Abstract
The plant extract piperine is used as a traditional Chinese medicine due to its anti-inflammatory effects and efficacy against numerous types of cancer. The aim of the present study was to investigate the antitumor mechanism of piperine in human osteosarcoma U2OS and 143B cell lines. The effects of piperine on cell apoptosis and invasion of human osteosarcoma cells were assessed using flow cytometry and Transwell assays. Moreover, western blotting was used to measure the effects of piperine on the protein expression levels of the metastasis markers matrix metalloproteinase-2 (MMP-2) and vascular endothelial growth factor (VEGF). In addition, the involvement of the Wnt/β-catenin signaling pathway in modulating the effects of piperine was examined via western blot analysis. The results of MTT and Transwell invasion assays indicated that piperine treatment dose-dependently reduced U2OS and 143B cell viability and invasion. Furthermore, a significant reduction was identified in MMP-2, VEGF, glycogen synthase kinase-3β and β-catenin protein expression levels, as well as the expression levels of their target proteins cyclooxygenase-2, cyclin D1 and c-myc, in U2OS cells after piperine treatment. In addition, similar results were observed in 143B cells. Therefore, the present study demonstrated the efficacy of piperine in osteosarcoma, and identified that the Wnt/β-catenin signaling pathway may modulate the antitumor effects of piperine on human U2OS and 143B cells.
Keywords: antitumor, piperine, osteosarcoma, Wnt/β-catenin signaling, cell viability, invasion
Introduction
Osteosarcoma has an annual incidence rate of 5/1,000,000 individuals and a mortality rate of >50% in patients <20 years old worldwide (1–4). Surgery combined with radiotherapy and chemotherapy is the primary treatment method for osteosarcoma (5). However, ≤80% of patients have poor prognosis due to metastatic lesions that are already present at the time of diagnosis, and the 5-year survival rate is ~30% (6). Given this poor disease prognosis, the development of effective therapeutic strategies and pharmaceuticals to reduce osteosarcoma malignancy are important.
Piperine is an alkaloid found in Piper nigrum Linn and Piper longum Linn (Piper nigrum L., family piperaceae). Piperine is used as a food flavoring and as a traditional Chinese medicine due to its pharmacological benefits (7,8). Moreover, piperine is used to treat gastrointestinal disorders such as constipation and diarrhea (9). Furthermore, it has well-characterized anti-inflammatory (10) and antitumor effects in numerous types of cancer, including breast, lung and liver cancer, and lymphoma (11–14). Piperine has been reported to dose-dependently (15–20) regulate cell growth and differentiation via the Akt/JNK/MAPK pathway (21), and can increase cytokine production via the mTOR signaling pathway (22).
Tumor metastasis is a complex process involving tumor cell dissociation, extracellular matrix degradation, infiltration and adhesion to vascular endothelial cells (23). Notably, matrix metalloproteinases (MMPs), such as MMP-2 and MMP-9, and collagen type IV are significantly upregulated in osteosarcoma and metastases, and are indices of poor prognosis (24). Moreover, MMP-2 downregulation can inhibit osteosarcoma metastasis and infiltration (21,25). Vascular endothelial growth factor (VEGF) is known to promote angiogenesis, and its upregulation is correlated with poor osteosarcoma prognosis (26,27). Furthermore, VEGF downregulation has been shown to reduce vascular density and inhibit metastases in osteosarcoma (28).
While the antitumor effect of piperine on U2OS cells has been reported (21), its underlying molecular mechanisms of action are not fully understood. As the Wnt/β-catenin signaling pathway is known to regulate cell proliferation and differentiation (29,30), the present study hypothesized that it may be involved in modulating the antitumor effects of piperine. Therefore, the aim of the present study was to test this hypothesis; the results may provide a novel insight into the antitumor mechanism of piperine.
Materials and methods
Chemical reagents
DMSO and MTT were purchased from Sigma-Aldrich (Merck KGaA). Piperine (molecular weight, 285.35 kDa; National Institutes for Food and Drug Control) was dissolved in DMSO at the concentration of 150 µM and stored at −20°C. An Annexin V-FITC/PI double staining cell apoptosis detection kit was obtained from Nanjing KeyGen Biotech Co., Ltd. NQBB FBS was obtained from Wuhan ChunDuBio Co., Ltd. Anti-MMP-2 (cat. no. 10373-2-AP; 1:1,000) was purchased from ProteinTech Group, Inc. Anti-VEGF (cat. no. GB11034; 1:3,000), anti-c-Myc (cat. no. GB13076; 1:500), anti-cyclin D1 (cat. no. GB11079; 1:1,000), anti-cyclooxygenase-2 (COX2; cat. no. GB11072; 1:500), anti-β-catenin (cat. no. GB11015; 1:500) and anti-glycogen synthase kinase-3β (GSK-3β; cat. no. GB11099; 1:1,000) were purchased from Wuhan Servicebio Technology Co., Ltd.
