoa032867. [DOI] [PubMed] [Google Scholar]
- 5.Li Y., Duan S., Yu I.T. Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air. 2005;15:96–111. doi: 10.1111/j.1600-0668.2004.00318.x. [DOI] [PubMed] [Google Scholar]
- 6.Hemmes J.H., Winkler K.C., Kool S.M. Virus survival as a seasonal factor in influenza and poliomyelitis. Nature. 1960;188:430–431. doi: 10.1038/188430a0. [DOI] [PubMed] [Google Scholar]
- 7.Riley E.C., Murphy G., Riley R.L. Airborne spread of measles in a surburban elementary school. Am J Epidemiol. 1978;107:421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- 8.Gwaltney J.M., Jr. Epidemiology of the common cold. Ann NY Acad Sci. 1980;353:54–60. doi: 10.1111/j.1749-6632.1980.tb18905.x. [DOI] [PubMed] [Google Scholar]
- 9.Gregg M.B. The epidemiology of influenza in humans. Ann NY Acad Sci. 1980;353:45–53. doi: 10.1111/j.1749-6632.1980.tb18904.x. [DOI] [PubMed] [Google Scholar]
- 10.Knight V. Viruses as agents of airborne contagion. Ann NY Acad Sci. 1980;353:147–156. doi: 10.1111/j.1749-6632.1980.tb18917.x. [DOI] [PubMed] [Google Scholar]
- 11.Hammond G.W., Raddatz R.L., Gelskey D.E. Impact of atmospheric dispersion and transport of viral aerosols on the epidemiology of influenza. Rev Infect Dis. 1989;11:494–497. doi: 10.1093/clinids/11.3.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldmann D.A. Transmission of viral respiratory infections in the home. Pediatr Infect Dis J. 2000;19:S97–S102. doi: 10.1097/00006454-200010001-00002. [DOI] [PubMed] [Google Scholar]
- 13.Goldmann D.A. Epidemiology and prevention of pediatric viral respiratory infections in health-care institutions. Emerg Infect Dis. 2001;7:249–253. doi: 10.3201/eid0702.010220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aitken C., Jeffries D.J. Nosocomial spread of viral disease. Clin Microbiol Rev. 2001;14:528–546. doi: 10.1128/CMR.14.3.528-546.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marks P.J., Vipond I.B., Regan F.M. A school outbreak of Norwalk-like virus: evidence for airborne transmission. Epidemiol Infect. 2003;131:727–736. doi: 10.1017/s0950268803008689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myatt T.A., Johnston S.L., Rudnick S. Airborne rhinovirus detection and effect of ultraviolet irradiation on detection by a semi-nested RT-PCR assay. BMC Public Health. 2003;3:5–11. doi: 10.1186/1471-2458-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leclair J.M., Zaia J.A., Levin M.J. Airborne transmission of chickenpox in a hospital. N Engl J Med. 1980;302:450–453. doi: 10.1056/NEJM198002213020807. [DOI] [PubMed] [Google Scholar]
- 18.Josephson A., Gombert M.E. Airborne transmission of nosocomial varicella from localized zoster. J Infect Dis. 1988;158:238–241. doi: 10.1093/infdis/158.1.238. [DOI] [PubMed] [Google Scholar]
- 19.Sawyer M.H., Chamberlain C.J., Wu Y.N., Aintablian N., Wallace M.R. Detection of varicella-zoster DNA in air samples from hospital rooms. J Infect Dis. 1994;169:91–94. doi: 10.1093/infdis/169.1.91. [DOI] [PubMed] [Google Scholar]
- 20.Asano Y., Yoshikawa T., Ihira M. Spread of varicella zoster DNA to family members and environments from siblings with varicella in a household. Pediatrics. 1999;103:e61. doi: 10.1542/peds.103.5.e61. [DOI] [PubMed] [Google Scholar]
- 21.Asano Y., Yoshikawa T., Kanematsu M. Rapid contamination with varicella zoster virus DNA to the throat of a daycare attendee and environmental surfaces from a child with varicella. Pediatr Int. 1999;41:233–236. doi: 10.1046/j.1442-200x.1999.4121049.x. [DOI] [PubMed] [Google Scholar]
- 22.Yoshikawa T., Ihira M., Suzuki K. Rapid contamination of the environment with varicella zoster virus DNA from a patient with herpes zoster. J Med Virol. 2001;63:64–66. [PubMed] [Google Scholar]
