Abstract
Background
The risk of developing nosocomial infectious diseases among medical personnel in the emergency department (ED) can result in tremendous psychologic stress. The objective of this study was to estimate the median amount of money ED personnel would be willing to pay for preventing nosocomial severe acute respiratory syndrome (SARS).
Methods
A contingent valuation approach with close-ended format was used. During the study period from June 15, 2003 through June 30, 2003, a convenience sample of all medical personnel working in the ED of National Taiwan University Hospital was carried out. Participants were interviewed by a standard questionnaire and were asked to choose whether or not they would pay at a specified price to purchase a hypothetical SARS vaccine. A logistic regression model was created to evaluate the relationship between willingness-to-pay and the log of the price offered in the bid questions. The median and mean amounts of willingness-to-pay were calculated.
Results
A total of 115 subjects were interviewed and most were nurses (68.7%). The median and mean amount subjects reported being willing to pay for a SARS vaccine was US $1762 and US $720, respectively. Subject responses were significantly related to the price of vaccination and their type of job.
Conclusions
Medical personnel in the ED reported that they would be willing to pay substantial monetary amounts for preventing nosocomial SARS.
Severe acute respiratory syndrome (SARS) can spread extensively among health care workers in various settings.1 The use of precautions, such as N95 masks, gloves, and gowns, can reduce nosocomial transmission of SARS.2 Despite the adoption of such precautions, clusters of SARS cases still occurred among properly protected medical personnel in the emergency department (ED) of National Taiwan University Hospital (NTUH) in 2003 May. Nine medical personnel developed illness that met the criteria for the World Health Organization case definition of suspected or probable SARS.3 A comfortable protective device that is suitable for long-term usage in EDs or vaccination may be needed to fully protect medical personnel in EDs from nosocomial transmission of SARS. Until such an ideal protective device or vaccination is available, medical personnel in EDs will continue to face the psychologic stress associated with the risk of contracting a potentially fatal illness.
The contingent valuation method (CVM) is an established research method for valuing nonmarket goods.4 CVM was initially applied to questions of environmental interest, such as wildlife preservation and water quality.5, 6 More recently, CVM has been used to estimate the value placed by people on such health care intervention as in vitro fertilization,7 and autologous blood donation.8 This method provides a means of acquiring monetary estimates of the value placed on intangible outcomes.9
In this study, CVM was used to estimate the median amount emergency medical personnel would be willing to pay for a hypothetical vaccine to prevent developing nosocomial SARS. This sum may serve as a quantitative proxy measure for factors such as workers' anxiety and distress in facing the threat from SARS.
Methods
Study design
This study surveyed the willingness of medical personnel to pay for a hypothetical vaccine. This study was approved by the Institutional Review Board of NTUH.
Study setting and population
The study was conducted among medical personnel working in the ED of NTUH, a 2000-bed public, tertiary-care, university-based medical center in Taipei City with an annual ED census of approximately 110,000 patients. The ED is staffed primarily by staff physicians and emergency medicine residents along with rotating residents from the internal medicine, surgery, and pediatrics departments.
All participants were medical personnel, including nurses, residents, and staff physicians, who were serving in the ED of NTUH during June 2003. Subjects were interviewed with a standardized questionnaire and were compensated US $3 in small gifts for their time and efforts. Medical personnel were considered ineligible for participation if they had just started employment in June 2003.
Study protocol
During the study period from June 15th, 2003 to June 30th, 2003, a convenient sample of all the medical personnel working in the ED of NTUH was carried out. The 9 cases of SARS were excluded. All the participants were interviewed by the authors with a standardized questionnaire. The questionnaire assessed demographic information, risk perceptions, and willingness-to-pay (WTP) for a hypothetical safe and effective vaccination. Subjects indicated their perceived risk of acquiring nosocomial SARS infection by selecting 1 of 5 different fixed response alternatives: 1/100, 1/1000, 1/10,000, 1/100,000, and 1/1,000,000. The time frame for the perceived risk is lifetime.