Cell culture
Human osteosarcoma U2OS and 143B cells were provided by Cheeloo College of Medicine, Shandong University. 143B cells were identified by STR from Shanghai Cinoasia Institute, and the results showed that the cells were not contaminated, had homology with HOS/KHOS-240s cells and were human osteosarcoma cells. The cells were cultured in McCoy's 5A medium (Gibco; Thermo Fisher Scientific, Inc.) containing 10% FBS at 37°C in a 5% CO2 humidified incubator until cells reached the logarithmic growth phase; cells were then harvested for subsequent experiments.
MTT cell viability assay
U2OS cells (4×103 cells/well) and 143B cells (1×103 cells/well) were seeded in 96-well plates and incubated at 37°C in a 5% CO2 humidified incubator with different piperine concentrations (0, 50, 100 and 150 µM) for 24, 48 and 72 h. Subsequently, cell viability was determined using an MTT kit (Cell Titer 96AQ; Promega Corporation). The supernatant was aspirated and 0.05% DMSO (150 µl) was added to each well, and then shake at a low speed (3.2 g) for 10 min to fully dissolve the formazan. The optical density (OD) values of piperine-treated cells were measured at 490 nm using an ELISA microplate reader (Rt2100c; Rayto Life and Analytical Sciences Co., Ltd.). Inhibition rate %=(1-OD value of experimental group/OD value of 0 µM group) × 100%.
Flow cytometry
U2OS cells (5.0×104 cells/well) and 143B cells (1.0×104 cells/well) were seeded in 6-well plates and incubated at 37°C in 5% CO2 with different concentrations of piperine (0, 50, 100 and 150 µM) for 48 h. Cells were then harvested and 3 ml pre-chilled PBS was added at 4°C, which were centrifugated at 337 × g for 5 min at room temperature and 200 µl binding buffer was then used to suspend the supernatant. Next, double fluorescence staining was performed with 20 µg/ml PI and 5 µl Annexin V-FITC for 15 min at room temperature before analysis with a flow cytometer (Beckman CytoFLEX; Beckman Coulter, Inc.) and FlowJo software version 10.0.7 (Stanford University). Annexin V-FITC (green) and PI (red) fluorescence intensities were detected using the FITC channel (FL1) and PI channel (FL2), respectively. Total apoptotic rate was calculated as follows: Total apoptotic rate=early apoptotic rate + late apoptotic rate.
Transwell invasion assay
A Matrigel Transwell 24 holes with an aperture of 3.0 µm (Corning, Inc.) assay was performed to assess cell invasion. Matrigel matrix (50 mg/l; BD Biosciences) was diluted in serum-free medium at a 1:3 ratio to reconstitute the basement membrane. U2OS and 143B cells (5×104 cells/ml) were separately added to the upper Transwell chamber, and 10% FBS-containing culture medium containing different concentrations (50–150 µM) of piperine was added to the lower chamber. After incubation for 48 h at 37°C in 5% CO2, the cells in the upper chamber were fixed with 75% ethanol at room temperature for 10 min, stained with 0.1% crystal violet for 5 min at 37°C and examined using light microscopy (Olympus Corporation) at ×400 magnification. In total, five random visual fields were used to count the total number of migrating cells, and the images were analyzed using Image-Pro Plus 6.0 software (Media Cybernetics, Inc.).