- 23.Suzuki K., Yoshikawa T., Tomitaka A. Detection of varicella zoster virus DNA in throat swabs of patients with herpes zoster and on air purifier filters. J Med Virol. 2002;66:567–570. doi: 10.1002/jmv.2182. [DOI] [PubMed] [Google Scholar]
- 24.Suzuki K., Yoshikawa T., Tomitaka A. Detection of aerosolized varicella-zoster virus DNA in patients with localized herpes zoster. J Infect Dis. 2004;189:1009–1012. doi: 10.1086/382029. [DOI] [PubMed] [Google Scholar]
- 25.Fraser DW. Legionellosis: evidence of airborne transmission. Ann NY Acad Sci. 1980;353:61–66. doi: 10.1111/j.1749-6632.1980.tb18906.x. [DOI] [PubMed] [Google Scholar]
- 26.Kaufmann A.F., Fox M.D., Boyce J.M. Airborne spread of brucellosis. Ann NY Acad Sci. 1980;353:105–114. doi: 10.1111/j.1749-6632.1980.tb18912.x. [DOI] [PubMed] [Google Scholar]
- 27.Brachman P.S. Inhalation anthrax. Ann NY Acad Sci. 1980;353:83–93. doi: 10.1111/j.1749-6632.1980.tb18910.x. [DOI] [PubMed] [Google Scholar]
- 28.Kelsen S.G., McGuckin M. The role of airborne bacteria in the contamination of fine particle nebulizers and the development of nosocomial pneumonia. Ann NY Acad Sci. 1980;353:218–229. doi: 10.1111/j.1749-6632.1980.tb18925.x. [DOI] [PubMed] [Google Scholar]
- 29.Bovallius A., Roffey R., Henningson E. Long-range transmission of bacteria. Ann NY Acad Sci. 1980;353:186–200. doi: 10.1111/j.1749-6632.1980.tb18922.x. [DOI] [PubMed] [Google Scholar]
- 30.McDonald L.C., Walker M., Carson L. Outbreak of Acinetobacter spp. bloodstream infections in a nursery associated with contaminated aerosols and air conditioners. Pediatr Infect Dis J. 1998;17:716–722. doi: 10.1097/00006454-199808000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Uduman S.A., Farrukh A.S., Nath K.N.R. An outbreak of Serratia marcescens infection in a special-care baby unit of a community hospital in United Arab Emirates: the importance of the air conditioner duct as a nosocomial reservoir. J Hosp Infect. 2002;52:175–180. doi: 10.1053/jhin.2002.1308. [DOI] [PubMed] [Google Scholar]
- 32.Dull P.M., Wilson K.E., Kournikakis B. Bacillis anthracis aerosolization associated with a contaminated mail sorting machine. Emerg Infect Dis. 2002;8:1044–1047. doi: 10.3201/eid0810.020356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fennelly K.P., Davidow A.L., Miller S.L. Airborne infection with Bacillus anthracis – from mills to mail. Emerg Infect Dis. 2004;10:996–1001. doi: 10.3201/eid1006.020738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Houk V.N. Spread of tuberculosis via recirculated air in a naval vessel. The Byrd study. Ann NY Acad Sci. 1980;353:10–24. doi: 10.1111/j.1749-6632.1980.tb18901.x. [DOI] [PubMed] [Google Scholar]
- 35.Hutton M.D., Stead W.W., Cauthen G.M. Nosocomial transmission of tuberculosis associated with a draining abscess. J Infect Dis. 1990;161:286–295. doi: 10.1093/infdis/161.2.286. [DOI] [PubMed] [Google Scholar]
- 36.Nardell E.A. Nosocomial tuberculosis in the AIDS era: strategies for interrupting transmission in developed countries. Bull Int Union Tuberc Lung Dis. 1991;66:107–111. [PubMed] [Google Scholar]
- 37.Rutala W.A., Jones S.M., Worthington J.M. Efficacy of portable filtration units in reducing aerosolized particles in the size range of Mycobacterium tuberculosis. Infect Control Hosp Epidemiol. 1995;16:391–398. doi: 10.1086/647136. [DOI] [PubMed] [Google Scholar]
- 38.Miller–Leiden S., Lobascio C., Nazaroff W.W. Effectiveness of in-room air filtration and dilution ventilation for tuberculosis infection control. J Air Waste Manag Assoc. 1996;46:869–882. doi: 10.1080/10473289.1996.10467523. [DOI] [PubMed] [Google Scholar]
- 39.Nicas M. Refining a risk model for occupational tuberculosis transmission. Am Ind Hyg Assoc J. 1996;57:16–22. doi: 10.1080/15428119691015179. [DOI] [PubMed] [Google Scholar]
- 40.Hannan M.M., Azadian B.S., Gazzard B.G. Hospital infection control in an era of HIV infection and multi-drug resistant tuberculosis. J Hosp Infect. 2000;44:5–11. doi: 10.1053/jhin.1999.0651. [DOI] [PubMed] [Google Scholar]
