Abstract
Background
The clinical outcome of the medial patellofemoral ligament reconstruction (MPFLR) based on graft length change pattern (length pattern group) was compared with MPFLR based on visual examination combined with palpation (visual/palpation group).
Methods
Physical findings, patient-reported outcome, and radiographic demonstration were evaluated pre- and postoperatively.
Results
The length pattern group had significantly lower risk of a positive apprehension test (Odds ratio 0.12, p < 0.01), and higher scores in postoperative Lysholm score (p = 0.046) and patient satisfaction (p = 0.036) than The visual/palpation group.
Conclusion
MPFLR based on graft length change pattern improved on patient-reported outcomes and apprehension test.
Level of evidence
Level Ⅲ, Retrospective comparative study.
Key terms: MPFLR, Graft length change pattern, Patella instability, Femoral side graft placement
1. Background
Medial patellofemoral ligament reconstruction (MPFLR) has become a popular treatment for patella instability over the past decade. However, previous systematic reviews of MPFLR showed a wide range of complication rates, including re-dislocation, loss of knee flexion, pain during knee flexion, and patellofemoral osteoarthritis.1,2
Graft tension change is considered one of the critical factors affecting the outcomes of MPFLR.3 Normal medial patellofemoral ligament (MPFL) tension change shows an isotonic pattern from extension up to 60° and then, a significant decrease above 60°.4 An abnormal increase in graft tension and patellofemoral pressure during knee flexion could result in pain during knee flexion, loss of knee flexion, patellofemoral osteoarthritis, and lateral patellar instability with stretched graft if graft is forced to stretch.3,5,6 A previous study reported that an excessive decrease in graft tension in the first 40° of knee flexion caused a recurrence of lateral patellar instability.5 Since the graft length change pattern directly affect the graft tension and the patellofemoral pressure, the graft length change pattern during full knee range of motion is one of the most important parameters to avoid complications.
Femoral side graft placement was reported to be the principal factor affecting graft length change pattern by biomechanical studies using normal cadaveric knee and computational simulation analyses.7, 8, 9, 10 On the other hand, a previous clinical study using intraoperative radiographic evaluation showed that the isometric point varied widely among patellar instability patients, unlike normal cadaveric study.11 At the present moment, the optimal femoral side graft placement in patellar instability patient have not defined.
Prior to 2011, we determined femoral side graft placement by visual examination combined with palpation based on the anatomic attachment site of the MPFL in normal cadavers.12,13 In 2011, we changed our approach to determination of femoral side graft placement based on the length change pattern of the reconstructed MPFL (the procedure mentioned in the methods). The purpose of this study was to evaluate clinical outcomes of MPFLR based on graft length change pattern (length pattern group) in comparison with MPFLR based on visual examination combined with palpation (visual/palpation group). The hypothesis underlying this study was that femoral side graft placement determined by graft length change pattern would improve the clinical outcomes of MPFLR.
2. Methods
2.1. Subjects
We conducted a retrospective review of 52 MPFLR that had been performed without combined tibial tuberosity transfer between September 2004 and October 2015 at our hospital. Exclusion criteria included: refusal of consent, postoperative infection, hereditary diseases, patients with an open growth plate, and lost to follow-up in within 2 years except for early re-dislocation (one patient who re-dislocated after 19 months operation was included). One patient had infection at the operation site, 1 patient had Ehlers-Danlos syndrome, 4 patients had open growth plates, and 2 patients were lost to follow-up within 2 years. Therefore, we excluded a total of 8 patients. Consequently, this study included 17 patients with MPFLR based on visual examination combined with palpation between September 2004 and January 2011 (visual/palpation group) and 27 patients with MPFLR based on graft length change pattern between March 2011 and October 2015 (length pattern group). Post hoc power analysis revealed that, with an alpha of 0.05, the sample size of this study achieved a power of 0.87 for differences in occurrence of positive apprehension test between the two groups. Demographic data, including age, gender, preoperative periods, and diagnosis were noted pre-operatively. Operation records were reviewed. This study was approved by the institutional review board, and informed consent was obtained from each patient.
