Abstract
Background
Neck pain is reported by many laborers who are at risk of experiencing musculoskeletal disorders due to muscle stiffness and hypokinetics. This study examined the effects of a lower trapezius exercise program on neck pain patients.
Material/Methods
The design of this study was a randomized controlled trial. A total of 40 neck pain patients participated in this study. Screening tests were performed and assigned to experimental group (n=20) and control group (n=20) using randomization program. Both groups underwent a scapula and thoracic spine stabilization exercise program. In addition, the experimental group implemented the lower trapezius strengthening exercise program. All interventions were applied 3 times per week for 4 weeks. Visual Analogue Scale (VAS), Neck Disability Index (NDI), postural alignment, muscle thickness and contraction rate were compared to evaluate the effect on intervention.
Results
Both groups showed significant differences in VAS, NDI, and postural alignment before and after intervention (P<0.05). In addition, the experimental group showed more significant difference in the amount of change in NDI and postural alignment values than the control group. The experimental group showed significant improvement in muscle thickness and contraction (P<0.05).
Conclusions
A lower trapezius strengthening exercise program is an effective method with clinical significance for reducing the level of neck dysfunction, and improving the postural alignment, muscle thickness, and contraction rate of the lower trapezius muscle.
MeSH Keywords: Exercise Therapy, Muscle Stretching Exercises, Neck Pain, Posture
Background
Approximately 68% of the total population has experienced neck pain at least once in their lifetime, and it easily transforms into a chronic state [1]. In today’s society, this is conspicuous in many laborers due to the increased use of computers, where the neck and shoulders are maintained in static postures to look at the computer screens [2]. This abnormal posture makes the area vulnerable to a range of musculoskeletal conditions by imparting large stresses to the neck and shoulders, as well as weakening the soft tissues by decreasing the biomechanical functions of the area, and inducing muscle stiffness and hypokinetics [3,4].
In the normal position of the head and neck, the center of the shoulder joints must be located vertically with both mastoid processes [4,5], and the muscles on the posterior side of the head and neck should maintain balance from consistent contraction [6]. However, the use of computers for a long period of time in an abnormal posture induces forward head posture or rounded shoulder postures [7]. Continuously maintaining improper posture is defined as upper crossed syndrome [8]. In this condition, rhomboids, serratus anterior, and lower trapezius are weakened, and pectoralis major, pectoralis minor, upper trapezius, and levator scapulae muscles are shortened, causing pain due to muscle imbalances [7,9].
Trapezius muscles play an important role in the movement of the scapula, specifically the lower trapezius has a key role in stabilizing the scapula [10]. Long-term hyper activation and shortening of the upper trapezius makes the lower trapezius weak, and this leads to muscle imbalance [11]. Many studies suggested therapeutic approaches that strengthens weak muscles and lengthens shortened muscles to achieve ideal postural alignment [8,12]. The O’Sullivan et al. (2007) [13] methods, which strengthen the lower trapezius without any compensation of the upper trapezius muscles, are emphasized, and examinations of the contraction of the lower trapezius using ultrasound are facilitated.
Previous studies suggested lower trapezius strengthening muscles as an intervention to patients with neck pain and proprioceptive changes in the scapula [14], but there is still an insufficient amount of evidence on the clinical results from lower trapezius strength changes [13]. The change in strength needs to be measured and evidence for the selective activation of the lower trapezius exercise in neck pain patients should be obtained.
There have been many studies on the application of various exercise methods to neck pain patients, but it was only in the recent years where the importance of lower trapezius thickness and contraction rate was emphasized [13,15]. Therefore, this study aims to explore the effects of lower trapezius strengthening of neck pain patients on pain, dysfunction, postural alignment, muscle thickness, and contraction rate.
Material and Methods
Participants
This study examined 53 participants from D city, who were in- or out-patients in P hospital for neck pain. The participants were included in the study if the midline of the outer ear is shifted more than 2.5 cm from the midline of the acromion [16], cranio-vertebral angle (CVA) of less than 53° [17], scored 3 or greater in visual analogue scale (VAS), and does not have any form of congenital deformity. The exclusion criteria were anyone who was diagnosed with an orthopedic condition via x-ray, traumatic neck injury, history of surgery in the spine or thoracic, or participation in less than 70% of the study interventions. All participants were provided with information regarding the process, study purpose, and they signed a written consent form.