Western blot analysis
U2OS and 143B cells were treated with different concentrations of piperine (0, 50, 100 and 150 µM) for 48 h prior to protein extraction at 37°C. After the cells were harvested and washed with RIPA buffer (Wuhan Servicebio Technology Co., Ltd.; cat. no. G2002) total protein from cells was extracted using a protein extraction kit (cat. no. KGBSP002; Nanjing KeyGen Biotech Co., Ltd.). Protein concentration was measured by bicinchonic acid protein kit (Wuhan Servicebio Technology Co., Ltd.) Proteins (20 µg) were then separated by SDS-PAGE with 10% gels. The separated protein bands were transferred onto nitrocellulose membranes blocked with 5% skimmed milk/TBST(0.1% Tween-20) at 37°C for 60 min, which were probed with the respective primary antibodies [Anti-MMP-2 (1:1,000; ProteinTech Group, Inc.) Anti-VEGF (1:3,000), anti-c-Myc (1:500), anti-cyclin D1 (1:1,000), anti-cyclooxygenase-2 (COX2; 1:500), anti-β-catenin (1:500) and anti-glycogen synthase kinase-3β (GSK-3β; 1:1,000; Wuhan Servicebio Technology Co., Ltd.)] overnight at 4°C. Subsequently, the membranes were incubated with a corresponding horseradish peroxidase-labeled secondary antibody (1:3,000; cat. no. 23301; Wuhan Servicebio Technology Co., Ltd.) for 30 min at room temperature, before being developed with an enhanced chemiluminescence reagent (Wuhan Servicebio Technology Co., Ltd.). Protein bands were analyzed using AlphaEaseFC software (ver 4.0.0; Alpha Innotech).
Statistical analysis
Statistical analyses were performed using SPSS version 16.0 software (SPSS, Inc.). Data from ≤3 independent experiments are presented as the mean ± SD. A one-way ANOVA followed by Bonferroni post-hoc analysis was performed to compare groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Piperine inhibits cell proliferation and induces apoptosis
MTT assay results indicated that piperine significantly inhibited U2OS and 143B cell proliferation (P<0.05; Fig. 1). It was revealed that cell density was reduced in the presence of piperine compared with untreated cells, with the lowest OD490 obtained for cells treated for 24 h with 150 µM piperine (P<0.01; Fig. 1A and C). Moreover, the strongest growth inhibition was observed in response to 150 µM piperine for 72 h (35% for U2OS and 35.7% for 143B; P<0.01; Fig. 1B and D). In U2OS cells, the apoptotic rate was positively associated with piperine concentration (Fig. 2). The apoptotic rate in the absence of piperine was 1.89%, whereas the apoptotic rates increased to 2.12, 4.63 and 19.1%, in the presence of 50, 100 and 150 µM piperine, respectively (P<0.05; Fig. 2A). For 143B cell the apoptotic rates was 10.29, 13.28, 24.85 and 36.7% in the presence of 0, 50, 100 and 150 µM piperine, respectively (P<0.05; Fig. 2B)
Figure 1.
Piperine inhibits U2OS and 143B cell proliferation, as determined by MTT assay. (A) U2OS and (C) 143B cell density OD490 profile of the control group (0 µM) and the piperine experimental groups at 24, 48 and 72 h after treatment. Inhibition rate %=(1-OD value of experimental group/OD value of 0 µM group) × 100%. Effect of piperine on percentage of (B) U2OS and (D) 143B cell growth inhibition at 24, 48, and 72 h after treatment. *P<0.05, **P<0.01 vs. Control (0 µM). #P<0.05, ##P<0.01 vs. Control (25 µM). OD, optical density.
Figure 2.
Piperine induces U2OS and 143B cells apoptosis. Flow cytometry profiles of Annexin V FITC/PI double stained (A) U2OS and (B) 143B cells after 48 h piperine treatment at 0µM, 50µM,100µM and 150 µM. C and D represent the apoptosis rate of U2OS and 143B cells after treatment with different concentrations of piperine for 48 h. **P<0.01 vs. Control (0 µM).
