Abstract
This study investigated the anticipated vaccination rate against pandemic human influenza A (H1N1) 2009 in the health care setting. Self-administered questionnaires were used to assess nurses' acceptance of vaccination against seasonal flu and H1N1. They were sent to nurses by post through various nurses' unions before initiation of the vaccination program. Only 13.3% of the respondents planned to receive the H1N1 vaccine, compared with 37.5% for the seasonal influenza vaccine. Vaccination against seasonal influenza in the preceding season strongly predicted the likelihood of H1N1 vaccination. The main reason cited for H1N1 vaccination was self-protection, and reasons for rejecting vaccination included possible side effects, ineffectiveness of the vaccine, and the mild nature of the disease. Personal contact with patients with H1N1 or severe acute respiratory syndrome at work did not significantly increase the likelihood of receiving the H1N1 vaccine. More than 40% of the respondents were undecided at the time of the survey. The promotion of vaccination against seasonal influenza may play a role in improving H1N1 vaccination coverage. Efforts are needed to address concerns about vaccination risk and to incorporate H1N1 vaccination in standard infection control practice with policy support.
Vaccination against influenza protects health care workers (HCWs) and patients from contracting influenza by reducing virus transmission in health service settings. Vaccination of HCWs is an important strategy, because infected HCWs can be a source of infection to patients. Reducing HCWs' risk of acquiring infection protects patients indirectly. Because it is easier to target HCWs for vaccination than the general public, vaccinating HCWs is a sound strategy to protect patients. However, vaccination coverage in HCWs has been notoriously unsatisfactory, with rates ranging from about 30% to 70% in different countries.1, 2, 3, 4 Major barriers to vaccination include misconceptions about the rationale for vaccination, perceived ineffectiveness of the vaccine, perceived unlikelihood of contracting influenza, potential side effects, fear of injection, and lack of time.5, 6, 7 The recent emergence of pandemic human influenza A (H1N1) in 2009 is stressing the health care system because of the lack of immunity in the public and the associated mortality and morbidity.8, 9 The possibility of genetic reassortment between different subtypes of influenza giving rise to more resistant genotype is another concern, which may potentially lead to new pandemics.10, 11, 12, 13 Vaccination is a time-honored strategy for preventing H1N1, which can predictably reduce mortality and morbidity.
Whereas there are abundant data on factors affecting the acceptance of seasonal influenza vaccine, those on H1N1 vaccination are scarce. In many countries, the first wave of pandemic H1N1 has come and gone. To enhance our preparedness for the impending second wave, which has yet to arrive in some countries in the northern hemisphere, we conducted a survey to estimate the acceptance rate of H1N1 vaccination in a group of nurses, and to explore factors that might be associated with vaccination uptake.
Methods
Nurses registered as members of the Hong Kong Nurses General Union, the Nurses Branch, and the Enrolled Nurses Branch of the Hong Kong Chinese Civil Servants Association were invited to participate in a self-administered anonymous questionnaire survey on infection control practices relating to influenza prevention that has been conducted every 1-2 years since 2006.14, 15 The 2009 questionnaire, constructed in Chinese, together with an introductory letter explaining the purpose and nature of the study, was delivered to each individual member's postal address. The content was developed after discussions with nurses in the field, followed by pilot testing before administration. Approval was obtained from the Survey and Behavioral Research Ethics Committee of The Chinese University of Hong Kong.
The questionnaire was divided into 4 parts. Part A assessed the respondent's vaccination status in terms of seasonal influenza in the preceding year and his or her willingness to receive vaccination against seasonal influenza and H1N1 in the coming season. The reasons for receiving or rejecting vaccination (eg, perceptions regarding protection of themselves, relatives, and patients, mandatory requirement, circumstances of the outbreak) were also assessed. The respondent was asked to select and rank 9 reasons that might have affected the decision for vaccination using a scale of 1 (most important) to 9 (least important). Part B assessed the respondent's exposure to H1N1 in the workplace or family. Part C assessed the respondent's agreement with government policies for preventing H1N1 and the perceived severity of H1N1 compared with H5N1 (avian) or seasonal influenza. The responses were evaluated on a Likert scale ranging from 1 (most disagreed) to 6 (most agreed). Part D consisted of questions on demographics and work nature in terms of clinical exposure.