Procedures
The design of this study was a randomized-controlled clinical trial conducted. G-power 3.19 software was used to calculate the sample size. The alpha level and power were set to 0.05 and 0.8, respectively. According to a previous pilot test, the effective size was set to 0.88, and at least 17 participants were required in each group. On the other hand, the minimum number of participants to be selected was 20 after taking a dropout rate of 15% in consideration [18]. All the 53 participants who participated the study voluntarily were screened, and 13 participants were excluded, including the participants who had the midline of the outer ear less than 2.5 cm from the midline of the acromion (n=5), participants whose CVA was greater than 53° (n=6), and refusal (n=2). In order to compare the effects before and after the interventions, initial assessments were made before assigning them to experimental (n=20) and control (n=20) groups using the randomization program [19]. Both groups were measured for VAS, neck disability index (NDI), postural alignment, and muscle thickness and contraction rate using the ultrasound before and after the intervention. All of the participants were provided an exercise program and the participants blinded to which group they were assigned to, and the data after the post-test assessments were recorded for analysis (Figure 1). All assessments were made by an experienced physical therapist with 5 years of clinical experience. This study was approved by the Ethical Committee of D University and is registered in World Health Organization (WHO) International Clinical Trials Registry Platform: KCT0004235.
Figure 1.
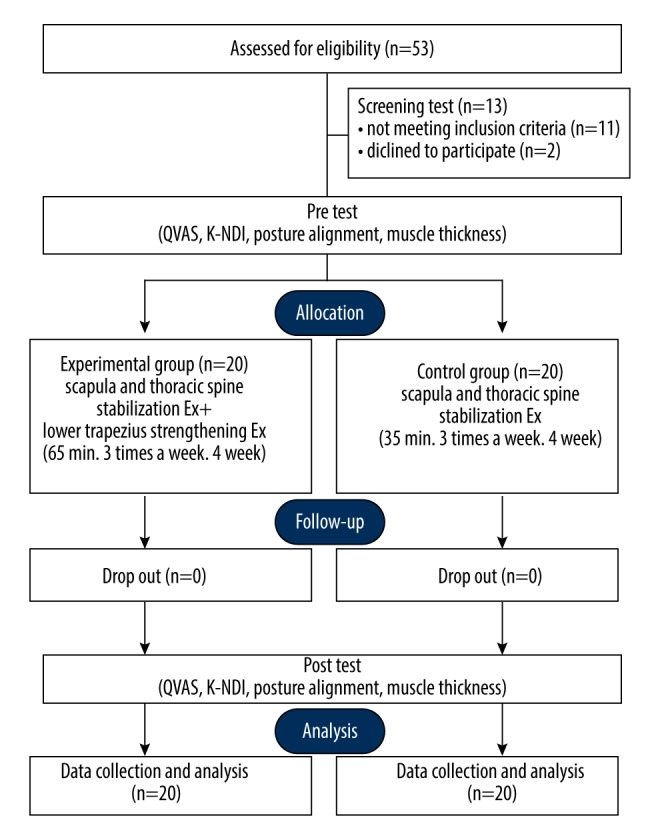
CONSORT flow chart.
Intervention
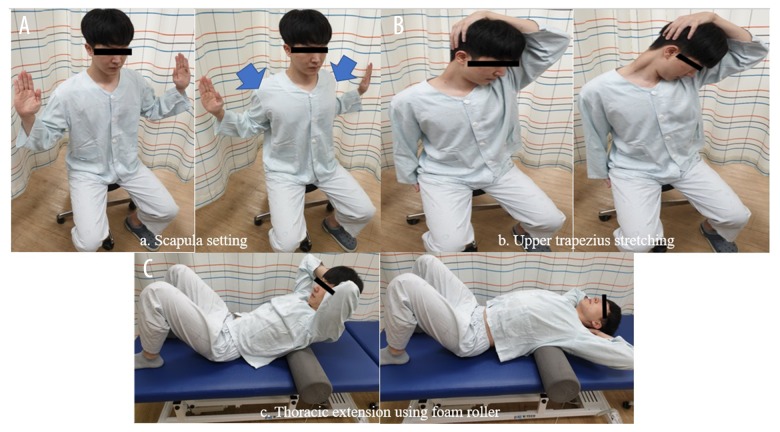
Both groups were given the intervention of scapula and thoracic spine stabilization exercise program which modified the intervention method of Cools et al. (2007) [10]. The exercise consisted of 3 programs of scapula setting, upper trapezius stretching, and thoracic spine extension using the foam roller.
Scapula setting
In the scapula setting program, the participant makes a chin tuck position to lengthen the posterior side of the neck in a sitting position. The arms are made to a W shape, where the palms face outward with the chest in a forward position. The chest is slightly elevated, and the scapulae come together downwards. Both hands are positioned slightly behind the shoulder line, where the elbows are touching the rib cage (Figure 2A).
Figure 2.
(A–C) Scapula and thoracic spine stabilization exercise program.
Upper trapezius stretching
The participant turns the head to one direction and the opposite arm is fixed under the buttocks. The other arm holds the head and stretched the neck to a diagonal direction. This position is held for 10 seconds to a range without any pain, and the same steps were repeated on the opposite direction. Maintaining 10 seconds for each direction is considered as 1 repetition (Figure 2B).
Extension of the thoracic spine
The participant places the foam roller under the lower thoracic segment making the bridge position. Both hands are behind the head with the fingers crossed. The thoracic spine is slowly extended up to the upper segments of the thoracic spine (Figure 2C).
