Summary
Background
Since the first case of Middle East respiratory syndrome coronavirus (MERS-CoV) in South Korea was reported on 20th May 2015, there have been 186 confirmed cases, 38 deaths and 16,752 suspected cases. Previously published research on South Korea's MERS outbreak was limited to the early stages, when few data were available. Now that the outbreak has ended, albeit unofficially, a more comprehensive review is appropriate.
Methods
Data were obtained through the MERS portal by the Ministry for Health and Welfare (MOHW) and Korea Centres for Disease Control and Prevention, press releases by MOHW, and reports by the MERS Policy Committee of the Korean Medical Association. Cases were analysed for general characteristics, exposure source, timeline and infection generation. Sex, age and underlying diseases were analysed for the 38 deaths.
Findings
Beginning with the index case that infected 28 others, an in-depth analysis was conducted. The average age was 55 years, which was a little higher than the global average of 50 years. As in most other countries, more men than women were affected. The case fatality rate was 19.9%, which was lower than the global rate of 38.7% and the rate in Saudi Arabia (36.5%). In total, 184 patients were infected nosocomially and there were no community-acquired infections. The main underlying diseases were respiratory diseases, cancer and hypertension. The main contributors to the outbreak were late diagnosis, quarantine failure of ‘super spreaders’, familial care-giving and visiting, non-disclosure by patients, poor communication by the South Korean Government, inadequate hospital infection management, and ‘doctor shopping’. The outbreak was entirely nosocomial, and was largely attributable to infection management and policy failures, rather than biomedical factors.
Keywords: MERS-CoV outbreak, Epidemiology, Public health, South Korea
Introduction
Middle East respiratory syndrome (MERS), first reported in Saudi Arabia in 2012, is becoming an increasing threat to global health security, much like Ebola or swine flu.1 Between March 2012 and 1st November 2015, the World Health Organization (WHO) reported 1611 confirmed cases and 575 deaths worldwide.2 MERS-outbreak countries include Saudi Arabia (1255 cases and 539 deaths), South Korea (185 cases and 36 deaths) and the United Arab Emirates (81 cases and 11 deaths).3
The first case of MERS in South Korea occurred on 20th May 2015 in a 68-year-old male who had contracted the disease while on a business trip to multiple Middle East countries. Subsequently, 186 cases were confirmed, with 38 deaths. In addition, 16,752 suspected cases had a substantial impact on the education, tourism, political and economic sectors.4 Domestic and international media sources attributed the spread of MERS in South Korea to many factors. Reuters reported that South Korea's MERS situation would not be abated without information transparency and cooperation with international virus hunters, pointing out the South Korean Government's refusal to seek help from international parties as particularly troubling.5 Science highlighted problems such as inadequate in-hospital ventilation, extensive transmission caused by unmanaged super spreaders, poor infection control measures, and refusal to disclose the names of hospitals where confirmed cases of MERS had been treated or sought treatment.6 The Korea Centre for Disease Control and Prevention (KCDC) reported that problems with the initial response in South Korea could be attributed to inconsistent definition and isolation of close contacts, subsequent failure to conduct pre-emptive quarantines, and the Government's failure to implement appropriate crisis communication measures.7
In the face of such speculation about the main reasons for the initial failure to contain the MERS outbreak in South Korea, the authors undertook a comprehensive review of the temporal progression of the outbreak and the infection histories of confirmed patients. An overview of worldwide publications on MERS between 1st January 2010 and 31st May 2015 did not include all of the South Korean cases,8 whilst previous reports from South Korea have not reviewed the outbreak comprehensively.7, 9, 10 The main objective of this study was to compare the South Korean experience with that of other countries, including clinical outcomes and infection control processes.
