Abstract
Background
Taiwan experienced one of the most serious outbreaks of severe acute respiratory syndrome (SARS) during the 2003 epidemic. Public health nurses faced unprecedented challenges in implementing an extensive quarantine policy to prevent disease spread. Their professional confidence, however, was shattered during the SARS crisis. This paper assesses factors related to public health nurses' confidence in managing community SARS control programs.
Methods
In May 2003, we sent structured questionnaires to all 361 health centers in Taiwan and asked the public health nurses responsible for epidemic control to complete. A total of 312 completed surveys were returned for a response rate of 86.4%. Descriptive methods and logistic regression were used to analyze the data.
Results
Most public health nurses (71.9%) expressed a general lack of confidence in handling the SARS epidemic. Confidence was significantly associated with perceived epidemic severity (OR, 0.58; 95% CI: 0.35-0.99), daily epidemic updates (OR, 2.26; 95% CI: 1.28-3.98), and number of cases in the community (OR, 2.21; 95% CI: 1.13-4.31).
Conclusion
Nurses' individual risk perception and prompt update of epidemic information significantly affect levels of professional confidence, a key factor influencing quarantine implementation success. Strategies to promote productive interagency collaboration and advocate participatory policy making involving health workers at all levels are needed to control effectively infectious disease outbreaks.
The global spread of severe acute respiratory syndrome (SARS) in 2003 was a prelude to other emerging infectious diseases in the 21st Century.1 Recent outbreaks of H5N1 avian influenza in Asia continue to remind the world of the threat of periodic and unpredictable recurrences of pandemic contagion.2
Since the beginning of the SARS outbreak, many scientists have worked to characterize the coronavirus,3, 4 trace epidemic patterns,5 and synthesize potential vaccines to prevent further outbreaks.6, 7 However, the global experience of managing SARS has revealed that reducing contact between people by implementing quarantine measures is as important as discovering effective remedies.8, 9
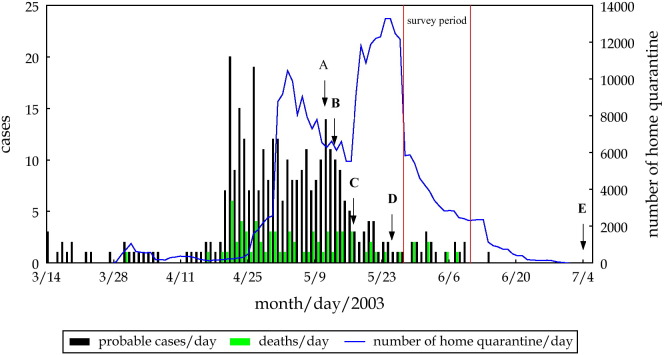
Taiwan reported 346 probable SARS cases and 73 SARS-related deaths during the outbreak in 2003, making it one of the most serious SARS epidemic areas in the world10, 11 Figure 1 shows the chronology of the 2003 SARS epidemic in Taiwan. Facing this unprecedented outbreak, the Taiwan government began implementation of compulsory home quarantine on March 28 to stop community transmission.12 Individuals who were suspected to have been infected with SARS were quarantined at home (or in special facilities) for 10 to 14 days. In those 4 months of the epidemic period, 131,132 individuals were quarantined in Taiwan. This includes 50,319 people who had close contact with SARS patients and 80,813 travelers who came to Taiwan from World Health Organization (WHO)-designated SARS-affected areas.11, 13
Fig 1.
Probable SARS cases per day, SARS deaths per day, and number of home quarantines per day in Taiwan during SARS outbreak period (March 14 to July 4, 2003). (A) WHO estimated that the Taiwan epidemic situation might be under control within 6 to 7 weeks (at the end of June). (B) Taiwan anti-SARS task force commander said it did not need 7 weeks to control the outbreak (at the end of June). (C) Taiwan premier said that the outbreak would be over by the end of June. (D) Taiwan anti-SARS task force commander said the epidemic situation was stable and advised people to return to their routine. (E) WHO removed Taiwan from its list of areas to which travelers were advised to avoid for all but essential travel.