Scapula and thoracic stabilization exercise programs were given to both the control and experimental group, where each program was administered as 3 sets of 10 repetitions for 20 seconds, and 20 seconds of break between each set. The interventions were applied every 4 weeks, 3 times a week, and 35 minutes per session, with the frequency and intensity applied individually according to the participant’s needs.
Lower trapezius strengthening exercise
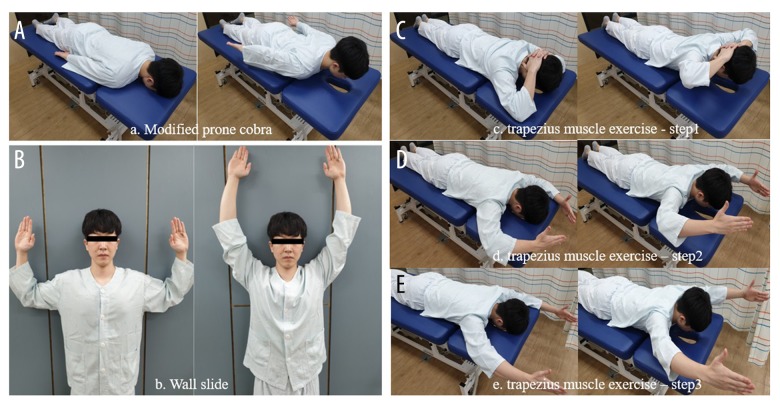
Lower trapezius strengthening exercise program was provided only to the experimental group. The program consisted of modified prone cobra, trapezius muscle exercise progression, and wall slide.
Modified prone cobra
Modified prone cobra exercise was suggested as a muscle strength test and exercise position for lower trapezius by Arlotta et al. (2011) [20]. The participant was instructed to sufficiently contract the lower trapezius muscle without compensating the upper trapezius. The participant raises the chest approximately 10 cm in a prone lying position to maintain the scapula pulled downwards for 10 seconds (Figure 3A).
Figure 3.
(A–E) Lower trapezius strengthening exercise program.
Wall slide
Wall sliding exercise is a lower trapezius strengthening exercise in a standing position, where both arms are lifted above the head [21]. The participant stands by the wall on the back. The shoulder joint is abducted and externally rotated to 90° and the elbow joint is flexed to 90°. Then the arms are lifted up and down contracting the lower trapezius without the compensation of the upper trapezius. (Figure 3B).
Trapezius muscle exercise progression
Trapezius muscle exercise progression is an exercise that strengthens the lower trapezius muscle without any compensation of upper trapezius and posterior deltoids [21]. Stage 1 starting position is made in prone lying. The shoulder and elbow joints are flexed to place the hands behind the head. The scapula is adducted, and the arms are out reaching for the ceiling for 10 seconds (Figure 3C). In stage 2, the starting position is in prone. The shoulder joint is abducted to 120°, elbow joint flexed in 90°, and the position is maintained for 10 seconds with the thumbs pointing towards the (Figure 3D). In stage 3, the starting position is also prone. The shoulder joint is abducted to 120°, elbow joint flexed, and 10 seconds is maintained with the thumbs towards the ceiling (Figure 3E).
The experimental group performed this lower trapezius strengthening exercise program for 10 by 3 sets for 10 seconds with a 20-second break between each set. The interventions were applied every 4 weeks, 3 times a week, and 30 minutes per session, with the frequency and intensity applied individually according to the participant’s needs.
Assessment methods
In order to assess the subjective pain level of the participants, VAS was used to measure the self-reported level of pain. A ruler with a 100 mm scale was used, with the left and right end of the ruler defined as “painless” 0 and “unbearable pain” 10, respectively [22]. The validity of this assessment is 0.05 and test-retest reliability is 0.99 [23].
In order to determine the dysfunction level, NDI was used. This questionnaire form assessment is scored on a scale between 0 to 5 in 10 items including level of pain, self-management, lifting items, reading, headache, concentration, work, driving, sleep, and leisure activities. The NDI score results in “no disability” in 0 to 4, “mild disability” in 5 to 14, “moderate disability” in 25 to 34, and “severe disability” in 25 to 34, and “total disability” in 35 or greater [24]. The interrater reliability was ICC=0.9 (r=0.85~0.95) [25].
To assess participants’ posture alignment, the participant maintains a stand-up position and the tripod is placed 1 meter away from the participant to take the photo (Figure 4). The measure the angles Image J (version1.46j, National Institute of Health, USA) was used [26]. The line that is horizontal with C7 and the line that is connected with tragus makes an angle. This angle meets with CVA, the line from C7 and tragus, and the line with the eyes on the lateral side and the tragus to measure cranial rotation angle (CRA). The same assessor took 3 photos and the mean angle was recorded. The test-retest reliability is 0.86 [27].
Figure 4.