Contingent valuation
To determine the monetary value of the precautions to our subjects, each subject was asked the following question: “Suppose there was a vaccine that could fully protect you from developing nosocomial SARS. Knowing what you know now, would you pay $X out of pocket for such a vaccine?” In the question for determining the monetary value of the vaccination, $X was selected at random from a group of 9 bids ranging in value from 1000 to 1,000,000 New Taiwan dollars (NT$). For the convenience of international comparison in the future, these values (in NT$) were then converted to 2003 US dollars at the rate of NT $34.96 : US $1 in further data processing.10 Subjects could provide either a “yes” or “no” response to the question, indicating whether they were willing to pay for the hypothetical vaccine at the price they had been quoted.
Data analysis
A logistic regression model was created to evaluate the relationship between WTP and the log of the price offered in the bid questions. In this regression model, we evaluated whether the probability of answering “yes” to the WTP) questions was related to the price listed. Data on the median and the mean WTP were reported. The effect of social–economic factors and different perceived risks of acquiring nosocomial transmission of SARS on WTP were assessed through the creation of a multivariate logistic regression model with a backward elimination algorithm.11 All statistical analyses were performed with SAS version 8.1 (SAS Institute, Cary, NC).
Results
During the study period, 120 subjects out of 158 ED personnel in total were recruited. Five subjects were unwilling to respond to the questionnaire. The characteristics of the remaining 115 participants are outlined in Table 1. The average age of study participants was 30.5 years, and 67.0% were women. Sixty-nine percent of participants were nurses, and 57% had graduated from college. Annual incomes of 41% of the participants were equal to or more than US $28,604.
Table 1.
Characteristics of the study population
| Study subjects (n = 115) | |
|---|---|
| Mean age (±SD), y | 30.5 (±6.34) |
| Gender (%) | |
| Female | 77 (67.0) |
| Job description (%) | |
| 1. Staff EP | 10 (8.7) |
| 2. Medical or surgical resident | 26 (22.6) |
| 3. Nurse | 79 (68.7) |
| Education level (%)∗ | |
| 1. Graduate school | 8 (7.0) |
| 2. College | 66 (57.4) |
| 3. High school | 40 (34.8) |
| Other§ | 1 (0.9) |
| Annual income level (%)∗ | |
| 1. <US $28604 | 67 (58.3) |
| 2. ≧UD $28604 | 47 (40.9) |
| Other§ | 1 (0.9) |
| Perceived risk (%)∗∗ | |
| < 0.001 | 39 (33.9) |
| 0.001 | 49 (42.6) |
| 0.01 | 27 (23.5) |
EP, emergency physician.
Percentages may not add up to 100 as a result of rounding.
The time frame for the perceived risk is lifetime.
Subjects refused to answer the question.
Among the 115 subjects who responded to the WTP question, a strong negative association was seen between the log of the dollar bid presented and the subject's WTP for a vaccine that could avert their development of nosocomial SARS infection ( Table 2). The odds ratio (OR) for WTP associated with a 10 fold increase in the bid presented to the study subject was 0.20. This suggests that in this sample, the odds of a person willing to pay for a vaccine costing US $100 would be 0.20 times the odds of WTP for a US $10 vaccine.
Table 2.
Logistic regression models of willingness to pay according to dollar bid
| OR | 95% CI | P value | |
|---|---|---|---|
| Univariate model | |||
| Log10 Dollar bid (per USD100) | 0.20 | 0.10-0.40 | <.01 |
| Multivariate model | |||
| Log10 Dollar bid (per USD100 | 0.14 | 0.06-0.35 | <.01 |
| Job (Staff EP vs Nurse) | 7.76 | 0.85-70.90 | .07 |
| Job (Resident vs Nurse) | 12.06 | 1.54-94.48 | .02 |
EP, emergency physician.