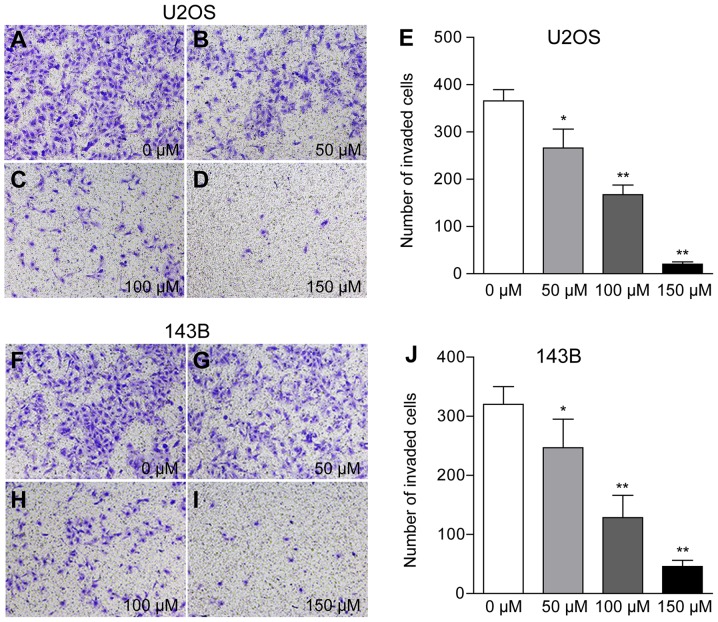
Piperine inhibits cell invasion by downregulating MMP-2 and VEGF protein expression
The present results suggested that osteosarcoma cells treated with 50, 100 and 150 µM piperine exhibited reduced cell(U2OS: Number of invading cells 266, 167 and 20 per field; 143B: 246, 128 and 45 per field, respectively; P<0.01; Fig. 3; Table I). Furthermore, western blotting results demonstrated a dose-dependent decrease in MMP-2 and VEGF protein expression levels in the presence of piperine, with the most significant reduction observed at 150 µM piperine for both proteins. However, with increasing concentration of piperine, U2OS had a more significant effect on MMP-2 and VEGF compared with 143B cells (Fig. 4).
Figure 3.
Transwell assay results showing piperine-mediated reduction in cell invasion. Images of (A-D) U2OS and (F-I) 143B cells treated with (A and F) 0, (B and G) 50, (C and H) 100 and (D and I) 150 µM piperine for 48 h. Magnification, ×100. (E and J) Semi-quantitative profile of microscopy images of piperine-treated U2OS cells.*P<0.05, **P<0.01 vs. 0 µM.
Table I.
Data from the Transwell assay
| Invaded cells | ||
|---|---|---|
| Treatment group, µM | U2OS | 143B |
| 0 | 365.6±23.8 | 320.3±30.0 |
| 50 | 266.2±39.7 | 246.9±48.3 |
| 100 | 167.2±20.6 | 128.5±37.7 |
| 150 | 20.4±4.8 | 45.8±10.2 |
Data are presented as the mean ± SD.
Figure 4.
Piperine downregulates VEGF and MMP-2 protein expression levels in U2OS and 143B cells. Western blot analysis of VEGF and MMP-2 protein expression levels in (A) U2OS and (C) 143B cells treated with 0, 50, 100 and 150 µM piperine. Actin was used as the loading control. (B and D) Semi-quantitative profiles of western blotting data of VEGF and MMP-2 at the four tested piperine concentrations. *P<0.05, **P<0.01 vs. 0 µM. MMP, matrix metalloproteinases; VEGF, vascular endothelial growth factor.
Piperine suppresses cell proliferation and invasion via the Wnt/β-catenin signaling pathway
Western blot analysis results revealed that the protein expression levels of GSK-3β and β-catenin were significantly reduced in U2OS cells after piperine treatment, and downregulation of these proteins was inversely associated with piperine concentration. Notably, the lowest protein expression levels were observed following treatment with 150 µM piperine (P<0.05; Fig. 5). In addition, reduced expression levels of the target proteins COX-2, cyclin D1 and c-myc were observed with increasing piperine concentrations (P<0.01; Fig. 5). In 143B cells, it was demonstrated that β-catenin protein expression was significantly reduced, and the expression levels of COX-2 and c-myc were decreased with increasing piperine concentrations.
Figure 5.
Effect of piperine treatment on the Wnt/β-catenin signaling pathway in U2OS and 143B cells. Western blot analysis of GSK-3β and β-catenin expression levels, and their target genes COX-2, cyclin D1 and c-myc after 48 h piperine treatment in (A) U2OS and (C) 143B cells. Actin was used as the loading control. (B and D) Semi-quantitative profile of the western blotting data. *P<0.05, **P<0.01 vs. 0 µM. COX-2, cyclooxygenase-2; GSK-3β, glycogen synthase kinase 3β.