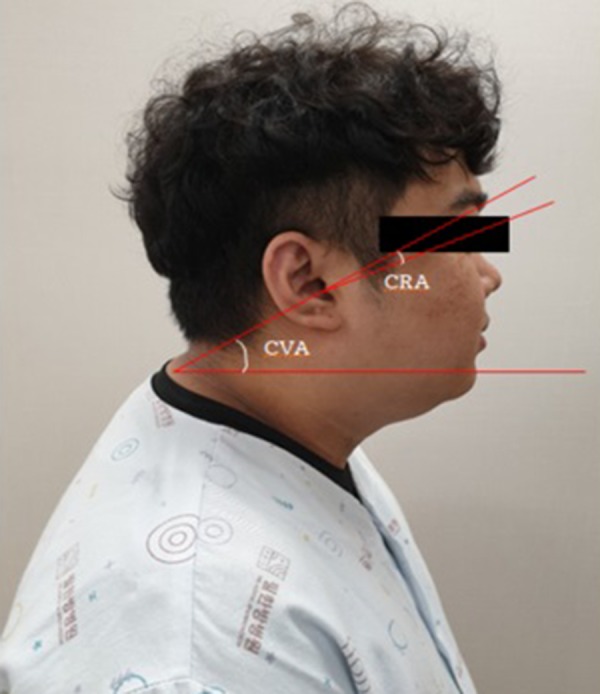
Cranio-vertebral angle (CVA) and cranial rotation angle (CRA).
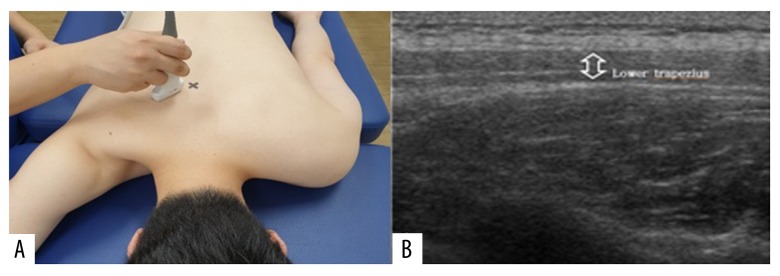
The thickness of lower trapezius was made using Mysono U6 (Samsung, Suwon, Korea) (Figure 5A). O’Sullivan et al. (2007) [13] suggested T8 as the most optimal point of reference for measurement using Mysono U6. For this measurement, the rater palpated C7 to palpate the spinous processes of the spine to mark T8. Ultrasound gel was applied on the area of the measurement. In B-mode, 3.5 MHz linear convex transducer was placed transversally on the lower trapezius. Then it was changed to M-mode to measure resting position and contraction position [28] (Figure 5B). The resting and contraction positions were each measured to calculate the contracted lower trapezius thickness as contraction rate=(contraction thickness/resting thickness). This test-retest reliability is high (ICC=1.00–1.00), and the intra-rater reliability is also high (ICC=0.91–0.96) [29].
Figure 5.
Muscle thickness measurement (A) and ultrasound images of lower trapezius muscle (B).
Statistical analysis
The collected data were analyzed using SPSS Win ver. 25.0 (IBM, Chicago, IL, USA). The mean and standard deviation values of the general characteristics of the participants were derived using descriptive statistics, and Shapiro-Wilk test was used for test or normality. The sex of the participants was analyzed using a χ2 test. A homogeneity test of the general characteristics and pre-measurement values was performed using a t-test. The differences between before and after the intervention effects of the 2 groups were analyzed using the independent t-test, and the differences before and after the intervention effects within 2 groups were analyzed using paired sample t-test. Repeated measure analysis of variance was used to identify the change following time and the effects of interaction between time and group. Statistical significance level was P<0.05.
Results
The general characteristics of the participants are shown in Table 1. The general characteristics of the 2 groups did not have statistically significant differences.
Table 1.
General characteristics.
| Experimental group (n=20) | Control group (n=20) | t/χ2 | P | |
|---|---|---|---|---|
| Sex (Male/Female) | 11/9 | 11/9 | 0.000 | 1 |
| Age (year) | 27.40±2.93# | 27.90±3.56 | −0.486 | 0.630 |
| Height (cm) | 171.15±8.72 | 171.40±7.13 | −0.099 | 0.921 |
| Weight (kg) | 70.00±15.44 | 70.85±13.32 | −0.186 | 0.853 |
| BMI | 23.71±3.97 | 23.94±3.24 | −0.202 | 0.841 |
| Onset (months) | 5.50±2.16 | 5.60±2.48 | −0.136 | 0.893 |
Mean±standard deviation;
BMI – body mass index.
Table 2 lists the pain level, dysfunction level, and postural alignment before and after the interventions. No significant differences in the pain level, dysfunction level, CVA, and CRA were observed between the 2 groups before the intervention (P<0.05), but both groups showed significant differences (P<0.05) in these parameters after the intervention. In addition, the differences in the NDI (d=1.11), CVA (d=−0.53), and CRA (d=0.50) between the groups showed a significant increase in the experimental group compared to the control group (P<0.05).