Data entry was performed using Microsoft Excel (Microsoft, Redmond, WA). Statistical analysis was performed with SPSS version 13.0 (SPSS Inc, Chicago, IL). Nonparametric tests were used to analyze ordinal data. Dichotomous data were further analyzed by binary logistic regression analysis for odds ratio (OR) calculation, with statistical significance defined as P < .05.
Results
General characteristics and vaccination profile
A total of 2929 questionnaires were sent out over a 4-week period in July and August 2009. Of these, 812 were returned, for a response rate of 27.7%. The majority (697; 85.8%) of the respondents were female Registered Nurses who had received formal 3-year training, versus enrolled nurses with a shorter (2-year) training and lower entry requirements. Of the 812 respondents, 650 (80%) were between 36 and 55 years old, and a high proportion (463; 57%) had practiced nursing for >20 years. Regarding clinical exposure, 66% (487) reported having frequent direct contact with patients.
Concerning Part A of the questionnaire, about 60% (494) had received seasonal influenza vaccination in the preceding year. For the coming flu season, 37.5% (305) were planning to receive seasonal influenza vaccine, 40.8% (331) rejected vaccination, and 21.6% (176) were undecided. Only 13.3% (108) of the respondents were considering vaccination against H1N1, with 45.4% (369) rejecting vaccination and 41.3% (335) undecided. Age, experience, and frequency of patient contacts were divided into several strata for further analysis. The smaller proportion of nurses accepting H1N1 vaccination was consistent across each stratum regardless of age, experience, or frequency of patient contacts. The nature of nursing practice and frequency of patient contact were not significantly associated with the decision for vaccination (OR, 1.29; 95% confidence interval [CI], 0.82-2.02).
For those who either had been vaccinated in the preceding influenza season or were planning to receive seasonal influenza vaccine, the majority (>85%) believed that vaccination could protect against infection. Work requirements and protecting others in the workplace from infection were less commonly cited reasons, reported by only about 50% of the respondents. For nurses who had not received vaccination in the previous year or declined vaccination in the coming year, the most frequent reason for doing was concern about side effects of the vaccine (65%-68%). This reason was cited more frequently by those who declined H1N1 vaccination (83.9%). Other reasons for declining the vaccination included the perceived mild nature of influenza (26.3%-30.8%) and the belief that the vaccine could not prevent infection (55.9%-58.5%). The latter reason was less common among those who declined H1N1 vaccination. The findings are summarized in Table 1 .
Table 1.
Reasons for accepting or declining seasonal influenza and H1N1 vaccination
| Number (%) of nurses accepting or declining vaccination |
|||
|---|---|---|---|
| Seasonal influenza vaccination in the preceding year | Seasonal influenza vaccination in the coming season | H1N1 vaccination in the coming season | |
| Reasons for accepting vaccination | |||
| Protecting oneself from infection | 272 (86.6) | 261 (86.7) | 98 (90.7) |
| Protecting others from infection in the health setting | 166 (52.9) | 158 (52.5) | 55 (50.9) |
| Work requirement | 194 (61.8%) | 181 (60.1) | 53 (49.1) |
| Reasons for declining vaccination | |||
| Ineffectiveness of vaccine to prevent infection | 238 (55.9) | 240 (58.5) | 173 (30) |
| Ineffectiveness of vaccine to protect others in the health setting from being infected | 67 (15.7) | 63 (15.4) | 69 (12) |
| Side effects after vaccination | 277 (65) | 279 (68) | 483 (83.9) |
| Mildness of influenza disease | 131 (30.8) | 108 (26.3) | 174 (30.2) |
| No requirement at work for vaccination | 28 (6.6) | 30 (7.3) | 35 (6.1) |
NOTE. The total percentage exceeds 100% because multiple responses were allowed.