- 41.Beggs C.B., Noakes C.J., Sleigh P.A. The transmission of tuberculosis in confirmed spaces: an analytical review of alternative epidemiological models. Int J Tuberc Lung Dis. 2003;7:1015–1026. [PubMed] [Google Scholar]
- 42.Ko G., Thompson K.M., Nardell E.A. Estimation of tuberculosis risk on a commercial airliner. Risk Anal. 2004;24:379–388. doi: 10.1111/j.0272-4332.2004.00439.x. [DOI] [PubMed] [Google Scholar]
- 43.Aylor D.E., Waggoner P.E. Aerial dissemination of fungal spores. Ann NY Acad Sci. 1980;353:116–122. [Google Scholar]
- 44.Herman L.G. Aspergillus in patient care areas. Ann NY Acad Sci. 1980;353:140–146. doi: 10.1111/j.1749-6632.1980.tb18916.x. [DOI] [PubMed] [Google Scholar]
- 45.Campbell C.C. (Philosophical) review of air currents as a continuing vector. Ann NY Acad Sci. 1980;353:123–139. doi: 10.1111/j.1749-6632.1980.tb18915.x. [DOI] [PubMed] [Google Scholar]
- 46.Ayliffe G.A.J., Babb J.R., Taylor L.J. 3rd edn. Arnold; London: 2001. Hospital-acquired infection. Principles and prevention. [Google Scholar]
- 47.Srinivasan A., Beck C., Buckley T. The ability of hospital ventilation systems to filter Aspergillus and other fungi following a building implosion. Infect Control Hosp Epidemiol. 2002;239:520–524. doi: 10.1086/502100. [DOI] [PubMed] [Google Scholar]
- 48.Hahn T., Cummings K.M., Michalek A.M. Efficacy of high-efficiency particulate air filtration in preventing aspergillosis in immunocompromised patients with hematologic malignancies. Infect Control Hosp Epidemiol. 2002;23:525–531. doi: 10.1086/502101. [DOI] [PubMed] [Google Scholar]
- 49.Cooper E.E., O'Reilly M.A., Guest D.I. Influence of building construction work on aspergillus infection in a hospital setting. Infect Control Hosp Epidemiol. 2003;24:472–476. doi: 10.1086/502239. [DOI] [PubMed] [Google Scholar]
- 50.Engelhart S., Hanfland J., Glasmacher A. Impact of portable air filtration units on exposure of haematology-oncology patients to airborne Aspergillus fumigatus spores under field conditions. J Hosp Infect. 2003;54:300–304. doi: 10.1016/s0195-6701(03)00176-2. [DOI] [PubMed] [Google Scholar]
- 51.Lutz B.D., Jin J., Rinaldi M.G. Outbreak of invasive aspergillus infection in surgical patients, associated with a contaminated air-handling system. Clin Infect Dis. 2003;37:786–793. doi: 10.1086/377537. [DOI] [PubMed] [Google Scholar]
- 52.Humphreys H. Positive-pressure isolation and the prevention of invasive aspergillosis. What is the evidence? J Hosp Infect. 2004;56:93–100. doi: 10.1016/j.jhin.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 53.Hensley M.E., Ke W., Hayden R.T. Levels of total fungus and aspergillus on a pediatric hematopoietic stem cell transplant unit. J Pediatr Oncol Nurs. 2004;21:67–78. doi: 10.1177/1043454203262696. [DOI] [PubMed] [Google Scholar]
- 54.Heinemann S., Symoens F., Gordts B. Environmental investigations and molecular typing of Aspergillus flavus during an outbreak of postoperative infections. J Hosp Infect. 2004;57:149–155. doi: 10.1016/j.jhin.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 55.Munoz P., Guinea J., Pelaez T. Nosocomial invasive aspergillosis in a heart transplant patient acquired during a break in the HEPA air filtration system. Transpl Infect Dis. 2004;6:50–54. doi: 10.1111/j.1399-3062.2004.00047.x. [DOI] [PubMed] [Google Scholar]
- 56.Pini G., Donato R., Faggi E. Two years of a fungal aerobiocontamination survey in a Florentine haematology ward. Eur J Epidemiol. 2004;19:693–698. doi: 10.1023/b:ejep.0000036778.13006.16. [DOI] [PubMed] [Google Scholar]
- 57.Beggs C.B. The airborne transmission of infection in hospital buildings: fact or fiction? Indoor Built Environ. 2003;12:9–19. [Google Scholar]