Methods
General characteristics, outbreak sites, and source of exposure of patients diagnosed with MERS
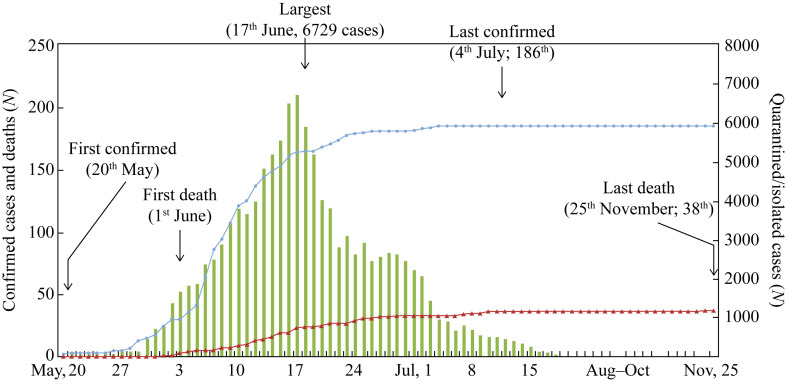
The timeline from the first confirmed MERS case in South Korea, and the first death to the latest death is outlined in Figure 1 . Data were analysed based on the South Korean Government's MERS information portal, and policy briefings officially managed by MOHW and KCDC.11, 12 The official daily briefing reports included patient serial number, day of diagnosis, infection route, sex, age and hospital. The sex and age of all 186 South Korean cases were determined. Outbreaks were defined as occurring in hospital, within the family or in the community. Sources of exposure were divided into three groups: healthcare professionals [doctors, nurses, medical technicians (e.g. radiologists) and medical transport staff]; infections contracted in hospitals by inpatients or outpatients; and infections acquired through visiting hospitalized patients or familial care-giving.
Figure 1.
Number of confirmed cases (blue circles), deaths (red triangles) and quarantines/isolations (green bars) for Middle East respiratory syndrome in South Korea (20th May to 25th November 2015).
Analysis of fatalities in patients with MERS
Thirty-eight deaths were identified via the official daily briefings from MOHW and KCDC. The sex, age and underlying diseases were recorded in these cases. Where patients had multiple underlying diseases, duplicate aggregation was permitted, with each disease treated as one case.
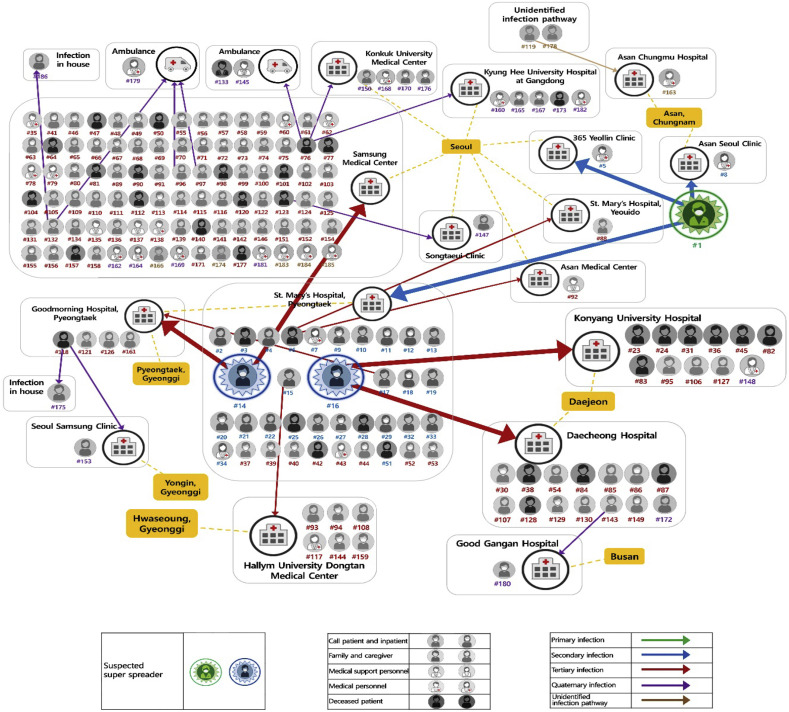
Distribution of transmission of MERS clusters and suspected super spreaders in South Korea
Super-spreading events are found to occur during infectious disease events in which, according to the Pareto principle, 20% of the infected population is the cause of transmitting the disease to the other 80%.13, 14 Three super spreaders were identified in this study: Patient 1, who infected 28 patients at St. Mary's Hospital, Pyeongtaek; Patient 14, who infected 85 patients at Samsung Medical Centre, Seoul; and Patient 16, who infected 23 patients at Konyang University Hospital and Daejeon Hospital.