Table 2.
Comparison of dependent variables according to the intervention between groups.
| Experimental group (n=20) | Control group (n=20) | t(p) | Time F(p) | Time*group F(p) |
||
|---|---|---|---|---|---|---|
| VAS (cm) | Pre | 6.85±1.23# | 6.75±1.16 | −0.261 (0.797) | 242.065 (0.000) | 0.059 (0.809) |
| Post | 3.60±1.14 | 3.60±1.31 | ||||
| Post-pre | −3.25±1.16 | −3.15±1.42 | 0.302 (0.766) | |||
| t(p) | −12.49 (0.000) | −9.89 (0.000) | ||||
| NDI (score) | Pre | 16.30±6.68 | 16.20±4.40 | −0.061 (0.952) | 108.769 (0.000) | 4.112 (0.050) |
| Post | 9.85±4.82 | 11.85±4.80 | ||||
| Post-pre | −6.45±3.15 | −4.35±3.39 | 2.511 (0.021) | |||
| t(p) | −9.15 (0.000) | −5.736 (0.000) | ||||
| CVA (angle) | Pre | 47.98±7.90 | 47.51±5.93 | −0.214 (0.833) | 220.144 (0.000) | 32.008 (0.000) |
| Post | 52.15±7.82 | 49.38±5.75 | ||||
| Post-pre | 4.18±1.46 | 1.70±1.11 | −5.186 (0.000) | |||
| t(p) | 12.790 (0.000) | 7.667 (0.000) | ||||
| CRA (angle) | Pre | 148.92±8.53 | 148.44±8.60 | −0.200 (0.844) | 278.450 (0.000) | 20.426 (0.000) |
| Post | 144.53±9.09 | 145.91±8.52 | ||||
| Post-pre | −4.40±1.69 | −2.52±0.77 | −5.186 (0.000) | |||
| t(p) | −11.660 (0.000) | −14.630 (0.000) | ||||
| Muscle thickness in contraction (mm) | Pre | 0.56±0.22 | 0.54±0.25 | −0.359 (0.724) | 120.843 (0.000) | 80.280 (0.000) |
| Post | 0.69±0.23 | 0.55±0.25 | ||||
| Post-pre | 0.13±0.05 | 0.01±0.03 | −9.44 (0.000) | |||
| t(p) | 11.968 (0.000) | 1.840 (0.081) | ||||
| Muscle thickness in resting (mm) | Pre | 0.30±0.07 | 0.29±0.09 | −0.289 (0.776) | 0.328 (0.570) | 0.007 (0.935) |
| Post | 0.30±0.06 | 0.30±0.07 | ||||
| Post-pre | 0.00±0.02 | 0.00±0.02 | −0.077 (0.94) | |||
| t(p) | 0.556 (0.585) | 0.304 (0.764) | ||||
| Contraction rate (%) | Pre | 1.82±0.34 | 1.78±0.34 | −0.497 (0.625) | 51.658 (0.000) | 39.728 (0.000) |
| Post | 2.27±0.40 | 1.81±0.41 | ||||
| Post-pre | 0.45±0.25 | 0.03±0.16 | −0.587 (.000) | |||
| t(p) | 7.975 (0.000) | 0.829 (0.417) |
Mean±standard deviation;
VAS – visual analog scale; NDI – neck disability index; CVA – craniovertebral angle; CRA – cranial rotation angle.
Muscle thickness and contraction rate before and after the interventions are shown in Table 2. Experimental group showed a significant difference (P<0.05) of the muscle thickness and contraction rate in during contraction, but there were no significant differences in resting state. There were no significant differences between the groups. The after the intervention results showed a significant difference (P<0.05) of the experimental group in muscle thickness and contraction rate in during contraction, but there were no significant differences in resting state. In addition, the differences in muscle thickness (d=−0.58) and contraction rate(d=−1.21) between the groups showed a significant increase in the experimental group than the control group (P<0.05).
Discussion
This study aimed to compare the effects of scapula and thoracic spine stabilization exercises and lower trapezius strengthening exercise program with 40 participants who have neck pain. All participants who participated in the exercise program showed a common improvement in pain level, neck dysfunction, and postural alignment (P<0.05). In addition, the experimental group were additionally provided with lower trapezius strengthening exercise program, and they showed clinically significant changes in muscle thickness and contraction rate (P<0.05).
In the past, the common methods of treatment for neck pain were thermotherapy, therapeutic massage, ultrasound, and electrotherapy [30]. These was on the basis that active exercises with high intensity will induce fatigue and worsen neck pain [31]. However, recent studies show that active intervention is effective for pain and function in chronic neck pain patients, and among the different intervention methods, muscle strengthening exercise program that improves activation of scapulothoracic muscles via muscle contraction affects stabilization and postural maintenance of the scapular [32–37].