Acceptance of the H1N1 vaccine
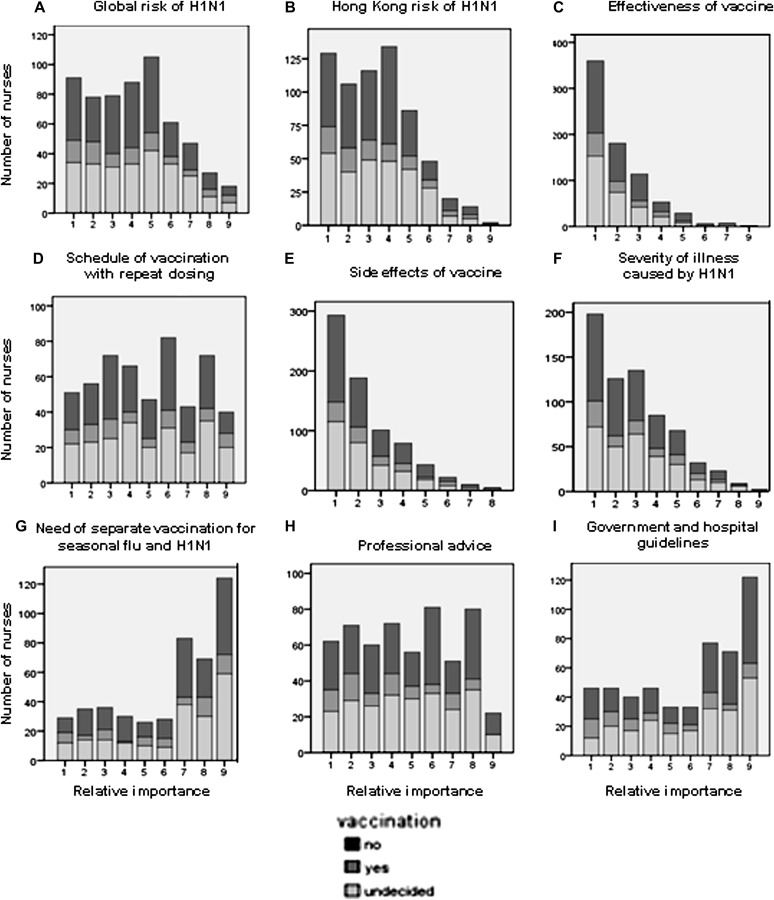
Only 108 (13.3%) of the respondents were planning to receive H1N1 vaccination when it became available. Figure 1 shows the relative importance of 9 factors in the decision for considering H1N1 vaccination. The number (percentage) of nurses choosing the 3 most important factors were vaccine effectiveness (364; 44.8%), potential side effects (190; 23.4%), and illness severity (138; 17%). Government policy and professional opinions were of little importance. A small proportion was concerned about the inconvenience of vaccination procedures, for example, the need to be vaccinated separately from seasonal influenza vaccine, or if 2 doses were needed.
Fig 1.
Relative importance of 9 factors, expressed as ranks from 1 (most important) to 9 (least important) by respondents who rejected (dark bar), accepted (gray bar), and were undecided about (light-gray bar) H1N1 vaccination.
Nurses that had received or were planning to receive seasonal flu vaccine had a significantly higher tendency to receive H1N1 vaccine (OR, 3.73; 95% CI, 2.43-5.73 vs OR, 26.89; 95% CI, 10.75-67.34, respectively). The OR of the 9 factors for H1N1 vaccination was determined when each was taken as “most important” versus the rest. In such instance, the most significant factor was government and hospital guidelines, with an OR for vaccination of 2.73 (95% CI, 1.36-5.49). Frequent contact with patients, the global and Hong Kong risk of H1N1, vaccination schedule, severity of the disease, and professional opinion all tended to increase the OR for vaccination, although these increases were not statistically significant (Table 2 ).
Table 2.