Results
General characteristics of confirmed MERS cases, outbreak sites and sources of exposure
The 186 MERS cases comprised 111 (59.7%) males and 75 (40.3%) females. Overall, the 50–59-years age group was most affected (22.6% of all cases), followed by the 60–69-years and 70–79-years age groups. Females with MERS tended to be older than males (Table I ). The 186 cases comprised the index case, his wife (infected in the household setting) and 184 nosocomially acquired cases. The most common route of exposure was through hospital visits (including family members who acted as care-givers), which accounted for 103 (55.7%) cases. Fifty-four (29.2%) cases occurred in patients who were hospitalized for other reasons, and 25 (13.5%) cases were occupationally acquired by healthcare workers (Table I).
Table I.
Epidemiological characteristics of Middle East respiratory syndrome (MERS) in South Korea (20th May to 25th November 2015)
| N | % | ||
|---|---|---|---|
| Sex | Total | 186 | 100 |
| Female | 75 | 40.3 | |
| Male | 111 | 59.7 | |
| Age (years) | <19 | 1 | 0.5 |
| 20–29 | 13 | 7.0 | |
| 30–39 | 26 | 14.0 | |
| 40–49 | 29 | 15.6 | |
| 50–59 | 42 | 22.6 | |
| 60–69 | 36 | 19.4 | |
| 70–79 | 30 | 16.1 | |
| 80–89 | 9 | 4.8 | |
| Average age (years) | 55 | - | - |
| Number of cumulative quarantine/isolate cases | 16,693 | ||
| Outbreak sitesa,b | Infection in hospital (including health professionals) |
184 | 99.4 |
| Infection within household | 1 | 0.6 | |
| Infection within communities | 0 | 0 | |
| Route of infection spreada | Infection through medical staff or allied health professionalsc | 28 | 15.1 |
| Infection at hospitals for the purpose of own treatmentd | 54 | 29.2 | |
| Infection due to hospital visits or care-givinge | 103 | 55.7 | |
This analysis targeted 185 cases, excluding the index case.
If a case was infected while providing care to a family member who was admitted while showing symptoms of MERS, this case was classified as an in-hospital infection. It was not possible to determine if the infection occurred during the MERS latent period. In the case of in-hospital infections, 25 medical staff were included.
Including doctors, nurses, medical technologists (e.g. radiologists) and patient transfer personnel in hospitals.
Outpatients or inpatients.
Including hospital visits and care-giving by family member.
Fatality rate and analysis of underlying disease of patients who died of MERS in South Korea
Twenty-six of the 38 fatalities were males; the fatality rate in males (23.4%) was higher than that in females (16.0%). The average age of patients who died was 67.9 years (Table II ). Twenty-nine patients had underlying diseases. The most common underlying diseases were respiratory disorders (11 cases, 30.5%), cancer (11 cases, 28.9%), hypertension (eight cases, 22.2%), cardiovascular diseases (five cases, 13.9%) and diabetes (four cases, 11.1%) (Table III ).
Table II.
Fatality rate of patients who died of Middle East respiratory syndrome (MERS) in South Korea (20th May to 25th October 2015)
| Sex | Total number of deathsa | Fatality rate (%)b | Average age (years) |
|---|---|---|---|
| Total | 38 | 20.4 | 67.9 |
| Male | 26 | 23.4 | 67.2 |
| Female | 12 | 16.0 | 69.6 |
This is the result of an analysis of the underlying diseases of cases that have died from MERS. For cases with multiple underlying diseases, each disease was counted as one case.
(Total number of deaths/total number of cases) × 100.
Table III.