Discussion
The present results suggested that piperine treatment increased apoptosis, and reduced cell invasion and proliferation of U2OS and 143B cells. Notably, cell proliferation was most significantly inhibited in response to treatment with the highest concentration of piperine (150 µM) for the longest treatment duration (72 h). Furthermore, the dose-dependent decrease observed in the protein expression levels of metastatic markers in the presence of piperine were in line with previous studies on the roles of these proteins in tumor metastasis and heterotopic angiogenesis (8,14,18). Therefore, the present results provided evidence on the role of piperine in inhibiting osteosarcoma cell proliferation and metastasis (21). In addition, the present western blotting results identified that the Wnt/β-catenin signaling pathway, which has a role in regulating osteosarcoma cell proliferation and apoptosis (31–34), may regulate piperine-mediated osteosarcoma apoptosis.
The core mediator of the Wnt/β-catenin signaling pathway, β-catenin, is regulated by phosphorylation, which is promoted by GSK-3β, and degradation via the ubiquitin/proteasome pathway (26). β-catenin mutations can cause abnormal activation of Wnt target genes, thus leading to cancer development (35). In addition, dysregulation of the Wnt signaling pathway can affect downstream gene expression (36). The present results suggested that piperine dose-dependently downregulated the protein expression levels of GSK-3β and β-catenin, as well as those of the downstream oncogenic proteins cyclin D1, c-Myc and COX-2. Therefore, piperine may effectively inhibit U2OS and 143B cell proliferation and metastasis, and ectopic angiogenesis via regulation of the Wnt/β-catenin signaling pathway. The PI3K/Akt pathway is frequently hyperactivated in osteosarcoma, and contributes to disease initiation and development (37). Moreover, inhibition of this pathway via small compounds is a potential therapeutic approach for osteosarcoma (38). Previous studies have shown that Wilms' tumor 1 knockdown in MG-63 cells results in deregulation of cell cycle proteins and downregulation of the PI3K/AKT pathway (39,40). Piperine has previously been reported to inhibit cell proliferation and metastasis of U2OS cells (21), and affect several signaling pathways, such as the Akt/MAPK and mTOR pathways (21,22,41), in several cancer cell types. However, to the best of our knowledge, the present study is the first to demonstrate that the Wnt/β-catenin signaling pathway may mediate the antitumor effects of piperine.
In the present study, it was demonstrated that piperine exerted a lower inhibitory effect on the 143B cell line compared with the U2OS cell line, and therefore, it was difficult to select a cell line to be used as control cells. Thus, the present study did not include a negative control. Furthermore, the cytotoxicity of piperine on healthy cells has not been thoroughly investigated in previous studies despite the well-characterized anticancer effects of piperine. However, it has been previously reported that piperine administration does not increase hepatorenal toxicity in nude mice (42,43). Thus, piperine may not cause osteosarcoma-specific cytotoxic effects.
In relation to the modest antitumor efficacy of piperine shown in the present study, further in vivo and clinical experiments are required to evaluate its efficacy on osteosarcoma proliferation, and to clarify the underlying molecular mechanisms. In addition, future studies will investigate whether combination drug treatment with cisplatin increases antitumor potency on osteosarcoma growth. The present study did not use agonists or antagonists to confirm the involvement of the Wnt/β-catenin pathway. However, the present study proposed that the expression levels of upstream signaling molecules in the Wnt/β-catenin pathway, such as β-catenin and GSK-3β, as well as the downstream target proteins COX-2, cyclin D1 and c-myc, could demonstrate the involvement of the Wnt/β-catenin pathway in piperine-mediated osteosarcoma inhibition. Furthermore, future in vivo experiments will use specific agonists and inhibitors of the Wnt/β-catenin pathway.
In conclusion, the present results suggested that the Wnt/β-catenin signaling pathway underlies the antitumor effects of piperine on U2OS and 143B cell proliferation, apoptosis and invasion. However, further research is needed to investigate the anti-osteosarcoma mechanism of piperine.
Acknowledgements
The authors would like to thank Professor Ming Zhang and Assistant Researcher Wenxia Li of Key Laboratory of Cardiovascular Remolding and Function Research Chinese Ministry of Health for their help in the present study.