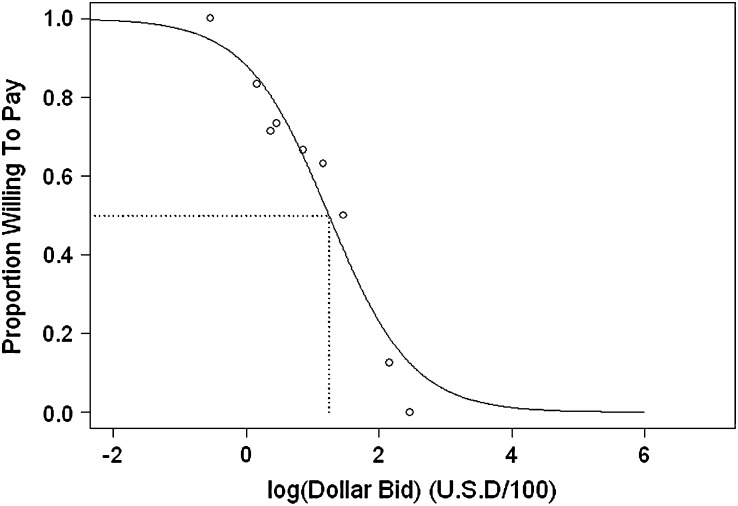
A fitted logistic curve of the expected proportion of subjects willing to pay for a vaccine over a range of costs is presented in Fig 1. The projected median amount subjects would be willing to pay was US $1762. Thus, presented with a vaccine costing US $1762, half the study subjects would have been expected to agree to purchase it. The mean amount our study subjects would be willing to pay was US $720.
Fig 1.
Proportion willing to pay for a vaccine to prevent nosocomial acquisition of severe acute respiratory syndrome.
Circles (O), proportion of subjects who responded “yes” to the question of whether they would be willing to pay for a hypothetical vaccine. Black line, a fitted logistic curve describing the proportion of subjects willing to pay. Dashed line, median amount subjects would be willing to pay.
A multivariable logistic regression model was created to adjust for potential confounding of WTP by subject-related covariates. In this multivariate model, we found the price of the vaccine and the type of jobs were significantly related to the WTP responses. The WTP responses were not significantly related to age, gender, perceived risk, education level, or income level. Increased amount of WTP was found in resident physicians as compared with nurses (OR, 12.06; 95% confidence interval [CI], 1.54–94.48). When adjusted for this confounding variable, the median amount subjects were willing to pay was US $2729, US $3922, and US $1333 in staff physicians, resident physicians, and nurses, respectively.
Discussion
SARS, avian flu, and other dangerous infectious diseases present a constant and significant threat to the health of medical personnel in EDs. The importance of recognizing the intangible costs of nosocomial transmission of these infectious diseases cannot be overemphasized. Economic analyses that include the costs of workers' anxiety and distress are likely to provide a more favorable assessment of a new vaccination. We used this study as an example to demonstrate that medical personnel would be willing to pay substantial monetary amounts to avert the risk of nosocomial SARS infection.
There are several clinical implications of our results. First, the anxiety and psychologic stress of healthy workers when they are facing threats from dangerous infectious diseases can be measured quantitatively or monetized. The estimates of WTP can be used as a reference to improve benefits and compensation for those healthy workers. Second, to policy makers, the preference assessment can also be of great assistance in guiding decisions on resource allocation. The aggregate WTP will be a substantial dollar amount and provide a solid ground for the investment in new vaccine development or more effective protective measures.
Based on our results, medical personnel in the ED showed very strong preference for a SARS vaccine. The usual costs of vaccines are all below or around US $10 in Taiwan. However, we found that the median amount medical personnel in the ED would be willing to pay for a SARS vaccine was US $1,762, which was exceedingly high compared to the usual cost of a vaccine and equal to 14% of the 2002 Taiwan gross domestic product per capita (US $12,588).12
While the SARS vaccine is still under development, the only effective mechanism for containment of SARS is quarantine. The cost of quarantine was estimated at Can $2611 to Can $4150 per averted infection in Canada.13 However, with the probability of infection among ED workers of NTUH around 0.07, the implied benefit per averted infection was approximately US $25,000 ($1762/0.07). Compared with the cost of quarantine, the potential benefit assessed by CVM was much larger. It may suggest that it's worth investing more resources in the control of SARS. Incorporating the monetary value of WTP in the cost–benefit analysis of a SARS vaccine would provide a more favorable result from the perspective of ED workers.