Epidemiological characteristics of 37 deaths from Middle East respiratory syndrome in South Korea (20th May to 25th October 2015)
| Case | Sex | Age (years) | Date of death | Confirmed date | Underlying diseases |
|---|---|---|---|---|---|
| 1 | Female | 57 | 1st June | 1st June | Asthma, hypertension, Cushing's syndrome |
| 2 | Male | 71 | 2nd June | 28th May | COPD, nephrectomy |
| 3 | Male | 82 | 3rd June | 4th June | Asthma, hypertension |
| 4 | Male | 76 | 4th June | 21st May | Cholangiocarcinoma, asthma, COPD |
| 5 | Male | 75 | 5th June | 6th June | Gastric cancer |
| 6 | Female | 68 | 8th June | 6th June | Valvular disease |
| 7 | Male | 80 | 8th June | 7th June | Pneumonia |
| 8 | Female | 75 | 10th June | 7th June | Multiple myeloma |
| 9 | Male | 62 | 10th June | 8th June | Hepatic cirrhosis, liver cancer |
| 10 | Male | 65 | 11th June | 7th June | Lung cancer |
| 11 | Male | 73 | 12th June | 1st June | COPD, asthma |
| 12 | Male | 78 | 12th June | 1st June | Asthma, hypertension |
| 13 | Female | 72 | 12th June | 6th June | Pneumonia, ARF |
| 14 | Female | 67 | 13th June | 10th June | Hypothyroidism, hypertension |
| 15 | Male | 58 | 14th June | 2nd June | DM |
| 16 | Male | 61 | 14th June | 6th June | None |
| 17 | Male | 49 | 15th June | 5th June | Alcoholic cirrhosis of liver, DM |
| 18 | Male | 58 | 15th June | 9th June | None |
| 19 | Male | 65 | 15th June | 11th June | None |
| 20 | Male | 69 | 17th June | 4th June | TB, hypertension |
| 21 | Female | 54 | 17th June | 5th June | Bronchiectasis, hypertension |
| 22 | Male | 64 | 17th June | 7th June | Hypertension, asthma, necrotizing pancreatitis, abdominal infection |
| 23 | Female | 82 | 17th June | 7th June | Hypertension, cataract surgery |
| 24 | Male | 75 | 19th June | 10th June | None |
| 25 | Male | 63 | 20th June | 10th June | Myocardial ischaemia, DM |
| 26 | Male | 84 | 22nd June | 9th June | Lung cancer |
| 27 | Male | 87 | 22nd June | 12th June | AF, heart failure, cancer, stroke |
| 28 | Male | 65 | 24th June | 6th June | None |
| 29 | Female | 70 | 24th June | 22nd June | None |
| 30 | Female | 79 | 25th June | 7th June | DM, cerebral infarction |
| 31 | Female | 80 | 26th June | 13th June | Bladder cancer |
| 32 | Male | 55 | 27th June | 9th June | None |
| 33 | Female | 81 | 29th June | 6th June | Hypertension, cardiac valvular disease, cerebral infarction |
| 34 | Female | 50 | 7th July | 23rd June | Lymphoma, TB |
| 35 | Male | 70 | 8th July | 12th June | None |
| 36 | Male | 60 | 10th July | 16th June | Lung cancer |
| 37 | Male | 66 | 25th October | 15th June | None |
| 38 | Male | 35 | 25th November | 5th June | Cutaneous lymphoma |
COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; TB, tuberculosis; ARF, acute renal failure; AF, atrial fibrillation.
Timeline of confirmed MERS cases in South Korea in 2015
From identification of the first MERS patient to mid-June 2015, the numbers of confirmed and suspected MERS cases increased rapidly. The first death from MERS occurred on 1st June 2015. On 17th June 2015, the number of suspected cases placed in isolation peaked at 6729. By 26th October 2015, 16,752 people had been isolated. The 186th confirmed case was diagnosed on 4th July 2015, and no further cases were confirmed. The last death occurred on 25th November 2015.
Distribution of MERS clusters and suspected super spreaders in South Korea
The MERS outbreak in South Korea involved both intra- and interhospital transmission.9 The index case visited four hospitals whilst symptomatic between 11th and 20th May 2015, when he was diagnosed with MERS. During this period, he infected 28 people. Patient 14 was likely to have been infected during his stay at St. Mary's Hospital, Pyeongtaek between 15th and 17th May 2015. He was subsequently admitted to the emergency room at Samsung Medical Centre on 20th May 2015, and was diagnosed with MERS on 30th May 2015. During his stay at Samsung Medical Centre, he infected 81 patients; he then infected a further four patients at Good-morning Hospital, Pyeongtaek. Patient 16 was also infected at St. Mary's Hospital, Pyeongtaek between 15th and 16th May; he then infected 23 people at Konyang University Hospital and Daejeon Hospital (Figure 2 ).
Figure 2.
Distribution of transmission of Middle East respiratory syndrome coronavirus clusters and suspected super spreaders in South Korea (20th May to 25th November 2015).