ORs of factors affecting acceptance of H1N1 vaccination
| Number (%) of nurses accepting the H1N1 vaccine | OR (95% CI) | |
|---|---|---|
| Sex | ||
| Female | 79/665 (11.9) | 0.37 (0.23-0.60) |
| Male | 29/108 (26.9) | |
| Nursing practice | ||
| Enrolled nurse | 14/125 (11.2) | 0.76 (0.42-1.38) |
| Registered Nurse | 92/646 (14.2) | |
| Seasonal flu vaccination in the preceding year | ||
| Yes | 72/313 (23.0) | 3.73 (2.43-5.73) |
| No | 35/485 (7.4) | |
| Seasonal flu vaccination in the coming season | ||
| Yes | 89/302 (29.5) | 26.91 (10.75-67.34) |
| No | 5/327 (1.5) | |
| Factors considered most important for H1N1 vaccination | ||
| Global risk of H1N1 | ||
| Yes | 15/91 (16.5) | 1.31 (0.71-2.41) |
| No | 66/504 (13.1) | |
| Hong Kong risk of H1N1 | ||
| Yes | 20/129 (15.5) | 1.20 (0.70-2.05) |
| No | 70/526 (13.3) | |
| Effectiveness of H1N1 vaccine | ||
| Yes | 50/360 (13.9) | 0.99 (0.65-1.49) |
| No | 55/391 (14.1) | |
| Schedule of vaccine with repeated dosing | ||
| Yes | 8/51 (15.7) | 1.23 (0.55-2.74) |
| No | 63/480 (13.1) | |
| Side effects of vaccine | ||
| Yes | 33/293 (11.3) | 0.68 (0.44-1.07) |
| No | 70/447 (15.7) | |
| Severity of illness caused by H1N1 | ||
| Yes | 29/198 (14.6) | 1.23 (0.76-1.98) |
| No | 59/481 (12.3) | |
| Need for separate vaccination against H1N1 and seasonal influenza vaccines | ||
| Yes | 7/29 (24.1) | 2.23 (0.91-5.46) |
| No | 54/432 (12.5) | |
| Professional advice | ||
| Yes | 12/62 (19.4) | 1.71 (0.86-3.39) |
| No | 61/495 (12.3) | |
| Government and hospital guidelines | ||
| Yes | 13/46 (28.3) | 2.73 (1.36-5.49) |
| No | 59/468 (12.6) | |
| Previous exposure to H1N1 | ||
| Contact with H1N1 patients at work | ||
| Yes | 25/184 (13.7) | 1.03 (0.63-1.67) |
| No | 78/584 (13.4) | |
| Been in a workplace where H1N1 patients were managed but without direct contact | ||
| Yes | 34/226 (14.2) | 1.09 (0.75-1.90) |
| No | 74/574 (12.9) | |
| Ever suspected of H1N1 infection but never confirmed | ||
| Yes | 1/8 (12.5) | 0.91 (0.11-7.47) |
| No | 107/789 (13.6) | |
| Ever confirmed with H1N1 infection | ||
| Yes | 1/6 (16.7) | 1.28 (0.15-11.0) |
| No | 107/791 (13.5) | |
| Never infected with H1N1 | ||
| Yes | 106/783 (13.5) | 0.94 (0.21-4.26) |
| No | 2/14 (14.3) | |
| No known friends/relatives infected with H1N1 | ||
| Yes | 31/226 (13.7) | 1.06 (0.67-1.66) |
| No | 71/542 (13.1) | |
| Family members in the household infected with H1N1 | ||
| Yes | 4/16 (25.0) | 2.25 (0.68-7.47) |
| No | 27/209 (12.9) | |
Regarding the respondents' personal experience with H1N1 (part B of the questionnaire) 584 (76%) of those accepting H1N1 vaccination had never come into contact with any patients with the infection. A minority (184; 24%) needed to manage H1N1 patients at work, whereas 226 (28%) reported that their workplace handled H1N1 patients, but no contact was required. Contact with H1N1 patients did not increase the OR of receiving vaccination (OR, 1.03; 95% CI, 0.63-1.67). There were only 8 (1%) suspected and 6 (0.75%) confirmed H1N1 cases in the study population; of these 14 cases, 6 (42.8%) were work-related. A family history of H1N1 infection was associated with a higher tendency to accept vaccination (OR, 2.25; 95% CI, 0.68-7.47) (Table 2).