Glossary
Abbreviations
- COX-2
cyclooxygenase-2
- GSK-3β
glycogen synthase kinase-3β
- MMP-2
matrix metalloproteinase-2
- VEGF
vascular endothelial growth factor
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
LN contributed to the conception of the study. YBQ performed the experiments, data analysis and wrote the manuscript. WY and MS contributed to data interpretation and analyses. All authors have read and approved the manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Petriceks AH, Salmi D. Educational case: Primary osteosarcoma. Acad Pathol. 2019;6:2374289518820337. doi: 10.1177/2374289518820337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pu F, Chen F, Chen S, Wang B, Liu J, Shao Z. Association between GSTP1 polymorphisms and prognosis of osteosarcoma in patients treated with chemotherapy: A meta-analysis. Onco Targets Ther. 2015;8:1835–1842. doi: 10.2147/OTT.S81115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van de Luijtgaarden AC, Kapusta L, Bellersen L, Bokkerink JP, Kaal SE, Versleijen-Jonkers YM, Schreuder HW, van der Graaf WT. High prevalence of late adverse events in malignant bone tumour survivors diagnosed at adult age. Neth J Med. 2014;72:516–522. [PubMed] [Google Scholar]
- 4.Whelan J, McTiernan A, Cooper N, Wong YK, Francis M, Vernon S, Strauss SJ. Incidence and survival of malignant bone sarcomas in England 1979–2007. Int J Cancer. 2012;131:E508–E517. doi: 10.1002/ijc.26426. [DOI] [PubMed] [Google Scholar]
- 5.Castillo-Tandazo W, Mutsaers AJ, Walkley CR. Osteosarcoma in the post genome Era: Preclinical models and approaches to identify tractable therapeutic targets. Curr Osteoporos Rep. 2019;17:343–352. doi: 10.1007/s11914-019-00534-w. [DOI] [PubMed] [Google Scholar]
- 6.Moore DD, Luu HH. Osteosarcoma. Cancer Treat Res. 2014;162:65–92. doi: 10.1007/978-3-319-07323-1_4. [DOI] [PubMed] [Google Scholar]
- 7.Zheng J, Zhou Y, Li Y, Xu DP, Li S, Li HB. Spices for prevention and treatment of cancers. Nutrients. 2016;8:E495. doi: 10.3390/nu8080495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parthasarathy N, Selwyn MA, Udayakumar M. Tropical dry evergreen forests of 627 peninsular India: Ecology and conservation significance. Trop Conservation Sci. 2008;1:89–110. doi: 10.1177/194008290800100203. [DOI] [Google Scholar]
- 9.Mehmood MH, Gilani AH. Pharmacological basis for the medicinal use of black pepper and piperine in gastrointestinal disorders. J Med Food. 2010;13:1086–1096. doi: 10.1089/jmf.2010.1065. [DOI] [PubMed] [Google Scholar]
- 10.Liu J, Chen M, Wang X, Wang Y, Duan C, Gao G, Lu L, Wu X, Wang X, Yang H. Piperine induces autophagy by enhancing protein phosphotase 2A activity in a rotenone-induced Parkinson's disease model. Oncotarget. 2016;7:60823–60843. doi: 10.18632/oncotarget.11661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aumeeruddy MZ, Mahomoodally MF. Combating breast cancer using combination therapy with 3 phytochemicals: Piperine, sulforaphane, and thymoquinone. Cancer. 2019;125:1600–1611. doi: 10.1002/cncr.32022. [DOI] [PubMed] [Google Scholar]
- 12.Lin Y, Xu J, Liao H, Li L, Pan L. Piperine induces apoptosis of lung cancer a549 cells via p53-dependent mitochondrial signaling pathway. Tumour Biol. 2014;35:3305–3310. doi: 10.1007/s13277-013-1433-4. [DOI] [PubMed] [Google Scholar]
- 13.Bhardwaj RK, Glaeser H, Becquemont L, Klotz U, Gupta SK, Fromm MF. Piperine, a major constituent of black pepper, inhibits human p-glycoprotein and cyp3a4. J Pharmacol Exp Ther. 2002;302:645–650. doi: 10.1124/jpet.102.034728. [DOI] [PubMed] [Google Scholar]