Discussion
South Korea has the world's second highest number of confirmed MERS cases after Saudi Arabia. While South Korea has officially reported 186 confirmed cases of MERS, WHO reports 185 confirmed cases.2 This discrepancy is due to the fact that the South Korean Government included a South Korean patient who was diagnosed with MERS in China during a business trip, despite the fact that he was a suspected case while in South Korea. As in Saudi Arabia, MERS was more common in males than in females in South Korea.15
MERS-CoV has the same coronavirus lineage as the severe acute respiratory syndrome coronavirus (SARS-CoV).16 Zumla et al. and Chowell et al. compared the general characteristics between MERS and SARS.8, 10 They reported that more than 90% of both MERS and SARS cases were adults. However, whereas 64.5% of MERS cases were males, 57% of SARS cases were females.8, 9, 10 The reason for this apparent difference between the two infections is unknown; it may be related to differences in the sex distribution of the total populations at risk of the two infections.17 The average age of confirmed MERS patients in South Korea was 55 years, which is a little higher than that reported by Zumla et al. (50 years).8, 9 Zumla et al. also reported a case of MERS in a 1 year old, although only 2% of cases were in children.8 The youngest confirmed case in South Korea was a 16-year-old male (Case No. 67, who was the son of Case No. 46).11, 12
The fatality rate for MERS in South Korea was 19.9%. In contrast, the European Centre for Disease Control and Prevention reported that the global MERS fatality rate between March 2012 and October 2015 was 38.6% (1616 confirmed cases and 624 deaths). There were marked regional differences in mortality rates: 41.1% in the Middle East, 53.3% in Europe and 40.0% in Africa, compared with 19.2% in Asian countries.3 Among probable SARS cases that occurred during 2002 and 2003, the global case fatality rate was lower at 9.6% (774 deaths in 8098 cases), but again there was considerable regional variation.18 One of the reasons why South Korea has a lower fatality rate than other MERS-outbreak countries may be accessibility to a high level of emergency medical treatment. The difference does not appear to be attributable to mutations in the virus.19 There was also a difference in the types of underlying conditions associated with fatal MERS in South Korea compared with Saudi Arabia. In Saudi Arabia, diabetes mellitus (74% of patients) was the most common underlying condition in fatal cases, followed by end-stage renal disease (52%), lung disease (43%) and cardiac disease (39%).20 However, in South Korea, respiratory disease (30.5%), cancer (27.8%) and hypertension (22.2%) were the most common underlying conditions.
Oboho et al. reported that 109 (97.3%) of 112 patients in the Jeddah area of Saudi Arabia, who were not healthcare workers, contracted MERS through contact with someone in a healthcare facility.20 Likewise, the present study found that 99.4% of cases were nosocomially acquired. The MERS infection routes in South Korea are characterized by both intra- and interhospital transmission.9 Cases of community-acquired transmission were not found, corroborating the findings of the WHO report that there was no evidence of transmission outside hospitals in South Korea.16, 21, 22 However, it was noted that MERS testing was only available to patients known to have been in close contact with a confirmed or suspected case; as such, more casual contacts of MERS cases may have been missed because they were not tested. However, global experience does indicate that MERS is predominantly a nosocomially acquired infection,18 so restrictions on visitors are likely to play a key role in controlling MERS.23
Immediately after the MERS outbreak in South Korea, many researchers reported various problems with the South Korean Government's MERS control measures. It was reported that South Korea's MERS outbreak was caused by poor hospital infection control standards and lack of monitoring close contacts, which was also the case in Saudi Arabia.19 It was highlighted that public risk communication was delayed because the South Korean Government prioritized the determination of all details of the outbreak rather than information disclosure. This resulted in widespread panic during the MERS crisis.24 Jack pointed out that while the biological basis for the initial failure