Public health administration in Taiwan is organized at 3 levels: national, city/county, and township. Generally speaking, national health policies are often formulated in the National Department of Health (DOH) with participation of city/county health bureau officials. The health centers (or health stations, as they are called) are the local agencies situated in the townships. The major responsibility of health centers is to implement public health protocols developed at the national and city/county levels. The directors of health centers are usually licensed physicians. Public health nurses are usually the supporting staff who carry out program assignments. The public health operation in Taiwan is managed under this clear chain of command. Under this system, Taiwan eradicated malaria infection in the 1960s, succeeded in having 82% of all married women aged 22 to 39 years practice contraception in the 1970s, and dropped 84% of hepatitis B carriers in the 1980s. Public health nurses working at the local health centers played a key role in achieving public health success in Taiwan.14 However, the public health nurses were unprepared in 2003 at the time of the SARS crisis.
SARS hit Taiwan in March 2003. In response to the outbreak, the DOH created an emergency operation office and appointed an anti-SARS task force commander to direct a comprehensive national SARS control program. Home quarantine was ordered for all suspected SARS cases. Health centers at all localities were asked to implement the home quarantine policy. Local public health nurses were not invited to participate in the national SARS control policy making but were requested to carry out the mission.
During the quarantine period, public health nurses were requested to undertake several public health measures, which included conducting initial registration, maintaining daily temperature records, disposing of personal trash, and providing social support and advice on medical care to those with a fever or SARS-related symptoms. Success in quarantine management was considered a crucial factor in the successful control of SARS. However, it was soon evident that public health nurses' lack of experience in managing community quarantine and their fear of being infected with SARS presented a major challenge.
This study was designed to understand better the challenges and threats facing public health nurses responsible for implementing SARS quarantine procedures. The results will be valuable for developing better strategies for controlling the rapid spread of infectious diseases such as SARS.
Methods
Questionnaire development
An attitudinal questionnaire was developed by researchers in May 2003 at the peak of the Taiwan SARS epidemic. Questionnaire items were designed on the basis of the working experience of a panel of public health nurses. The questionnaire went through a content validation process. Six experts from public health or community nursing fields served as the expert panel in checking the validity of questionnaire items. The drafted questionnaire was piloted for understandability among 5 public health nurses in northern Taiwan. Moreover, within 1 week after the questionnaires were returned, the researchers randomly selected and phoned 32 respondents (approximately 10% of the total) to check the reliability of their written answers. The test/retest reliability for this questionnaire was high (Pearson correlation coefficients for continuous variables: 0.87-0.97; Spearman rank correlation coefficients for categorical variables: 0.90-0.97).
One section of the questionnaire was designed to collect baseline information, including (1) demographics, (2) number of quarantined cases managed and responsibilities within the previous week (itemizing quarantine-related extra workload), and (3) the date the nurses predicted SARS epidemic would end. Another section (using categorical scales) asked about SARS-related operations that included the frequency of (1) epidemic information updated in the health center, (2) SARS-related training courses received, and (3) assistance of community volunteers on quarantine measures. The third section contained questions (using 10-point Likert scale: 1 = the worst to 10 = the best) about the effectiveness of the nurse's institution in managing the SARS epidemic, including the nurse's assessment of (1) the institutional functioning on community home quarantine, (2) the quality of training received for controlling infectious disease outbreaks, and (3) the adequacy of support (for both manpower and financing) received from superior health agencies (DOH or city/county health bureaus). In the fourth section of the questionnaire (also using 10-point Likert scale), the nurses were asked to assess the severity of the epidemic, the public's awareness of the epidemic situation, the public's fear of SARS, and the public's compliance with official quarantine measures. Finally, the nurses were asked to list major difficulties they encountered in managing the SARS epidemic.