Income-sensitivity (ie, differential WTP according to income) is an important issue in assessing WTP for health technologies because it raises crucial questions about equitable distribution of health resources. We did find income-sensitivity in our study. However, the responses of our participants were related to their job description, a surrogate measure of income, and education level. Data on factors such as marital status or the presence of dependent children, which could affect risk attitudes by increasing the circle of people who suffer the consequences of SARS infection by a family member, may be needed to explain the results.
Assessment of the effect of the perceived risks that might confound WTP for a hypothetical SARS vaccine in this study revealed no significant positive or negative relationship between the perceived risks of developing nosocomial SARS infection and WTP for a SARS vaccine. This result was not consistent with the findings of a study by Bosompra et al of psychosocial factors associated with the public's WTP for genetic testing for cancer risk.14 It is possible that the number of our participants was not large enough to detect the effect on WTP for a SARS vaccine was largely explained by the price of vaccination. These questions warrant additional exploration.
Several formats of WTP survey questions, such as open-ended questions, closed-ended questions with dichotomous choice, and payment card questions, are currently in use. Many CVM researchers still do not agree about which valuation question is the most appropriate.4, 15, 16, 17 Open-ended questions has been used in early CVM applications but are relatively difficult to answer. A payment card valuation question is an improvement over the open-ended valuation question, but some arguments exist as to whether there are range and centering biases.15, 18, 19 Following the recommendation and praxis of some health economic studies,8, 9, 17, 20 the closed-ended question with dichotomous choice was used in this study. The advantage of the dichotomous choice question is that each respondent is asked a single valuation question that is relatively easy to answer. The major disadvantage is that the CVM researcher only learns the threshold of each respondent's WTP, and more sophisticated econometric methods are necessary to develop an average WTP amount.15
Even with adjustments for some important factors, values for other populations may differ. Our results included both the median amount subjects would be willing to pay and also the corresponding percentage of gross domestic product per capita to allow comparison of our results with studies from other countries. However, as with other studies in health care, extrapolation of population results to the behavior of particular individuals must be made with caution. Participants were not actually forced to pay the amount they claimed they would have been willing to provide;21 nonetheless, the decrease in WTP as bids increased suggests that subjects were price-sensitive, notwithstanding the hypothetical nature of this transaction.
This pilot study was intended to illustrate the importance of assessing intangible costs associated with a dangerous infectious disease. The number of participants in the study was not very large. The survey respondents were all ED personnel in a hospital that experienced an outbreak of SARS. Further studies are needed to determine whether our results can be generalized to other populations.
In conclusion, medical personnel in the ED reported that they would be willing to pay substantial monetary amounts for preventing nosocomial SARS. We suggest these findings should be considered in further studies for promoting safety of medical care providers.
Acknowledgments
The authors would like to thank Hsin-Yi Chen for her help in the statistics.
References
- 1.Centers for Disease Control and Prevention Cluster of severe acute respiratory syndromes cases among protected health-care workers—Toronto, Canada, April 2003. JAMA. 2003;289:2788–2789. doi: 10.1001/jama.289.21.2788. [DOI] [PubMed] [Google Scholar]
- 2.Seto W.H., Tsang D., Yung R.W., Ching T.Y., Ng T.K., Ho M., Advisors of Expert SARS Group of Hospital Authority Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Case definitions for surveillance of Severe Acute Respiratory Syndrome (SARS). Available from: http://www.who.int/csr/sars/casedifinition/en. Accessed December 20, 2006.