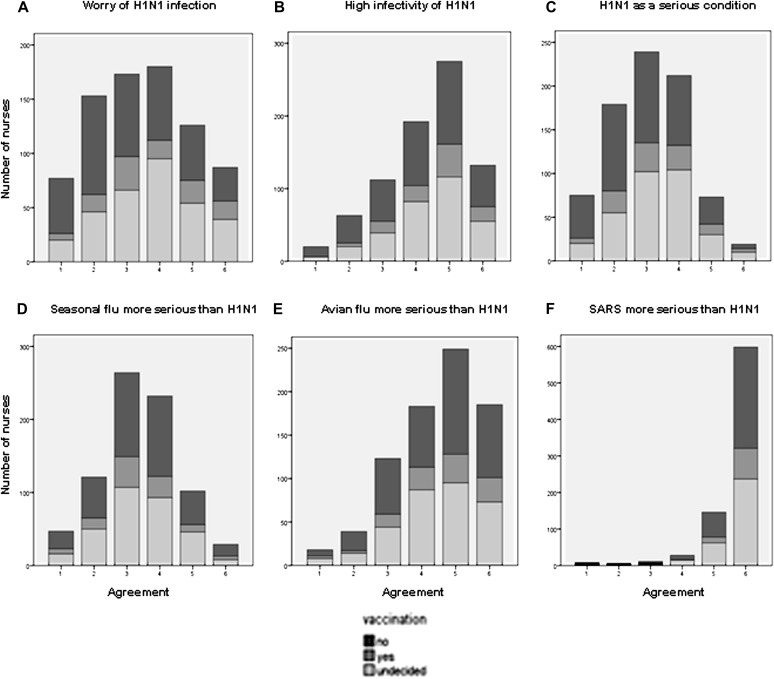
Attitudes toward H1N1
Figure 2 graphically presents the respondents' attitudes toward H1N1 (part C of the questionnaire). Nurses who declined H1N1 vaccination tended to be less worried about becoming infected and were less inclined to perceive H1N1 as a severe infectious disease, although they basically agreed that it was highly infectious. Overall, many (496; 62.4%) considered seasonal influenza and H1N1 to be of similar severity, and most agreed that H5N1 (617; 77.4%) and severe acute respiratory syndrome (SARS) (772; 96.8%) were more serious than H1N1. Regardless of their attitudes, most of the nurses agreed with government policies for controlling the H1N1 epidemic.
Fig 2.
Perception on H1N1 rated on a Likert scale from 1 (most disagreed) to 6 (most agreed) for level of agreement in respondents who rejected (dark bar), accepted (gray bar), and were undecided about (light-gray bar) H1N1 vaccination.