Data collection procedures
The main island of Taiwan has a total of 361 health centers. On May 26, 2003, 1 questionnaire was mailed to each of the 361 health centers to be completed by the head nurse or the nurse in charge of SARS epidemic control. A reminder letter was sent 1 week later to nonresponding centers. A total of 312 completed surveys were returned for a response rate of 86.4%.
Data analysis
Logistic regression was used to identify variables associated with the nurses' lack of confidence in SARS control. Nurses who estimated that the SARS epidemic would not be declared “ended” by the WHO until mid-September 2003 or later (the WHO declared Taiwan SARS free on July 5) were categorized as “less confident.” Logistic regression also identified variables associated with public compliance of official anti-SARS measures. Variables in univariate models that exerted a significant effect were subjected to multivariate logistics to assess significance level. Statistical analyses were performed using SAS 8.01 (SAS Institute Inc., Cary, NC). All reported P values were 2-sided; P < .05 was considered statistically significant.
Results
As shown in Table 1, approximately half (49%) of the respondents were 40 to 49 years of age, one third (33%) 30 to 39 years, and 15% older than 50 years. Most respondents (70%) had at least 10 years of experience working in a health center. Approximately 28% of respondents believed the SARS outbreak would be controlled by mid-July; the remainder of the respondents believed control would not occur until mid-September (38%), mid-December, or later (29%). Many public health nurses encountered difficulties while performing SARS-related duties. They expressed dissatisfaction with the shortage of protective equipment such as N95 masks and gloves (44%), public resistance to following protection measures (42%), poor interagency communication (37%), and lack of standard operating procedures (30%).
Table 1.
Demographic characteristics of interviewees, their confidence in SARS control, and major difficulties encountered when performing SARS-related measures
| N | % | |
|---|---|---|
| Age (yr) | 301 | |
| ≤30 | 12 | 4.0 |
| 30-39 | 99 | 32.9 |
| 40-49 | 146 | 48.5 |
| ≥50 | 44 | 14.6 |
| Years working in health centers | 304 | |
| ≤10 | 93 | 30.6 |
| 10-19 | 94 | 30.9 |
| 20-29 | 108 | 35.5 |
| ≥30 | 9 | 3.0 |
| Date predicted for control of SARS outbreak in Taiwan | 306 | |
| By July 2003 | 10 | 3.3 |
| By mid-July 2003 | 76 | 24.8 |
| By mid-September 2003 | 116 | 37.9 |
| By mid-December 2003 | 88 | 28.8 |
| Not until 2004 or uncontrollable | 16 | 5.2 |
| Major difficulties encountered during the SARS epidemic period | 312 | |
| Inadequate self-protection equipment provided | 138 | 44.3 |
| People's reluctance to follow official measures | 131 | 42.0 |
| Poor communication among agencies involved | 114 | 36.5 |
| Lack of standard operating procedures | 92 | 29.5 |
As shown in Table 2, nurses' perceptions of epidemic severity were negatively associated with confidence that the epidemic could be controlled (OR, 0.58; 95% CI: 0.35-0.99). Nurses in health centers receiving fewer epidemic updates were more likely to doubt the effectiveness of epidemic control measures (OR, 2.26; 95% CI: 1.28-3.98). Nurses working in areas with relatively fewer probable SARS cases were less confident in control efforts (OR, 2.21; 95% CI: 1.13-4.31).
Table 2.