2.2. Operative procedures
All operations were performed by a senior doctor who is a head of the department of sports medicine or 5 senior doctors who had more than fifteen years of experience in orthopedic surgery under supervision of a head of the department. The MPFLR was performed beginning with a standard arthroscopic examination. Eight of 17 patients (47.0%) in length pattern group and 14 of 27 patients (51.8%) in visual/palpation group underwent lateral retinacular release before MPFLR in cases with excessively tight lateral retinaculum, in order to correct the patellar tracking.
Double-stranded hamstring tendon were used as graft tissue. A straight skin incision of approximately 3 cm along the proximal half of the medial edge of the patella. The medial edge of the patella was exposed. The reconstruction route was created bluntly between the second and third layers from the medial patellar incision to the femoral attachment of the medial collateral ligament (MCL). Another straight 2 cm incision was made at the femoral insertion of the MCL. The provisional femoral side graft placement was determined in between the medial femoral epicondyle and the adductor tubercle with visual examination combined with palpation of each prominence through the incision. In the visual/palpation group, this position was used as the final graft placement. In the length pattern group, a 2.4 mm-diameter guidewire was inserted at this position and a folded polyester vessel tape was hooked onto the guidewire, introduced through the reconstruction route to the medial patellar site, and provisionally fixed to the proximal one-third of the patella with sutures at 70° of knee flexion. length of the vessel tape, patellar stability and patellar tracking were confirmed from 0° to 135 or more degrees of knee flexion. Proper pattern was defined an isometric or a slightly shorter pattern during knee flexion same as normal medial patellofemoral ligament.4 If the length change did not show proper pattern the guidewire was moved to a posterior-distal or distal position and the same confirmation procedure was repeated until the optimal graft placement was determined. Once the optimal femoral side graft placement was determined, the vessel tape was removed and a 4.5 mm-diameter tunnel was created to the lateral cortex of the femur using an EndoDrill (Smith & Nephew Endoscopy, Andover, MA). Thereafter, a femoral socket with a diameter matching the graft diameter was created and the graft was fixed with the EndoButton CL (Smith & Nephew Endoscopy, Andover, MA).
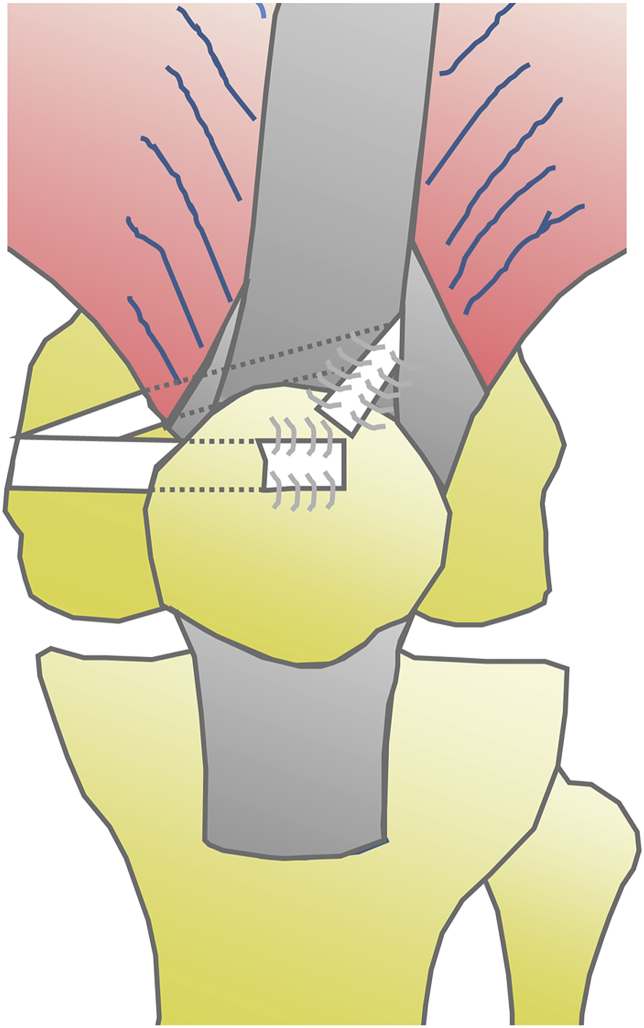
For the patellar side fixation, the graft was positioned to mimic its native attachment site based on an anatomic study.14 Namely, both the proximal bundle attached to the vastus intermedius tendon (proximal bundle) and the bundle attached to the proximal two-thirds of the patella (patellar bundle) were created (Fig. 1). After the femoral side fixation, the graft was introduced through the reconstruction route to the medial patellar site. A 4.5 mm-diameter curved tunnel was created at the proximal one-third of the patella, and the patellar bundle was introduced through the tunnel to the surface. The patellar bundle was sutured against the prepatellar fascia using No. 0 braided polyester sutures with adequate tension at 70° of knee flexion, where the patella was stabilized into the trochlear groove. For the proximal bundle, a 1 cm longitudinal cut was made at the lateral border of the rectus femoris tendon, just proximal to the patellar insertion site. A curved clamp was bluntly introduced from the cut to the medial patellar site under the vastus intermedius and vastus medialis tendon to create the reconstruction route, and then the proximal bundle was introduced to the lateral border of the rectus femoris tendon. The proximal bundle was sutured against the quadriceps fascia and the prepatellar fascia using No. 0 braided polyester sutures with adequate tension at 70° of knee flexion.