Discussion
Reasons for receiving or declining vaccination
Based on our results, we anticipated a low uptake rate for H1N1 vaccination in nurses in Hong Kong. The proportion of nurses planning to receive the H1N1 vaccine was much lower in that that for the seasonal influenza vaccine (13.3% vs 37.5%), despite the similarities of the two diseases in transmissibility and clinical outcomes as reported through clinical and epidemiologic observations.12 Because influenza vaccination is not a mandatory requirement for HCWs, vaccination coverage naturally hinges on the individual's willingness to get vaccinated, which in turn is dependent on the perceived risks and benefits of vaccination. Our study suggests that self-protection was the main reason for receiving vaccination against both H1N1 and seasonal influenza. Surprisingly, past experience with respiratory infection did not increase the likelihood of receiving H1N1 vaccination. Nurses who had come into contact with patients infected with H1N1 were not more likely to receive H1N1 vaccination (OR, 1.03). More nurses who had been in contact with H1N1 patients at work (44/137; 32.1%) believed that H1N1 is a minor disease compared with those who had not been in contact H1N1 patients at work (43/176; 24.4%). Moreover, many nurses considered seasonal influenza and H1N1 to be less serious than H5N1 or SARS. Personal exposure to the infection was not an important factor, although the number of respondents might be too small to allow meaningful interpretation. Nonetheless, our earlier studies had demonstrated a positive impact of this factor on nurses' preparedness against avian flu outbreaks.14, 15
We explored a whole range of factors that might be associated with nonacceptance of H1N1 vaccination (Table 2). Unlike other studies on seasonal influenza vaccination, many of these potential factors did not have sufficiently strong statistical power to predict vaccination behavior against H1N1 in our nurses. Those rejecting H1N1 vaccination had 2 major concerns, perceived ineffectiveness and potential adverse effects of the vaccine, cited by >50% of the respondents, consistent with previous studies.1, 2, 16, 17 About one-third of those declining vaccination considered either form of influenza to be a mild disease. Misconceptions about seasonal influenza vaccination are common among nurses, even after education programs, as reported by Raftopoulos18 and Ofstead et al.19 In particular, the purpose of vaccination to protect an at-risk population, rather than as self-protection, was hardly recognized. The factors associated with a declining H1N1 vaccination rate might well be similar to those for seasonal influenza vaccination, because many nurses considered the 2 diseases to be of similar severity. It can be argued that the perceived benefit of vaccination is easily offset by the possible, yet uncertain side effects of the H1N1 vaccine. We did not explore the cost of the vaccine as a factor in our study, because vaccination is free to all nursing staff in Hong Kong.
Improving vaccination coverage
An estimated 50% of the H1N1 cases in the United States are acquired in health care settings.20 High vaccination coverage is crucial to preventing transmission of the infection. Given that >40% of our survey respondents were undecided about receiving the H1N1 vaccination, the final vaccination coverage will depend on external factors that might affect their major concerns, rather than on promotion of vaccination as an effective tool to prevent infection transmission. Interestingly, acceptance of seasonal influenza vaccination was a very strong predictor for acceptance of H1N1 vaccination. Similar findings from an Internet survey of US adults was reported by Maurer et al.21 Vaccination against seasonal influenza in the preceding year was associated with an OR of 26 for receiving the H1N1 vaccine in the coming season. This finding is in agreement with previous studies of seasonal influenza vaccination in HCWs.1, 2, 3, 5 Thus, it has been speculated that efforts to increase seasonal influenza vaccination coverage will lead to increased H1N1 vaccination coverage. In our study, >60% of the nurses had received seasonal influenza vaccination in the previous year; however, the estimated vaccination rate for the coming flu season had dropped to 37.5%, though some 20% of the respondents were undecided at the time of the survey. If all undecided nurses subsequently received vaccination, then the proportions vaccinated against H1N1 and seasonal influenza would be quite similar, reaching ≥50% of the total cohort.
How can vaccination coverage be improved? First, vaccination policy for HCWs should be developed separately from that for the general public, given the differing concerns and priorities in the 2 populations. Currently, HCWs are a priority category for receiving H1N1 vaccination in Hong Kong, a practice also adopted in the United States and other parts of the world.22 Such an approach could be counterproductive, however, because so many HCWs do not consider themselves at risk of infection. In our study, nurses demonstrated positive attitudes toward government policies on controlling the epidemic irrespective of their degree of acceptance of H1N1 vaccination. Ironically, professional advice and official guidelines were relatively unimportant factors for those who rejected vaccination, a finding similar to that in a recent local study.17 This discrepancy has arisen because policy guidelines addressing the specific needs of HCWs have yet to be developed.
Second, vaccination as an important measure to protect vulnerable populations should be emphasized in infection control training. Currently, priority populations for H1N1 vaccination include elderly persons, pregnant women, and persons with chronic disease. The purpose of offering vaccination to these latter groups is to prevent disease and reduce morbidity and mortality. Theoretically, vaccination of HCWs could serve a dual purpose of occupational safety and infection control, the latter to reduce the incidence of nosocomial infection. In our study, those accepting vaccinations perceived H1N1 or seasonal influenza vaccination not as an infection control measure, but simply as a means of self-protection. Rectifying this prevailing attitude should be considered through policy and educational strategies.