Factors contributing to a loss of nurse confidence in controlling the SARS outbreak∗
| Univariate |
Multivariate |
|||
|---|---|---|---|---|
| 95% CI | OR | 95% CI | OR | |
| Public health nurse characteristics | ||||
| Working experience (≤10 yr/>10 yr) | 0.96 | 0.56-1.66 | 0.90 | 0.51-1.59 |
| Perceived epidemic severity (less severe/more severe)† | 0.63 | 0.38-1.05 | 0.58 | 0.35-0.99‡ |
| Public responses | ||||
| Awareness of current SARS epidemic (less/more)† | 1.04 | 0.63-1.71 | ||
| Perceived fear of SARS epidemic (less/more)† | 0.86 | 0.50-1.40 | ||
| Compliance with official measures (poor/good)† | 0.97 | 0.56-1.69 | ||
| Working environment in health centers | ||||
| Functioning on community home quarantine (less/more)† | 1.08 | 0.65-1.81 | ||
| Human resources/financial support from higher health authorities (less/more)† | 1.88 | 1.03-3.43‡ | 1.66 | 0.90-3.09 |
| Updated epidemic information daily (no/yes) | 2.02 | 1.18-3.47‡ | 2.26 | 1.28-3.98‡ |
| Volunteer help (no/yes) | 1.38 | 0.83-2.29 | ||
| Staff training (no/yes) | 1.40 | 0.70-2.82 | ||
| SARS outbreak severity at local level | ||||
| Total probable cases reported in the county (<20/≥20) | 2.02 | 1.18-3.47‡ | 2.21 | 1.13-4.31‡ |
| Number of quarantined persons covered by a nurse (≥4/<4) | 1.58 | 0.96-2.61 | ||
N = 306 nurses reported loss of confidence (306 nurses completed the questionnaire items used in these two logistic regressions).
Cut-off points based on median scores of respective questions measured on a 10-point Likert scale.
P < .05.
Several factors contributed to the public's lack of cooperation with SARS-related home quarantine measures ( Table 3). According to the nurses, people were less likely to cooperate with quarantine measures when (1) they were less knowledgeable about SARS (OR, 3.66; 95% CI: 1.99-6.75), (2) they expressed less fear of SARS (OR, 3.39; 95% CI: 1.85-6.21), (3) the health centers were not functioning well (OR, 2.16; 95% CI: 1.17-4.00), and (4) the health centers received inadequate manpower or financial support from higher health authorities (OR, 2.67; 95% CI: 1.33-5.38).
Table 3.
Factors contributing to poor compliance by the general public with official measures aimed at SARS epidemic control∗
| Univariate |
Multivariate |
|||
|---|---|---|---|---|
| 95% CI | OR | 95% CI | OR | |
| Public health nurse characteristics | ||||
| Working experience (≤10 yr/>10 yr) | 1.51 | 0.86-2.66 | 1.12 | 0.60-2.10 |
| Perceived epidemic severity (less severe/severer)† | 1.78 | 1.09-2.94‡ | 1.15 | 0.65-2.03 |
| Public responses | ||||
| Awareness of current SARS epidemic (less/more)† | 3.12 | 1.85-5.28‡ | 3.66 | 1.99-6.75‡ |
| Perceived fear of SARS epidemic (less/more)† | 2.50 | 1.51-4.13‡ | 3.39 | 1.85-6.21‡ |
| Working environment in health centers | ||||
| Functioning on community home quarantine (less/more)† | 3.00 | 1.71-5.27‡ | 2.16 | 1.17-4.00‡ |
| Human resources/financial support from higher health authorities (less/more)† | 2.66 | 1.41-5.02‡ | 2.67 | 1.33-5.38‡ |
| Updated epidemic information daily (no/yes) | 1.76 | 1.04-2.97‡ | 1.31 | 0.73-2.34 |
| Volunteer help (no/yes) | 1.24 | 0.75-2.05 | ||
| Staff training (no/yes) | 1.22 | 0.62-2.37 | ||
| SARS outbreak severity at local level | ||||
| Total probable cases reported in the county (<20/≥20) | 0.70 | 0.34-1.44 | ||
| Number of quarantined persons cared for by a public health nurse (<4/≥4) | 0.74 | 0.45-1.23 | ||
N = 301 nurses reported poor compliance (301 nurses completed the questionnaire items used in these two logistic regressions).