Fig. 1.
Schematic view of operation: Two reconstruction bundles were attached from femoral tunnel to the vastus intermedius tendon and to the proximal two-thirds of the patella (white bundles).
Patients were encouraged to practice quadriceps setting and range of motion exercise beginning 2 days after surgery. Static partial weight-bearing was permitted in knee extension with a knee brace and crutches. After patients were able to raise a leg without any extension lag, they were allowed to walk freely without a knee brace and crutches.
2.3. Evaluation methods
Clinical outcomes, including incidence of postoperative patellar re-dislocation, lateral patellar apprehension signs, range of motion, incidence of pain during knee flexion, Tegner score, Kujala score, and Lysholm score, were recorded at the final follow-up. Patient answered subjective satisfaction scores out of 100 points at the final follow-up. One hundred percent indicated that patient completely satisfied their knee condition and zero percent indicated patient dissatisfied their knee condition at all. Missing data were collected by telephone questionnaire. Passive maximum flexion angle was measured using a standard goniometer while the patient was supine. Sulcus angle, congruence angle, lateral tilt angle, lateral patellar displacement, and radiographic patellofemoral osteoarthritis progression were measured and evaluated on axial views at 30° of knee flexion at preoperative and at latest postoperative. The Insall-Salvati ratio and trochlear dysplasia according to the Dejour classification were measured on true lateral views.15 Magnetic resonance imaging (MRI) was utilized to measure the tibial tubercle–trochlear groove (TT-TG) distance.
2.4. Evaluation of femoral tunnel positioning
Femoral tunnel positioning was evaluated by postoperative true lateral radiographs as described previously.11 The anterior reference line was defined as the median line between the medial and lateral trochlear line that were drawn parallel to the femoral axis at the top of each medial and lateral trochlea of the femur (Fig. 2). The posterior reference line was positioned on posterior femoral condylar and drawn parallel to the anterior reference line. The distal reference line was positioned on distal top of femoral condylar and drawn vertical to the anterior reference line. The maximum anterior-posterior diameter of the femoral condyle was calculated as the anterior reference line to the posterior reference line and used as a standard (100%). The anterior-posterior ratio was calculated as the percentage of the distance between the tunnel position and the posterior reference line in the maximum anterior-posterior diameter. The proximal–distal ratio was calculated as the percentage of the distance between the tunnel position and the distal reference line in the maximum anterior-posterior diameter.
Fig. 2.
Schematic view of radiological assessment of the femoral tunnel.
The anterior reference line was defined as the median line between the medial ridge and lateral ridge line that were drawn parallel to the femoral axis at the top of each medial and lateral trochlea of the femur. The posterior reference line was drawn parallel to the anterior reference line on posterior femoral condylar. The distal reference line was positioned on distal top of femoral condylar and drawn vertical to the anterior reference line. The maximum anterior-posterior diameter of the femoral condyle was calculated as the anterior reference line to the posterior reference line and used as a standard (100%). The anterior-posterior ratio was calculated as the percentage of the distance between the tunnel position (red asterisk) and the posterior reference line in the maximum anterior-posterior diameter. The proximal–distal ratio was calculated as the percentage of the distance between the tunnel position and the distal reference line in the maximum anterior-posterior diameter.