- 58.Kundsin R.B. Documentation of airborne infection during surgery. Ann NY Acad Sci. 1980;353:255–262. doi: 10.1111/j.1749-6632.1980.tb18928.x. [DOI] [PubMed] [Google Scholar]
- 59.Hambraeus A. Aerobiology in the operating room – a review. J Hosp Infect. 1988;11(Suppl. A):68–76. doi: 10.1016/0195-6701(88)90169-7. [DOI] [PubMed] [Google Scholar]
- 60.Holton J., Ridgway G.L., Reynoldson A.J. A microbiologists view of commissioning operating theatres. J Hosp Infect. 1990;16:29–34. doi: 10.1016/0195-6701(90)90046-q. [DOI] [PubMed] [Google Scholar]
- 61.Ayliffe G.A.J. Role of the environment of the operating suite in surgical wound infection. Rev Infect Dis. 1991;13(Suppl. 10):S800–S804. doi: 10.1093/clinids/13.supplement_10.s800. [DOI] [PubMed] [Google Scholar]
- 62.Whyte W., Hambraeus A., Laurell G. The relative importance of the routes and sources of wound contamination during general surgery. II. Airborne. J Hosp Infect. 1992;22:41–54. doi: 10.1016/0195-6701(92)90129-a. [DOI] [PubMed] [Google Scholar]
- 63.NHS Estates; 1994. Hospital Technical Memorandum (HTM) 2025. (Ventilation of healthcare premises). [Google Scholar]
- 64.Holton J., Ridgway G.L. Commissioning operating theatres. J Hosp Infect. 1993;23:153–160. doi: 10.1016/0195-6701(93)90019-v. [DOI] [PubMed] [Google Scholar]
- 65.Gundermann K.O. Spread of microorganisms by air-conditioning systems – especially in hospitals. Ann NY Acad Sci. 1980;353:209–217. doi: 10.1111/j.1749-6632.1980.tb18924.x. [DOI] [PubMed] [Google Scholar]
- 66.Li Y, Leung G, Tang JW, et al. Role of ventilation in airborne transmission of infectious agents in the built environment – a multidisciplinary systematic review. Indoor Air; in press. [DOI] [PubMed]
- 67.Hambraeus A., Laurell G. Infections in a burns unit. An attempt to study the airborne transfer of bacteria. Contrib Microbiol Immunol. 1973;1:459–468. [PubMed] [Google Scholar]
- 68.Demling R.H., Maly J. The treatment of burn patients in a laminar airflow environment. Ann NY Acad Sci. 1980;353:294–299. doi: 10.1111/j.1749-6632.1980.tb18932.x. [DOI] [PubMed] [Google Scholar]
- 69.Behringer G.E., Burke J.F. The contribution of a bacterially isolated environment to the prevention of infections in seriously burned patients. Ann NY Acad Sci. 1980;353:300–307. doi: 10.1111/j.1749-6632.1980.tb18933.x. [DOI] [PubMed] [Google Scholar]
- 70.Bauer T.M., Ofner E., Just H.M. An epidemiological study assessing the relative importance of airborne and direct contact transmission of microorganisms in a medical intensive care unit. J Hosp Infect. 1990;15:301–309. doi: 10.1016/0195-6701(90)90087-5. [DOI] [PubMed] [Google Scholar]
- 71.Gilmour I.J., Boyle M.J., Streifel A. The effects of circuit and humidifier type on contamination potential during mechanical ventilation: a laboratory study. Am J Infect Control. 1995;23:65–72. doi: 10.1016/0196-6553(95)90096-9. [DOI] [PubMed] [Google Scholar]
- 72.Somogyi R., Vesely A.E., Azami T. Dispersal of respiratory droplets with open vs closed oxygen delivery masks: implications for the transmission of severe acute respiratory syndrome. Chest. 2004;125:1155–1157. doi: 10.1378/chest.125.3.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hui DS, Ip M, Tang JW, et al. Airflows around oxygen masks: a potential source of infection? Chest; in press. [DOI] [PMC free article] [PubMed]
- 74.Shpuntoff H., Shpuntoff R.L. High-speed dental handpieces and spread of airborne infections. N Y State Dent J. 1993;59:21–23. [PubMed] [Google Scholar]
- 75.Miller R.L. Characteristics of blood-containing aerosols generated by common powered dental instruments. Am Ind Hyg Assoc J. 1995;56:670–676. doi: 10.1080/15428119591016683. [DOI] [PubMed] [Google Scholar]
- 76.Barnes J.B., Harrel S.K., Rivera-Hidalgo F. Blood contamination of the aerosols produced by in vivo use of ultrasonic scalers. J Periodontol. 1998;69:434–438. doi: 10.1902/jop.1998.69.4.434. [DOI] [PubMed] [Google Scholar]