to contain MERS is unclear, a number of factors contributed significantly, including ‘doctor shopping’ behaviour (i.e. a patient seeks treatment from various hospitals for the same ailment), lack of epidemiology experts, the culture of frequent hospital visits and familial care-giving, and the South Korean Government's steadfast stance on keeping information contained.25 WHO experts indicated that problems with the initial spread of MERS in South Korea included prevalent occurrences among medical staff, lack of hospital infection management procedures, extremely crowded emergency rooms and multi-bed rooms in some hospitals, ‘doctor shopping’ behaviour, and the spread of infection through patient's family members or friends during hospital visits.26 Finally, Choi et al. reported that South Korea's initial failure to control MERS was caused by South Korea's rigid application of MERS control guidelines which failed to isolate all close contacts, failure to recognize super-spreading events, environmental factors such as inadequate ventilation, insufficient infectious disease management capacity in secondary hospitals, and the South Korean Government's inadequate crisis management communication.4
Many healthcare professionals in South Korea reported that the spread of MERS in South Korea could be characterized by the fact that hospitals acted as the main infection location, and by super-spreading events, where one case infects a number of others. 4, 9, 10 The occurrence of super-spreading events is known to be determined by physiological factors of the host, transmissibility of the pathogen, and the environment (e.g. crowding).27 Lim pointed out that as the MERS-CoV isolated in South Korea did not differ from that isolated in other countries, there is a lack of biological evidence to support the occurrence of super-spreading events.28 As such, super-spreading events must have been caused by environmental factors, including the South Korean Government's inadequate crisis response management. Other countries should be aware of this in their response to imported MERS cases. The debate on MERS infection handling in South Korea continues, with many local experts proposing improvement measures locally to prevent future national outbreaks of infectious diseases.29, 30, 31, 32, 33
This narrative account of the South Korean experience of MERS describes some issues that are of local importance alone, but also contains some important lessons of wider relevance. First, the importance of early detection of cases; second, the role of super spreaders of the virus; and third, the importance of restricting hospital visitors as a control measure. It is also suggested that hospitals need to be prepared for eventualities such as MERS, such as by ensuring that they have the necessary facilities and equipment for patient isolation. For countries such as South Korea where medical care is insurance based, insurance coverage for infectious diseases should be included in insurance plans to ensure that there are no delays in clinical care.
Conflict of interest statement
None declared.
References
- 1.Petersen E., Hui D.S., Perlman S., Zumla A. Middle East respiratory syndrome – advancing the public health, and research agenda on MERS – lessons from the South Korea outbreak. Int J Infect Dis. 2015;36:54–55. doi: 10.1016/j.ijid.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO; Geneva: 2015. Middle East respiratory syndrome coronavirus (MERS-CoV)http://www.who.int/emergencies/mers-cov/en/ Available at: [last accessed October 2015] [Google Scholar]
- 3.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2015. Middle East respiratory syndrome coronavirus (MERSCoV) 21st update. [Google Scholar]
- 4.Jun K. The Wall Street Journal; 2015. How MERS could affect South Korea's economy.http://blogs.wsj.com/economics/2015/06/10/how-mers-could-affect-south-koreas-economy/ Available at: [last accessed October 2015] [Google Scholar]
- 5.Kelland K. Reuters; 2015. Transparency, teamwork key to beating deadly South Korea MERS outbreak.http://www.reuters.com/article/2015/06/03/us-health-mers-transparency-idUSKBN0OJ1XW20150603 Available at: [last accessed October 2015] [Google Scholar]
- 6.Kupferschmidt K. Did poor ventilation lead to MERS ‘superspread’ in Korea? Science 2015. Available at: http://news.sciencemag.org/asiapacific/2015/06/did-poor-ventilation-lead-mers-superspread-korea [last accessed October 2015].