2.5. Statistical analysis
Statistical analyses were performed by GraphPad Prism 5. Sulcus angle, congruence angle, lateral tilt angle, lateral patellar displacement, and femoral tunnel positioning were compared between the two groups using a t-test, after confirming normality using a histogram, and equal variance using the F test. Dejour classification, Tegner score, Kujala score, Lysholm score, age, preoperative periods, and follow-up periods were compared between the 2 groups using a Mann-Whitney test. Paired t-test was performed to compare between postoperative data and preoperative data. Results were considered statistically different for p-values lower than 0.05 (p < 0.05). Data were expressed as mean with ±standard deviation (SD) or the range of the data.
3. Results
3.1. Patient characteristics
Age at operation, gender, preinjury Tegner scores, and the preoperative periods did not show significant differences between the two groups (Table 1). The follow-up period averaged 90 months in the visual/palpation group and 46 months in the length pattern group. The preoperative radiographic data did not show significant differences between the two groups in Table 1. Two patients in the visual/palpation group and 5 patients in the length pattern group demonstrated patella alta with an Insall–Salvati index of greater than 1.5. Two patients in the visual/palpation group and 3 patients in the length pattern group had greater than 20 mm of TT–TG distance, and those 5 patients did not show poor outcome. Preoperative radiographic data did not show significant differences between the two groups.
Table 1.
Patients’ characteristics.
| Visual palpation group (mean ± SD) | Length pattern group (mean ± SD) | P Value | |
|---|---|---|---|
| Age (y) (range) | 24.4 (13–57) | 21.6 (14–45) | 0.98 |
| Female | 14 | 20 | 0.72 |
| Male | 3 | 7 | |
| Preinjury Tegner score (range) | 5.6 (3–7) | 5.1 (3–7) | 0.42 |
| Preoperative periods (month) (range) | 74. 7 (4–360) | 63.2 (1–396) | 0.68 |
| Follow-up periods (month) (range) | 90.1 (19–160) | 46.0 (24–76) | <0.01 |
| Radiological data | |||
| Insall salvati index | 1.25 ± 0.20 | 1.35 ± 0.22 | 0.38 |
| TT–TG distance (mm) | 14.8 ± 4.5 | 14.8 ± 5.7 | 1 |
| sulcus angle | 151 ± 8 | 147 ± 8 | 0.19 |
| Trochlear dysplasia (Dejour classification: normal/A/B/C/D) | 2/4/4/6/1 | 4/7/6/8/2 | 0.99 |
| Preoperative congruence angle (degrees) | −17.0 ± 36.6 | −9.4 ± 21.7 | 0.20 |
| Preoperative lateral tilt angle (degrees) | −12.5 ± 32.9 | −3.0 ± 8.8 | 0.43 |
| Preoperative lateral patellar displacement (mm) | 4.2 ± 9.4 | 5.1 ± 7.2 | 0.70 |
3.2. Postoperative improvement in radiographic findings
Congruence angle, lateral tilt angle and lateral patellar displacement significantly improved after the operation in the length pattern group (respectably P value: 0.015, <0.01, 0.048 Table 2). In the visual/palpation group, lateral tilt angle showed significant improvement (respectably P value: <0.01), whereas congruence angle and lateral patellar displacement did not show significant differences (respectably P value: 0.058, 0.33).
Table 2.