Third, combining the human H1N1 and seasonal influenza vaccines in a single vaccination program may help improve the uptake rate. Admittedly, the coverage of seasonal influenza vaccination has remained suboptimal, even though the percentage of nurses accepting the vaccination is much higher than that for H1N1 vaccination. Incorporating the H1N1 vaccine in the seasonal influenza regimen, as advocated for the southern hemisphere in the coming year, could boost the coverage to that for the seasonal influenza vaccine.23 However, this would still not be good enough if the objective of vaccinating HCWs is to control transmission, for which a near-100% coverage is the goal.
Study limitations
Our study has some limitations. First, only a small number of nurses were represented in the survey. The total number of registered nurses and enrolled nurses in Hong Kong was 37,447 as of December 2008.24 For practical reasons, it was impossible to include all nurses due to limited resources and the lack of a uniform survey platform. Second, some 30% of the nurses in our cohort did not have frequent patient contact, a factor that should be noted when extrapolating results to the health care profession at large. We have not been able to categorize the population according to the nature of the workplace. It would be interesting to compare the responses in nurses with different jobs, such as those in outpatient clinics, hospitals, and nonclinical settings. Third, most of the responding nurses were mature and highly experienced, characteristic of members of the nursing associations surveyed. Younger nurses and those with less experience might not have been captured. Moreover, the use of a mail-in survey might have caused some bias in the responses. It could be argued that those who took time to return the questionnaire were probably more ready to express their thought and opinions. Finally, nursing culture varies across countries, and so our results might not be applicable to other places.
Acknowledgments
We thank Cecilia So, Hong Kong Nurses General Union, Nurses Branch, and Enrolled Nurses Branch of the Hong Kong Chinese Civil Servants Association, and all members of the 3 associations who participated in this survey. The results presented in this article do not reflect the views of the associations that facilitated the administration of the research. We also thank David Sorrell for general advice.
Footnotes
Conflicts of interest: None to report.
References
- 1.Nowalk M.P., Lin C.J., Zimmerman R.K., Fox D.E., Raymund M., Tanis M.D. Self-reported influenza vaccination rates among health care workers in a large health system. Am J Infect Control. 2008;36:574–581. doi: 10.1016/j.ajic.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Abramson Z.H., Levi O. Influenza vaccination among primary healthcare workers. Vaccine. 2008;26:2482–2489. doi: 10.1016/j.vaccine.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 3.de Juanes J.R., Garcia de Codes A., Arrazola M.P., Jaen F., Sanz M.I., Gonzalez A. Influenza vaccination coverage among hospital personnel over three consecutive vaccination campaigns (2001-2002 to 2003-2004) Vaccine. 2007;25:201–204. doi: 10.1016/j.vaccine.2005.10.057. [DOI] [PubMed] [Google Scholar]
- 4.Walker F.J., Singleton J.A., Lu P., Wooten K.G., Strikas R.A. Influenza vaccination of healthcare workers in the United States, 1989–2002. Infect Control Hosp Epidemiol. 2006;27:257–265. doi: 10.1086/501538. [DOI] [PubMed] [Google Scholar]
- 5.Hofmann F., Ferracin C., Marsh G., Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34:142–147. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 6.Willis B.C., Wortley P. Nurses' attitudes and beliefs about influenza and the influenza vaccine: a summary of focus groups in Alabama and Michigan. Am J Infect Control. 2007;35:20–24. doi: 10.1016/j.ajic.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Weingarten S., Riedinger M., Bolton L.B., Miles P., Ault M. Barriers to influenza vaccine acceptance: a survey of physicians and nurses. Am J Infect Control. 1989;17:202–207. doi: 10.1016/0196-6553(89)90129-6. [DOI] [PubMed] [Google Scholar]