Cut-off points were based on median scores of respective questions that were measured by a 10-point Likert scale.
P < .05.
Discussion
This study is the only study reporting on the assessment of frontline nurses' reactions to home quarantines implemented by most health centers in Taiwan during the 2003 SARS outbreak. Survey respondents were mainly head nurses with more than 10 years of health center experience and were very familiar with their organizations, clients, communities, and issues surrounding quarantine operations. Furthermore, because they were required to interact directly with quarantined persons, they had the best opportunity to understand the community's response to the SARS outbreak.15 Also, because the survey was conducted just after the SARS epidemic had peaked, the related experiences were fresh in their minds, and recall bias would have been minimal. Therefore, this report can be a valuable reference for the control and management of SARS-like contagious disease outbreaks.
The WHO removed Taiwan from its list of SARS-infected areas on July 5, 200316; however, even at the beginning of June, many Taiwanese, including public health officials and lay people, remained pessimistic about the success of SARS control measures. As shown in Table 1, most public health nurses (71.9%) believed that the outbreak would not end until mid-September or even later. There was at least a 2-month difference between frontline nurses' estimates and the actual timing of the epidemic's end, indicating a low confidence level on the part of the nurses. This is serious because the pessimistic attitudes of nurses could affect the morale of quarantined subjects, people in the community, and, eventually, the success of the SARS control program.
Why did public health nurses lack confidence in implementing the anti-SARS program? As shown in Table 2, individual risk perception, working environment of the health centers, and epidemic severity in the community were contributing factors. During the SARS epidemic, the Taiwan government made efforts, via media announcements, to assure the public that the situation was under control. From May 2003, all major television channels broadcast daily the “SARS Front-line” program on the evening news. The premier and the commander of the Anti-SARS Task Force also repeatedly delivered public announcements that said the outbreak would soon be over.17, 18, 19 However, these optimistic public announcements were not always trusted by frontline nurses. The daily epidemic reports received by the nurses always seemed to be outdated. As the severity of the epidemic lessened day by day, the outdated data that showed a more severe phase of epidemic were counterproductive to boosting nurses' trust in the government's optimistic announcements. It appears that providing public health nurses with rapidly updated information is of utmost importance. Results also show that risk communication at the time of infectious disease outbreak should be based on timely, rapidly updated, and evidence-based data to supplement routine government announcements.
We determined whether nurse confidence in epidemic control measures was a function of extra hours and activities required for managing the epidemic. Results indicated that lower confidence levels were associated with fewer cases in the community (Table 2). Without an immediate threat, health centers in counties/cities with few SARS cases might not have fully mobilized their community resources to prepare the public or their nurses for SARS prevention and control measures. Because the national media broadcasted sensationally on the severity of SARS epidemics, public health nurses without sufficient preparation and support might have been more vulnerable to rumors and speculation about negative aspects of the outbreak such as mortality rate, resulting in a loss of confidence in organized efforts to control the SARS epidemic.
Another factor contributing to nurses' low confidence may be related to their lack of opportunity to participate in the formation of national policy, which they are asked to implement at the local level. According to the aforementioned traditional chain of command in the Taiwanese public health bureaucracy, when the SARS policy was developed, standard procedures for field operations were decided by the national office. Without having policy fine-tuned with input from frontline nurses, this top-down policy could not promptly respond to local needs that changed rapidly according to the disastrous nature of SARS contingencies. It is obvious that the long-established champion of the Taiwanese public health system needs an effective feedback mechanism to renovate its response to newly emerging infectious outbreaks. A platform that encourages participatory decision making involving health professionals at all levels should be critically emphasized in developing a national policy to control SARS-like outbreaks of pandemic contagion.