Comparison of preoperative and postoperative radiographic data.
| Preoperative (mean ± SD) | Postoperative (mean ± SD) | P Value | |
|---|---|---|---|
| The length pattern group | |||
| Congruence angle (degrees) | −9.4 ± 21.7 | −0.4 ± 19.3 | 0.015 |
| Lateral tilt angle (degrees) | −3.0 ± 8.8 | 2.9 ± 6.0 | <0.01 |
| Lateral patellar displacement (mm) | 5.1 ± 7.2 | 2.5 ± 9.7 | 0.048 |
| The visual palpation group | |||
| Congruence angle (degrees) | −17.0 ± 36.6 | −2.1 ± 36.0 | 0.058 |
| Lateral tilt angle (degrees) | −12.5 ± 32.9 | 2.7 ± 6.5 | <0.01 |
| Lateral patellar displacement (mm) | 4.2 ± 9.4 | 1.9 ± 6.7 | 0.33 |
3.3. Clinical outcomes
Three patients in the visual/palpation group had postoperative patellar re-dislocation and were recommended re-operation at 19, 35, and 42 months postoperatively. On the other hand, no patient in the length pattern group had postoperative patellar re-dislocation (Odds ratio (OR) 0.08, p = 0.051; Table 3). Patients in the length pattern group had a significantly lower risk of positive apprehension test than those in the visual/palpation group (OR 0.12, p < 0.01). Patients in the length pattern group showed a significantly higher postoperative Lysholm score and patient satisfaction score than those in the visual/palpation group (respectably P value: p = 0.046, p = 0.036).
Table 3.
Comparison clinical outcomes between the visual palpation group and length pattern group.
| Visual palpation group (mean ± SD) | Length pattern group (mean ± SD) | Odd ratio (95%CI)/P Value | |
|---|---|---|---|
| Incidence of postoperative patellar re-dislocation | 3/17 | 0/27 | OR 0.08 (0.004–1.6)/0.051 |
| Positive apprehension test | 10/17 | 4/27 | OR 0.12 (0.03–0.51)/< 0.01 |
| incidence of postoperative pain during knee flexion |
2/17 | 0/27 | OR 0.11 (0.005–2.5)/0.14 |
| Lysholm score | 84.7 ± 16.2 | 95.1 ± 5.4 | 0.046 |
| Kujala score | 90.1 ± 16.2 | 96.8 ± 6.5 | 0.065 |
| Patient satisfactory score | 73.4 ± 26.6 | 89.1 ± 13.2 | 0.036 |
| loss of knee flexion (≧10) | 0/17 | 0/27 | 1 |
| radiographic patellofemoral osteoarthritis progression |
2/17 | 0/27 | OR 0.11 (0.005–2.5)/0.14 |
| Femoral tunnel position | |||
| The anterior-posterior ratio (%) | 51.8 ± 9.5 | 47.6 ± 10.9 | 0.21 |
| The proximal-distal ratio (%) | 62.1 ± 15.9 | 49.9 ± 11.2 | <0.01 |
3.4. Femoral tunnel position
The mean femoral tunnel position in the length pattern group was significantly more distal than that in the visual/palpation group (p = 0.006) (Table 3). The mean femoral tunnel position in the length pattern group was a tendency of more posterior than the mean femoral tunnel position in the visual/palpation group.
4. Discussion
The most important finding of the present retrospective study was that this technique of MPFLR based on graft length change pattern enhanced patient satisfaction, reduced risk of positive apprehension test, and improved radiographic findings without any post-operative complications in the treatment of patella instability. To our knowledge, this is the first direct comparison study of clinical and radiographic outcomes between MPFLR based on graft length change pattern and MPFLR based on visual examination combined with palpation. These results demonstrated that locating the femoral tunnel based on graft length change pattern was an effective method for MPFLR.
Excessive patellofemoral contact forces with excessive graft tension during flexion is known to trigger pain during knee flexion, loss of knee flexion, and patellofemoral osteoarthritis.5 Furthermore, excessive graft tension during flexion can lead to elongation of the graft and postoperative re-dislocation. On the other hands, in MPFLR based on graft length change pattern, an isometric pattern or a slight shorter graft length change pattern during knee flexion without excessive graft tension is confirmed. Therefore, the concept of MPFLR based on graft length change pattern can theoretically reduce these critical complications. In the current study, there were no critical complications, such as pain during knee flexion, loss of knee flexion, patellofemoral osteoarthritis, and post-operative re-dislocation in length pattern group. Our results support the validity of intraoperative observation of graft length change pattern for the treatment of patella instability.