- 77.Harrel S.K., Molinari J. Aerosols and splatter in dentistry. JADA. 2004;135:429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Johnson G.K., Robinson W.S. Human immunodeficiency virus-1 (HIV-1) in the vapors of surgical power instruments. J Med Virol. 1991;33:47–50. doi: 10.1002/jmv.1890330110. [DOI] [PubMed] [Google Scholar]
- 79.Heinsohn P., Jewett D.L. Exposure to blood-containing aerosols in the operating room: a preliminary study. Am Ind Hyg Assoc J. 1993;54:446–453. doi: 10.1080/15298669391354946. [DOI] [PubMed] [Google Scholar]
- 80.Jewett D.L., Heinsohn P., Bennett C. Blood-containing aerosols generated by surgical techniques: a possible infectious hazard. Am Ind Hyg Assoc J. 1992;53:228–231. doi: 10.1080/15298669291359564. [DOI] [PubMed] [Google Scholar]
- 81.Nogler M., Lass-Florl C., Wimmer C. Aerosols produced by high-speed cutters in cervical spine surgery: extent of environmental contamination. Eur Spine J. 2001;10:274–277. doi: 10.1007/s005860100310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nogler M., Lass-Florl C., Ogon M. Environmental and body contamination through aerosols produced by high-speed cutters in lumbar spine surgery. Spine. 2001;26:2156–2159. doi: 10.1097/00007632-200110010-00023. [DOI] [PubMed] [Google Scholar]
- 83.Nogler M., Lass-Florl C., Wimmer C. Contamination during removal of cement in revision hip arthroplasty. A cadaver study using ultrasound and high-speed cutters. J Bone Joint Surg Br. 2003;85:436–439. doi: 10.1302/0301-620x.85b3.12451. [DOI] [PubMed] [Google Scholar]
- 84.Wong K.C., Leung K.S. Transmission and prevention of occupational infections in orthopaedic surgeons. J Bone Joint Surg Am. 2004;86-A:1065–1076. doi: 10.2106/00004623-200405000-00029. [DOI] [PubMed] [Google Scholar]
- 85.Bausam H.T., Schaub S.A., Kenyon K.F., Small M.J. Comparison of coliphage and bacterial aerosols at a wastewater spray irrigation site. Appl Environ Microbiol. 1982;43:28–38. doi: 10.1128/aem.43.1.28-38.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baylor E.R., Baylor M.B. Surf-to-wind transfer of viruses. Ann NY Acad Sci. 1980;353:201–208. doi: 10.1111/j.1749-6632.1980.tb18923.x. [DOI] [PubMed] [Google Scholar]
- 87.Gerba C.P., Wallis C., Melnick J.L. Microbiological hazards of household toilets: droplet production and the fate of residual organisms. Appl Microbiol. 1975;30:229–237. doi: 10.1128/am.30.2.229-237.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tang J.W., Eames I., Li Y. Door-opening motion can potentially lead to a transient breakdown in negative-pressure isolation conditions: the importance of vorticity and buoyancy airflows. J Hosp Infect. 2005;61:283–286. doi: 10.1016/j.jhin.2005.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Centers for Disease Control and Prevention Guidelines for environmental infection control in health-care facilities. MMWR Morb Mortal Wkly Rep. 2003;52 RR–10. [Google Scholar]
- 90.Heymann D.L., editor. Control of communicable diseases manual. 18th edn. American Public Health Association; Washington: 2004. [Google Scholar]
- 91.Hinds W.C. John Wiley & Sons; New York: 1982. Aerosol technology. [Google Scholar]
- 92.Wells W.F. On air-borne infection. II. Droplets and droplet nuclei. Am J Hyg. 1934;20:611–618. [Google Scholar]
- 93.Fennelly K.P., Martyny J.W., Fulton K.E., Orme I.M., Cave D.M., Heifets L.B. Cough-generated aerosols of Mycobacterium tuberculosis: a new method to study infectiousness. Am J Respir Crit Care Med. 2004;169:604–609. doi: 10.1164/rccm.200308-1101OC. [DOI] [PubMed] [Google Scholar]
- 94.Bjorn E., Nielsen P.V. Dispersal of exhaled air and personal exposure in displacement ventilated room. Indoor Air. 2002;12:147–164. doi: 10.1034/j.1600-0668.2002.08126.x. [DOI] [PubMed] [Google Scholar]