- 8.Perez-Padilla R., de la Rosa-Zamboni D., Ponce de Leon S., Hernandez M., Quinones-Falconi F., Bautista E. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361:680–689. doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 9.Chowell G., Bertozzi S.M., Colchero M.A., Lopez-Gatell H., Alpuche-Aranda C., Hernandez M. Severe respiratory disease concurrent with the circulation of H1N1 Influenza. N Engl J Med. 2009;361:674–679. doi: 10.1056/NEJMoa0904023. [DOI] [PubMed] [Google Scholar]
- 10.Neumann G., Noda T., Kawaoka Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature. 2009;459:931–939. doi: 10.1038/nature08157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peiris J.S.M., Poon L.L.M., Guan Y. Emergence of a novel swine-origin influenza A virus (S-OIV) H1N1 virus in humans. J Clin Virol. 2009;45:169–173. doi: 10.1016/j.jcv.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gatherer D. The 2009 H1N1 influenza outbreak in its historical context. J Clin Virol. 2009;45:174–178. doi: 10.1016/j.jcv.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Shinde V., Bridges C.B., Uyeki T.M., Shu B., Balish A., Xu X. Triple-reassortant swine influenza A (H1) in humans in the United States, 2005-2009. N Engl J Med. 2009;360:2616–2625. doi: 10.1056/NEJMoa0903812. [DOI] [PubMed] [Google Scholar]
- 14.Tam D.K.P., Lee S., Lee S.S. Impact of SARS on avian influenza preparedness in healthcare workers. Infection. 2007;35:320–325. doi: 10.1007/s15010-007-6353-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tam D.K.P., Lee Sh, Lee S. Impact of severe acute respiratory syndrome and the perceived avian influenza epidemic on the increased rate of influenza vaccination among nurses in Hong Kong. Infect Control Hospital Epidemiol. 2008;29:256–261. doi: 10.1086/527507. [DOI] [PubMed] [Google Scholar]
- 16.Looijmans-van den Akker I., van Delden J.J.M., Verheij T.J.M., van Essen G.A., van der Sande M.A.B., Hulscher M.E. Which determinants should be targeted to increase influenza vaccination uptake among health care workers in nursing homes? Vaccine. 2009;27:4724–4730. doi: 10.1016/j.vaccine.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Chor J.S.Y., Ngai K.L.K., Goggins W.B., Wong M.C.S., Wong S.Y.S., Lee N. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ. 2009;339 doi: 10.1136/bmj.b3391. b3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raftopoulos V. Attitudes of nurses in Greece towards influenza vaccination. Nurs Stand. 2008;23:35–42. doi: 10.7748/ns2008.10.23.4.35.c6675. [DOI] [PubMed] [Google Scholar]
- 19.Ofstead C.L., Tucker S.J., Beebe T.J., Poland G.A. Influenza vaccination among registered nurses: information receipt, knowledge, and decision making at an institution with a multifaceted educational program. Infect Control Hosp Epidemiol. 2008;29:99–106. doi: 10.1086/526431. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Novel influenza A (H1N1) virus infections among health-care personnel—United States, April–May 2009. MMWR Morb Mortal Wkly Rep. 2009;58:641–645. [PubMed] [Google Scholar]
- 21.Maurer J., Harris K.M., Parker A., Lurie N. Does receipt of seasonal influenza vaccine predict intention to receive novel H1N1 vaccine: evidence from a nationally representative survey of US adults. Vaccine. 2009;27:5732–5734. doi: 10.1016/j.vaccine.2009.07.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zarocostas J. Healthcare workers should get top priority for vaccination against A/H1N1 flu, WHO says. BMJ. 2009;339 doi: 10.1136/bmj.b2877. b2877. [DOI] [PubMed] [Google Scholar]
- 23.Sekkides O. Responding to the renewed H1N1 pandemic. Lancet Infect Dis. 2009;9:729. [Google Scholar]
- 24.Hong Kong Department of Health. Health facts for Hong Kong. Available from: http://www.dh.gov.hk/english/statistics/statistics_hs/files/Health_Statistics_pamphlet_2009e.pdf. Accessed May 10, 2010.