Tunwattanapong et al. (2016) [38] reported that pain was reduced significantly (P<0.05, effect size d=1.44) when 96 office workers were provided with 4 weeks of neck and scapula exercise program. Chung et al. (2012) [39] reported that 35 chronic neck pain patients showed significant decrease (P<0.05, effect size d=1.67) in neck functional disability index after 12 weeks of neck flexion exercises. This study showed significant decrease (P<0.05, effect size d=2.74) in pain level through 4 weeks of lower trapezius strengthening exercise program, and neck function disability level showed a significant decrease (P<0.05, effect size d=1.17) from 32.6% to 19.7%.
The flexion angle increases in neck pain patients, and at the same time, upper trapezius, which is a neck flexion muscle, increases in activation and the lower trapezius shows weakening in muscle strength and endurance [8]. According to Lin et al. (2006) [40], activated muscles such as the upper trapezius must be inhibited, and exercises that promote deactivated muscles such as the lower trapezius must be provided. In addition, Harman et al. (2005) [41] reported that CVA and CRA showed significant changes (P<0.05, effect size d=0.19) when physical therapists who had forward head position performed stretching and muscle strengthening exercises for 10 weeks. This study also showed significant increase (P<0.05, effect size d=−0.53) in CVA and CRA when intensive muscle strengthening exercise program for lower trapezius was provided.
Koppenhaver et al. (2009) [42] suggested that ultrasonography is a non-invasive method for evaluating the treatment effects and can measure the deep muscles accurately. In addition, the changes in the mobilization sequence that occur during muscle activation can be observed. Magnetic resonance imaging (MRI) and computes tomography (CT) may be used for visual assessment of muscle forms such as area and size [43], but this equipment has limitations in mobility, measurement of active movements, and high cost. Ultrasonography method is not only easily mobile, but also allows simultaneous observation of deep and shallow muscles and gives visual feedback for dynamic muscle activation [44]. In addition, studies on muscle thickness measurement using ultrasound is still lacking [45], and this study may be an evidence for methodology using ultrasound for measuring lower trapezius thickness during both contraction and resting states. This study demonstrates significant increase (P<0.05) of muscle thickness in contractions (effect size d=−0.58) and muscle contraction rate (effect size d=−1.21) before and after the intervention of lower trapezius strengthening exercise in neck pain patients. This was consistent with the study of Saliba et al. (2010) [46] which administered muscle strengthening exercise program for 51 patients, and also with the study by Arlotta et al. (2011) [20] who demonstrated that muscle contraction rate has increased in 18 healthy adults through lower trapezius strengthening exercise.
This study suggests that lower trapezius muscle strengthening exercise strengthens the weak muscles, and it decreases the imbalances in scapulothoracic muscles and increases stabilization in the neck and scapula to improve neck pain and dysfunction levels. Additionally, Sahrmann (2001) [21] reported that scapulothoracic muscle control is crucial for clinical management of neck pain patients. This provided intensive muscle strengthening exercise program for weakened lower trapezius to increase the ratio of lower trapezius muscle strength to upper trapezius [47], and it could be suggested that there was an effect on the decrease of dysfunction due to scapulothoracic imbalance and postural alignment improvement.
The limitations of this study were as follows. First, the average age of the participants was 27 years. Hence, the data obtained cannot be generalized to cervical pain patients of all ages. The second limitation was that there were no criteria for the onset of neck pain, result it to be difficult to prove the effects on acute and chronic neck pain patients. Thirdly, there may be some errors from the angle of the convex transducer and consistent pressure during the ultrasound measurement. However, in order to minimize the limitations, a physical therapist with many experiences in ultrasound measurements assessed alone. Future studies should consider these limitations and discuss the modification of lower trapezius strengthening exercise program and the effects.
The results of this study showed significant effects in all items including VAS, NDI, and postural alignment when 4 weeks of scapula and thoracic stabilization exercises and lower trapezius strengthening exercises were provided to neck pain patients. As a result, regulation of the scapula thoracic muscle affects the muscle activity, and positively affects the utilization of the muscle clinically. This demonstrates positive effects to neck pain patients, specifically lower trapezius strengthening exercise effectively activates muscle thickness and contraction rate than scapula and thoracic stabilization exercises, ultimately improving decreased dysfunction, and postural alignment. Therefore, lower trapezius muscle strengthening exercises can be an efficient exercise program for patients with neck pain.
Conclusions
This study aimed to investigate the effects of lower trapezius strengthening exercise on pain, dysfunction, muscle thickness, and muscle contraction rate of neck pain patients. The experimental group, which also performed the lower trapezius strengthening exercise, showed significant improvement in the level of neck dysfunction, as well as improvement in postural alignment, muscle thickness, and contraction rate of the lower trapezius muscle. These results suggest that lower trapezius strengthening exercise is clinically effective for neck pain patients.
Footnotes
Conflict of interest
None.