The graft length change with femoral side graft placement based on visual examination combined with palpation does not show always proper pattern in theory. Firstly, the isometric point varied widely among patellar instability patients, unlike normal cadaveric study.11 Secondly, it is difficult to find the correct anatomic femoral MPFL attachment site in clinical situations.16 There is an opinion that assessing femoral graft placement relying solely on visual examination combined with palpation is not appropriate. Furthermore, retrospective reviews showed that 64% of MPFLR femoral tunnels were placed on non-anatomical place.17 In the current study, in 14 of 27 cases in the length pattern group, the provisional femoral graft placement based on visual examination combined with palpation did not show proper length change pattern.
To move the femoral side graft placement to a more posterior-distal or distal position improved graft length change pattern in our study. Biomechanical studies and computational simulation analyses in normal cadaver knees have demonstrated that the posterior-distal position showed an isotonic pattern or a slight decrease in length change pattern during knee flexion compared to the anterior-proximal position.7,9,18,19 A clinical study also concluded that more posterior-distal positioning showed higher probability of isometric pattern or a slight shorter in graft length during knee flexion compared to anterior-proximal positioning in patella instability patient knees.11
There are several limitations in the current study. Firstly, we had a small number of patients involved in the current study. However, results in the present paper had statistical significance and were consistent with previous reports. Secondly, the follow-up period for patients in the length pattern group was shorter than that for the visual/palpation group. In this study, postoperative follow-up duration up to critical complications occurred in the visual/palpation group was shorter than the mean follow-up period of the length pattern group. However, shorter follow up periods in the length pattern group might likely underestimate recurrence of patellar dislocation. Thirdly, the visual/palpation group had poor patient-reported outcomes and high complication rates. However, for instance, postoperative Kujala scores of the visual/palpation group in the current study is better than the mean postoperative Kujala score in the review paper.20 Furthermore, the current study was conducted in the same hospital and under the same experienced orthopedist. And, 10 of 17 cases in visual/palpation group showed positive apprehension sign in physical examination. Conversely, several papers showed a wide range of incidence of positive apprehension up to 50%.21,22 This discrepancy results in largely attributable to the subjective nature of the apprehension test and a difference of the technique.
5. Conclusion
In conclusion, MPFLR based on graft length change pattern for the treatment of patella instability improved on patient-reported outcomes, radiographic findings, and apprehension test without any complication. Our results demonstrate that locating the femoral tunnel based on graft length change pattern is an effective method for MPFLR.
Declaration of competing interest
Hiroki Katagiri, Kazumasa Miyatake, Toshifumi Watanabe, Masafumi Horie, Ichiro Sekiy, Takeshi Muneta, and Hideyuki Koga declare that they have no conflict of interest.
Acknowledgements
The authors thank Atsushi Okawa, MD, PhD, for continuous support, Miyoko Ojima for management of our department, and Editage (www.editage.jp) for English language editing.
Footnotes
This study was conducted at Tokyo Medical and Dental University Hospital of Medicine.
This study was approved by the institutional review board. All patients provided their full written informed consent for participation in this clinical research prior to the operative procedure.
All authors read, approved the final manuscript and takes responsibility for the integrity of the data and the accuracy of the data analysis.