- 95.Booth T.F., Kournikakis B., Bastien N. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis. 2005;191:1472–1477. doi: 10.1086/429634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xiao W.J., Wang M.L., Wei W. Detection of SARS-CoV and RNA on aerosol samples from SARS-patients admitted to hospitalZhonghua Liu Xing Bing Xue Za Zhi. 2004;25:882–885. [in Chinese] [PubMed] [Google Scholar]
- 97.Wong S.S., Yuen K.Y. Avian influenza virus infections in humans. Chest. 2006;129:156–168. doi: 10.1378/chest.129.1.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Health Protection Agency . Department of Health; London: 2005. Guidance for pandemic influenza: infection control in hospitals and primary care settings. [Google Scholar]
- 99.Ferguson N.M., Cummings D.A., Cauchemez S. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437:209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 100.Mills C.E., Robins J.M., Lipsitch M. Transmissibility of 1918 pandemic influenza. Nature. 2004;432:904–906. doi: 10.1038/nature03063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fraser C., Riley S., Anderson R.M., Ferguson N.M. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101:6146–6151. doi: 10.1073/pnas.0307506101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mims C., Playfair J., Roitt I., Wakelin D., Williams R., editors. Epidemiologic aspects of the control of infection and disease. In: Medical microbiology. 2nd edn. Mosby; London: 1998. pp. 467–480. [Google Scholar]
- 103.Anderson R.M., May R.M. Oxford University Press; Oxford: 1992. Infectious diseases of humans. [Google Scholar]
- 104.Lipsitch M., Cohen T., Cooper B. Transmission dynamics and control of severe acute respiratory syndrome. Science. 2003;300:1966–1970. doi: 10.1126/science.1086616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Riley S., Fraser C., Donnelly C.A. Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions. Science. 2003;300:1961–1966. doi: 10.1126/science.1086478. [DOI] [PubMed] [Google Scholar]
- 106.Ayliffe G.A.J., Babb J.R., Taylor L.J., editors. Hospital-acquired infection. Principles and prevention. 3rd edn. Arnold; London: 2001. [Google Scholar]
- 107.Cole E.C., Cook C.E. Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies. Am J Infect Control. 1998;26:453–464. doi: 10.1016/S0196-6553(98)70046-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wells W.F. Harvard University Press; Cambridge: 1955. Airborne contagion and air hygiene. [Google Scholar]
- 109.Lim P.L., Kurup A., Gopalakrishna G. Laboratory-acquired severe acute respiratory syndrome. N Engl J Med. 2004;350:1740–1745. doi: 10.1056/NEJMoa032565. [DOI] [PubMed] [Google Scholar]
- 110.Meselson M., Guillemin J., Hugh-Jones M. The Sverdlovsk anthrax outbreak of 1979. Science. 1994;266:1202–1208. doi: 10.1126/science.7973702. [DOI] [PubMed] [Google Scholar]
- 111.Fitzgerald D., Haas D.W. Mycobacterium tuberculosis. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and practice of infectious diseases. 6th edn. Churchill Livingstone; Philadelphia: 2005. pp. 2852–2886. [Google Scholar]
- 112.Edwards D.A., Man J.C., Brand P. Inhaling to mitigate exhaled bioaerosols. Proc Natl Acad Sci U S A. 2004;101:17383–17388. doi: 10.1073/pnas.0408159101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lew T.W., Kwek T.K., Tai D. Acute respiratory distress syndrome in critically ill patients with severe acute respiratory syndrome. JAMA. 2003;16:374–380. doi: 10.1001/jama.290.3.374. [DOI] [PubMed] [Google Scholar]
- 114.Manocha S., Walley K.R., Russell J.A. Severe acute respiratory distress syndrome (SARS): a critical care perspective. Crit Care Med. 2003;31:2684–2692. doi: 10.1097/01.CCM.0000091929.51288.5F. [DOI] [PubMed] [Google Scholar]