Source of support: Departmental sources
References
- 1.Hoving JL, De Vet HC, Twisk JW, et al. Prognostic factors for neck pain in general practice. Pain. 2004;110:639–45. doi: 10.1016/j.pain.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Korhonen T, Ketola R, Toivonen R, et al. Work related and individual predictors for incident neck pain among office employees working with video display units. Occup Environ Med. 2003;60:475–82. doi: 10.1136/oem.60.7.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanchanomai S, Janwantanakul P, Pensri P, Jiamjarasrangsi W. Prevalence of and factors associated with musculoskeletal symptoms in the spine attributed to computer use in undergraduate students. Work. 2012;43:497–506. doi: 10.3233/WOR-2012-1387. [DOI] [PubMed] [Google Scholar]
- 4.Falla D, Jull G, Russell T, et al. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:408–17. doi: 10.2522/ptj.20060009. [DOI] [PubMed] [Google Scholar]
- 5.Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (Phila Pa 1976) 2002;27:1835–43. doi: 10.1097/00007632-200209010-00004. [DOI] [PubMed] [Google Scholar]
- 6.Colby LA. Therapeutic exercise: Foundations and techniques. Philadelphia PA: FA Davis Company; 2007. [Google Scholar]
- 7.Mekhora K, Liston C, Nanthavanij S, Cole JH. The effect of ergonomic intervention on discomfort in computer users with tension neck syndrome. Int J Ind Ergon. 2000;26:367–79. [Google Scholar]
- 8.Janda V. Muscles and motor control in cervicogenic disorders Teoksessa Grant, R(toim) Physical Therapy of the Cervical and Thoracic Spine. Amsterdam: Elsevier Science; 2002. [Google Scholar]
- 9.Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6:51. [PMC free article] [PubMed] [Google Scholar]
- 10.Cools A, Declercq G, Cambier D, et al. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007;17:25–33. doi: 10.1111/j.1600-0838.2006.00570.x. [DOI] [PubMed] [Google Scholar]
- 11.Wright EF, Domenech MA, Fischer JR., Jr Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000;131:202–10. doi: 10.14219/jada.archive.2000.0148. [DOI] [PubMed] [Google Scholar]
- 12.Kendall FP, Mccreary EK, Provance PG. Muscles: Testing and function with posture and pain. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 13.O’Sullivan C, Bentman S, Bennett K, Stokes M. Rehabilitative ultrasound imaging of the lower trapezius muscle: Technical description and reliability. J Orthop Sports Phys Ther. 2007;37:620–26. doi: 10.2519/jospt.2007.2446. [DOI] [PubMed] [Google Scholar]
- 14.Mottram SL, Woledge RC, Morrissey D. Motion analysis study of a scapular orientation exercise and subjects’ ability to learn the exercise. Man Ther. 2009;14:13–18. doi: 10.1016/j.math.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Song WR, Kim SY, Jang HJ. A comparison of change in thickness for lower trapezius muscle during lower trapezius muscle isometric exercise and reliability of ultrasound imaging. Physical Therapy Korea. 2012;19:31–39. [Google Scholar]
- 16.Salahzadeh Z, Maroufi N, Ahmadi A, et al. Assessment of forward head posture in females: Observational and photogrammetry methods. J Back Musculoskelet Rehabil. 2014;27:131–39. doi: 10.3233/BMR-130426. [DOI] [PubMed] [Google Scholar]
- 17.Nemmers TM, Miller JW, Hartman MD. Variability of the forward head posture in healthy community-dwelling older women. J Geriatr Phys Ther. 2009;32:10–14. doi: 10.1519/00139143-200932010-00003. [DOI] [PubMed] [Google Scholar]
- 18.Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 19.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4:26. doi: 10.1186/1471-2288-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arlotta M, Lovasco G, Mclean L. Selective recruitment of the lower fibers of the trapezius muscle. J Electromyogr Kinesiol. 2011;21:403–10. doi: 10.1016/j.jelekin.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Sahrmann S. Diagnosis and treatment of movement impairment syndromes. Elsevier Health Sciences; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Price DD, Staud R, Robinson ME. How should we use the visual analogue scale (VAS) in rehabilitation outcomes? II: Visual analogue scales as ratio scales: An alternative to the view of Kersten et al. J Rehabil Med. 2012;44(9):800–1. doi: 10.2340/16501977-1031. discussion 803–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boonstra AM, Preuper HRS, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31:165–69. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 24.Vernon H, Mior S. The Neck Disability Index: A study of reliability and validity. J Manipulative Physiol Ther. 1991;14(7):409–15. [PubMed] [Google Scholar]
- 25.Song KJ, Choi BW, Choi BR, Seo GB. Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine (Phila Pa 1976) 2010;35:E1045–49. doi: 10.1097/BRS.0b013e3181df78e9. [DOI] [PubMed] [Google Scholar]