- 14.Sunila ES, Kuttan G. Immunomodulatory and antitumor activity of piper longum linn and piperine. J Ethnopharmacol. 2004;90:339–346. doi: 10.1016/j.jep.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 15.Greenshields AL, Doucette CD, Sutton KM, Madera L, Annan H, Yaffe PB, Knickle AF, Dong Z, Hoskin DW. Piperine inhibits the growth and motility of triple-negative breast cancer cells. Cancer Lett. 2015;357:129–140. doi: 10.1016/j.canlet.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 16.Gunasekaran V, Elangovan K, Niranjali Devaraj S. Targeting hepatocellular carcinoma with piperine by radical-mediated mitochondrial pathway of apoptosis: An in vitro and in vivo study. Food Chem Toxicol. 2017;105:106–118. doi: 10.1016/j.fct.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 17.Hwang YP, Yun HJ, Kim HG, Han EH, Choi JH, Chung YC, Jeong HG. Suppression of phorbol-12-myristate-13-acetate-induced tumor cell invasion by piperine via the inhibition of PKCα/ERK1/2-dependent matrix metalloproteinase-9 expression. Toxicol Lett. 2011;203:9–19. doi: 10.1016/j.toxlet.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 18.Pathak N, Khandelwal S. Cytoprotective and immunomodulating properties of piperine on murine splenocytes: An in vitro study. Eur J Pharmacol. 2007;576:160–170. doi: 10.1016/j.ejphar.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 19.Taqvi SI, Shah AJ, Gilani AH. Blood pressure lowering and vasomodulator effects of piperine. J Cardiovasc Pharmacol. 2008;52:452–458. doi: 10.1097/FJC.0b013e31818d07c0. [DOI] [PubMed] [Google Scholar]
- 20.Wattanathorn J, Chonpathompikunlert P, Muchimapura S, Priprem A, Tankamnerdthai O. Piperine, the potential functional food for mood and cognitive disorders. Food Chem Toxicol. 2008;46:3106–3110. doi: 10.1016/j.fct.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Zhu X, Li H, Li B, Sun L, Xie T, Zhu T, Zhou H, Ye Z. Piperine inhibits proliferation of human osteosarcoma cells via G2/M phase arrest and metastasis by suppressing MMP-2/-9 expression. Int Immunopharmacol. 2015;24:50–58. doi: 10.1016/j.intimp.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 22.Pan H, Xu LH, Huang MY, Zha QB, Zhao GX, Hou XF, Shi ZJ, Lin QR, Ouyang DY, He XH. Piperine metabolically regulates peritoneal resident macrophages to potentiate their functions against bacterial infection. Oncotarget. 2015;6:32468–32483. doi: 10.18632/oncotarget.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oudin MJ, Weaver VM. Physical and chemical gradients in the tumor microenvironment regulate tumor cell invasion, migration, and metastasis. Cold Spring Harb Symp Quant Biol. 2016;81:189–205. doi: 10.1101/sqb.2016.81.030817. [DOI] [PubMed] [Google Scholar]
- 24.Li H, Zhang K, Liu LH, Ouyang Y, Bu J, Guo HB, Xiao T. A systematic review of matrix metalloproteinase 9 as a biomarker of survival in patients with osteosarcoma. Tumour Biol. 2014;35:5487–5491. doi: 10.1007/s13277-014-1717-3. [DOI] [PubMed] [Google Scholar]
- 25.Fromigue O, Hamidouche Z, Marie PJ. Blockade of the RhoA-JNK-c-Jun-MMP2 cascade by atorvastatin reduces osteosarcoma cell invasion. J Biol Chem. 2008;283:30549–30556. doi: 10.1074/jbc.M801436200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ling L, Nurcombe V, Cool SM. Wnt signaling controls the fate of mesenchymal stem cells. Gene. 2009;433:1–7. doi: 10.1016/j.gene.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 27.Peng N, Gao S, Guo X, Wang G, Cheng C, Li M, Liu K. Silencing of VEGF inhibits human osteosarcoma angiogenesis and promotes cell apoptosis via VEGF/PI3K/AKT signaling pathway. Am J Transl Res. 2016;8:1005–1015. [PMC free article] [PubMed] [Google Scholar]