- 7.Choi J.W., Kim K.H., Cho Y.M., Kim S.H. Current epidemiological situation of Middle East respiratory syndrome coronavirus clusters and implications for public health response in South Korea. J Korean Med Assoc. 2015;58:487–497. [Google Scholar]
- 8.Zumla A., Hui D.S., Perlman S. Middle East respiratory syndrome. Lancet. 2015;386:995–1007. doi: 10.1016/S0140-6736(15)60454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;37:e2015033. doi: 10.4178/epih/e2015033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chowell G., Abdirizak F., Lee S. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mers.go.kr . Centre for Disease control and Prevention, Korea; 2015. MERS portal.http://www.mers.go.kr/mers/html/jsp/main.jsp Available at: [last accessed October 2015] [Google Scholar]
- 12.Policy Briefing Room . 2015. Policy briefing room homepage.http://www.korea.kr/briefing/mainList.do Policy briefing, Korea; Available at: [last accessed October 2015] [Google Scholar]
- 13.Woolhouse M.E., Dye C., Etard J.F. Heterogeneities in the transmission of infectious agents: implications for the design of control programs. Proc Natl Acad Sci USA. 1997;94:338–342. doi: 10.1073/pnas.94.1.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lloyd-Smith J.O., Schreiber S.J., Kopp P.E., Getz W.M. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alghamdi I.G., Hussain I.I., Almalki S.S., Alghamdi M.S., Alghamdi M.M., El-sheemy M.A. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417–423. doi: 10.2147/IJGM.S67061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assiri A., McGeer A., Perl T.M. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J., Sheng W., Fang C. Clinical manifestations, laboratory findings, and treatment outcomes of SARS patients. Emerg Infect Dis. 2004;10:818–824. doi: 10.3201/eid1005.030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hui D.S.C., Chan M.C.H., Wu A.K., Ng P.C. Severe acute respiratory syndrome (SARS): epidemiology and clinical features. Postgrad Med J. 2004;80:373–381. doi: 10.1136/pgmj.2004.020263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hui D.S., Perlman S., Zumla A. Spread of MERS to South Korea and China. Lancet Respir Med. 2015;3:509–510. doi: 10.1016/S2213-2600(15)00238-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oboho I.K., Tomczyk S.A., Al-Asmari A.M. 2014 MERS-CoV outbreak in Jeddah – a link to health care facilities. N Engl J Med. 2015;372:846–854. doi: 10.1056/NEJMoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee S.S., Wong N.S. Probable transmission chains of Middle East respiratory syndrome coronavirus and the multiple generations of secondary infection in South Korea. Int J Infect Dis. 2015;38:65–67. doi: 10.1016/j.ijid.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . WHO; Geneva: 2015. WHO | MERS-CoV joint mission findings discussion.http://www.who.int/mediacentre/news/mers/briefing-notes/update-15-06-2015/en/ Available at: [last accessed October 2015] [Google Scholar]
- 23.Banach D.B., Bearman G.M., Morgan D.J., Munoz-Price L.S. Infection control precautions for visitors to healthcare facilities. Expert Rev Anti Infect Ther. 2015;13:1047–1050. doi: 10.1586/14787210.2015.1068119. [DOI] [PubMed] [Google Scholar]
- 24.Fung I.C., Tse Z.T.H., Chan B.S.B., Fu K.W. Middle East respiratory syndrome in the Republic of Korea: transparency and communication are key. Western Pac Surveill Response J. 2015;6:1–2. doi: 10.5365/WPSAR.2015.6.2.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jack A. Why the panic? South Korea's MERS response questioned. BMJ. 2015;350:h3403. doi: 10.1136/bmj.h3403. [DOI] [PubMed] [Google Scholar]
- 26.Wpro.who.int . WPRO; 2015. High-level messages.http://www.wpro.who.int/mediacentre/mers-hlmsg/en/ Available at: [last accessed October 2015] [Google Scholar]
- 27.Sherertz R.J., Reagan D.R., Hampton K.D. A cloud adult: the Staphylococcus aureus-virus interaction revisited. Ann Intern Med. 1996;124:539–547. doi: 10.7326/0003-4819-124-6-199603150-00001. [DOI] [PubMed] [Google Scholar]
- 28.Lim P.L. Middle East respiratory syndrome (MERS) in Asia: lessons gleaned from the South Korean outbreak. Trans R Soc Trop Med Hyg. 2015;109:541–542. doi: 10.1093/trstmh/trv064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim Y. Healthcare policy and healthcare utilization behavior to improve hospital infection control after the Middle East respiratory syndrome outbreak. J Korean Med Assoc. 2015;58:598. [Google Scholar]
- 30.Lee K.H. Emergency medical services in response to the Middle East respiratory syndrome outbreak in Korea. J Korean Med Assoc. 2015;58:611. [Google Scholar]
- 31.Choi J.W., Kim K.H., Moon J.M., Kim M.S. Public health crisis response and establishment of a crisis communication system in South Korea: lessons learned from the MERS outbreak. J Korean Med Assoc. 2015;58:624. [Google Scholar]
- 32.Choi J.W. Lessons learned from Middle East respiratory syndrome coronavirus cluster in Korea. J Korean Med Assoc. 2015;58:595. [Google Scholar]
- 33.Choi J.W., Lee J.S., Kim K.H. Proposed master plan for reform of the national infectious disease prevention, and management system in Korea. J Korean Med Assoc. 2015;58:723. [Google Scholar]