- 115.Fowler R.A., Lapinsky S.E., Hallett D. Critically ill patients with severe acute respiratory syndrome. JAMA. 2003;290:367–373. doi: 10.1001/jama.290.3.367. [DOI] [PubMed] [Google Scholar]
- 116.Lapinsky S.E., Hawryluck L. ICU management of severe acute respiratory syndrome. Intensive Care Med. 2003;29:870–905. doi: 10.1007/s00134-003-1821-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kiel D.E., Wilson D.J. Combining door swing pumping with density driven flow. ASHRAE Trans. 1989;95:590–599. [Google Scholar]
- 118.Wilson D.J., Kiel D.E. Gravity driven counterflow through an open door in a sealed room. Build Environ. 1990;25:379–388. [Google Scholar]
- 119.Bush J.W.M., Eames I. Fluid displacement by bubbles rising in a thin gap. Int J Multiphase Flow. 1998;24:411–430. [Google Scholar]
- 120.Cox C.S. The microbiology of air. In: Collier L., Balows A., Sussman M., editors. Topley & Wilson's microbiology and microbial infections. 9th edn. Arnold, Oxford University Press; London: 1998. pp. 339–350. [Google Scholar]
- 121.Goldner J.L., Moggio M., Beissinger S.F., McCollum D.E. Ultraviolet light for the control of airborne bacteria in the operating room. Ann NY Acad Sci. 1980;353:271–284. doi: 10.1111/j.1749-6632.1980.tb18930.x. [DOI] [PubMed] [Google Scholar]
- 122.Lowell J.D., Kundsin R.B., Schwartz C.M., Pozin D. Ultraviolet radiation and reduction of deep wound infection following hip and knee arthroplasty. Ann NY Acad Sci. 1980;353:285–293. doi: 10.1111/j.1749-6632.1980.tb18931.x. [DOI] [PubMed] [Google Scholar]
- 123.Lidwell O.M. Ultraviolet radiation and the control of airborne contamination in the operating room. J Hosp Infect. 1994;28:245–248. doi: 10.1016/0195-6701(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 124.Riley R.L. Prevention and control of airborne infection in the community. Ann NY Acad Sci. 1980;353:331–339. doi: 10.1111/j.1749-6632.1980.tb18936.x. [DOI] [PubMed] [Google Scholar]
- 125.Stephenson E.H., Larson E.W., Dominik J.W. Effect of environmental factors on aerosol-induced Lassa virus infection. J Med Virol. 1984;14:295–303. doi: 10.1002/jmv.1890140402. [DOI] [PubMed] [Google Scholar]
- 126.Ijaz M.K., Brunner A.H., Sattar S.A. Survival characteristics of airborne human coronavirus 229E. J Gen Virol. 1985;66:2743–2748. doi: 10.1099/0022-1317-66-12-2743. [DOI] [PubMed] [Google Scholar]
- 127.Bean B., Moore B.M., Sterner B. Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146:47–51. doi: 10.1093/infdis/146.1.47. [DOI] [PubMed] [Google Scholar]
- 128.Lai M.Y., Cheng P.K., Lim W.W. Survival of severe acute respiratory syndrome coronavirus. Clin Infect Dis. 2005;41:e67–e71. doi: 10.1086/433186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dinter P.S., Muller W. The tenacity of bacteria in the airborne state. VI Tenacity of airborne S. senftenberg. Zentralbl Bakteriol Mikrobiol Hyg. 1988;186:278–288. [PubMed] [Google Scholar]
- 130.NHS Estates; 1994. Hospital Technical Memorandum (HTM) 2025. (Ventilation of healthcare premises). [Google Scholar]
- 131.Holton J., Ridgway G.L. Commissioning operating theatres. J Hosp Infect. 1993;23:153–160. doi: 10.1016/0195-6701(93)90019-v. [DOI] [PubMed] [Google Scholar]
- 132.Franz D.R., Jahrling P.B., Friedlander A.M. Clinical recognition and management of patients exposed to biological warfare agents. JAMA. 1997;278:399–411. doi: 10.1001/jama.278.5.399. [DOI] [PubMed] [Google Scholar]
- 133.Bloch A.B., Orenstein W.A., Ewing W.M. Measles outbreak in a pediatric practice: airborne transmission in an office setting. Pediatrics. 1985;75:676–683. [PubMed] [Google Scholar]
- 134.Gustafson T.L., Lavely G.B., Brawner E.R., Jr. An outbreak of airborne nosocomial varicella. Pediatrics. 1982;70:550–556. [PubMed] [Google Scholar]
- 135.Hoge C.W., Reichler M.R., Dominguez E.A. An epidemic of pneumococcal disease in an overcrowded, inadequately ventilated jail. N Engl J Med. 1994;331:643–648. doi: 10.1056/NEJM199409083311004. [DOI] [PubMed] [Google Scholar]