- 28.Manzano-Moreno FJ, Costela-Ruiz VJ, Melguizo-Rodríguez L, Illescas-Montes R, García-Martínez O, Ruiz C, Ramos-Torrecillas J. Inhibition of VEGF gene expression in osteoblast cells by different NSAIDs. Arch Oral Biol. 2008;92:75–78. doi: 10.1016/j.archoralbio.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 29.Olivares-Navarrete R, Hyzy S, Wieland M, Boyan BD, Schwartz Z. The roles of Wnt signaling modulators Dickkopf-1 (Dkk1) and Dickkopf-2 (Dkk2) and cell maturation state in osteogenesis on microstructured titanium surfaces. Biomaterials. 2010;31:2015–2024. doi: 10.1016/j.biomaterials.2009.11.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tian J, He H, Lei G. Wnt/β-catenin pathway in bone cancers. Tumour Biol. 2014;35:9439–9445. doi: 10.1007/s13277-014-2433-8. [DOI] [PubMed] [Google Scholar]
- 31.Brafman D, Willert K. Wnt/β-catenin signaling during early vertebrate neural development. Dev Neurobiol. 2017;77:1239–1259. doi: 10.1002/dneu.22517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Di Fiore R, Guercio A, Puleio R, Di Marco P, Drago-Ferrante R, D'Anneo A, De Blasio A, Carlisi D, Di Bella S, Pentimalli F, et al. Modeling human osteosarcoma in mice through 3AB-OS cancer stem cell xenografts. J Cell Biochem. 2012;113:3380–3392. doi: 10.1002/jcb.24214. [DOI] [PubMed] [Google Scholar]
- 33.Katoh M, Katoh M. Molecular genetics and targeted therapy of WNT-related human diseases (Review) Int J Mol Med. 2017;40:587–606. doi: 10.3892/ijmm.2017.3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krishnamurthy N, Kurzrock R. Targeting the Wnt/beta-catenin pathway in cancer: Update on effectors and inhibitors. Cancer Treat Rev. 2018;62:50–60. doi: 10.1016/j.ctrv.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ng TL, Gown AM, Barry TS, Cheang MC, Chan AK, Turbin DA, Hsu FD, West RB, Nielsen TO. Nuclear beta-catenin in mesenchymal tumors. Mod Pathol. 2005;18:68–74. doi: 10.1038/modpathol.3800272. [DOI] [PubMed] [Google Scholar]
- 36.Ghosh N, Hossain U, Mandal A, Sil PC. The wnt signaling pathway: A potential therapeutic target against cancer. Ann N Y Acad Sci. 2019;1443:54–74. doi: 10.1111/nyas.14027. [DOI] [PubMed] [Google Scholar]
- 37.Zhang X, Qu P, Zhao H, Zhao T, Cao N. Cox 2 promotes epithelial-mesenchymal transition and migration in osteosarcoma MG 63 cells via PI3K/AKT/NF kB signaling. Mol Med Rep. 2019;20:3811–3819. doi: 10.3892/mmr.2019.10598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu G, Yuan D, Sun P, Liu W, Wu PF, Liu H, Yu GY. Linc00968 functions as an oncogene in osteosarcoma by activating the PI3K/AKT/mTOR signaling. J Cell Physiol. 2018;233:8639–8647. doi: 10.1002/jcp.26624. [DOI] [PubMed] [Google Scholar]
- 39.Zhang J, Yu XH, Yan YG, Wang C, Wang WJ. PI3K/Akt signaling in osteosarcoma. Clin Chim Acta. 2015;444:182–192. doi: 10.1016/j.cca.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 40.Graziano AC, Cardile V, Avola R, Vicario N, Parenti C, Salvatorelli L, Magro G, Parenti R. Wilms' tumor gene 1 silencing inhibits proliferation of human osteosarcoma MG-63 cell line by cell cycle arrest and apoptosis activation. Oncotarget. 2017;8:13917–13931. doi: 10.18632/oncotarget.14715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Perry JA, Kiezun A, Tonzi P, Van Allen EM, Carter SL, Baca SC, Cowley GS, Bhatt AS, Rheinbay E, Pedamallu CS, et al. Complementary genomic approaches highlight the PI3K/mTOR pathway as a common vulnerability in osteosarcoma. Proc Natl Acad Sci USA. 2014;111:E5564–E5573. doi: 10.1073/pnas.1419260111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yoo ES, Choo GS, Kim SH, Woo JS, Kim HJ, Park YS, Kim BS, Kim SK, Park BK, Cho SD, et al. Antitumor and apoptosis-inducing effects of piperine on human melanoma cells. Anticancer Res. 2019;39:1883–1892. doi: 10.21873/anticanres.13296. [DOI] [PubMed] [Google Scholar]
- 43.Lai LH, Fu QH, Liu Y, Jiang K, Guo QM, Chen QY, Yan B, Wang QQ, Shen JG. Piperine suppresses tumor growth and metastasis in vitro and in vivo in a 4T1 murine breast cancer model. Acta Pharmacol Sin. 2012;33:523–530. doi: 10.1038/aps.2011.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.