List of Abbreviations
- MPFLR
Medial patellofemoral ligament reconstruction
- MPFL
Medial patellofemoral ligament
- MCL
Medial collateral ligament
- MRI
Magnetic resonance imaging
- TT-TG
Tibial tubercle–trochlear groove
- SD
Standard deviation
- OR
Odds ratio
Author contributions
HK conceived the study and performed all experiments and participated in its design. KM participated in its design and performed analysis. TW acquired the data. MH analyzed and calculated the data. IS and TM participated in its design. HK had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parikh S.N., Nathan S.T., Wall E.J., Eismann E.A. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41(5):1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 3.Bollier M., Fulkerson J., Cosgarea A., Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27(8):1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 4.Arai Y., Nakagawa S., Higuchi T. Comparative analysis of medial patellofemoral ligament length change pattern in patients with patellar dislocation using open-MRI. Knee Surg Sports Traumatol Arthrosc : Off J ESSKA. 2017;25(8):2330–2336. doi: 10.1007/s00167-015-3689-2. [DOI] [PubMed] [Google Scholar]
- 5.Sanchis-Alfonso V., Montesinos-Berry E., Ramirez-Fuentes C., Leal-Blanquet J., Gelber P.E., Monllau J.C. Failed medial patellofemoral ligament reconstruction: causes and surgical strategies. World J Orthoped. 2017;8(2):115–129. doi: 10.5312/wjo.v8.i2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanchis-Alfonso V., Ramirez-Fuentes C., Montesinos-Berry E., Domenech J., Marti-Bonmati L. Femoral insertion site of the graft used to replace the medial patellofemoral ligament influences the ligament dynamic changes during knee flexion and the clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2433–2441. doi: 10.1007/s00167-015-3905-0. [DOI] [PubMed] [Google Scholar]
- 7.Stephen J.M., Lumpaopong P., Deehan D.J., Kader D., Amis A.A. The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med. 2012;40(8):1871–1879. doi: 10.1177/0363546512449998. [DOI] [PubMed] [Google Scholar]
- 8.Elias J.J., Cosgarea A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 9.Oka S., Matsushita T., Kubo S. Simulation of the optimal femoral insertion site in medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2364–2371. doi: 10.1007/s00167-014-3192-1. [DOI] [PubMed] [Google Scholar]
- 10.Yoo Y.S., Chang H.G., Seo Y.J. Changes in the length of the medial patellofemoral ligament: an in vivo analysis using 3-dimensional computed tomography. Am J Sports Med. 2012;40(9):2142–2148. doi: 10.1177/0363546512453301. [DOI] [PubMed] [Google Scholar]
- 11.Tateishi T., Tsuchiya M., Motosugi N. Graft length change and radiographic assessment of femoral drill hole position for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):400–407. doi: 10.1007/s00167-010-1235-9. [DOI] [PubMed] [Google Scholar]
- 12.Steensen R.N., Dopirak R.M., McDonald W.G., 3rd The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32(6):1509–1513. doi: 10.1177/0363546503261505. [DOI] [PubMed] [Google Scholar]
- 13.Smirk C., Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221–227. doi: 10.1016/s0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 14.Mochizuki T., Nimura A., Tateishi T., Yamaguchi K., Muneta T., Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):305–310. doi: 10.1007/s00167-012-1993-7. [DOI] [PubMed] [Google Scholar]
- 15.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 16.Herschel R., Hasler A., Tscholl P.M., Fucentese S.F. Visual-palpatory versus fluoroscopic intraoperative determination of the femoral entry point in medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2545–2549. doi: 10.1007/s00167-016-4057-6. [DOI] [PubMed] [Google Scholar]
- 17.McCarthy M., Ridley T.J., Bollier M., Wolf B., Albright J., Amendola A. Femoral tunnel placement in medial patellofemoral ligament reconstruction. Iowa Orthop J. 2013;33:58–63. [PMC free article] [PubMed] [Google Scholar]
- 18.Tischer T., Geier A., Lenz R., Woernle C., Bader R. Impact of the patella height on the strain pattern of the medial patellofemoral ligament after reconstruction: a computer model-based study. Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4190-2. [DOI] [PubMed] [Google Scholar]
- 19.Burrus M.T., Werner B.C., Cancienne J.M., Gwathmey F.W., Diduch D.R. MPFL graft fixation in low degrees of knee flexion minimizes errors made in the femoral location. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3092–3098. doi: 10.1007/s00167-016-4111-4. [DOI] [PubMed] [Google Scholar]
- 20.Mackay N.D., Smith N.A., Parsons N., Spalding T., Thompson P., Sprowson A.P. Medial patellofemoral ligament reconstruction for patellar dislocation: a systematic review. Orthop J Sports Med. 2014;2(8) doi: 10.1177/2325967114544021. 2325967114544021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christiansen S.E., Jacobsen B.W., Lund B., Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Krych A.J., O'Malley M.P., Johnson N.R. Functional testing and return to sport following stabilization surgery for recurrent lateral patellar instability in competitive athletes. Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4409-2. [DOI] [PubMed] [Google Scholar]