Frontline nurses reported that one of the most frustrating experiences during the SARS epidemic was the reluctance of people to follow quarantine guidelines. This was independent of local epidemic severity but significantly related to people's cognitive preparedness and the efficiency of interagency collaborations (Table 3). Quarantine restricts the movement of people who can potentially expose others to a disease.20, 21 How to implement effectively a community-wide quarantine therefore presents a major challenge to health agencies. Table 3 shows that people who were less knowledgeable about the SARS outbreak and those who expressed little fear of infection were less compliant in following anti-SARS measures. In the future, more efforts should be placed on educating people to increase their health knowledge and beliefs, especially about risk susceptibility and severity, and belief in the benefits of taking health actions.22, 23 Moreover, effective community health education programs that emphasize community-based participatory research and education should be considered.24, 25 From a national perspective, a comprehensive SARS control strategy should also be developed that would streamline communication and resource sharing among health agencies at all levels.
In summary, public health nurses' confidence in the control of a SARS outbreak and people's compliance with quarantine measures are 2 major factors that can affect the success of a SARS-control program. Other important determinants to a successful program include effective risk communication, participatory policy making that involves health workers at all levels, and intergovernmental collaboration at national and local levels. Factors critical to SARS management are similar to those for crisis management of avian influenza outbreaks and of the results of terrorist acts.26, 27, 28, 29 Lessons learned in this study can serve as useful guidelines to prevent and manage emerging infectious disease outbreaks.
Zhunan Town, Taiwan; Taipei, Taiwan; and New Orleans, Louisiana
References
- 1.Ziebuhr J. SARS: unprecedented global response to a newly emerging disease. Int J Med Microbiol. 2003;293:229–231. doi: 10.1078/1438-4221-00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tracy C.S., Upshur R.E., Daar A.S. Avian influenza and pandemics. N Engl J Med. 2005;352:1928. doi: 10.1056/NEJM200505053521819. [DOI] [PubMed] [Google Scholar]
- 3.Lai M.M. SARS virus: the beginning of the unraveling of a new coronavirus. J Biomed Sci. 2003;10(6 Pt 2):664–675. doi: 10.1007/BF02256318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stadler K., Masignani V., Eickmann M., Becker S., Abrignani S., Klenk H.D. SARS: beginning to understand a new virus. Nat Rev Microbiol. 2003;1:209–218. doi: 10.1038/nrmicro775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng T.W., Turinici G., Danchin A. A double epidemic model for the SARS propagation. BMC Infect Dis. 2003;3:19. doi: 10.1186/1471-2334-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fujii T., Nakamura T., Iwamoto A. Current concepts in SARS treatment. J Infect Chemother. 2004;10:1–7. doi: 10.1007/s10156-003-0296-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cinatl J., Morgenstern B., Bauer G., Chandra P., Rabenau H., Doerr H.W. Treatment of SARS with human interferons. Lancet. 2003;362:293–294. doi: 10.1016/S0140-6736(03)13973-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pang X., Zhu Z., Xu F., Guo J., Gong X., Liu D. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. JAMA. 2003;290:3215–3221. doi: 10.1001/jama.290.24.3215. [DOI] [PubMed] [Google Scholar]
- 9.Madani T.A. Preventive strategies to keep Saudi Arabia SARS-free. Am J Infect Control. 2004;32:120–121. doi: 10.1016/j.ajic.2003.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsieh Y.H. SARS and the Internet. N Engl J Med. 2003;349:711–712. doi: 10.1056/NEJMc031470. [DOI] [PubMed] [Google Scholar]
- 11.Center for Disease Control Taiwan. Information below was mainly re-classified according to the current SARS definition and test results in laboratory from WHO. Center for Disease Control Taiwan, R.O.C., 2003. Available at: http://www.cdc.gov.tw/sars/4%B0%EA%A4%BASARS%AC%DB%C3%F6%B8%EA%B0T/%A5x%C6WSARS%AC%CC%B1%A1%B2%7B%AAp.htm. Accessed August 14, 2003.