- 26.Chiu CA, Li J, Hwang H, et al. Image capture device with integrated barcode scanning. Google Patents 2013
- 27.Cuccia AM, Carola C. The measurement of craniocervical posture: A simple method to evaluate head position. Int J Pediatr Otorhinolaryngol. 2009;73:1732–36. doi: 10.1016/j.ijporl.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 28.Yamaguti WP, Claudino RC, Neto AP, et al. Diaphragmatic breathing training program improves abdominal motion during natural breathing in patients with chronic obstructive pulmonary disease: A randomized controlled trial. Arch Phys Med Rehabil. 2012;93:571–77. doi: 10.1016/j.apmr.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 29.Arlotta M, LoVasco G, McLean L. Selective recruitment of the lower fibers of the trapezius muscle. J Electromyogr Kinesiol. 2011;21(3):403–10. doi: 10.1016/j.jelekin.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 30.David J, Modi S, Aluko A, et al. Chronic neck pain: A comparison of acupuncture treatment and physiotherapy. Br J Rheumatol. 1998;37:1118–22. doi: 10.1093/rheumatology/37.10.1118. [DOI] [PubMed] [Google Scholar]
- 31.Ylinen J, Nykänen M, Kautiainen H, Häkkinen A. Evaluation of repeatability of pressure algometry on the neck muscles for clinical use. Man Ther. 2007;12:192–97. doi: 10.1016/j.math.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 32.Andersen LL, Kjaer M, Sögaard K, et al. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis Rheum. 2008;59:84–91. doi: 10.1002/art.23256. [DOI] [PubMed] [Google Scholar]
- 33.Bronfort G, Evans R, Nelson B, et al. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine (Phila Pa 1976) 2001;26:788–97. doi: 10.1097/00007632-200104010-00020. [DOI] [PubMed] [Google Scholar]
- 34.Chiu TT, Hui-Chan CW, Cheing G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabil. 2005;19:850–60. doi: 10.1191/0269215505cr920oa. [DOI] [PubMed] [Google Scholar]
- 35.Röijezon U, Björklund M, Bergenheim M, Djupsjöbacka M. A novel method for neck coordination exercise – a pilot study on persons with chronic non-specific neck pain. J Neuroeng Rehabil. 2008;5:36. doi: 10.1186/1743-0003-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Taimela S, Takala E-P, Asklöf T, et al. Active treatment of chronic neck pain: A prospective randomized intervention. Spine (Phila Pa 1976) 2000;25:1021–27. doi: 10.1097/00007632-200004150-00018. [DOI] [PubMed] [Google Scholar]
- 37.Ylinen J, Takala E-P, Nykänen M, et al. Active neck muscle training in the treatment of chronic neck pain in women: A randomized controlled trial. JAMA. 2003;289:2509–16. doi: 10.1001/jama.289.19.2509. [DOI] [PubMed] [Google Scholar]
- 38.Tunwattanapong P, Kongkasuwan R, Kuptniratsaikul V. The effectiveness of a neck and shoulder stretching exercise program among office workers with neck pain: A randomized controlled trial. Clin Rehabil. 2016;30:64–72. doi: 10.1177/0269215515575747. [DOI] [PubMed] [Google Scholar]
- 39.Chung SH, Her JG, Ko T, et al. Effects of exercise on deep cervical flexors in patients with chronic neck pain. Journal of Physical Therapy Science. 2012;24:629–32. [Google Scholar]
- 40.Lin J-J, Lim HK, Soto-Quijano DA, et al. Altered patterns of muscle activation during performance of four functional tasks in patients with shoulder disorders: Interpretation from voluntary response index. J Electromyogr Kinesiol. 2006;16:458–68. doi: 10.1016/j.jelekin.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: A randomized, controlled 10-week trial. J Man Manip Ther. 2005;13:163–76. [Google Scholar]
- 42.Koppenhaver SL, Hebert JJ, Fritz JM, et al. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil. 2009;90:87–94. doi: 10.1016/j.apmr.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 43.Kristjansson E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic and symptomatic subjects. Man Ther. 2004;9:83–88. doi: 10.1016/S1356-689X(03)00059-6. [DOI] [PubMed] [Google Scholar]
- 44.Kermode F. Benefits of utilising real-time ultrasound imaging in the rehabilitation of the lumbar spine stabilising muscles following low back injury in the elite athlete – a single case study. Phys Ther Sport. 2004;5:13–16. [Google Scholar]
- 45.Hodges P, Pengel L, Herbert R, Gandevia S. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003;27:682–92. doi: 10.1002/mus.10375. [DOI] [PubMed] [Google Scholar]
- 46.Saliba SA, Croy T, Guthrie R, et al. Differences in transverse abdominis activation with stable and unstable bridging exercises in individuals with low back pain. N Am J Sports Phys Ther. 2010;5:63–73. [PMC free article] [PubMed] [Google Scholar]
- 47.Reinold MM, Escamilla R, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39:105–17. doi: 10.2519/jospt.2009.2835. [DOI] [PubMed] [Google Scholar]