- 136.Menzies D., Fanning A., Yuan L. Hospital ventilation and risk for tuberculous infection in Canadian health care workers. Ann Intern Med. 2000;133:779–789. doi: 10.7326/0003-4819-133-10-200011210-00010. [DOI] [PubMed] [Google Scholar]
- 137.Riley R.L., Mills C.C., O'Grady F. Infectiousness of air from a tuberculosis ward: ultraviolet irradiation of infected air: comparative infectiousness of different patients. Am Rev Respir Dis. 1962;85:511–525. doi: 10.1164/arrd.1962.85.4.511. [DOI] [PubMed] [Google Scholar]
- 138.Moser M.R., Bender T.R., Margolis H.S. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110:1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 139.Schulman J.L., Kilbourne E.D. Airborne transmission of influenza virus infection in mice. Nature. 1962;195:1129–1130. doi: 10.1038/1951129a0. [DOI] [PubMed] [Google Scholar]
- 140.Wehrle P.F., Posch J., Richter K.H. An airborne outbreak of smallpox in a German hospital and its significance with respect to other recent outbreaks in Europe. Bull World Health Organ. 1970;43:669–679. [PMC free article] [PubMed] [Google Scholar]
- 141.Seto W.H., Tsang D., Yung R.W. Advisors of expert SARS group of Hospital Authority. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Holmberg S., Li Y. Modelling of indoor environment – particle dispersion and deposition. Indoor Air. 1998;8:113–122. [Google Scholar]
- 143.Leung G.M., Lam T.H., Ho L.M. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. 2003;57:857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lo J.Y., Tsang T.H., Leung Y.H. Respiratory infections during SARS outbreak, Hong Kong, 2003. Emerg Infect Dis. 2005;11:1738–1741. doi: 10.3201/eid1111.050729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Etheridge D., Sandberg M. John Wiley & Sons; Chichester: 1996. Building ventilation – theory and measurement. [Google Scholar]
- 146.Janssen J.E. The history of ventilation and temperature control. ASHRAE J. 1999;10:47–52. [Google Scholar]
- 147.Centers for Disease Control and Prevention Guidelines for preventing transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Morb Mortal Wkly Rep. 2005;54 RR–17. [PubMed] [Google Scholar]
- 148.Linden P.F. The fluid mechanics of natural ventilation. Ann Rev Fluid Mech. 1999;31:201–238. [Google Scholar]
- 149.Qian H., Li Y., Nielsen P.V. Dispersion of exhaled droplet nuclei in a two-bed hospital ward with three different ventilation systems. Indoor Air. 2006;16:111–128. doi: 10.1111/j.1600-0668.2005.00407.x. [DOI] [PubMed] [Google Scholar]
- 150.ASHRAE Handbook . Fundamentals (SI ed.): thermal comfort. American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), Inc.; Atlanta: 2001. p. 8.1–8.29. [Google Scholar]
- 151.Guidelines for design and construction of hospital and health care facilities, 1996–97. American Institute of Architects Press; Washington: 1996. American Institute of Architects. [Google Scholar]
- 152.ASHRAE Handbook . HVAC applications (SI ed.): health care facilities. American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), Inc.; Atlanta: 2003. p. 7.1–7.14. [Google Scholar]
- 153.Department of Human Services . Standing Committee on Infection Control, Department of Human Services; Victoria, Australia: 1999. Guidelines for the classification and design of isolation rooms in health care facilities. [Google Scholar]
- 154.Health Canada Guidelines for preventing the transmission of tuberculosis in Canadian health care facilities and other institutional settings – IVE. Engineering controls to minimize TB transmission. Can Commun Dis Rep. 1996;22S1 [PubMed] [Google Scholar]
- 155.Kao P.H., Yang R.J. Virus diffusion in isolation rooms. J Hosp Infect. 2006;62:338–345. doi: 10.1016/j.jhin.2005.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]