- 12.Twu S.J., Chen T.J., Chen C.J., Olsen S.J., Lee L.T., Fisk T. Control measures for severe acute respiratory syndrome (SARS) in Taiwan. Emerg Infect Dis. 2003;9:718–720. doi: 10.3201/eid0906.030283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Use of quarantine to prevent transmission of severe acute respiratory syndrome–Taiwan, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:680–683. [PubMed] [Google Scholar]
- 14.Lee ML. Health care system in a transitional society: a Taiwan experience. A conference speech delivered at the International Research Foundation for Development. Geneva. June 26, 2000.
- 15.Thompson D.R., Lopez V., Lee D., Twinn S. SARS: a perspective from a school of nursing in Hong Kong. J Clin Nurs. 2004;13:131–135. doi: 10.1046/j.1365-2702.2003.00884.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Taiwan, China: SARS transmission interrupted in last outbreak area. Available at: http://anonymouse.ws/cgi-bin/anon-www.cgi/http://www.who.int/csr/don/2003_07_05/en/. Accessed July 5, 2003.
- 17.Liberty Times. WHO estimated that the Taiwan epidemic situation might be under control in six to seven weeks. Available at: http://www.libertytimes.com.tw/2003/new/may/12/today-t1.htm). Accessed May 12, 2003.
- 18.China Times. The premier said that the outbreak would be over by the end of June. Available at: http://forums.chinatimes.com.tw/report/SARS/Government/htm/92051718.htm. Accessed June 13, 2003.
- 19.SARS Contingency Committee news release. The chief commander of anti-SARS Project in Taiwan said it did not need seven weeks to control the outbreak. Available at: http://www.doh.gov.tw/NewVersion/proclaim/sars_list.asp. Accessed May 13, 2003.
- 20.Centers for Disease Control and Prevention Efficiency of quarantine during an epidemic of severe acute respiratory syndrome–Beijing, China, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:1037–1040. [PubMed] [Google Scholar]
- 21.Hsieh Y.H., Chen C.W., Hsu S.B. SARS outbreak, Taiwan, 2003. Emerg Infect Dis. 2004;10:201–206. doi: 10.3201/eid1002.030515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leung M.W., Yen I.H., Minkler M. Community based participatory research: a promising approach for increasing epidemiology's relevance in the 21st century. Int J Epidemiol. 2004;33:499–506. doi: 10.1093/ije/dyh010. [DOI] [PubMed] [Google Scholar]
- 23.Holkup P.A., Tripp-Reimer T., Salois E.M., Weinert C. Community-based participatory research: an approach to intervention research with a Native American community. ANS Adv Nurs Sci. 2004;27:162–175. doi: 10.1097/00012272-200407000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roger France F.H. WHO views on perspectives in health informatics. Int J Med Inform. 2000;58-59:11–19. doi: 10.1016/s1386-5056(00)00071-x. [DOI] [PubMed] [Google Scholar]
- 25.Wallerstein N., Bernstein E. Introduction to community empowerment, participatory education, and health. Health Educ Q. 1994;21:141–148. doi: 10.1177/109019819402100202. [DOI] [PubMed] [Google Scholar]
- 26.Frewer L. The public and effective risk communication. Toxicol Lett. 2004;149:391–397. doi: 10.1016/j.toxlet.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 27.Bostrom A., Lofstedt R.E. Communicating risk: wireless and hardwired. Risk Anal. 2003;23:241–248. doi: 10.1111/1539-6924.00304. [DOI] [PubMed] [Google Scholar]
- 28.Griffin R.J., Dunwoody S., Zabala F. Public reliance on risk communication channels in the wake of a Cryptosporidium outbreak. Risk Anal. 1998;18:367–375. doi: 10.1111/j.1539-6924.1998.tb00350.x. [DOI] [PubMed] [Google Scholar]
- 29.Sandman P.M. Bioterrorism risk communication policy. J Health Commun. 2003;8(Suppl 1):146–147. doi: 10.1080/713851981. [DOI] [PubMed] [Google Scholar]