- 4.Kenkel D., Berger M., Blomquist G. Contingent Valuation of Health. In: Tolley G., Kenkel D., Fabian R., editors. Valuing Health for Policy. The University of Chicago Press; Chicago: 1994. pp. 72–104. [Google Scholar]
- 5.Desvousges W., Smith V., Fisher A. Option price estimates for water quality improvements: a contingent valuation study for the Monongahela River. J Environ Econ Manage. 1987;14:248–267. [Google Scholar]
- 6.Boxall P., Adamowicz W., Swait J., Williams M., Louviere J. A comparison of stated preference methods for environmental valuation. Ecologic Econ. 1996;18:243–253. [Google Scholar]
- 7.Neumann P., Johanneson M. The willingness to pay for in-vitro fertilization: a pilot study using contingent valuation. Med Care. 1994;32:686–699. doi: 10.1097/00005650-199407000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lee S., Neumann P., Churchill H., Cannon M., Weinstein M., Joanneson M. Patients' willingness to pay for autologous blood donation. Health Policy. 1997;40:1–12. doi: 10.1016/s0168-8510(96)00879-2. [DOI] [PubMed] [Google Scholar]
- 9.Fisman D.N., Mittleman M.A., Sorock G.S., Harris A.D. Willingness to pay to avoid sharps-related injuries: a study in injured health care workers. Am J Infect Control. 2002;30:283–287. doi: 10.1067/mic.2002.124586. [DOI] [PubMed] [Google Scholar]
- 10.Statistics Taiwan . Statistics Taiwan; Taipei: 2003. Foreign currency exchange rate. [Google Scholar]
- 11.Kleinbaum D., Kupper L., Muller K., Nizam A. Duxbury Press; Pacific Grove (CA): 1998. Selecting the best regression equation: applied regression analysis and other multivariable methods. p. 386-442. [Google Scholar]
- 12.Statistics Taiwan . Statistics Taiwan; Taipei: 2003. Gross domestic product per capita. [Google Scholar]
- 13.Gupta A.G., Moyer C.A., Stern D.T. The economic impact of quarantine: SARS in Toronto as a case study. J Infect. 2005:386–393. doi: 10.1016/j.jinf.2004.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bosompra K., Ashikaga T., Flynn B.S., Worden J.K., Solomon L.J. Psychosocial factors associated with the public's willingness to pay for genetic testing for cancer risk: a structural equations model. Health Educ Res. 2001;16:157–172. doi: 10.1093/her/16.2.157. [DOI] [PubMed] [Google Scholar]
- 15.Whitehead J.C. A practitioner's primer on the contingent valuation method. In: Alberini A., Kahn J.R., editors. Handbook on Contengent Valuation. Edward Elgar Publishing; Northampton (MA): 2006. pp. 66–91. [Google Scholar]
- 16.Balistreri E., McClelland G., Poe G., Schulze W. Can hypothetical questions reveal true values? A laboratory comparison of dichotomous choice and open-ended contigent values with auction values. Environmental and Resource Economics. 2001;18:275–292. [Google Scholar]
- 17.Frew E.J., Whynes D.K., Wolstenholme J.L. Eliciting willingness to pay: comparing closed-ended with open-ended and payment scale formats. Med Decis Making. 2003;23:150–159. doi: 10.1177/0272989X03251245. [DOI] [PubMed] [Google Scholar]
- 18.Rowe R.D., Schulze W.D., Breffle W.S. A test for payment card biases. J Environ Econom Manage. 1996;31:178–185. [Google Scholar]
- 19.Klose T. The contingent valuation method in health care. Health Policy. 1997;47:97–123. doi: 10.1016/s0168-8510(99)00010-x. [DOI] [PubMed] [Google Scholar]
- 20.Johannesson M., Jonsson B., Karlsson G. Outcome measurement in economic evaluation. Health Econ. 1996;5:279–296. doi: 10.1002/(SICI)1099-1050(199607)5:4<279::AID-HEC218>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 21.Blumenschein K., Johanneson M., Yokoyama K., Freeman P. Hypothetical versus real willingness to pay in the health sector: results from a field experiment. J Health Econ. 2001;20:441–457. doi: 10.1016/s0167-6296(01)00075-3. [DOI] [PubMed] [Google Scholar]